Abstract
The present study examines two core therapeutic principles of Motivational Interviewing (MI) with alcohol and other substance use disorders. Specifically, therapist focus on client ambivalence and commitment to change, as well as a more general indicator of goal assessment, were tested as process predictors of subsequent alcohol use across four sessions of Motivational Enhancement Therapy. Participants were adult alcohol users involved in a large multi-site clinical trial (Project MATCH; two arms Aftercare [AC] and Outpatient [OP]). A series of multi-level models examined the effect of proposed MI ingredients on alcohol use (percent abstinent days; drinks per drinking day) over a 12-week treatment period, and whether these effects interacted with time and client baseline motivation. Therapist effort to elicit client commitment to change alcohol use was associated with greater rates of abstinence among both AC and OP participants, and reduced drinking quantity among OP participants. However, therapist focus on ambivalence was associated with greater drinking quantity among OP participants, and when motivation was low, among AC participants. Goal assessment was a marginal to non-significant predictor across outcomes, and all interactions with time were non-significant. Therapist reported treatment foci are important to subsequent patterns of drinking within a multi-session MI, but the role of ambivalence and discrepancy is worthy of further clinical and empirical consideration.
Keywords: Ambivalence, Brief Interventions, Commitment to Change, Process Research, Stages of Change, Treatment Ingredients, Motivational Interviewing
Introduction
Scientific attention has shifted to understanding the underlying mechanisms that account for the efficacy of brief interventions based in the principles of Motivational Interviewing (MI). Meta-analytic review supports MI efficacy over minimal comparison conditions (Burke, Arkowitz, & Menchola, 2003; Moyer, Finney, Swearingen, & Vergun, 2001) as well as broad utility across a number of problem areas and clinical contexts (Hettema, Steele, & Miller, 2005). Further, MI has demonstrated comparable effectiveness to more time intensive behavioral alcohol or other drug treatments (Lundahl & Burke, 2009; Vasilaki, Hosier, & Cox, 2006). At this stage of its development, a theory of how MI works is emergent (Miller & Rose, 2009) and with growing empirical support (Apodaca & Longabaugh, 2009; Miller & Rose, 2009). Looking into the ‘black box’ of a treatment with established efficacy enables a refinement of theory via empirical test of its individual elements, which can result in streamlined intervention delivery, knowledge of optimal conditions for implementation, and ultimately, improved outcomes.
MI treatment ingredients
MI researchers now seek to uncover its active ingredients and the mechanisms most responsible for overall client improvement. Active treatment ingredients are treatment elements, processes, and/or therapist behaviors that predict client mechanisms and/or long-term main effects (Longabaugh & Magill, 2011). Treatment ingredients that do not affect subsequent mechanisms or outcomes are inert ingredients while those found to predict poor outcomes are contra-indicated ingredients (Longabaugh & Magill, 2011). A majority of research on MI treatment ingredients has emphasized therapist micro-skills in the context of single session interventions. This body of work has shown that therapist behaviors/skills proscribed in MI (e.g., warnings, excessive advising, confronting) are contra-indicated ingredients (e.g., Gaume, Bertholet, Faouzi, Gmel, & Deappen, 2010; Moyers & Martin, 2006; Moyers, Martin, Tonigan, Houck, & Amrhein, 2007; Moyers, Martin, Houck, Christopher, & Tonigan, 2009). Similarly, prescribed behaviors/skills (e.g., open questions, complex reflections) have positively predicted subsequent mediators (e.g., Catley, Harris, Mayo, Hall, Okuyemi et al., 2006; Gaume, Gmel, Faouzi, & Deappen 2008; 2010; Magill, Apodaca, Barnett, & Monti, 2010; Moyers & Martin, 2006; Moyers et al., 2007; 2009) as well as long-term outcomes (Gaume, Gmel, Faouzi, & Deappen, 2009), and are therefore supported as active MI ingredients. MI therapeutic skills, however, are located within more global measures of MI process such as therapist MI relational style and MI principles.
Technical, relational, and conflict resolution aspects of MI process
Arkowitz and colleagues (2008) identify the technical, relational, and conflict resolution hypotheses of MI, and these can be considered three different levels of MI process analysis (see also Miller & Rose, 2009). The technical hypothesis speaks to those therapist skills/behaviors that predict subsequent statements for (change talk) or against (sustain talk) making behavioral changes, which is a proposed and empirically supported mechanism of action in MI (Amrhein, 2004; Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003). Therapist skills/behaviors are only one level of analysis when looking at active treatment ingredients. The relational hypothesis, identifies the importance of nonspecific therapeutic processes that promote a safe and non-judgmental atmosphere for the exploration of behavior change (Arkowitz, Miller, Westra, & Rollnick, 2008; Miller & Rose, 2009). This line of study has considered primarily global ratings of the overall ‘gestalt’ of the session, and this includes constructs such as empathy and MI Spirit (defined by three primary dimensions: collaboration, evocation, and autonomy). Therapist global rated MI Spirit has predicted outcome for alcohol (Gaume et al., 2008; McNally, Palfai, & Kahler, 2005) but not marijuana (Strang & McCambridge, 2004) users. In addition, MI Spirit and global empathy have been associated with greater involvement in MI sessions as defined by expression of affect, cooperation, and self disclosure (Catley et al., 2006; Moyers, Miller, & Hendrickson, 2005) as well as working alliance (Boardman, Catley, Grobe, Little, & Ahluwalia, 2006).
While both the technical and relational dimensions of proposed MI efficacy have growing empirical evidence, the conflict resolution hypothesis has received less formal investigation in the literature. A well-known definition of MI is as a client-centered and directive approach aimed at exploring and resolving client ambivalence (Miller & Rollnick, 2002). It is client-centered in its orientation to the patient as the agent of change. It is directive in its use of technical reflective listening skills to selectively reinforce client self-motivational statements in the context of a dialogue that examines both the positive and negative aspects of behavior change. The goal is resolve inner conflicts surrounding change as manifested in increasingly frequent and strong client statements in favor of change coupled with reduced sustain talk statements.
Commitment and ambivalence in motivational enhancement therapy
The present study examines two core features of the MI therapeutic style: focus on commitment to change while also focusing on the client’s ambivalence about change. As such, it is a representation of the MI conflict resolution hypothesis where a focus on commitment, coupled with ambivalence, should result in positive behavioral changes. It considers these processes in the context of a four session motivational enhancement intervention, which provides a unique opportunity to examine these purported active ingredients as time-varying predictors of subsequent alcohol use (frequency and quantity). For this reason, we also considered a more general measure of client goal and drinking assessment expected to be of importance to intervention on multiple occasions rather than the more common, single-session, MI format. Here, theoretically derived measures of MI process should act independently of therapist general assessment interventions. Analyses were conducted with Motivational Enhancement Therapy (MET) data from the Project MATCH Aftercare (AC) and Outpatient (OP) samples.
Within the original Project MATCH causal models for the MET condition, constructs relevant to an MI theory of change were proposed to interact with client characteristics in predicting long-term outcomes. Clients with high pre-treatment anger were expected to show superior outcomes in MET when contrasted with cognitive behavioral therapy (CBT) and twelve-step facilitation therapy (TSF). This model was supported for OP participants, but not AC participants at 12-month follow-up with additional support for reduced resistance (indicated by increased alliance, problem recognition, and taking steps toward change) as a mechanism of this effect (Waldron, Miller, & Tonigan, 2001). Subsequent work demonstrated similar relationships within a single AC sample. The authors found that therapist directiveness interacted with client anger to produce poorer drinking outcomes in CBT compared to MET, but not TSF (Karno & Longabaugh, 2004). Our measure of focus on ambivalence includes three related constructs: explore ambivalence, raise a discrepancy between drinking behavior and personal goals and values, and roll with resistance, and therefore provides a complementary look at these exploratory yet non-confrontational processes within MET.
More recent research by Moyers and colleagues (2009) showed that positive change language in the first Project MATCH MET session mediated the relationship between first session MI-consistent micro-skills and drinking quantity at mid-treatment (week 5; combined AC/OP sample). Our measure of focus on commitment includes three related constructs: elicit self-motivational statements, encourage steps to change, and discuss commitment to abstinence, and therefore provides a measure of MI consistent clinical emphasis on client commitment and intention. Finally, the Project MATCH casual models also proposed superior outcomes for low motivation (DiClemente, Carbonari, Zweben, Morrell, & Lee, 2001) and low problem recognition (Miller & Tonigan, 2001) clients in MET when contrasted with CBT and TSF, but these matching hypotheses were unsupported. However, client motivation was prognostic of drinking outcome more generally (DiClemente et al., 2001). As such, we looked at client motivation as a possible moderator of the within treatment MET therapist predictors of interest.
Purpose
The current study examines three putative active ingredients of MI in the context of a multi-session MET intervention. It builds upon emerging empirical support for the multiple levels of MI process (i.e., technical skills, relational processes, and global style/principles) while also considering whether active ingredient effects are conditional upon a theoretically and clinically relevant baseline characteristic. Our aims were to first examine processes within MI sessions descriptively to look at trends over time. Next, we utilized a series of multi-level models to test the effects of three treatment ingredients prospectively on subsequent client drinking within treatment. Specifically, therapist focus on commitment, focus on ambivalence/discrepancy, and general goal assessment were tested as predictors of drinking on average as well as the rate of change in drinking (predictor by time interaction). We expected that both commitment and ambivalence would be positive predictors of subsequent change above and beyond the more general measure of goal/drinking assessment. We then explored whether the effects of these variables would vary by client baseline stage of change.
Method
Sample and procedure
In Project MATCH, the aftercare (AC; n = 774) and outpatient (OP; n = 952) samples were recruited following residential or detoxification treatment, respectively. The AC sample showed greater alcohol severity than the OP sample, including a higher proportion reporting prior alcohol use disorder treatment (AC: 62%; OP: 45%), higher dependence symptoms (AC: M = 6.8[SD = 1.9]; OP: M = 5.8[SD = 1.9]) and higher ASI Psychiatric Severity (AC: M = .19[SD = .19]; OP: M = .23[SD = .21] Project MATCH Research Group, 1997). The majority of participants in each arm (95% – 98%) met criteria for alcohol dependence, as assessed with the Structured Clinical Interview for DSM-III-R. Participants signed informed consent, and the protocol was approved by relevant Institutional Review Boards across 13 Clinical Research Sites. Following recruitment, participants were randomized to one of three 12-week individually-delivered interventions: Cognitive Behavioral Therapy (CBT; Kadden et al., 1992), Twelve-Step Facilitation Therapy (TSF; Nowinski, Baker, & Carroll, 1992), and MET (Miller, Zweban, DiClemente, & Rychtarik, 1992). The MET condition was the focus of the present study.
There were n = 261 participants in the AC MET sample and n = 316 in the OP MET sample. AC general descriptives are as follows: mean age = 42(SD = 11); 82% male; 81% Caucasian; 75% alcohol dependent as indicated by the AUDIT. OP general descriptives are as follows: mean age = 38(SD = 10); 80% male; 74% Caucasian; 60% alcohol dependent as indicated by the AUDIT. Mean participant motivation (URICA score; DiClemente & Hughes, 1990) in both the AC and OP arms was the Action Stage (M = 12.59[SD = 1.86], M = 12.07[SD = 1.77], respectively). Participant retention rates within treatment (up to week 12) were 83.6% and 80.4% in the AC and OP samples, respectively. More complete details regarding this trial are available elsewhere (e.g., Project MATCH Research Group, 1997, 1998).
MET intervention condition
The MET condition consisted of four individual treatment sessions, occurring at weeks 1, 2, 6 and 12 of the study. Developed specifically for use in Project MATCH by Miller and colleagues (1992), the intervention was based on the principles of Motivational Interviewing [MI]), a collaborative, person-centered form of guiding to elicit and strengthen motivation for change (Miller & Rollnick, 2002). The manualized protocol consisted of the following content areas: delivery of personalized feedback, enhancing motivation for change, and planning for change (sessions 1 and 2) and reinforcing progress and revising the plan for change (sessions 3 and 4; Miller et al., 1992). In addition, therapeutic style emphasized four core principles: express empathy, support self-efficacy, roll with resistance, and develop discrepancy. Study therapists had at least a certificate in counseling, at least two years of post-education clinical experience, experience working alcohol users, and allegiance to family, systems, or client-centered methods of therapy (Carroll, Kadden, Donovan, Zweban. & Rounsaville, 1994). Training consisted of didactic instruction and extensive supervised practice sessions until therapists achieved certified proficiency. On an ongoing basis, one-third of sessions were reviewed by the coordinating center (by Dr. Miller) and monthly feedback provided; in addition therapists received weekly on-site supervision (Carroll et al., 1994). There were 14 therapists in the aftercare condition and 13 in the outpatient condition. The intervention was delivered with a high level or treatment integrity and discriminability in relation to the CBT and TSF conditions (Carroll, Connors, Cooney, DiClemente, Donovan et al., 1998).
Measures
Baseline covariates
The proportion of abstinent days in the 30 days prior to baseline assessment was derived from the calendar-based Form 90 Interview (Miller, 1996; Miller & Del Boca, 1994). Client baseline motivation was measured with the University of Rhode Island Change Assessment (URICA; DiClemente & Hughes, 1990). The 32-item likert-rated measure results in four sub-scales Precontemplation, Contemplation, Action, and Maintenance. The overall motivation measure was derived by combining the mean Contemplation, Action, and Maintenance scores and then subtracting the Precontemplation score from this value. The URICA has demonstrated internal consistency although results on the validity of sub-scale clusters have been mixed (Carey, Purnine, Maisto, & Carey, 2006).
Treatment measures
The 15-item therapist report measure contained 12 5-point extensiveness (“not at all”, “a little”, “somewhat”, “considerably”, “extensively”) measures of MET clinical emphasis. For the present work, three composite measures were created1. The first composite captured two of the four core MI principles, therapist emphasis on client ambivalence and discrepancy (3 items, “To what extent did the therapist”: focus on ambivalence, roll with resistance, develop discrepancy; AC α = .492 to .64 over four sessions; OP α = .61 to .78 over four sessions). The second composite addressed therapist focus on client commitment to change (3 items, “To what extent did the therapist”: elicit self-motivational statements, encourage steps toward change, discuss client commitment to abstinence; AC α = .65 to .71 across four sessions; OP α = .62 to .70 across four sessions). The final indicator was a goal assessment composite that consisted of two items: “To what extent did the therapist” assess treatment goals and assess client drinking (AC α = .322 to .60 across four sessions; OP α = .272 to .65 across four sessions) that were included in the therapist report for all three Project MATCH conditions.
Alcohol outcomes
Alcohol consumption was assessed using the Form 90 (Miller, 1996; Miller & Del Boca, 1994). The two drinking outcome variables were: percentage of abstinent days (PDA) and number of drinks per drinking day (DDD); these measures were arcsine and square root transformed, respectively. This was to reduce distributional skew as well as to remain consistent with existing reports on the Project MATCH PDA and DDD measures.
Data-analysis
Client baseline and therapist predictor descriptives were examined with means, standard deviations, and frequencies. A series of multi-level models examined therapist intervention effects (measured at each session) on alcohol use (measured in between sessions), while controlling for the effects of baseline alcohol use (PDA; DDD) and the linear effect of time. A nested analytic approach examined: 1) the main effects of the three MI ingredients on drinking in between sessions (PDA; DDD) over the course of the within-treatment period (12 weeks), 2) the effects of these predictors on the slope of change in drinking over time (xi by time), and 3) the interaction of these predictors with client readiness in relation to drinking on average and the slope of change drinking over time (wi by xi by time; Singer & Willett, 2003). All variables examined in interaction terms were centered at the mean to reduce possible multicollinearity among predictors (Aiken & West, 1991). Analyses were conducted in SAS 9.2 PROC MIXED. If significant interactions were detected, the significance of simple slopes were tested using methods described by Bauer and Curran (2005; see also Preacher, Curran, & Bauer, 2006).
Results
Therapist predictor and client alcohol use over time
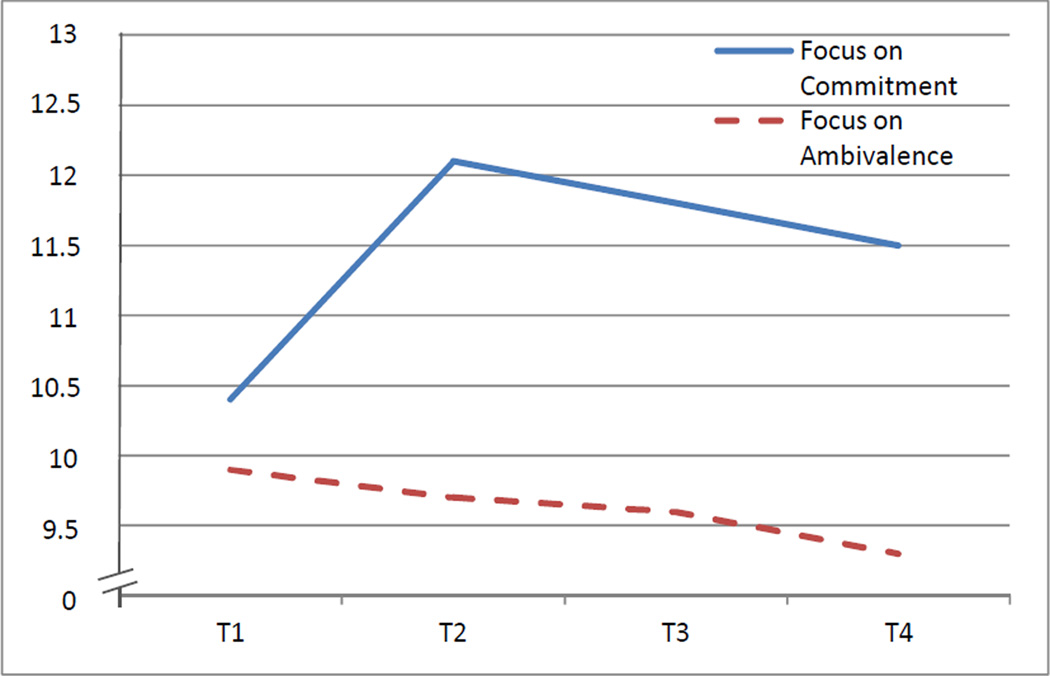
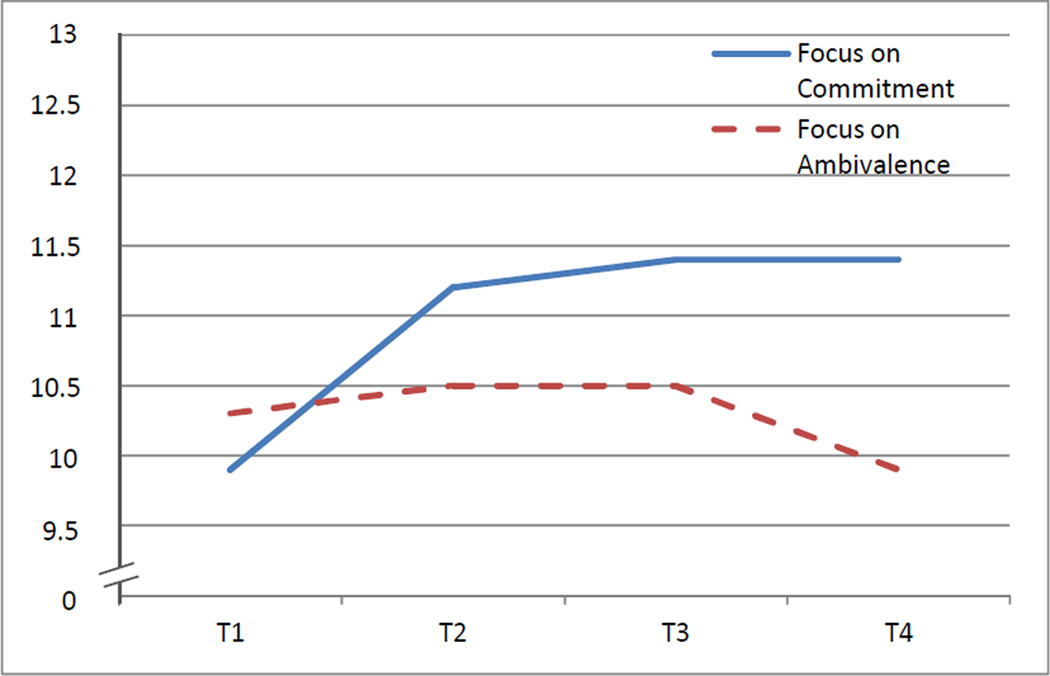
Table 1 shows descriptive data on the three treatment variables at each time point. Descriptively, therapist focus on client ambivalence and developed discrepancy occurred “somewhat” across study arms though slightly higher with OP participants. This emphasis decreased with time in AC (p < .001; Figure 1) and remained relatively stable in OP with a decrease after session three (Figure 2). An emphasis on commitment to change was “considerably” emphasized. Figure 2 shows this focus was higher for AC participants, and had a peak emphasis for both conditions in session two. For goal assessment, AC emphasis was somewhat higher than the OP emphasis, and occurred “considerably” across MET sessions. This emphasis increased with time in AC (p < .001) and remained relatively stable in OP. Table 1 additionally shows client alcohol use in between sessions. For AC participants, average abstinence was 93.5% (18.7) with 2.06 (4.96) drinks per drinking day; both frequency and quantity of alcohol use increased for AC participants over time (p <.001). For OP participants, average abstinence was 79.5% (39.2) with 4.6 (6.5) drinks per drinking day. In contrast to AC participants, OP participants showed a non-significant decrease in drinking frequency over time and an increase in drinking quantity on drinking days (p <.001).
Table 1.
Descriptive data on therapist process predictors
| Therapist Process Predictors | Time 1 M(SD) |
Time 2 M(SD) |
Time 3 M(SD) |
Time 4 M(SD) |
|---|---|---|---|---|
| Aftercare | ||||
| Ambivalence (range 3 – 15) | 9.87(2.36) | 9.70(2.41) | 9.63(2.37) | 9.25(2.70)** |
| Commitment (range 3 – 15) | 10.42(2.10) | 12.11(1.94) | 11.79(1.90) | 11.52(2.09)** |
| Assessment (range 2 – 10) | 5.33(1.70) | 7.55(1.34) | 7.63(1.58) | 7.55(1.59)** |
| PDA in between sessions | 96.29(15.19) | 93.86(17.78) | 90.46(21.69)** | |
| DDD in between sessions | 0.81(3.00) | 2.53(5.51) | 3.02(5.89)** | |
| Outpatient | ||||
| Ambivalence (range 3 – 15) | 10.29(1.78) | 10.47(1.93) | 10.48(2.14) | 9.93(2.50) |
| Commitment (range 3 – 15) | 9.93(1.96) | 11.30(1.74) | 11.40(1.79) | 11.43(1.82)** |
| Assessment (range 2 – 10) | 7.56(3.33) | 7.11(1.45) | 7.21(1.56) | 7.20(1.52) |
| PDA in between sessions | 77.99(33.85) | 79.41(29.39) | 89.90(26.04) | |
| DDD in between sessions | 4.10(7.07) | 5.03(5.65) | 4.65(5.50)** |
Notes.
Linear time effect significant at .001 level.
Figure 1.
Therapist process predictors across four sessions: AC sample\
Figure 2.
Therapist process predictors across four sessions: OP sample
Effects on subsequent drinking within treatment
Table 2 shows the results for therapist MI variables in relation to subsequent client drinking after controlling for baseline abstinence and the linear effect of time. Therapist focus on ambivalence did not predict client drinking among the AC participants, and was associated with worse drinking outcomes (increased DDD) among OP participants. Therapist focus on commitment was associated with improved drinking outcomes for all participants (greater PDA among both AC and OP clients, along with reduced DDD for OP clients and a trend-level effect (p = .06) for AC clients. Therapist assessment of client goals and drinking was associated with worse client drinking (greater DDD) at the .05 level among AC participants, and no effect for OP participants. While some effects were demonstrated for drinking on average, therapist process predictors did not affect the rate of change in drinking over time in the AC and OP samples.
Table 2.
Therapist MI process predictors in relation to client within treatment alcohol use
| Fixed Effects (Level 2) | PDA | DDD | ||||
|---|---|---|---|---|---|---|
| b | t(df) | p | b | t(df) | p | |
| Aftercare | ||||||
| BL alcohol use | −0.01 | −0.19(316) | .849 | −0.07 | −1.17(316) | .243 |
| Time | −0.06 | −4.48(316) | <.001 | 0.29 | 4.38(316) | <.001 |
| Ambivalence | −0.00 | −0.78(316) | .44 | 0.04 | 1.31(316) | .19 |
| Commitment | 0.02 | 2.30(316) | .02 | −0.07 | −1.90(316) | .06 |
| Assessment | −0.01 | −1.59(316) | .11 | 0.08 | 1.94(316) | .05 |
| Interactions with time | ||||||
| Ambivalence by time | −0.01 | −1.78(313) | .08 | 0.04 | 1.53(313) | .13 |
| Commitment by time | 0.01 | 1.66(313) | .09 | −0.05 | −1.15(313) | .25 |
| Assessment by time | −0.00 | −0.29(313) | .77 | −0.04 | −0.80(313) | .42 |
| Outpatient | ||||||
| BL alcohol use | 0.41 | 6.61(428) | <.001 | 0.08 | 1.06(428) | .287 |
| Time | −0.02 | −1.92(428) | .06 | 0.31 | 5.44(428) | <.001 |
| Ambivalence | −0.01 | −1.15(428) | .25 | 0.07 | 2.39(428) | .02 |
| Commitment | 0.02 | 2.58(428) | .01 | −0.10 | −2.95(428) | <.01 |
| Assessment | −0.01 | −1.68(428) | .09 | 0.02 | 1.01(428) | .31 |
| Interactions with time | ||||||
| Ambivalence by time | 0.01 | 1.19(425) | .23 | 0.00 | 0.08(425) | .93 |
| Commitment by time | 0.00 | 0.33(425) | .76 | −0.05 | −1.18(425) | .24 |
| Assessment by time | 0.00 | 0.40(425) | .68 | −0.04 | −0.93(425) | .35 |
Notes.
Effects significant at p ≤ .05 highlighted in bold font.
BL alcohol was measured by PDA and DDD.
Outcome transformations maintain directionality and relative magnitude in interpreting coefficient estimates.
Moderation by client motivational readiness
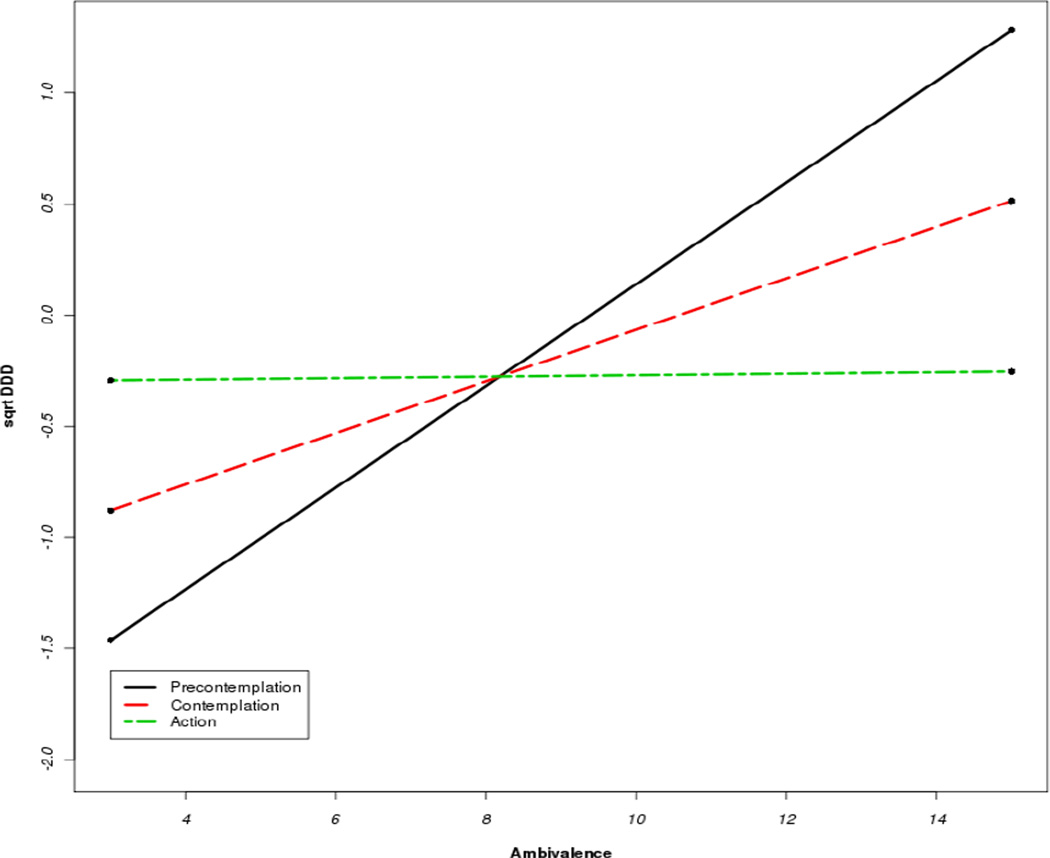
Table 3 shows results for therapist process predictors interacted with client baseline motivation. These interactions were non-significant with the exception of therapist focus on ambivalence with clients low in motivation in the aftercare sample. As depicted in Figure 3, the tests of simple slopes showed a focus on ambivalence was associated with the most positive slope in DDD when clients were in the Precontemplation Stage (b = 0.23(0.08), t = 2.84, p < .005) and the Contemplation Stage (b = 0.12(0.04), t = 3.08, p < .005). The 3-way interactions with time (i.e., whether therapist effect on rate of change varied by client motivation) were non-significant in both the AC and OP samples.
Table 3.
Therapist MI process predictors by client motivation in relation to within treatment alcohol use
| Fixed Effects (Level 2) | PDA | DDD | ||||
|---|---|---|---|---|---|---|
| b | t | p | b | t | p | |
| Aftercare | ||||||
| Baseline motivation | 0.02 | 1.56(300) | .12 | −0.04 | −1.06(299) | .29 |
| Ambivalence by motivation | 0.00 | 0.41(300) | .68 | −0.04 | −2.27(299) | .02 |
| Commitment by motivation | −0.01 | −1.69(300) | .09 | 0.04 | 1.61(299) | .11 |
| Assessment by motivation | 0.00 | 0.81(300) | .42 | −0.02 | −0.87(299) | .38 |
| Outpatient | ||||||
| Baseline motivation | 0.04 | 2.75(402) | .01 | −0.05 | −1.14(402) | .26 |
| Ambivalence by motivation | 0.01 | 1.74(402) | .08 | −0.01 | −0.41(402) | .68 |
| Commitment by motivation | −0.00 | −1.33(402) | .18 | 0.00 | 0.02(402) | .98 |
| Assessment by motivation | 0.00 | 0.21(402) | .83 | −0.01 | −0.53(402) | .60 |
Notes.
Effects significant at p ≤ .05 highlighted in bold font.
Outcome transformations maintain directionality and relative magnitude in interpreting coefficient estimates.
Figure 3.
Therapist focus on ambivalence by client readiness among AC participants
Discussion
The technical aspect of how MI works refers to the idea that when the therapist makes proficient use of specific skills, this will increase client change talk, which will predict behavior change (Arkowitz et al., 2008; Miller & Rose, 2009). A second aspect considered comprises relational factors, including elements such as empathy, positive regard, and the therapeutic focus of the clinician. A unique and central aspect of the MI approach is that motivation is not assumed by the therapist but discovered through the interchange between the therapist and client. Arguments for change are systematically sought “…while maintaining a warm and supportive atmosphere for exploration of ambivalent feelings” (Miller, 1996, p. 840). This report focuses on these two elements of the MI therapeutic style, therapist focus on ambivalence about change and therapist focus on commitment to change, as putative active ingredients.
Therapist focus on ambivalence
Contrary to our expectations, therapist focus on ambivalence across four sessions of MET was not a consistent predictor of reduced drinking frequency. In fact, it was actually associated with worse drinking quantity outcomes (number of drinks per drinking day) among OP clients, and among AC clients who were at the Precontemplation and Contemplation Stages. There are a number of possible explanations for these findings. First, while a focus on ambivalence might be an important part of the change process, it may not be directly predictive of outcome in and of itself. In other words, perhaps most (or even all) clients receiving treatment in this study were led to explore their ambivalence, but only those who achieved conflict resolution of their ambivalence and thus a stronger commitment to change had better drinking outcomes. This interpretation must be validated in future research by examining the temporal sequence of ambivalence and discrepancy based interventions in relation to subsequent indicators of commitment (e.g., slope of change statements, agreement to complete a change plan). Second, the present study actually supported a focus on ambivalence as a contraindicated treatment ingredient in relation to drinking quantity. This may, however, reflect the reciprocal nature of the therapeutic relationship in that clients who were feeling unsure about whether to change their drinking or were struggling with slips might have led MET therapists to see a continued need to explore ambivalence, develop discrepancy, and roll with resistance. This possibility may also be supported by our results showing absent time-dependent effects. Specifically, effects were seen for drinking quantity on average but not a positive slope (i.e., effect on the rate of increase) in heavy drinking over the course of MET treatment.
Finally, therapist focus on ambivalence predicted worse drinking quantity outcomes among clients in the OP arm of the study, and when motivation was low, in the AC arm. This highlights differences in patient populations across study arms. Those in the OP sample likely had more variability to their level of motivation and commitment because they entered treatment immediately following a detoxification episode. In contrast, those in the AC arm of the study had completed inpatient treatment (14 to 28 days), and continued outpatient care in MATCH could have represented these patients’ Action Stage. Therefore, the effect of focus on ambivalence on drinking quantity would only be detected only among those AC clients with remaining contemplative and precontemplative feelings. However, recent work has shown that first session change language did not systematically differ in the expected directions across motivational stages within a Project MATCH sample (Hallgren & Moyers, 2011). While stage of change may not invariably predict therapist focus on ambivalence, this constellation of interventions appear to be emphasized more often with clients who are struggling, but will not necessarily result in resolution to commitment.
Therapist focus on commitment
Therapist focus on commitment was associated with improved drinking outcomes for all participants across both outcome measures. Thus, focus on commitment is an independent, active ingredient within this sample. This finding is also consistent with the emerging literature emphasizing the importance of commitment in MI process and efficacy. For example, in a review of the literature on MI mechanisms of change, Apodaca and Longabaugh (2009) found MI leads to higher levels of intention to change substance use in comparison with standard care control groups, and that intention also has a consistent positive effect on outcomes. Among the numerous client variables examined, commitment/change talk was highlighted as one of the most consistent and promising candidates as a potential mechanism of change (Apodaca & Longabaugh, 2009), lending sound support for therapist eliciting commitment as a key ingredient in MI efficacy. Research has since added further evidence linking client commitment during treatment to improved drinking outcomes at followup (e.g., Moyers, et al., 2009; Vader, Walters, Prabhu, Houck, & Field, 2010), but preparatory change language (reasons, need, desire, ability) may also play a vital role with more contemplative samples (Gaume, Bertholet, Faouzi, Gmel, & Deappen, in press). Continued research is needed to examine how change language constructs, which map on conceptually to motivational constructs, may vary within patient sub-samples representing various stages of readiness.
An additional finding of interest relates to the timing of therapist process variables. As seen in Figures 1 and 2, therapists in both the outpatient and aftercare arms of the study tended to focus more on commitment as clients progressed through treatment, and with a peak at session two. In contrast, there was relatively less focus on ambivalence over time. This represents a prototypic view of MI’s prescribed goal to help clients to “explore and resolve ambivalence” as part of the change process. In other words, therapist focus on ambivalence should be higher at the beginning of treatment during the phase of “exploring”. As ambivalence resolves, there should be less need for ambivalence focus, and the therapeutic focus shifts to enhancing commitment to change. This transition maps onto what is described as “Phase One” and “Phase Two” of MI (Miller & Rollnick, 2002). In this view, it is important for the therapist to explore both sides of the ambivalence, and that MI would be incomplete if it failed to evoke both counter-change as well as pro-change arguments. To our knowledge, this report is the first operationalized examination of the conflict resolution hypothesis of MI. While time dependent effects on drinking were not seen in our analyses, this model is worthy of continued testing. Our findings additionally show there are certain clients where resolution may not be attained, at least within a 12 week/four session protocol.
Finally, processes of ambivalence and commitment rose above other therapist foci tested as putative ingredients of MI. First, our third MI relational style variable, focus on empathy and self-efficacy, was consistently non-significant and therefore trimmed from the analyses. Next, therapist assessment of client goals and drinking was associated with worse drinking quantity among AC participants and not among OP participants. This later variable was conceptualized as a non-specific control in that these interventions are more common across behavioral treatments while additionally having some overlap with the two MI ingredients tested. Therefore therapist focus on ambivalence and commitment were independent of the more general process of goal assessment.
Limitations and conclusions
This study has some limitations to consider. Because the sample for the current study was derived from Project MATCH, caution is warranted. The version of MI used in that study, MET, represented a distinct application of MI delivered across four sessions, which is in contrast to a number of MI process studies that have been conducted with single-session applications. At the same time, the four-session protocol of MET allowed for analytic advances that are a strength of the current study. In addition, due to limitations in process measurement, we were unable to examine whether the active ingredients were uniquely predictive in the MET condition, or additionally important in CBT and TSF. Further, our measures are best framed as approximations of MI processes that should be replicated with observational rating approaches. While clustering observer-rated behaviors into ambivalence or commitment-based interventions will not necessarily improve the internal consistency of derived measures, it can validate the accuracy of therapist report while also allowing even greater time-dynamic within-session assessment than prospective modeling across treatment sessions. The present study is an important first step in this regard. It attends to key dynamic of motivational interventions and within a longitudinal multi-session framework. Finally, generalizability from the present study may best apply to populations similar to those who participated in Project MATCH (treatment seeking and primarily alcohol dependent), and replication across samples representative of varying stages of the change process is needed. Finally, while lagged longitudinal models increase confidence in our results, some caution is always warranted when drawing conclusions from correlational studies.
The present study adds to the evidence supporting a focus on commitment as an active ingredient in MI. However, whether this ingredient is unique to MI remains unknown. Further study of this process, established and empirically supported in the MI literature, will provide important information as to its role in behavioral interventions more broadly. The present study did not support the positive predictive role of a focus on ambivalence; rather, this work suggests that ambivalence has complex relations to motivation and drinking. The role of this emphasis by the MI therapist warrants continued study to identify where it can and cannot be used to its theoretically-proposed conflict resolution effect.
ACKNOWLEDGEMENT
This manuscript is based on a study, Within and Post-Session Change Mechanisms in Treatment for Alcohol Use Disorders, supported by the National Institute on Alcohol Abuse and Alcoholism (K23-AA018126). The findings are the responsibility of the authors and do not reflect positions of the National Institutes of Health.
Footnotes
We examined a fourth composite that included two additional MI principles: express empathy and support self-efficacy. However, this variable was non-significant and therefore trimmed from our models. Two items, extent to which the therapist included the significant other and provided personalized feedback, were not assessed in the present work.
This value at session 1.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc.; 1991. [Google Scholar]
- Amrhein PC. How Does Motivational Interviewing Work? What Client Talk Reveals. Journal of Cognitive Psychotherapy. 2004;18(4):323–336. [Google Scholar]
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of action in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. PMID:19413785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arkowitz H, Miller WR, Westra HA, Rollnick S. Motivational Interviewing in the treatment of psychological problems: Conclusions and future directions. In: Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational Interviewing in the Treatment of Psychological Problems. New York: Guilford; 2008. [Google Scholar]
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40(3):373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? Journal of Substance Abuse Treatment. 2006;31(4):329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Burke B, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Carey KB, Purnine DM, Maisto SA, Carey MP. Assessing Readiness to Change Substance Abuse: A Critical Review of Instruments. Clinical Psychology: Science and Practice. 1999;6(3):245–266. [Google Scholar]
- Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Kadden RR, et al. Internal validity of Project MATCH treatments: Discriminability and integrity. Journal of Consulting and Clinical Psychology. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kadden RM, Donovan DM, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. Journal of Studies on Alcohol and Drugs, Supplement. 1994;12:149–155. doi: 10.15288/jsas.1994.s12.149. [DOI] [PubMed] [Google Scholar]
- Catley D, Harris K, Mayo MS, Hall S, Okuyemi KS, Boardman T, Ahluwalia JS. Adherence to principles of motivational interviewing and client within-session behavior. Behavioural and Cognitive Psychotherapy. 2006;34(1):43–56. [Google Scholar]
- DiClemente CC, Carbonari J, Zweben A, Morrel T, Lee RE. Motivation hypothesis causal chain analysis. In: Longabaugh R, Wirtz PW, editors. Project MATCH hypotheses: Results and causal chain analyses. Washington, DC: Government Printing Office; 2001. pp. 206–222. NIAAA Project MATCH Monograph Series Vol. 8, DHHS Publication No (ADM) 01-4238). [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. Journal of Substance Abuse. 1990;2(2):217–235. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Gaume J, Bertholet N, Faouzi M, Gmel G, Daeppen J. Counselor motivational interviewing skills and young adult change talk articulation during brief motivational interventions. Journal of Substance Abuse Treatment. 2010;39(3):272–281. doi: 10.1016/j.jsat.2010.06.010. [DOI] [PubMed] [Google Scholar]
- Gaume J, Bertholet N, Faouzi M, Gmel G, Daeppen JB. Does change talk during brief motivational interventions with young men predict change in alcohol use? Journal of Substance Abuse Treatment. doi: 10.1016/j.jsat.2012.04.005. (Under Review). Submitted to the. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Daeppen JB. Brief alcohol interventions: Do counselors’ and patients’ communication characteristics predict change? Alcohol and Alcoholism. 2008;43:62–69. doi: 10.1093/alcalc/agm141. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Faouzi M, Daeppen J. Counselor skill influences outcomes of brief motivational interventions. Journal of Substance Abuse Treatment. 2009;37(2):151–159. doi: 10.1016/j.jsat.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Hallgren KA, Moyers TB. Does readiness to change predict in-session motivational language? Correspondence between two conceptualizations of client motivation. Addiction. 2011;106(7):1261–1269. doi: 10.1111/j.1360-0443.2011.03421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Kadden R, Carroll KM, Donovan D, Cooney N, Monti P, et al. Cognitive-Behavioral Coping Skills Therapy Manual: A clinical research guide for therapists treatment individuals with alcohol abuse and dependence. Washington, DC: Government Printing Office; 1992. NIAAA Project MATCH Monograph Series. Vol. 3 [Publication No (ADM) 92-1895)]. [Google Scholar]
- Karno MP, Longabaugh R. What do we know? Process analysis and the search for a better understanding of project MATCH'S anger-by-treatment matching effect. Journal of Studies on Alcohol. 2004;65(4):501–512. doi: 10.15288/jsa.2004.65.501. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Magill M. Recent advances in behavioral addiction treatments: focusing on mechanisms of change. Current Psychiatry Reports. 2011;13(5):382–389. doi: 10.1007/s11920-011-0220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. Journal of Clinical Psychology. 2009;65(11):1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- McNally AM, Palfai TP, Kahler CW. Motivational interventions for heavy drinking college students: examining the role of discrepancy-related psychological processes. Psychology of Addictive Behaviors. 2005;19(1):79–87. doi: 10.1037/0893-164X.19.1.79. [DOI] [PubMed] [Google Scholar]
- Magill M, Apodaca TR, Barnett NP, Monti PM. The route to change: Within-session predictors of change plan completion in a motivational interview. Journal of Substance Abuse Treatment. 2010;38(3):299–305. doi: 10.1016/j.jsat.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal Of Studies On Alcohol. 1994;(SUPPL):12112–12118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR. Manual for Form-90: A structured assessment interview for drinking and related behaviors. Washington, DC: Government Printing Office; 1996. NIAAA Project MATCH Monograph Series. Vol. 5 [Publication No. (ADM) 96-4004)]. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford; 1991/2002. [Google Scholar]
- Miller WR, Rollnick S. Ten things that Motivational Interviewing is not. Behavioural and Cognitive Psychotherapy. 2009;37:129–140. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Alcohol problem recognition and outcomes. In: Longabaugh R, Wirtz PW, editors. Project MATCH hypotheses: Results and causal chain analyses. Washington, DC: Government Printing Office; 2001. pp. 223–238. NIAAA Project MATCH Monograph Series Vol. 8, DHHS Publication No. (ADM) 01-4238). [Google Scholar]
- Miller WR, Zweban A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual: A clinical research guide for therapists treatment individuals with alcohol abuse and dependence. Washington, DC: Government Printing Office; 1992. NIAAA Project MATCH Monograph Series. Vol. 2 [Publication No. (ADM) 92-1894)]. [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. Journal of Substance Abuse Treatment. 2006;30:245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31(S3):40S–47S. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology. 2009;77(6):1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, Miller WR, Hendrickson SML. How Does Motivational Interviewing Work? Therapist Interpersonal Skill Predicts Client Involvement Within Motivational Interviewing Sessions. Journal of Consulting and Clinical Psychology. 2005;73(4):590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll KM. Twelve-Step Facilitation Therapy Manual: A clinical research guide for therapists treatment individuals with alcohol abuse and dependence. Washington, DC: Government Printing Office; 1992. NIAAA Project MATCH Monograph Series. Vol. 1 [Publication No. (ADM) 92-1893)]. [Google Scholar]
- Preacher K, Curran P, Bauer D. Computational Tools for Probing Interactions in Multiple Linear Regression, Multilevel Modeling, and Latent Curve Analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY US: Oxford University Press; 2003. [Google Scholar]
- Spitzer RL, Williams JB. Structured Clinical Interview for DSM-III (SCID) New York: Biometrics Research Division, New York State Psychiatric Institute; 1985. [Google Scholar]
- Strang J, McCambridge J. Can the practitioner correctly predict outcome in motivational interviewing? Journal of Substance Abuse Treatment. 2004;27(1):83–88. doi: 10.1016/j.jsat.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Vader AM, Walters ST, Prabhu GC, Houck JM, Field CA. The language of motivational interviewing and feedback: Counselor language, client language, and client drinking outcomes. Psychology of Addictive Behaviors. 2010;24:190–197. doi: 10.1037/a0018749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilaki E, Hosier SG, Cox W. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Miller WR, Tonigan JS. Client anger as a predictor of differential response to treatment. In: Longabaugh R, Wirtz PW, editors. Project MATCH hypotheses: Results and causal chain analyses. Washington, DC: Government Printing Office; 2001. pp. 134–148. NIAAA Project MATCH Monograph Series Vol. 8, DHHS Publication No. (ADM) 01-4238). [Google Scholar]