Abstract
Objective
To determine the clinical value of uterine artery Doppler Pulsatility index (PI) at 22–24 + 6 weeks scan and importance of maternal history and mean arterial pressure (MAP) in the prediction of pre-eclampsia.
Materials and Methods
This was a prospective screening study of 200 women with singleton pregnancy. Maternal history and blood pressure were recorded, and MAP was calculated. Transabdominal Doppler ultrasound of uterine artery was performed. Mean PI was calculated, and the presence or the absence of bilateral early diastolic notch was noted. Women were then followed up through pregnancy and delivery for the development of pre-eclampsia, gestational hypertension, and SGA.
Results
The mean ± SD PI value for subjects who had an adverse pregnancy outcome was significantly higher (0.84 ± 0.28) than mean ± SD PI value for subjects who had normal pregnancy outcome (0.71 ± 0.16) with P value <0.000.
Conclusion
Second trimester uterine artery Doppler is a useful screening method for identification of high risk pregnancy in women who can be kept under close surveillance for better maternal and neonatal outcome. This test works better when combined with previous history of pre-eclampsia and MAP.
Keywords: Pre-eclampsia, Prediction, Maternal history, Uterine artery Doppler, Mean arterial pressure
Introduction
Pre-eclampsia, which affects about 2 % of pregnancies, is thought to be the consequence of impaired trophoblastic invasion of the maternal spiral arteries and their conversion from narrow vessels to wide non-muscular channels [1].
The early detection of the risk of this complication may allow for the improvement of the outcome by increasing patient surveillance or by initiating a therapeutic intervention [2].
With the use of Doppler technology, it has been possible to show a strong positive correlation between uterine vascular resistance, expressed by an elevated pulsatility index (PI) or persistence of an early diastolic notch in the Doppler waveform and hypertensive disease in pregnancy, especially pre-eclampsia and fetal growth restriction (FGR) [3].
An abnormal uterine artery Doppler velocimetry result between 22 and 26 weeks of gestation is considered to be a surrogate marker of chronic uteroplacental ischemia [4].
Risk factors associated with pre-eclampsia include maternal diabetes, chronic hypertension, renal disease, thrombophilias, and autoimmune disorders. Obstetric factors associated with high risk are multiple pregnancies, previous pre-eclampsia, and molar or hydropic pregnancies. Other risk factors are first pregnancy, and extremes of age and obesity. A family history of pre-eclampsia may suggest a genetic predisposition [5].
Doppler assessment is noninvasive and thus acceptable to patients. It is a specialized technique, both in terms of the equipments required and the operator’s expertise. It could be fairly easily performed at the time of detailed anomaly scan [6].
This study was undertaken to evaluate the association between uterine artery Doppler velocimetry at 22–24 + 6 weeks gestation, maternal history, mean arterial pressure (MAP) and the development of pre-eclampsia (early and late onset), gestational hypertension, and small for gestational age (SGA) babies.
Materials and Methods
This was a prospective screening study conducted at the department of Obstetrics and Gynecology, Sir Sayajirao General Hospital, Baroda Medical College over a period of 1 year. A total of 250 subjects were enrolled. Women with singleton pregnancy attending routine antenatal care at 22–24 + 6 weeks were recruited. Gestational age was calculated from last menstrual period (LMP) and confirmed by first trimester ultrasound where LMP was not known.
Demographic and clinical risk factors were noted: maternal age, religion, cigarette smoking, alcohol intake, medical history (including chronic hypertension, diabetes mellitus, antiphospholipid syndrome thrombophilia, HIV Infection, and sickle cell disease), method of conception [spontaneous versus use of ovulogens or in vitro fertilization (IVF)], parity, obstetric history (including previous pregnancy with pre-eclampsia), family history of pre-eclampsia)and maternal height, weight, and Body Mass Index (BMI).
Blood pressure was taken by standard mercury manometer with the women in sitting position, their arms supported at the level of the heart. After resting for 5 min, blood pressure was measured in both arms, and a series of recordings were made at 5-min intervals for three times. The MAP of each arm was calculated, and the arm with the highest final MAP was used for subsequent measurements as well as for the analysis of results.
Transabdominal Doppler ultrasound of uterine artery was performed using a 5-MHz transducer, MYLAB 50 (Esaote Ltd., Italy) color Doppler, and 4D ultrasound machine. All scans were performed by a single operator. The examination was performed by the same observer using the method recommended by the Fetal Medicine Foundation.
Spectral Doppler signals from three similar consecutive waveforms were obtained, and the PI measured, and the mean PI was calculated. The presence or the absence of bilateral early diastolic notch was noted.
Women were then followed up through pregnancy and delivery for the development of complications such as pre-eclampsia, gestational hypertension, and SGA.
Statistical Analysis
The data were entered in an excel sheet. Data analysis was performed using SPSS version 17. For intergroup comparisons, the tests of significance were χ2-test and one way Anova test. The sensitivity, specificity, and positive predictive values and likelihood ratios for different mean uterine artery PI (Ut.API) cut-offs in the prediction of adverse pregnancy outcomes were calculated. Logistic regression and receiver operating characteristic (ROC) curve analysis were performed to define the best predictors for the outcomes examined. The area under the curve (AUC) and the 95 % CI were calculated. For this, we used the Medcalc for windows software. Results were considered to be statistically significant when P < 0.05.
Results
Table 1 shows the distribution of the mean, 5th percentile, 50th percentile, and 95th percentile values of PI in our study population.
Table 1.
Mean, 5th, 50th, and 95th percentiles for the mean uterine artery pulsatility index (Ut.API) between 22 and 24 + 6 weeks of gestation
| PI | ||||||
|---|---|---|---|---|---|---|
| Week | Mean | SD | 5th percentile | 50th percentile | 95th percentile | n |
| 22 | 0.80 | 0.22 | 0.56 | 0.74 | 1.27 | 62 |
| 23 | 0.70 | 0.19 | 0.43 | 0.66 | 1.13 | 75 |
| 24 | 0.75 | 0.21 | 0.42 | 0.71 | 1.11 | 63 |
The mean ± SD PI at 22 weeks was 0.80 ± 0.22, and at 24 weeks, the value was 0.75 ± 0.21. The PI values varied from 0.42 at 5th percentile at 24 weeks to 95th percentile values of 1.11, thus showing a decreasing trend from 22 to 24 weeks.
Table 2 shows the mean ± SD PI values in pregnancies with normal and abnormal outcomes.
Table 2.
Uterine artery Doppler findings in normal and abnormal pregnancies
| Type of pregnancy outcome | PI | ||
|---|---|---|---|
| n | Mean ± SD | p | |
| Normal | 138 | 0.7 ± 0.16 | 0.000 |
| Abnormal | 62 | 0.84 ± 0.28 | |
The mean ± SD PI value for subjects who had a normal pregnancy outcome was 0.71 ± 0.16, and the mean ± SD PI value for subjects who had an adverse pregnancy outcome was 0.84 ± 0.28. This association between the PI value and adverse pregnancy outcome is highly significant at P < 0.000.
Table 3 shows the screening characteristics of the 2nd trimester uterine artery Doppler at a PI value of >90th percentile for the adverse pregnancy outcome. The mean PI value at 90th percentile was 1.047.
Table 3.
Screening characteristics of the 2nd trimester uterine artery Doppler PI > 90th percentile for pregnancy outcome in study population
| Type of pregnancy outcome | Sensitivity (%) | Specificity | Positive predictive value | Negative predictive value | Positive likelihood ratio (95 % CI) | Negative predictive value (95 % CI) |
|---|---|---|---|---|---|---|
| Pre-eclampsia | 30.30 | 94.01 | 50 | 87.22 | 5.06 (2.29, 11.18) | 0.74 (0.59, 0.93) |
| Gestational hypertension | 33.33 | 91.49 | 20 | 95.56 | 3.92 (1.55, 9.9) | 0.73 (0.49, 1.09) |
| SGA | 16.67 | 90.91 | 20 | 88.89 | 1.83 (0.67, 5.03) | 0.92 (0.76, 1.1) |
| Pre-eclampsia with SGA | 33.33 | 90.72 | 10 | 97.78 | 3.59 (1.07, 12.1) | 0.73 (0.42, 1.3) |
The sensitivity of Ut.API was the best in the prediction of pre-eclampsia with SGA and gestational hypertension at 33.33 %. The specificity of Ut.API > 90th percentile was the best for pre-eclampsia at 94 %.
The PPV of Ut.API > 90th percentile was the best for pre-eclampsia at 50 %, and NPV of Ut.API > 90th percentile was the best for pre-eclampsia with SGA at 97.78 %. These figures are in general agreement with those found in other studies [7].
Positive likelihood ratio with 95 % CI was the best for pre-eclampsia at 5.06 (2.29–11.18).
Table 4 shows the mean PI values in pregnancies that resulted in adverse pregnancy outcomes versus the mean PI values in pregnancies without the adverse outcomes. The difference in mean PI was significant for pre-eclampsia at P < 0.000 and for gestational hypertension at P < 0.03.
Table 4.
A comparison of the statistically significant differences in mean Doppler measurements obtained from pregnancies that resulted in development of pre-eclampsia, SGA, and gestational hypertension
| Uterine artery PI | No pre-eclampsia | Pre-eclampsia | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | 95 % CI | n | Mean | SD | 95 % CI | P value | |
| Mean PI | 167 | 0.7 | 0.18 | 0.698–0.702 | 33 | 0.9 | 0.31 | 0.895–0.905 | 0.000 |
| AGA | SGA | ||||||||
| Mean PI | 176 | 0.7 | 0.21 | 0.698–0.702 | 24 | 0.8 | 0.23 | 0.795–0.805 | 0.495 |
| No gestational hypertension | Gestational hypertension | ||||||||
| Mean PI | 188 | 0.7 | 0.21 | 0.698–0.702 | 12 | 0.9 | 0.24 | 0.886–0.914 | 0.031 |
Table 5 shows the comparison of the performance of screenings for early and late pre-eclampsia, gestational hypertension and SGA by UTAPI, MAP, and past history of pre-eclampsia.
Table 5.
Comparison of the performance of screening for pre-eclampsia, gestational hypertension, and SGA by Ut.API, MAP, and past history of pre-eclampsia
| Performance of screening test AUC and (95 %CI) | Early pre-eclampsia | Late pre-eclampsia | Gestational hypertension | Small for gestational age |
|---|---|---|---|---|
| Ut.API | 0.945 (0.904–0.972) P < 0.0001 |
0.609 (0.538–0.677) P < 0.0861 |
0.664 (0.594–0.729) P < 0.07 |
0.548 (0.476–0.618) P < 0.48 |
| MAP | 0.896 (0.845–0.935) P < 0.0001 |
0.676 (0.606–0.740) P < 0.0006 |
0.529 (0.457–0.599) P < 0.76 |
0.554 (0.482–0.624) P < 0.438 |
| Past history of pre–eclampsia | 0.795 (0.733–0.849) P < 0.08 |
0.607 (0.535–0.675) P < 0.01 |
0.501 (0.430–0.572) P < 0.98 |
0.594 (0.522–0.662) P < 0.04 |
| Combined factors | – | 0.721 (0.611–0.83) | 0.602 (0.426–0.778) | 0.562 (0.434–0.689) |
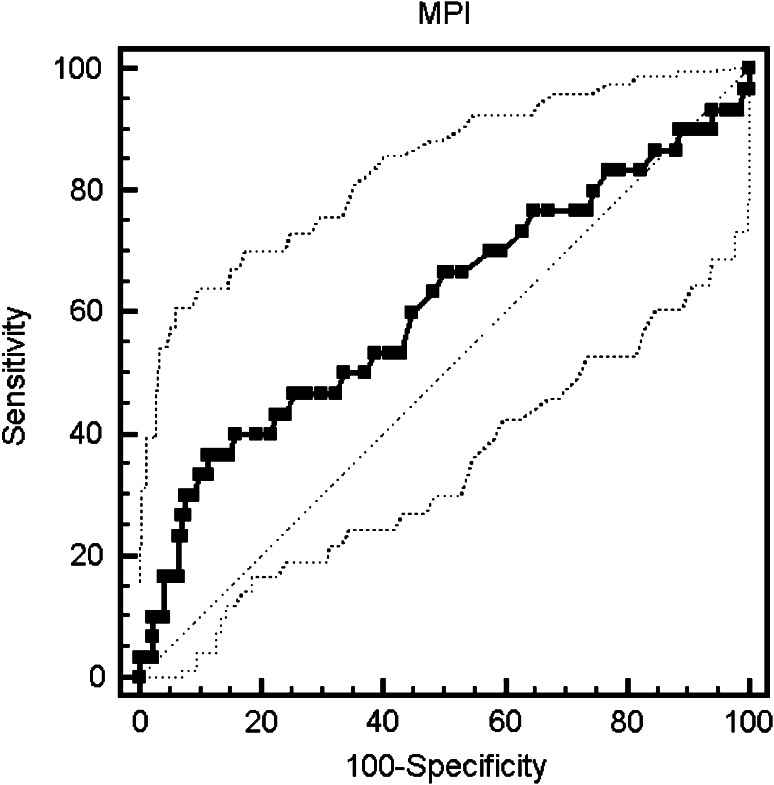
The AUC and 95 % CI for UTAPI are highly significant for early onset PE; AUC and 95 % CI for MAP are highly significant for both early-onset and late-onset PE (Fig. 1).
Fig. 1.
The ROC of prediction of late pre-eclampsia using mean Ut.API. AUC is 0.609; 95 % CI: 0.538–0.677; significance level 0.08
Discussion
This prospective study was conducted on 250 consecutive women at 22–24 weeks gestation, to study the relationship between uterine artery Doppler and adverse pregnancy outcomes. Fifty women were lost to follow-up, and their pregnancy outcomes are not known to us. The final analysis was performed on 200 women.
Seventeen women had a history of pre-eclampsia in previous pregnancies. Seventy-three (36.5 %) of the 200 subjects were primigravidae. One 38 subjects had normal pregnancy outcome, whereas 62 (31 %) had adverse pregnancy outcomes in the form of pre-eclampsia (n = 33), SGA (n = 24), and gestational hypertension (n = 12). The Ut.API values showed a decreasing trend from 22 to 24 weeks of gestation. Seven subjects showed a diastolic notch of which six were unilateral, and one was bilateral.
The birth weight in mean ± SD in normal pregnancy group was 2,685 ± 376 g, and in the group with an adverse outcome, it was 2,406 ± 393 g. This observation was statistically significant at P < 0.000.
The mean ± SD PI at 22 weeks was 0.80 ± 0.22, and at 24 weeks, its value was 0.75 ± 0.21. The PI values varied from 0.42 at 5th percentile at 24 weeks to 95th percentile values of 1.11, thus showing a decreasing trend from 22 to 24 weeks. Other studies have also confirmed that Ut.API showed a significant and progressive decline with gestation. Continuing throughout the third trimester until 34 weeks, although the prevalence of bilateral notch remains almost stable beyond 25 weeks of gestation [7–10].
Gomez et al. [11], has published reference intervals for mean uterine PI values from 11 to 41 weeks. In this reference table, the corresponding value for 5th percentile at 24 weeks was 0.64, and the value of 95th percentile was 1.35. We have been unable to locate published reference ranges for the Indian population.
The median PI was 0.715. The 5th percentile value was 0.44, 90th percentile was 1.047, and 95th percentile was 1.1748. There were only 10 of women whose mean PI was at 95th percentile, and so for purpose of analysis we have taken the 90th percentile cut off.
The mean ± SD PI value for subjects who had a normal pregnancy outcome was 0.71 ± 0.16, and the mean ± SD PI value for subjects who had an adverse pregnancy outcome was 0.84 ± 0.28. This association between the PI value and adverse pregnancy outcome is highly significant at P < 0.000.
Aardema et al. [12], in a study in Netherlands, found that the PI at 22 weeks in women with normal pregnancy outcome was 0.94 (0.76–1.24), and the medial PI in women with poor pregnancy was 1.73 (1.16–2.36). This association was also highly significant.
Harringon et al. [13] compared the uterine artery mean Doppler values obtained from pregnancies that resulted in appropriate for gestational age (AGA) babies and those which resulted in delivery of SGA babies. The mean PI, in subjects who delivered an AGA baby was significantly less as compared to the values in women who delivered a SGA baby.
Palma-Dias et al. [14] in a study on 954 subjects have shown the screening test characteristics of mean PI > 1.55. The sensitivity varied from 18.1 % for FGR to 29.2 % for pre-eclampsia. The PPV varied from 25.5 % for FGR to 47.1 % for placental insufficiency. This study used the transvaginal route for screening.
Three risk factors were found to be useful in prediction of adverse pregnancy outcome in combination: previous history of pre-eclampsia, MAP and Ut.API > 90th percentile. Onwudiwe et al. [1] studied 3,529 singleton pregnancies at 22–24 weeks gestation using multiple regression analysis. They found that Ut.API and MAP provided a significantly independent contribution in prediction of pre-eclampsia, gestational hypertension, and SGA. They also demonstrated that screening on the basis of maternal characteristics alone would identify only about 30 % of pregnancies destined to develop pre-eclampsia at a false positive rate of 10 %. A more effective approach is the one that combines maternal history with measurement of blood pressure and Ut.API.
This screening can be quite easily offered to women at the 22-week anomaly scan. Although, at present, no prophylactic interventions are known to reduce the risk of PE, detection of women at risk for adverse pregnancy outcome in the second trimester will help us put them under increased surveillance to ensure a good maternal and fetal outcome.
The values of Ut.API in our study for the 90th and 95th percentile were 1.04 and 1.17 respectively. These values are much lower than those reported in the worldwide literature that we reviewed. A large multicentric trial would be required to address this issue. We are not aware of any such nomograms for the Indian population.
Conclusion
Second trimester uterine artery Doppler is a useful screening method for identification of high risk pregnancy in women who can be kept under close surveillance for better maternal and neonatal outcome. This test works better when combined with previous history of pre-eclampsia and MAP.
References
- 1.Onwudiwe N, Yu CKH, Poon LCY, Spiliopoulos I, Nicolaides KH. Prediction of pre-eclampsia by a combination of maternal history, uterine artery Doppler and mean arterial pressure. Ultrasound Obstet Gynecol. 2008;32:877–883. doi: 10.1002/uog.6124. [DOI] [PubMed] [Google Scholar]
- 2.Ohkuchi A, Minakami H, Sato F, Mori H, Nakano T, Tateno M. Predicting the risk of pre-eclampsia and small for gestational age infant by quantitative assessment of the diastolic notch in uterine artery flow velocity waveforms in unselected women. Ultrasound Obstet Gynecol. 2000;16:171–178. doi: 10.1046/j.1469-0705.2000.00192.x. [DOI] [PubMed] [Google Scholar]
- 3.Zimmermann P, Eiri Ö, Koskinen J, Kujansuu E, Ranta T. Doppler assessment of the uterine and uteroplacental circulation in the second trimester in pregnancies at high risk for pre-eclampsia and/or intrauterine growth retardation: comparison and correlation between different Doppler parameters. Ultrasound Obstet Gynecol. 1997;9:330–338. doi: 10.1046/j.1469-0705.1997.09050330.x. [DOI] [PubMed] [Google Scholar]
- 4.Espinoza J, Romero R, Jyn KN, Gomez R, Kusunovic JP, Goncalves LF. Identification of patients at high risk for early onset and/or severe pre-eclampsia with the use uterine artery Doppler velocimetry and placental growth factors. Am J Obstet Gynecol. 2007;96(4):326.01–326.13. doi: 10.1016/j.ajog.2006.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cnossen S, Morris RR, Gerben R, Ben WJ, Joris AM, Coomarasamy A. Use of uterine artery Doppler Sonography to predict pre-eclampsia and intrauterine growth restriction: a systematic review and bivariable meta-analysis. CMAJ. 2008;178(6):701–711. doi: 10.1503/cmaj.070430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cnossen JS, Joris AM, Khalid SK, et al. Prediction of pre-eclampsia: a protocol for systematic reviews of test accuracy. BMC Pregnancy Childbirth. 2006;6:29. [DOI] [PMC free article] [PubMed]
- 7.Papageorghiou AT, Yu CKH, Bindra R, Pandis G, Nicolaides KH. Multi-center screening for pre-eclampsia and fetal growth restriction by trans-vaginal uterine artery Doppler at 23 weeks of gestation. Ultrasound Obstet Gynecol. 2001;18:441–449. doi: 10.1046/j.0960-7692.2001.00572.x. [DOI] [PubMed] [Google Scholar]
- 8.Plasencia W, Maiz N, Poon L, Yu C, Nicholaides KH. Uterine artery Doppler at 11 + 0 to 13 + 6 weeks and 21 + 0 to 24 + 6 weeks in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol. 2008;32:138–146. doi: 10.1002/uog.5402. [DOI] [PubMed] [Google Scholar]
- 9.Aardema MW, De Wolf BTHM, Saro MCS, Osterhof H, Fidler V, Aarnoudse JG. Quantification of the diastolic notch in Doppler ultrasound screening of uterine arteries. Ultrasound Obstet Gynecol. 2000;16:630–634. doi: 10.1046/j.1469-0705.2000.00289.x. [DOI] [PubMed] [Google Scholar]
- 10.Yazici FG, Tok E, Gulhan S, Ertunc D, Ozdemir G, Dilek S. Relationship of early diastolic notch in uterine artery Doppler measurements with pregnancy complications in low risk pregnancies. Perinatal J. 2005;13:152–157. [Google Scholar]
- 11.Gomez O, Figueras F, Fernadez S, Bennasar M, Martinez JM, Puerto B, Gratacos E. Reference ranges for uterine artery mean pulsatility index at 11–41 weeks of gestation. Ultrasound Obstet Gynecol. 2008;32:128–132. doi: 10.1002/uog.5315. [DOI] [PubMed] [Google Scholar]
- 12.Aardema MW, Saro MCS, Lander M, De Wolf BT, Oosterhof H, Aarnoudse JG. Second trimester Doppler ultrasound screening of the uterine arteries differentiates between subsequent normal and poor outcomes of hypertensive pregnancy: two different pathophysiological entities. Clin Sci. 2004;106:377–382. doi: 10.1042/CS20030385. [DOI] [PubMed] [Google Scholar]
- 13.Harrington K, Goldfrad C, Carpenter R, Campbell S. Transvaginal uterine and umbilical artery Doppler examination at 12–16 weeks and the subsequent development of pre-eclampsia and intrauterine growth retardation. Ultrasound Obstet Gynecol. 1997;9:94–100. doi: 10.1046/j.1469-0705.1997.09020094.x. [DOI] [PubMed] [Google Scholar]
- 14.Palma-Dias RS, Mercedes MC, Brietzke E, Fritsch A, Schlatter D, Maurmann CB, et al. Screening for placental insufficiency by transvaginal uterine artery Doppler at 22–24 weeks of gestation. Fetal Diagn Ther. 2008;24:462–469. doi: 10.1159/000178141. [DOI] [PubMed] [Google Scholar]