Abstract
During replantation of distal fingertip amputation, identification of the artery is the most important but time consuming procedure. Depending on the damaged arterial structure, we classified distal fingertip amputations into 4 zones, on the basis of three dimensional concept. Zone 1 injury was defined as damage to the proximal central pulp artery; zone 2 injury, damage to the branch of the central pulp artery; zone 3 injury, damage to the distal central pulp artery; and zone 4 injury, no injury to the central pulp artery, injury only to the lateral pulp artery. From April 2010 to June 2011, 27 patients were evaluated. Successful replantation was observed in 21 patients. Skin necrosis occurred in six patients. For distal fingertip amputation classification based on the damaged arterial system is an easy method to find out the appropriate artery which should be anastomosed during replantation.
Keywords: Replantation, Distal fingertip amputation, Central pulp artery
Introduction
Distal fingertip amputations (DFA) were classified into various categories [1, 2, 3]. In most of the studies, the reported classifications were based on two dimensional concept. Sebastin and Chung [4] reported a systematic review on replantation of DFA. Their classification is based on transverse amputation type [4].
We often experience that if an amputation occurs in a lateral or volar oblique direction, the injury patterns do not fall into the existing classifications. In this regard, to include all injury patterns into one single classification system, first we defined DFA as “an amputation state that occurred distal to the distal tranverse volar digital arch”. And then we classified the amputation pattern into four zones, according to the site of damage to the central pulp artery (CPA), branches of it and lateral pulp artery (LPA); considering the diameter of the vessel and finally analyzed the clinical results.
The purpose of this study is to classify the distal fingertip amputation, on the basis of three dimensional concept, according to the arterial supply to find out an easy way to localize appropriate artery which should be anastomosed during replantation.
Materials and Methods
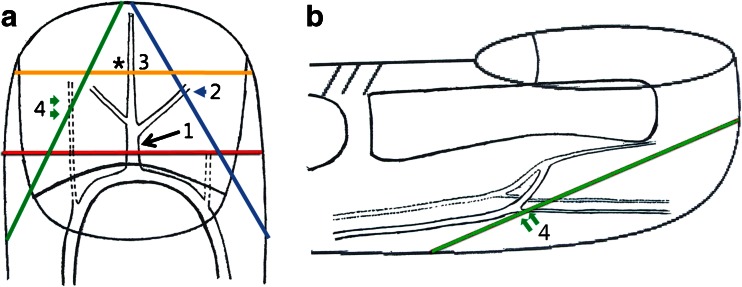
From April 2010 to June 2011, we evaluated all the patients with DFA treated by replantation in our centre. We classified DFA into four zones by the damage of arterial structures based on operative findings (Fig. 1, Table 1).
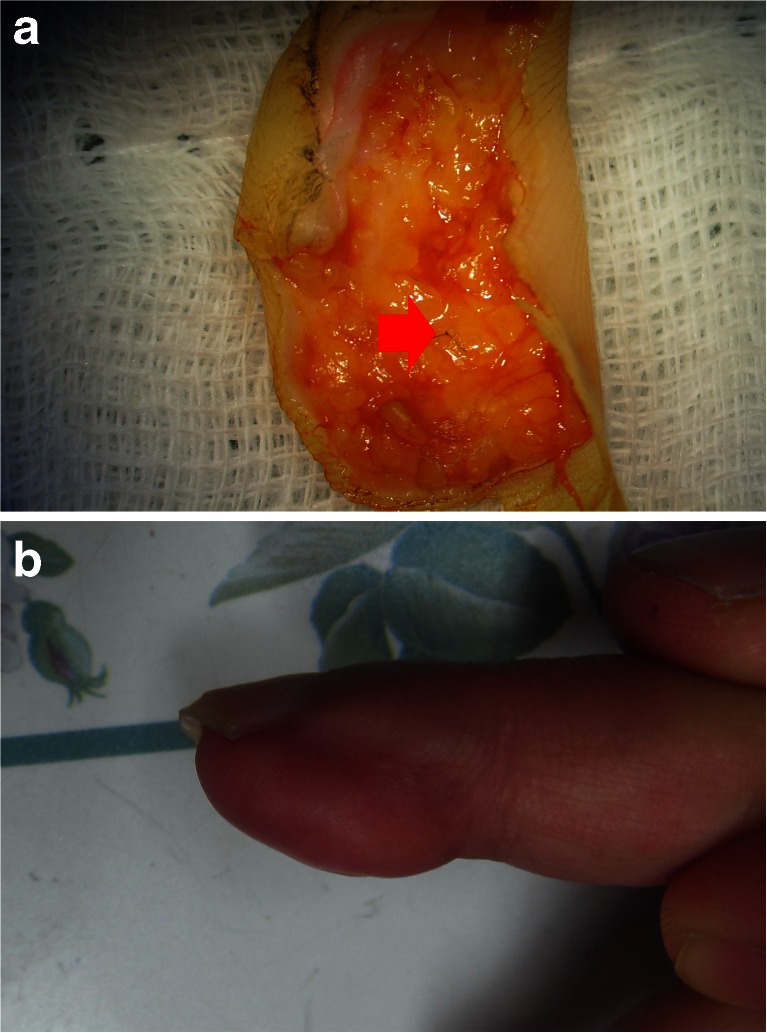
Fig. 1.
a Zone 1. Damage of the proximal CPA (Arrow). Most cases show transverse amputation forms. Zone 2. Damage of the branch of CPA (Arrow head). Zone 3. Damage of the distal CPA (Asterion). Zone 4. No damage to the CPA and its branches. Only LPA is damaged (Double arrow) and b usually amputation occurs in a volar oblique direction
Table 1.
Demographic and clinical outcome of the patients
| Zone | Total number | Mean age (years) | Sex(M:F) | Operation time (hours) | Number of stitches (range) |
|---|---|---|---|---|---|
| 1 | 11 | 35.9 | 8:3 | 2.77 | 3–5 |
| 2 | 5 | 45.8 | 5:0 | 2.15 | 4–6 |
| 3 | 7 | 41 | 6:1 | 1.89 | 3–4 |
| 4 | 4 | 41.5 | 3:1 | 2.12 | 3–4 |
| Total | 27 | 41.05 | 22:5 | 2.23 |
Zone 1 injury was defined as amputation at the proximal CPA. The direction of the amputation was either transverse or lateral oblique in most cases (Figs. 1a and 2). Zone 2 injury was defined as amputation at the branch of the CPA. The main direction of the amputation was lateral oblique (Figs. 1a and 3). Zone 3 injury was defined as amputation at the distal CPA. The main direction of the amputation was transverse (Figs. 1a and 4). Lastly, zone 4 injury was defined as damage of the LPA without the involvement of the CPA and its branch. The direction of the amputation was volar oblique (Figs. 1a, b and 5). When we found that injury occurred at multiple blood vessels, that is to CPA, its branch or LPA; we classified the injury in terms of the diameter of the vessel. That is, we included that case into the group of involvement of larger diameter vessel.
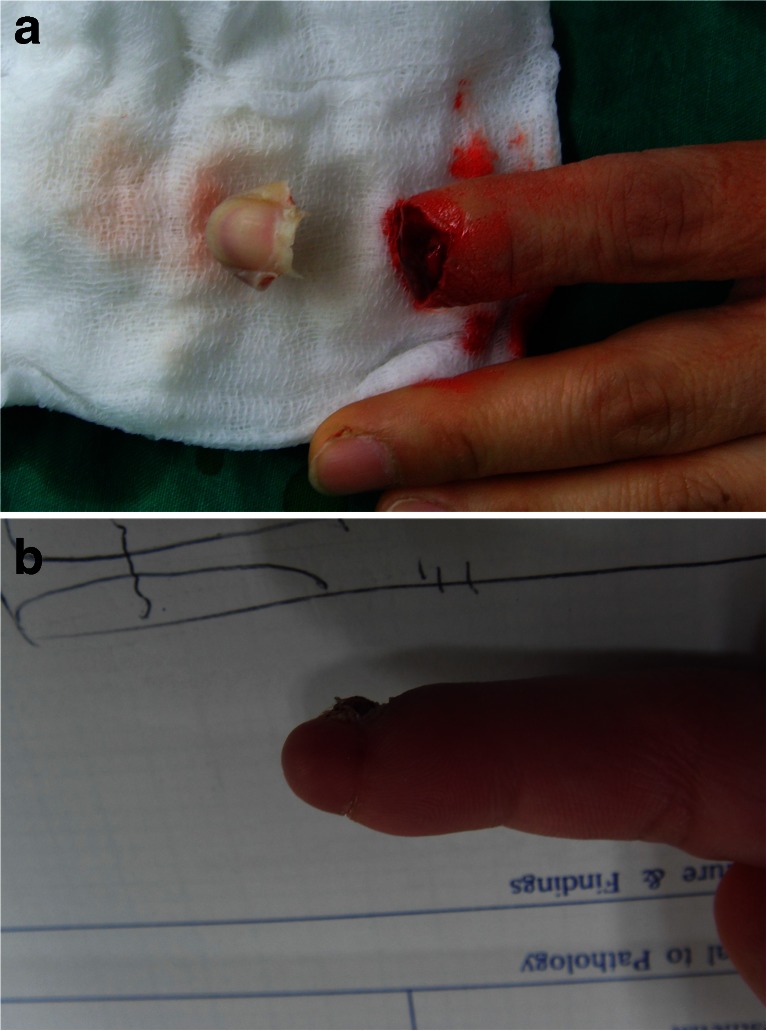
Fig. 2.
Zone 1. a Most cases show transverse amputation forms. b At 2 months after surgery, the result is successful
Fig. 3.
Zone 2. a Most cases show lateral oblique amputation forms. b At 1 month after surgery, all tissues survive
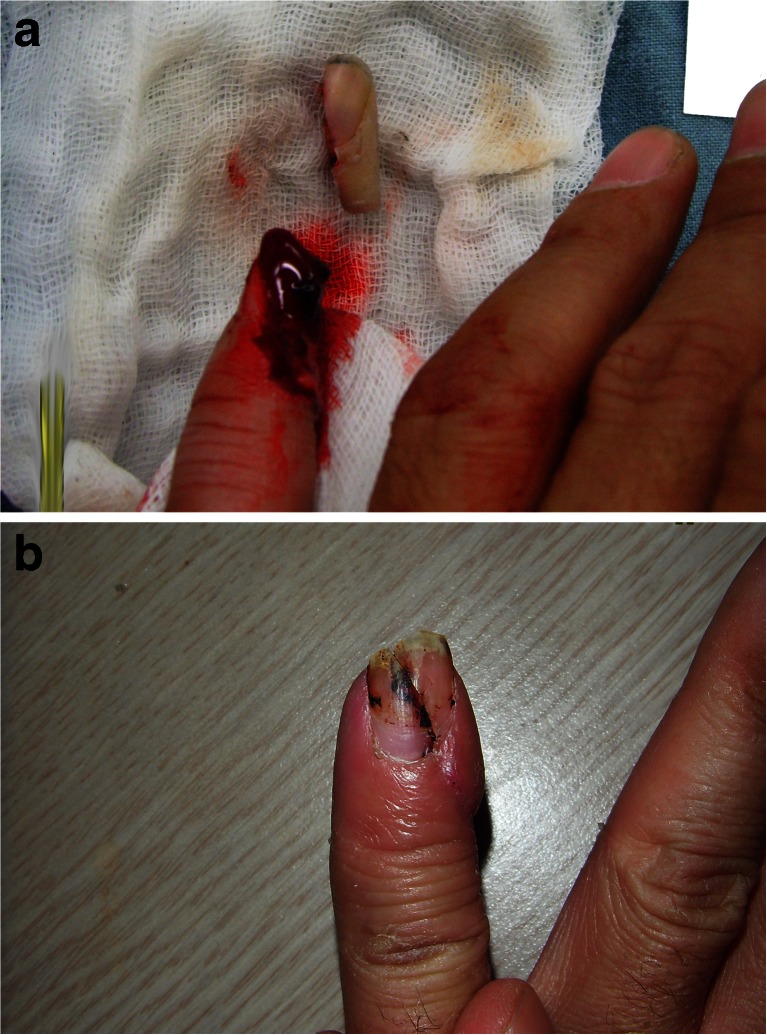
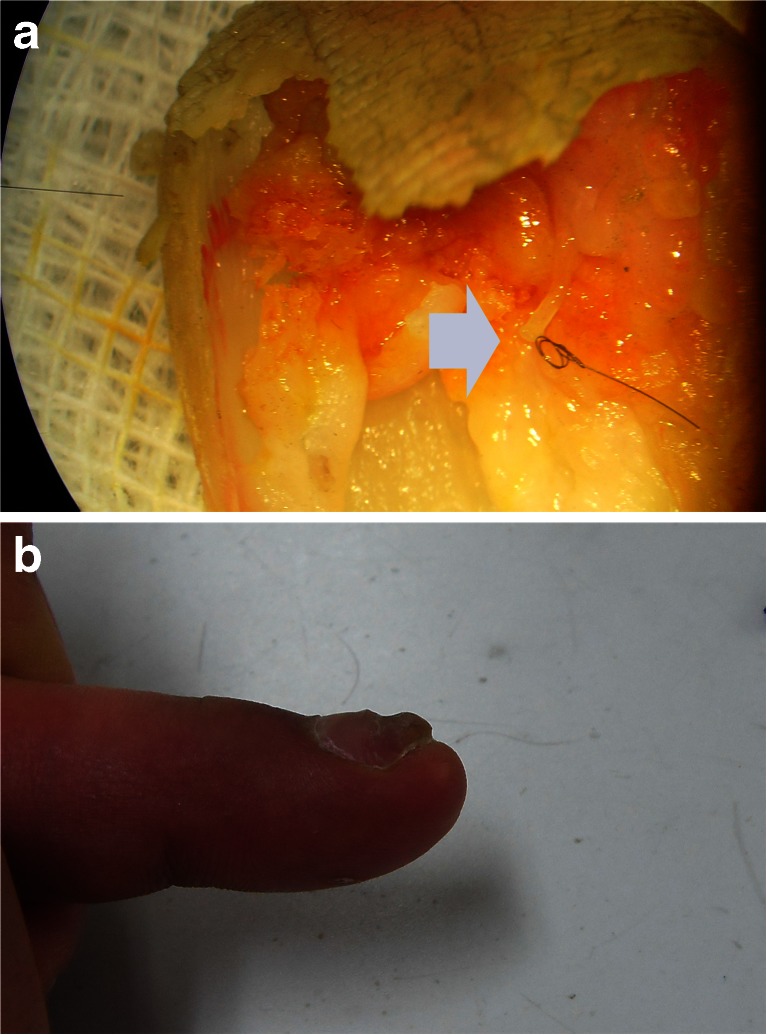
Fig. 4.
Zone 3. a At microscopic examination, the CPA is found in the middle of the finger. No branch is found (Arrow). b At 2 months after surgery, the result is successful
Fig. 5.
Zone 4. a To determine the location of the artery, marking is made during surgery (Arrow). The marked artery is located laterally. b At 6 months after surgery, the skin shows good survival
We evaluated 27 patients with a minimum follow-up of 1 month. The mean follow up period was 2.8 months (range, 1.0–6.4 months). There were 22 male and five female patients. The mean age was 40.0 years (range, 15–58 years). Injury mechanisms were avulsion in three patients, crushing in 17, and guillotine in seven. The mean operation time was 2.3 h (range, 1.5–4.3 h). In all cases, we performed one arterial anastomosis, no venous anastomosis or arterio-venous shunting procedure or ananstomosis of nerves were done. During operation, magnification of operation field was 20 times, and suture materials used were monofilament 10-0 or 11-0 nylon. The range of stiches were 3–5 for zone 1 injury; 4–6 for zone 2 injury; 3–4 for zone 3 and zone 4 injury. In every case, after replantation we confirmed immediate post-anastomic circulation by a cut on replanted part. If there was no external bleeding, we re-explored the anastomotic site, removed the clot and again performed the anastomosis.
Postoperatively, we used intravenous heparin (20 IU/kg/h) for 7 days, and aspirin (325 mg/day) for 14 days along with analgesics and antibiotics. We continued salvage procedure by external bleeding technique in all patients to prevent venous congestion with an average duration of 9.9 days (range, 7–12 days).
Replantation was performed using the same technique to each zone by one surgeon.
To evaluate the success rate of each zone, x2 test was done. Logistic regression analysis was performed for variables (zone, number of stitches, type of injury) on success rate.
Results
Among the 27 patients, 11 were in zone 1, five were in zone 2, seven were in zone 3, and four patients were in zone 4 (Table 1).
After 3 weeks of replantation, by debridement of fingertip crust, we determined whether there was skin necrosis or not. When there was skin necrosis and the necrosis needed further procedure, we consider it as failure.
Successful replantation occurred in 21 cases. The respective success rates were eight in zone 1, four in zone 2, six in zone 3, and three in zone 4. However, the success rate of each zone was not significant statistically (p = 0.930, x2 test) (Table 2). Six cases developed skin necrosis. In zone 1, skin necrosis was observed in three cases, two of which were treated with V-Y advancement flaps, and one was treated with full-thickness skin graft. One case in zone 2 and one in zone 3 with skin necrosis were treated with V-Y advancement flap. One skin necrosis patient in zone 4 was underwent debridement and subsequently treated with full thickness skin graft. However, this patient complained of sustained pain in the finger.
Table 2.
Success rate of each zone
| Zone | Success number | Failure number | Total | Most injury mechanism | Injury pattern | Damaged artery | Test statistic |
|---|---|---|---|---|---|---|---|
| 1 | 8 | 3 | 11 | Crushing | Transverse or lateral oblique | Proximal central pulp artery | x2 = 0.450, df = 3 |
| 2 | 4 | 1 | 5 | Guillotine | Lateral oblique | Branch of central pulp artery | p = 0.930 |
| 3 | 6 | 1 | 7 | Crushing | Transverse | Distal central pulp artery | |
| 4 | 3 | 1 | 4 | Avulsion | Volar oblique | Lateral pulp artery | |
| Total | 21 | 6 | 27 |
As our main concentration was on survival of the replanted part, our follow up period was limited. In all survival patients there were nail deformity, pulp atrophy and even shortening of the finger. But patients were happy with their replanted finger tip with deformed nail. Variables (zone, number of stitch, type of injury) were analyzed using logistic regression analysis (Table 3). But the results were not statistically significant.
Table 3.
Analysis of variables on success rate (zone, number of stitches, type of injury)
| B | S.E. | Wald | df | P-value | Exp(B) | 95 % of CI | |
|---|---|---|---|---|---|---|---|
| Zone | 0.38 | 0.59 | 0.42 | 1 | 0.519 | 1.46 | 0.46–4.64 |
| Number of stiches | 0.41 | 0.74 | 0.31 | 1 | 0.578 | 1.51 | 0.36–6.37 |
| Type of injury | −0.38 | 0.85 | 0.20 | 1 | 0.657 | 0.69 | 0.13–3.61 |
p < 0.05 is statistically significant
B = regression coefficient, S.E. = standard error, df = degree of freedom, Exp(B) = exponentiation of the B coefficient, Cl = confidence interval
Discussion
Digital arteries in each side of the fingers meet distal to the distal insertion of the flexor digitorum profundus to form the distal transverse volar digital arch and then branches into three or four arteries [5, 6]. These arteries decrease in size from 0.8 mm to 0.3 mm in the branch. CPA usually has the largest diameter among the branches [6]. In the process of arch formation, CPA is located in the deep space of the pulp near the distal phalanx (Fig. 1). Its location is deeper than LPA [2, 7].
In case of zone 1 injury, morphologically the majority of amputation was transverse or lateral oblique. To find out the ruptured CPA in the proximal part, we checked the bleeding point after releasing the tourniquet. In the distal stump, we checked the corresponding point of the proximal bleeding site. However it was not found easily and the procedure was also time consuming. We always found CPA in the deeper area near the bone.
Zone 2 injury, which referred to the amputation at the branch of CPA, showed lateral oblique amputation. At the mid-level of the CPA, a transverse branch was observed and it was used for anastomosis. The arterial diameter of the branch of CPA is more than LPA, and the large cross section in zone 2 than zone 1, are the main reasons of high success tendency in zone 2 than zone 4 and 1.
Zone 3 injury was the most distal injury. Injuries at this zone were treated by various surgical methods other than replantation e.g. composite grafting, V-Y advancement flap, and cross-finger flap [8–11]. As in most of the cases, the blood vessels of the distal stump were damaged by crushing injury; we first checked the distal portion of CPA in amputed part. After finding out the artery in distal amputed stump, replantation was attempted.
Koshima et al. [5] reported that the digital artery changed to subdermal arterioles in the finger pulp. For the injuries in zone 3, we usually do anastomosis between the distal portion of CPA and subdermal arterioles, instead of proximal portion of CPA, as proximal portion of CPA was located in the deep space of the pulp and usually damaged by crushing injury. Before anastomosis, we always checked the bleeding of subdermal arteriole after releasing the tourniquet. We consider that high success tendency of this zone is mainly due to small volume of tissue and relatively large cross sectional area. The method of anastomos is also enhances the success rate. Injury at this zone sometimes may not need microsurgical repair, but demands higher technical skill during replantation.
Injuries in zone 4 were volar oblique amputation form morphologically. As described above, volar oblique amputation can often preserve the CPA as it is located in the deep pulp space, while damaging the LPA only. Major difference between zone 2 and zone 4 is injury to the branch of CPA. If there is damage on the branch of CPA near its origin, amputation is classified into the zone 2. And when there is damage to LPA with intact CPA, we classified it as zone 4. In this zone, first we check the proximal part with releasing the tourniquet whether CPA is intact or not. If CPA is intact, the injury is classified into zone 4. And in this zone, we explored only the lateral portion of the distal stump to find out LPA. There are many difficulties in anastomosing the LPA because of its small diameter and the injury pattern. So, there is relatively high failure rate.
Conclusion
Knowledge about the anatomy of finger pulp arterial system is beneficial for distal fingertip replantation. This three dimensional concept classification, based on the damaged arterial system, is useful to predict the site of the ruptured artery to be anastomosed. It can make distal fingertip replantation easier.
Acknowledgments
Conflict of Interest
All named authors hereby declare that they have no conflicts of interest to disclose.
References
- 1.Shi D, Qi J, Li D, Zhu L, Jin W, Cai D. Fingertip replantation at or beyond the nail base in children. Microsurgery. 2010;30(5):380–385. doi: 10.1002/micr.20743. [DOI] [PubMed] [Google Scholar]
- 2.Yamano Y. Replantation of the amputated distal part of the fingers. J Hand Surg Am. 1985;10(2):211–218. doi: 10.1016/s0363-5023(85)80107-6. [DOI] [PubMed] [Google Scholar]
- 3.Foucher G. Distal replantation. J Hand Surg Am. 1986;11(3):456–457. doi: 10.1016/s0363-5023(86)80171-x. [DOI] [PubMed] [Google Scholar]
- 4.Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128(3):723–737. doi: 10.1097/PRS.0b013e318221dc83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koshima I, Urushibara K, Fukuda N, Ohkochi M, Nagase T, Gonda K, Asato H, Yoshimura K. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg. 2006;118(7):1579–1584. doi: 10.1097/01.prs.0000232987.54881.a7. [DOI] [PubMed] [Google Scholar]
- 6.Scheker LR, Becker GW. Distal finger replantation. J Hand Surg Am. 2011;36(3):521–528. doi: 10.1016/j.jhsa.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Cheng GL, Pan DD, Yang ZX, Qu ZY. Replantation of digits amputated at or about the distal interphalangeal joint. Ann Plast Surg. 1985;15(6):465–473. doi: 10.1097/00000637-198512000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Atasoy E, Ioakimidis E, Kasdan ML, Kutz JE, Kleinert HE. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am. 1970;52(5):921–926. [PubMed] [Google Scholar]
- 9.Chen SY, Wang CH, Fu JP, Chang SC, Chen SG. Composite grafting for traumatic fingertip amputation in adults: technique reinforcement and experience in 31 digits. J Trauma. 2011;70(1):148–153. doi: 10.1097/TA.0b013e3181cc8553. [DOI] [PubMed] [Google Scholar]
- 10.Kutler W. A new method for finger tip amputation. J Am Med Assoc. 1947;133(1):29. doi: 10.1001/jama.1947.62880010007007. [DOI] [PubMed] [Google Scholar]
- 11.Tempest MN. Cross-finger flaps in the treatment of injuries to the finger tip. Plast Reconstr Surg. 1952;9(3):205–222. doi: 10.1097/00006534-195203000-00002. [DOI] [PubMed] [Google Scholar]