Abstract
Objective
The purpose of this study was to evaluate displacement of the mandibular condyle after orthognathic surgery using a condylar-repositioning device.
Methods
The patient group comprised 20 adults who underwent bimaxillary surgery between August 2008 and July 2011. The degree of condylar displacement was measured by pre- and postoperative tomographic analysis using centric relation bite and a wire during surgery. A survey assessing temporomandibular joint (TMJ) sound, pain, and locking was performed. The 20 tomographs and surveys were analyzed using the Wilcoxon signed-rank test and McNemar's test, respectively.
Results
No significant changes were observed in the anterior, superior, or posterior joint space of the TMJ (p > 0.05). In addition, no significant change was observed in TMJ sound (p > 0.05). However, TMJ pain and locking both decreased significantly after surgery (p < 0.05).
Conclusions
Due to its simplicity, this method may be feasible and useful for repositioning condyles.
Keywords: Centric relation, Temporomandibular joint, Orthognathic surgery
INTRODUCTION
Repositioning of the proximal segment during bimaxillary surgery is a critical factor influencing the maintenance of temporomandibular joint (TMJ) function. A postoperative change in the condylar position with respect to the glenoid fossa can have multiple undesirable effects, including internal derangement of the TMJ, loss of mandible angle, increase in relapse, condyle sagging, and loss or reduction in mastication.1,2 Since Leonard3 first attempted to settle the condylar position using a proximal segment-orienting device, various methods and condylar-repositioning devices have been reported; however, the necessity and effects of these devices remain controversial. Previously introduced methods to reposition the proximal segment can be grouped into manual methods,4 rigid retention,3,5-7 sonographic monitoring,8 and navigation.9,10
The first attempt to stabilize the mandible and reduce TMJ dysfunction after surgery was performed by Leonard3, who reproduced the condylar position using a proximal segment-orienting device while performing mandible surgery. Although this method reduced circulation to the proximal segment to some degree, reproduction of the condylar position was limited in all angles. Since then, various condylar-positioning methods have been introduced by many oral surgeons. Luhr11 introduced a condylar-positioning plate method that reproduces the condylar position in 3 dimensions. Helm and Stepke12 performed mandibular surgery using Luhr's condylar-positioning plate, and utilized axiography to confirm that this method was effective in securing proper condylar position and TMJ function. Epker and Wylie1 introduced the condylar-repositioning method, which uses a condyle-proximal segment control device. Heffez et al.13 proposed a simple and effective method using a modified bracket and K-wire device. Subsequently, Raveh et al.,14 Fujimura and Nagura15 introduced a method that could be applied more easily. Harada et al.16 introduced a new condylar-positioning appliance that could be applied to 2-jaw osteotomy. Gateno et al.8 and Landes17 proposed the method of condylar repositioning while monitoring using sonography, while Bettega et al.9,10 introduced a computer-guided condylar-positioning method. Although condylar-positioning methods have been studied and developed in recent decades, there has been controversy over their effects and accuracy. Moreover, most oral surgeons tend to avoid making special efforts in achieving condylar repositioning because of the high cost and time spent on production of an additional condylar-repositioning device prior to surgery, the increase in operating time, the adaptation required of the patient, and other factors.18,19 Boulétreau et al.20 showed that 73% of oral and maxillofacial surgeons in France fixed the bone fragment of the condyle based on their experience in orthognathic surgery.
Temporomandibular disorder (TMD) is a typical complication that can occur due to a change in condylar position after orthognathic surgery. Many studies have been performed on the influence of the condylar position after surgery on TMD. However, little is known about the correlation between condylar-repositioning devices and the occurrence of new TMD; thus, further studies on this topic are required.
Condylar repositioning during bimaxillary surgery, which involves simultaneous surgery of both the mandible and maxilla, is more difficult than that during single-jaw surgery. The ideal condylar position after sagittal split osteotomy remains controversial. The dental occlusion changes during orthodontic treatment and is affected by neuromuscular function, gravity, level of consciousness, and postural habits. The aim of this study was to evaluate pre- and postoperative condylar positions among patients treated with bimaxillary surgery using centric relation (CR) bite and a simple device.
MATERIALS AND METHODS
Materials
Patients diagnosed with skeletal Class III malocclusion and receiving a LeFort I osteotomy and bilateral sagittal split ramus osteotomy (BSSO) from August 2008 to June 2011 at Department of Oral and Maxillofacial Surgery, Hallym University Sacred Heart Hospital (Anyang, Korea) were recruited for this study. All the surgeries were performed by the same surgeon. The patients comprised 20 adults (5 men, 15 women) with a mean age of 25.2 years (range, 18 - 51 years). Six patients had TMD. The average amount of mandible set-back was 7.5 mm (range, 4 - 12.5 mm), and fixation of the proximal and distal segments was performed using 1 miniplate and 4 miniscrews on each side.
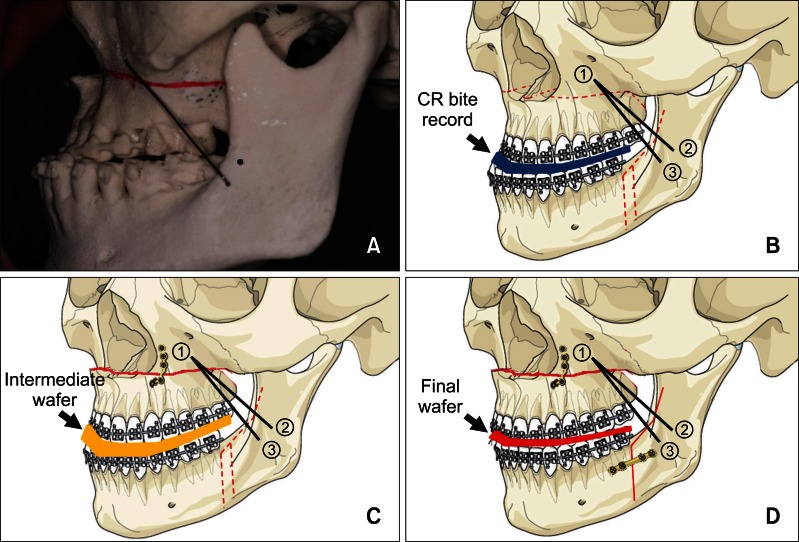
The CR bite records were obtained with each patient in an upright, conscious posture using Dawson's bilateral manipulation method 1 day prior to surgery. Using an rapid prorototype (RP) model previously created using 3-dimensional computed tomography, a set of 3 reference points was generated. One (point ①) was placed on the upper part of the estimated osteotomy line of the maxilla, and another (point ②) was placed on the lateral cortical surface of the proximal segment of the mandible. The wire was bent approximately to fit points ① and ②. The third reference point (point ③) was set using the same wire on the proximal segment, approximately 1 cm from point ②. The distances between ① and ② and between ① and ③ were equal, and the same wire was used. Two different wires for the right and left sides were prepared (Figure 1).
Figure 1.
A, A condylar-repositioning wire produced prior to surgery using a rapid prototype model. B, The setting of 1 point at the upper part of the estimated osteotomy line of the maxilla (①) and 2 points at the lateral margin of the ramus (②, ③) as reference points using a wire bent prior to surgery after placing a centric relation bite record in the mouth. C, D, Maxilla and mandible fixation after placement of the intermediate wafer and final wafer and performing condylar reposition using the reference points and wires.
In the operating room, the osteotomy was prepared using conventional methods. Prior to the bone split, CR bite records was placed in the mouth, and the 3 reference points were recreated using small round burrs on the lateral cortical surface of the proximal segment and the maxilla using the previously prepared wires. Two reference points on the mandible were set approximately 1 cm apart using the same wire. Fixation of the maxilla was completed, bilateral sagittal split osteotomy and intermaxillary fixation were performed, and the proximal segment was repositioned bimanually. The position of the proximal segment was checked together with the wires on each side and fixed using a titanium miniplate and screws (Figure 2).
Figure 2.
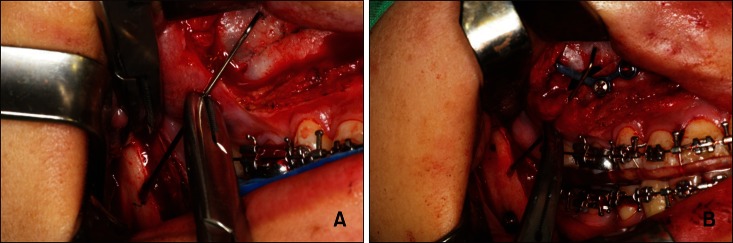
A, The reference points were marked using a wire after placing a centric relation bite device prior to the sagittal split osteotomy. B, The position of the condyle was reconfirmed following fixation.
Methods
TMJ tomographs were obtained after placing the previously collected CR bite record in the mouth 1 day prior to surgery. A similar tomograph was obtained in the closed condition with the final wafer 2 days after surgery. Each tomograph was examined by the same staff, and the change in TMJ space after surgery was verified by measuring the superior, anterior, and posterior joint spaces before and after surgery. To evaluate changes in patient symptoms with respect to the TMJ, a clinical review and survey also were performed 1 week prior to and 1 month after surgery.
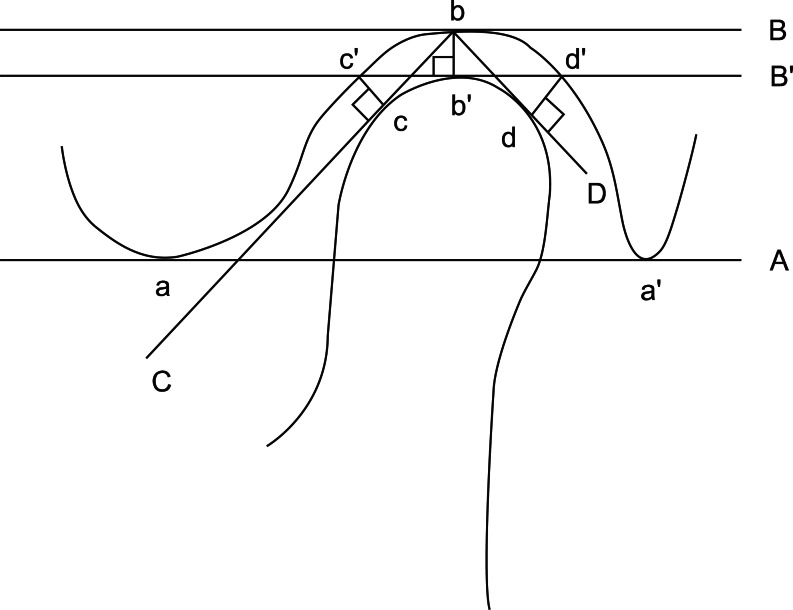
TMJ tomography
TMJ tomography was performed using ORTHOSTAGE Auto IIIN CMT (Asahi Roentgen Ind. Co. Ltd., Kyoto, Japan ). The TMJ space was measured using the method described by Athanasiou and Mavreas (Table 1, Figure 3).21 The superior joint space (SJS, b-b'), anterior joint space (AJS, c-c'), and posterior joint space (PJS, d-d') were used in this investigation.21
Table 1.
Reference landmarks and planes used in this study
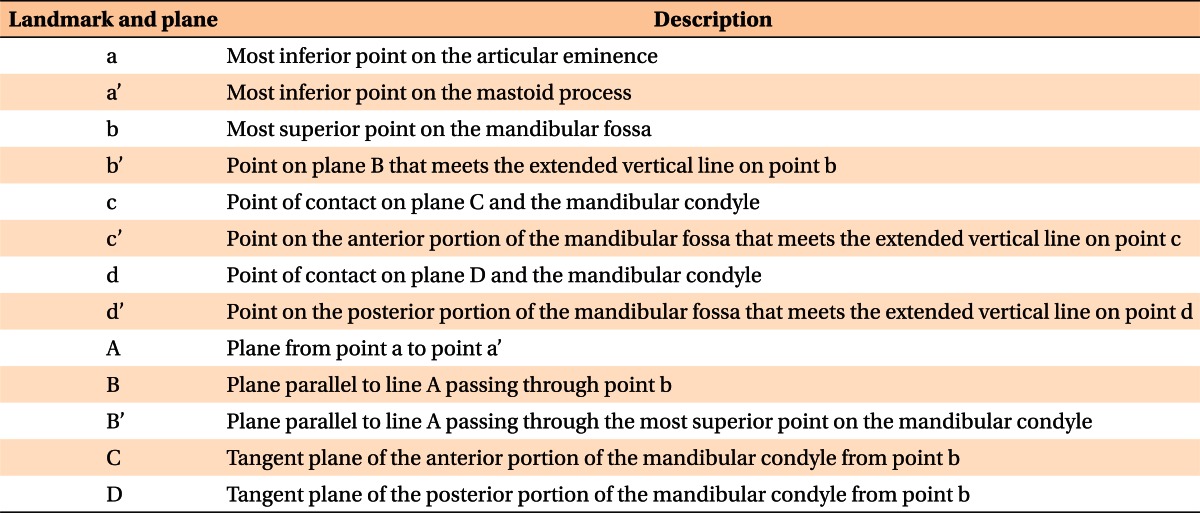
Figure 3.
Schematic representation of the reference point and reference segment. See Table 1 for the abbreviations.
TMJ symptoms
TMJ symptoms were divided into broad groups of pain, joint sound, and locking. The patients were asked to describe their pain using a point system: 0, no symptoms; 1, intermittent manifestations; 2, frequent manifestations; and 3, very frequent manifestations that impeded daily life. For sound and locking, subjects were asked whether sound and locking existed.
Statistical analyses
Statistical analyses were performed using SPSS 12.0 for Windows (SPSS Inc, Chicago, IL, USA). The means and standard deviations were calculated for each variable. Tests of normality were performed, and the Wilcoxon signed-rank test was used to assess the statistical significance of joint space differences. A level of p < 0.05 was considered significant. The presence of systematic errors and their magnitude were examined using Dahlberg's formula. All tracings and measurements were performed manually twice with a 2-week interval by 1 examiner under optimal conditions. The method error was calculated as 0.33 mm for SJS, 0.40 mm for AJS, and 0.47 mm for PJS, all of which were statistically insignificant (p ≥ 0.05).
(d, difference between the means of the first and second tracings; n, number of duplicate registrations)
RESULTS
A Shapiro-Wilk test of normality was performed for all variables. The results were 0.013 for SJS, 0.00 for AJS, and 0.00 for PJS. The results of Wilcoxon signed-rank tests are shown in Table 2.
Table 2.
Distance of joint spaces measured using TMJ tomographs (N = 20)
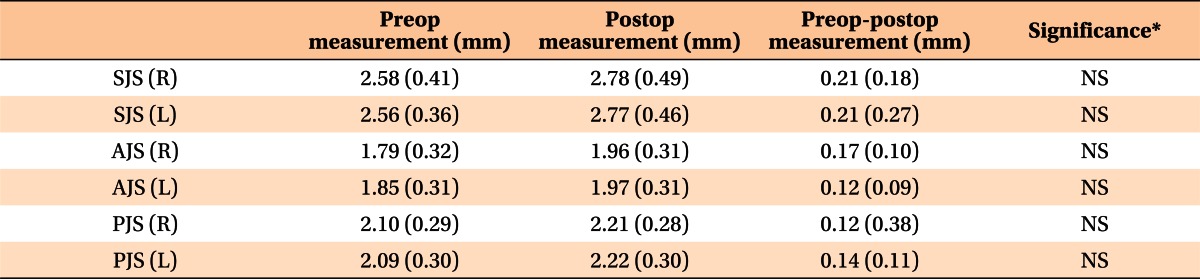
Values are presented as mean (standard deviation).
*Wilcoxon signed-rank test was used to compare preoperative (preop) and postoperative (postop) data.
TMJ, Temporomandibular joint; SJS, superior joint space; AJS, anterior joint space; PJS, posterior joint space; L, left; R, right; NS, not significant.
Superior joint space
No significant change in the SJS was identified after surgery (p ≥ 0.05). The left and right sides of the SJS increased by an average of 0.21 mm. Of the 20 cases, only 1 displayed a change greater than 0.5 mm on the right and left sides.
Anterior joint space
No significant change in the AJS was identified after surgery (p ≥ 0.05). The AJS increased by an average of 0.17 mm on the right side and 0.12 mm on the left side. No case showed a change greater than 0.5 mm.
Posterior joint space
No significant change in the PJS was identified after surgery (p ≥ 0.05). The right side increased by an average of 0.12 mm, while the left side increased by an average of 0.14 mm. Of the 20 cases, only 3 on the right side and 1 on the left side had a change greater than 0.5 mm.
TMJ symptoms (Table 3)
Table 3.
Questionnaire findings
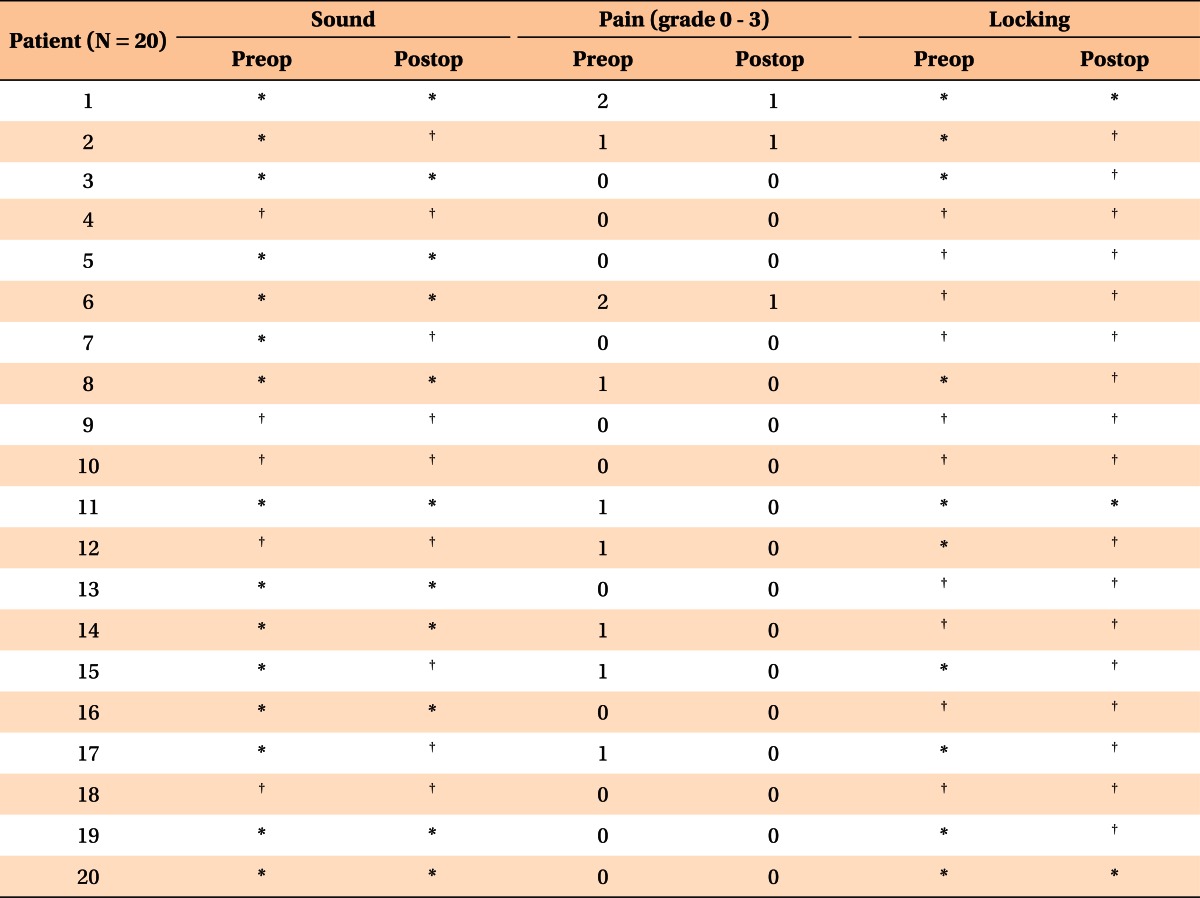
*Symptom exists; †symptom nonexistent.
Preop, Preoperative; postop, postoperative.
Fifteen patients (75%) demonstrated TMJ sound prior to surgery, and 11 (55%) reported TMJ sound following surgery. Results of McNemar's test showed that this reduction was not significant (p ≥ 0.05). Nine patients (30%) had presurgery TMJ pain, and 3 (15%) had TMJ pain postsurgery, which was a significant reduction (p < 0.05). Ten patients (50%) had presurgery TMJ locking, and 3 (15%) had TMJ locking postsurgery, which was a significant decrease (p < 0.05).
DISCUSSION
Changes in condylar position are influenced by posture, muscle tone, gravity, the investigating operator, fixation method, and wafers. Muscle tone is important for maintaining TMJ contact. Boucher and Jacoby22 described how anesthetized and paralyzed patients had a condylar position 2 mm posterior, compared with that in the same patients when conscious with the same seating force applied. Zak et al.23 affirmed that general anesthesia itself appears to be sufficient for changing condylar position. In 6 of 10 patients, condylar position changed between anesthetized and awake status. Other studies have reported that the mandible moves up to 2 mm posteriorly, and that a vertical drop of the condyles occurs when under general anesthesia.22,24,25 Politi et al.26 introduced an intraoperative wakening method to prevent this condylar sag. During bimaxillary orthognathic surgery, the mandibular proximal segment is positioned manually, and immediately after fixation, occlusion is checked using light digital pressure on the chin. The patients then are awakened rapidly to a state of conscious analgosedation, and asked to open, close, and laterally move their mandible. The percentage of condylar sags diagnosed and corrected during intraoperative wakening in the experimental group was similar to that after the operation in the control group.26
The change in condylar position after surgery has great influence on the occurrence and recurrence of complications. Epker and Wylie1 discussed 3 reasons why accurate surgery of the mandible proximal segment is necessary, which include stabilizing surgical outcome, reducing negative influence on the TMJ, and increasing mastication efficiency.
The reproducibility and effectiveness of CR and centric occlusion (CO, maximum intercuspation) for the reproduction of condylar position remains controversial. Large CO and CR discrepancies have been shown in patients with jaw abnormalities who also have either malocclusion or TMD.27,28 One study reported that anteroposterior and superoinferior CO-CR discrepancies were greatest in Class II Division 1 cases, with a maximum of 4.3 mm. These discrepancies may be due to compensatory postures to mask aesthetic anomalies and overcome masticatory or speech difficulties. Thus, the author recommended obtaining a CR bite record while in the supine position during the planning of all orthognathic surgeries.29 The purpose of orthognathic surgery can be considered to be the alignment of CO, which can be changed due to teeth, and CR, which is associated with the skeletal relationship.
In this study, we obtained a CR bite record prior to surgery, which was used as a condylar-repositioning guide for the reasons mentioned above. Typically, preoperative planning for orthognathic surgery is performed for CO while the patient is in the upright conscious position, despite the surgery taking place with the patient in an anesthetized supine CR position. This CR bite record allows for reproduction of the condylar position with the patient in the upright position and awake. It is assumed for the surgery and model surgery procedures that the conscious vertical CR and CO will coincide with the anesthetized supine CR and CO. We used the final wafer as the CO bite record.
The CR of the patient was introduced on the basis of the definition proposed by Dawson,30 Gilboe,31 and Carlson et al.,32 i.e., "the most anterior and superior position of the condyles at the mandibular fossa, with the articular disk interposed between them".30-32 Dawson's30 bilateral manipulation method has the advantage of being relatively easy to reproduce.33
There has been controversy regarding whether the change in condylar position after BSSO causes or aggravates internal derangement of the TMJ. Most clinicians believe that improperly positioned condyles can cause muscle pain, joint pain, internal derangement of the TMJ, and arthrosis. Many reports have been published on the relationship between TMJ dysfunction and orthognathic surgery. Panula et al.34 reported that signs and symptoms of TMJ dysfunction were observed in 73.3% of patients prior to surgery, which reduced to 60% after surgery. Furthermore, the incidence of headache reduced from 63% before surgery to 25%.34 Westermark et al.35 reported that the incidence of TMJ symptoms reduced from 43% before surgery to 28% after surgery. De Clercq et al.36 reported that 40% of patients displayed improvements in TMJ function and that 11% of patients displayed aggravation after surgery. In contrast, Wolford et al.37 reported that TMJ dysfunction after surgery, especially in the case of mandible advancement, was aggravated in patients with TMJ dysfunction. Although most authors suggest that the signs and symptoms of TMD can be aggravated by changes in condylar position after BSSO, there are few reports that examine the type of change in the TMJ using a condylar-positioning device (CPD).38 Thus, the use of CPDs has not been considered crucial for skeletal stability, or perhaps clinicians who have studied skeletal stability have not routinely used CPDs. In this study, condylar repositioning was performed using a CR bite record collected prior to surgery, and the position changes were correlated with TMJ symptoms. In 15 of 20 cases, various TMJ symptoms were displayed before surgery, but TMJ pain and locking were significantly reduced following surgery. There was no case in which the symptoms became severe. There was no significant change in TMJ sound, but the number of patients with TMJ sound decreased after surgery. These results demonstrate that the use of a CPD did not appear to aggravate TMJ symptoms.
Is a CPD necessary in orthognathic surgery? A CPD is a valuable tool in the transition from nonrigid to rigid fixation, but these devices are cumbersome, and there is no scientific evidence to support their routine use in orthognathic surgery. Gerressen et al.39 and Costa et al.38 reported that a manual positioning technique enabled equally stable results in orthognathic surgery. They suggested that manual repositioning of the proximal segment continues to be the method of choice because it is easier and less expensive for intraoperatively identifying a malpositioned condyle. Previously published articles have advocated the use of CPDs or intraoperative imaging records only in cases of presurgical TMJ dysfunction or insufficient surgical experience. However, there has been a significant increase in posterior displacement of CR from the conscious upright to the anesthetized supine position, the device is more precise than a surgeon's hand, and the possibility of mistakes remains even for expert surgeons.9,29 Mani pulation of the condylar segments requires significant manual manipulation. CPDs are required to develop accuracy in condylar positioning. If there is a simple, inexpensive device available, the use of a CPD is recommended for all surgeons.
The condylar-repositioning method used in this study has several advantages. First, the preparation is simple; taking a CR bite record and bending the wire on the RP model prior to surgery is all that is required. Second, the procedure requires only 2 - 3 minutes; thus it would not have a large influence on operating time. Only one case displayed a change of 1.1 mm in the left SJS; however, relapse was not observed, and TMJ symptoms remained unchanged.
This procedure also has some restrictions. There is a limitation in reproducing the position of the proximal segment in 3 dimensions. There is also a possibility that the wax used to collect the CR bite record prior to surgery and for the final wafer may change. Errors due to such changes may be minimized by thoroughly and accurately understanding and preparing the wax and resin, and by using the wax in accordance with its physical properties. We used 3 reference points to define 1 plane in a 3-dimensional space. The 3 points and length of the wire located a proximal segment in the same position on the sagittal plane. However, the condylar position may be changed transversely. Béziat et al.40 reported in 2009 that changes in the anteroposterior direction were found following bilateral sagittal split osteotomy in 74% of cases, with an average magnitude of 0.32 mm, whereas changes in the transverse dimension were less frequent (54% of cases), with a magnitude of less than 0.19 mm. The changes in the anteroposterior direction were greater than those in the transverse dimension; therefore, measurements for the anteroposterior dimension are sufficient for evaluation.
Mandible malposition of 1 mm or less after surgery is not typically associated with clinical problems.41 Most surgeons intuitively recognize that these occlusal discrepancies fall within the limits of the TMJ dynamic envelope of adaptation, and are accommodated without any surgical intervention. Any discrepancy in condylar position is capable of self-correction over time by a creeping adjustment within the fossa in response to the isometric pterygomasseteric muscle tone of swallowing and talking.29 Medial or lateral compression can cause TMJ remodeling and resorption, which can lead to late relapse. This relapse occurs when the clamping or bicortical screws close the gap between the segments. To avoid condylar torqueing, the plate should be bent to passively contact the mandible. When the screws are tightened, the plate should not change the mediolateral or anteroposterior condylar position. For these reasons, we chose a miniplate and placed it passively, maintaining the condyle in its properly seated position.
Our method is not designed to achieve accurate 3-dimensional positioning of the condyle, but it is a simple and useful aid for sagittal positioning of the condyle.
CONCLUSION
The following results were acquired from 20 patients who underwent surgery to reposition the condyles using CR bite records, which were collected 1 day prior to surgery, including osteotomy and setting of the distal segments under CO during bimaxillary surgery. The results comprised the change in condylar position, which was measured with TMJ tomography, and symptoms of the TMJ, which were analyzed from clinical reviews and surveys. First, TMJ tomography showed no significant change in condylar position after surgery, and condylar position showed considerable reproducibility between pre- and postoperative images. Second, the clinical review and survey showed that there was a significant reduction in TMJ pain and locking in these cases. The method used in this study may be simple and effective for repositioning the condyle without additional devices or an increase in operating time. However, the procedure allows limited evaluation in 3 dimensions, and additional computed tomography studies are required. Moreover, a long-term follow-up of TMJ symptoms is required.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Epker BN, Wylie GA. Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible. Oral Surg Oral Med Oral Pathol. 1986;62:613–617. doi: 10.1016/0030-4220(86)90251-3. [DOI] [PubMed] [Google Scholar]
- 2.Timmis DP, Aragon SB, Van Sickels JE. Masticatory dysfunction with rigid and nonrigid osteosynthesis of sagittal split osteotomies. Oral Surg Oral Med Oral Pathol. 1986;62:119–123. doi: 10.1016/0030-4220(86)90027-7. [DOI] [PubMed] [Google Scholar]
- 3.Leonard M. Preventing rotation of the proximal fragment in the sagittal ramus split operation. J Oral Surg. 1976;34:942. [PubMed] [Google Scholar]
- 4.Bell WH, Proffit WR, White RP. Surgical correction of dentofacial deformities. Philadelphia: Saunders; 1980. [Google Scholar]
- 5.Luhr HG, Kubein-Meesenburg D. Rigid skeletal fixation in maxillary osteotomies. Intraoperative control of condylar position. Clin Plast Surg. 1989;16:157–163. [PubMed] [Google Scholar]
- 6.Luhr HG. The significance of condylar position using rigid fixation in orthognathic surgery. Clin Plast Surg. 1989;16:147–156. [PubMed] [Google Scholar]
- 7.Hiatt WR, Schelkun PM, Moore DL. Condylar positioning in orthognathic surgery. J Oral Maxillofac Surg. 1988;46:1110–1112. doi: 10.1016/0278-2391(88)90461-2. [DOI] [PubMed] [Google Scholar]
- 8.Gateno J, Miloro M, Hendler BH, Horrow M. The use of ultrasound to determine the position of the mandibular condyle. J Oral Maxillofac Surg. 1993;51:1081–1086. doi: 10.1016/s0278-2391(10)80444-6. [DOI] [PubMed] [Google Scholar]
- 9.Bettega G, Cinquin P, Lebeau J, Raphaël B. Computer-assisted orthognathic surgery: clinical evaluation of a mandibular condyle repositioning system. J Oral Maxillofac Surg. 2002;60:27–34. doi: 10.1053/joms.2002.29069. [DOI] [PubMed] [Google Scholar]
- 10.Bettega G, Dessenne V, Raphaël B, Cinquin P. Computer-assisted mandibular condyle positioning in orthognathic surgery. J Oral Maxillofac Surg. 1996;54:553–558. doi: 10.1016/s0278-2391(96)90630-8. [DOI] [PubMed] [Google Scholar]
- 11.Luhr HG. Skelettverlagernde Operationen zur Harmonisierung des Gesichtsprofiles. In: Pfeifer G, editor. Die Ästhetik von Form und Funktion in der Plastischen und Wiederherstellungschirurgie. Stuttgart: Springer; 1985. [Google Scholar]
- 12.Helm G, Stepke MT. Maintenance of the preoperative condyle position in orthognathic surgery. J Craniomaxillofac Surg. 1997;25:34–38. doi: 10.1016/s1010-5182(97)80022-4. [DOI] [PubMed] [Google Scholar]
- 13.Heffez L, Marsik J, Bressman J. A simple means of maintaining the condyle-fossa relationship. J Oral Maxillofac Surg. 1987;45:288–290. doi: 10.1016/0278-2391(87)90134-0. [DOI] [PubMed] [Google Scholar]
- 14.Raveh J, Vuillemin T, Lädrach K, Sutter F. New techniques for reproduction of the condyle relation and reduction of complications after sagittal ramus split osteotomy of the mandible. J Oral Maxillofac Surg. 1988;46:751–757. doi: 10.1016/0278-2391(88)90185-1. [DOI] [PubMed] [Google Scholar]
- 15.Fujimura N, Nagura H. New appliance for repositioning the proximal segment during rigid fixation of the sagittal split ramus osteotomy. J Oral Maxillofac Surg. 1991;49:1026–1027. doi: 10.1016/0278-2391(91)90072-t. [DOI] [PubMed] [Google Scholar]
- 16.Harada K, Okada Y, Nagura H, Enomoto S. A new repositioning system for the proximal segment in sagittal split ramus osteotomy of the mandible. Int J Oral Maxillofac Surg. 1994;23:71–73. doi: 10.1016/s0901-5027(05)80594-6. [DOI] [PubMed] [Google Scholar]
- 17.Landes CA. Proximal segment positioning in bilateral sagittal split osteotomy: intraoperative dynamic positioning and monitoring by sonography. J Oral Maxillofac Surg. 2004;62:22–28. doi: 10.1016/j.joms.2003.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Will LA, Joondeph DR, Hohl TH, West RA. Condylar position following mandibular advancement: its relationship to relapse. J Oral Maxillofac Surg. 1984;42:578–588. doi: 10.1016/0278-2391(84)90088-0. [DOI] [PubMed] [Google Scholar]
- 19.Jäger A, Kubein-Meesenburg D, Luhr HG. Longitudinal study of combined orthodontic and surgical treatment of Class II malocclusion with deep overbite. Int J Adult Orthodon Orthognath Surg. 1991;6:29–38. [PubMed] [Google Scholar]
- 20.Boulétreau P, Bettega G, Breton P, Freidel M. Results of an evaluation of clinical practice in orthognathic surgery in France in 2002. Rev Stomatol Chir Maxillofac. 2003;104:326–329. [PubMed] [Google Scholar]
- 21.Athanasiou AE, Mavreas D. Tomographic assessment of alterations of the temporomandibular joint after surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1991;6:105–112. [PubMed] [Google Scholar]
- 22.Boucher L, Jacoby J. Posterior border movements of the human mandible. J Prosthet Dent. 1961;11:836–841. [Google Scholar]
- 23.Zak MJ, Dolan EA, Angelillo JC, McGraw TA. No effect of neuromuscular blockade on the temporomandibular joint position during general anesthesia. Anesth Prog. 1992;39:212–214. [PMC free article] [PubMed] [Google Scholar]
- 24.Helkimo M, Ingervall B, Carlsson GE. Variation of retruded and muscular position of mandible under different recording conditions. Acta Odontol Scand. 1971;29:423–437. doi: 10.3109/00016357109026530. [DOI] [PubMed] [Google Scholar]
- 25.McMillen LB. Border movements of the human mandible. J Prosthet Dent. 1972;27:524–532. doi: 10.1016/0022-3913(72)90265-x. [DOI] [PubMed] [Google Scholar]
- 26.Politi M, Toro C, Costa F, Polini F, Robiony M. Intra operative awakening of the patient during orthognathic surgery: a method to prevent the condylar sag. J Oral Maxillofac Surg. 2007;65:109–114. doi: 10.1016/j.joms.2005.10.064. [DOI] [PubMed] [Google Scholar]
- 27.Deng X, Wan Z, He SS, Wamalwa P, Chen S, Zhang ZY. The centric relation-maximum intercuspation discrepancy in adult angle's class II pretreatment patients. Hua Xi Kou Qiang Yi Xue Za Zhi. 2011;29:48–52. [PubMed] [Google Scholar]
- 28.Afzal A, Shameem A. Comparison of condylar positions in centric relation and centric occlusion in pre-treatment malocclusion cases. J Coll Physicians Surg Pak. 2005;15:620–623. [PubMed] [Google Scholar]
- 29.Bamber MA, Abang Z, Ng WF, Harris M, Linney A. The effect of posture and anesthesia on the occlusal relationship in orthognathic surgery. J Oral Maxillofac Surg. 1999;57:1164–1172. doi: 10.1016/s0278-2391(99)90476-7. [DOI] [PubMed] [Google Scholar]
- 30.Dawson PE. Temporomandibular joint pain-dysfunction problems can be solved. J Prosthet Dent. 1973;29:100–112. doi: 10.1016/0022-3913(73)90148-0. [DOI] [PubMed] [Google Scholar]
- 31.Gilboe DB. Centric relation: functional anatomy. J Can Dent Assoc. 1983;49:345–348. [PubMed] [Google Scholar]
- 32.Carlson CR, Okeson JP, Falace DA, Nitz AJ, Curran SL, Anderson D. Comparison of psychologic and physiologic functioning between patients with masticatory muscle pain and matched controls. J Orofac Pain. 1993;7:15–22. [PubMed] [Google Scholar]
- 33.McCollum BB. The mandibular hinge axis and a method of locating it. J Prosthet Dent. 1960;10:428–435. [Google Scholar]
- 34.Panula K, Somppi M, Finne K, Oikarinen K. Effects of orthognathic surgery on temporomandibular joint dysfunction. A controlled prospective 4-year follow-up study. Int J Oral Maxillofac Surg. 2000;29:183–187. [PubMed] [Google Scholar]
- 35.Westermark A, Shayeghi F, Thor A. Temporomandibular dysfunction in 1,516 patients before and after orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 2001;16:145–151. [PubMed] [Google Scholar]
- 36.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JS. Orthognathic surgery: patients' subjective findings with focus on the temporomandibular joint. J Craniomaxillofac Surg. 1998;26:29–34. doi: 10.1016/s1010-5182(98)80032-2. [DOI] [PubMed] [Google Scholar]
- 37.Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg. 2003;61:655–660. doi: 10.1053/joms.2003.50131. [DOI] [PubMed] [Google Scholar]
- 38.Costa F, Robiony M, Toro C, Sembronio S, Polini F, Politi M. Condylar positioning devices for orthognathic surgery: a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:179–190. doi: 10.1016/j.tripleo.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 39.Gerressen M, Stockbrink G, Smeets R, Riediger D, Ghassemi A. Skeletal stability following bilateral sagittal split osteotomy (BSSO) with and without condylar positioning device. J Oral Maxillofac Surg. 2007;65:1297–1302. doi: 10.1016/j.joms.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 40.Béziat JL, Babic B, Ferreira S, Gleizal A. Justification for the mandibular-maxillary order in bimaxillary osteotomy. Rev Stomatol Chir Maxillofac. 2009;110:323–326. doi: 10.1016/j.stomax.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 41.Perez D, Ellis E., 3rd Sequencing bimaxillary surgery: mandible first. J Oral Maxillofac Surg. 2011;69:2217–2224. doi: 10.1016/j.joms.2010.10.053. [DOI] [PubMed] [Google Scholar]