Abstract
INTRODUCTION
Intra-thoracic herniation of abdominal organs following diaphragmatic rupture represents an unusual clinical occurrence that poses great diagnostic difficulty.
PRESENTATION OF CASE
We report a rare case of delayed total hepatothorax caused by a right sided post-traumatic diaphragmatic rupture in a 67 year old male. Reduction of the liver in the abdominal cavity and repair of the diaphragm was feasible via a thoraco-abdominal approach. Postoperative chest radiography showed normal position of the right diaphragmatic border.
DISCUSSION
Characteristics of right diaphragmatic rupture and subsequent complications are reviewed with the aim to reinforce physicians’ awareness of this uncommon clinical condition in order to establish a timely diagnosis and reduce the mortality related burden.
CONCLUSION
Surgeons should consider this entity in the differential diagnosis of injured patients experiencing sudden respiratory distress during hospitalization as well as days or months after discharge.
Keywords: Diaphragmatic rupture, Hepatothorax, Diagnosis, Management
1. Introduction
Diaphragmatic injuries are unusual, life-threatening1 clinical conditions occurring after an abrupt increase of intra-abdominal pressure.2 More specifically they have been reported in 1–7% of the patients with a major blunt trauma, and 10–15% of the patients suffering from a penetrating trauma.3,4 Left sided diaphragmatic ruptures occur more frequently, with a reported ratio of 25 to 1.5 This preponderance is attributed to the buffering effect of the liver against external forces in the right hemidiaphragm.2
Intrathoracic herniation of abdominal organs following diaphragmatic injury is rare6 and difficult to recognize.3,6 Remarkably occurs in only 2 out of 10 cases of right diaphragmatic rupture.6 Stomach, spleen and colon are organs more frequently herniated.3 We present a case of a 67 year old male with delayed intra-thoracic herniation of the entire liver due to a right diaphragmatic rupture following an isolated blunt thoracic trauma.
2. Case presentation
A 67 year old Caucasian male presented to our department due to a blunt thoracic trauma after a fall from a height of 2 m. The patient complained of right chest pain that had been worsened by deep inspiration. On admission he was haemodynamically stable. His vital signs were as follows: heart rate, 103 beats/min blood pressure, 130/90 mmHg; oxygen saturation, 98% while breathing ambient air; temperature, 36.9 °C. Physical examination disclosed a slight decrease of breath sounds during pulmonary auscultation upon the right hemithorax. Initial laboratory work up including full blood count, renal and liver function tests did not reveal any abnormal finding.
A chest X-ray on admission showed rib fractures, a small right-sided hemo-pneumothorax and moderate elevation of the right hemithorax which was not considered significant (Fig. 1). Computed tomography (CT) thoracic scan confirmed previous findings. Abdominal ultrasound was normal. An intra-thoracic chest tube was consequently introduced and hemo-pneumothorax was successfully drained.
Fig. 1.

Antero-posterior erect chest X ray on admission showing rib fractures and a small right-sided pleural effusion.
However, on the fifth hospital day the patient presented a progressive deterioration of his respiratory status manifested with dyspnoea along with a significant decrease of oxygen saturation at 89% while he was breathing ambient air. His vital signs were as follows: blood pressure, 160/90 mmHg; pulse, 113 beats/min; respiratory rate, 19 breaths/min. A repeated chest X-ray showed an increased elevation of the right hemidiaphragm compared to the chest radiography on admission (Fig. 2). A CT thoracic scan was consequently performed, showing total displacement of the liver into the right hemithorax (Fig. 3). The patient was transferred to the operation room and underwent an exploratory midline laparotomy with the character of emergency. Intraoperatively was detected a right sided diaphragmatic rupture and intra-thoracic herniation of the entire liver (Fig. 4). Mobilization of the liver and relocation into the abdominal cavity was feasible only after a right thoraco-abdominal incision (Fig. 5). Suture of the diaphragm was finally performed and chest drain was placed in the right hemithorax. After surgical reduction of the liver in the abdominal cavity and repair of the diaphragmatic rupture a repeated chest X-ray disclosed normal positioning of the right diaphragmatic border. Postoperatively, the patient's clinical course was uneventful and was discharged home on the 10th postoperative day without any complication. During a 12 month follow up the patient remained asymptomatic.
Fig. 2.
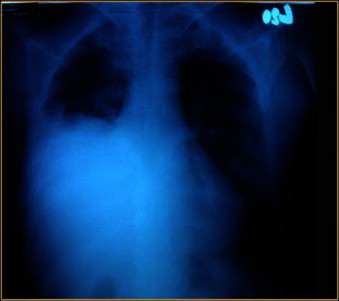
Repeated chest X-ray 5 days after initial presentation showing an increased elevation of the right hemidiaphragm compared with the image on admission (e.g. Fig. 1).
Fig. 3.

Axial section of thoracic computed tomography demonstrating displacement of the entire liver into the thoracic cavity.
Fig. 4.
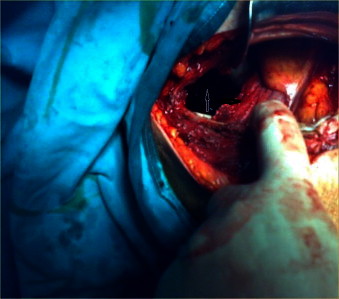
Intra-operative image of exploratory laparotomy confirming total hepatic diaphragmatic herniation with visualization of the lower surface of the liver (white arrow) through a right sided diaphragmatic defect (black arrow).
Fig. 5.
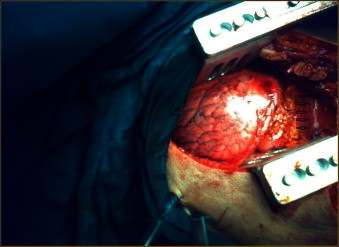
Intra-operative image of the right thoracic cavity with visualization of the upper hepatic surface (arrows).
3. Discussion
Right sided diaphragmatic ruptures are rare conditions presenting with non specific clinical and radiological findings making prompt diagnosis challenging.3 Interestingly, they are often not detected early leading to severe complications3 associated with high mortality rates.5 Various hypotheses have been formulated for the delayed presentation of a diaphragmatic rupture.1 One of them suggests the occurrence of a devitalization process of the diaphragmatic muscle which may last for several hours or days after the initial trauma.1,7 The most plausible explanation is that diaphragmatic injuries are manifested clinically only after intra-thoracic herniation of abdominal viscera.4
Diaphragmatic rupture complicated by intra-thoracic herniation of an abdominal organ was first described by Sennertus in 1541, when he performed an autopsy to a patient deceased from herniation of a strangulated colon through a diaphragmatic defect caused by a gunshot wood before seven months.1,7 Clinical characteristics of the patients with diaphragmatic rupture are silent and non specific.1 In the acute phase patients are usually admitted to the emergency setting with co-existing injuries that may obscure the diagnosis.2 Thoracic pain, cough, tahypnea and dyspnoea are the most commonly reported symptoms.1,8 Hepatothorax represents a rare and severe complication of right diaphragmatic rupture.9 Remarkably, a systematic literature review performed by Rashid et al., disclosed a total number of 13 right sided diaphragmatic ruptures reported in the medical literature.1 Hepatothorax and more specifically herniation of the right hepatic lobe occurred in only 6 out of 13 cases reported.1 Herniation of the liver in the thoracic cavity may compromise pulmonary and cardiovascular functions by causing severe atelectasis of the right lung and tension of the mediastinum.3
Chest radiography represents the basic investigation for the diagnosis although it presents low sensitivity and specificity.3 Its preoperative diagnostic value is limited in the presence of haemothorax or a right sided diaphragmatic defect.9 Computed tomography abdominal and thoracic scans remain highly specific tools10 for the establishment of a preoperative diagnosis in the acute care setting.3 For this reason, when a right diaphragmatic rupture is suspected, abdominal CT should be directly performed.3 Surgical repair of hepatothorax should be urgent and consists of liver reduction and repair of the diaphragmatic defect through a trans-thoracic or trans-abdominal approach.3 The use of interrupted or continuous non-absorbable suturing along with the intra-thoracic placement of chest tubes represents the classical strategy.3
4. Conclusions
Here we presented a case of delayed right diaphragmatic rupture complicated by a severe total hepatothorax. Asymptomatic clinical picture during hospitalization delayed diagnosis.
Preoperative detection of a diaphragmatic rupture is crucial for prevention of life-threatening complications such as hepatothorax. For this reason physicians have to cultivate a ‘detective judgment’ for rare conditions11 and maintain a high level of clinical suspicion when they encounter patients with sudden onset of respiratory distress or upper abdominal symptoms days, months or years after a minor blunt thoracic or abdominal trauma.
Conflict of interest
The authors declare that they have no competing interests.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this manuscript and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of this journal.
Author contributions
Miltiades Kastanakis, Ioannis Kokinos and Emmanouil Bobolakis performed the operation. Dimitrios Anyfantakis and Miltiades Kastanakis prepared the first draft of the manuscript. George Petrakis was involved with the revision of the manuscript. All authors have read and approved the final manuscript.
References
- 1.Rashid F., Chakrabarty M.M., Singh R., Iftikhar S.Y. A review on delayed presentation of diaphragmatic rupture. World Journal of Emergency Surgery. 2009;4:32. doi: 10.1186/1749-7922-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Disler D.G., Deluca S.A. Traumatic rupture of the diaphragm and herniation of the liver. American Family Physician. 1992;46:453–456. [PubMed] [Google Scholar]
- 3.Baek S.J., Kim J., Lee S.H. Hepatothorax due to a right diaphragmatic rupture related to duodenal ulcer perforation. World Journal of Gastroenterology. 2012;18:5649–5652. doi: 10.3748/wjg.v18.i39.5649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyers B.F., McCabe C.J. Traumatic diaphragmatic hernia. Occult marker of serious injury. Annals of Surgery. 1993;218:783–790. doi: 10.1097/00000658-199312000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vilallonga R., Pastor V., Alvarez L., Charco R., Armengol M., Navarro S. Right-sided diaphragmatic rupture after blunt trauma. An unusual entity. World Journal of Emergency Surgery. 2011;6:3. doi: 10.1186/1749-7922-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kozak O., Mentes O., Harlak A., Yigit T., Kilbas Z., Aslan I. Late presentation of blunt right diaphragmatic rupture (hepatic hernia) American Journal of Emergency Medicine. 2008;26:638. doi: 10.1016/j.ajem.2007.10.032. e3-5. [DOI] [PubMed] [Google Scholar]
- 7.Goh B.K., Wong A.S., Tay K.H., Hoe M.N. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. Journal of the Canadian Association of Emergency Physicians. 2004;6:277–280. doi: 10.1017/s148180350000926x. [DOI] [PubMed] [Google Scholar]
- 8.Shreck G.L., Toalson T.W. Delayed presentation of traumatic rupture of the diaphragm. Journal of the Oklahoma State Medical Association. 2003;96:181–183. [PubMed] [Google Scholar]
- 9.Porcelli M., Prychyna O., Rosenthal A., Decostanza J. Hepatothorax: a rare outcome of high-speed trauma. Case Reports in Emergency Medicine. 2011;2011:905641. doi: 10.1155/2011/905641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Killeen K.L., Shanmuganathan K., Mirvis S.E. Imaging of traumatic diaphragmatic injuries. Seminars in Ultrasound, CT and MR. 2002;23:184–192. doi: 10.1016/s0887-2171(02)90004-1. [DOI] [PubMed] [Google Scholar]
- 11.Anyfantakis D., Symvoulakis E.K., Cristodoulakis E.V., Frantzeskakis G. Ruling in the diagnosis of methanol intoxication in a young heavy drinker: a case report. Journal of Medicine and Life. 2012;5:332–334. [PMC free article] [PubMed] [Google Scholar]


