Abstract
Leprosy (Hansen’s disease) is caused by the obligate intracellular organism Mycobacterium leprae. It is an infectious, chronic granulomatous disease transmitted through close contact. The latest current data shows that in 2010, eleven new cases of leprosy were reported to the National Notifiable Diseases Surveillance System in Australia. We report the case of a patient with untreated chronic lepromatous leprosy diagnosed in Queensland, 2012. Delay in diagnosis may have been due to the rarity of this condition.
Keywords: Leprosy, Aboriginal, deformity
Implications for Practice
Leprosy is endemic in some countries with 219,075 new cases in 2011 reported to the World Health Organisation (WHO).
Leprosy has a social and health impact on affected individuals, as it is a slowly progressive disease with significant physical deformity to the face and extremities and may lead to social marginalisation if not treated.
This case report highlights that leprosy, an infectious, chronic disease, is still present in the Australian community.
Background
Leprosy (Hansen’s disease) is caused by the obligate intracellular organism Mycobacterium leprae. 1 It is an infectious, chronic granulomatous disease transmitted through close contact or droplet spread, with an incubation period of two to six years. Most immuno-competent contacts do not contract the disease as they are able to mount a sufficient immune response.1 Primarily the peripheral nerves and skin are affected causing tissue destruction and subsequent disability and deformity.1,4
Leprosy prevalence is diminishing worldwide but 219,075 new cases in 2011 were reported to the WHO, mainly in countries where leprosy is endemic.3 The majority of these cases were identified in India, Indonesia and Brazil.3 In contrast, the most recent data shows in Australia there were only eleven new cases of leprosy reported to the National Notifiable Diseases Surveillance System in 2010.2 Therefore because leprosy is rare in Australia, diagnoses may be delayed due to the lack of recognition of the clinical signs. If not treated, affected individuals develop significant physical deformity to the face and extremities which may lead to social marginalisation.1 This case report identifies a patient with chronic leprosy in whom diagnosis was delayed because of non-recognition of the clinical signs.
Case details
A 28-year-old aboriginal male presented with a one day history of fever, shortness of breath, dry cough, sore throat, lethargy, dizzy spells and a loss of appetite on a background of a 12-month history of bilateral chronic lower limb wounds. He had no significant personal medical history.
Social history : The patient consumed up to four cartons of cask wine per day. He was a current smoker with a history of 80 cigarettes per day, for the last 15 years. The patient was homeless, currently residing on the riverbank. He had never travelled interstate or overseas. His family history included a deceased uncle who had been treated for lepromatous leprosy, Mycobacterium tuberculosis infection, and type 2 diabetes mellitus.
Examination findings: All extremities were dry and cracked. The patient had leonine facies with diffuse nodular thickening of the face and ears (Figure 1). There was total loss of both eyebrows and flattening of the nose. There was evidence of thickened ulnar, radial and great auricular nerve. There were destructive changes to the right hand including shortening of all the digits with loss of the nails (Figure 2). He had loss of sensation to all fingers on the right hand. The left hand was preserved. Multiple denuded well-demarcated superficial ulcers were present bilaterally over both shins and ankles (Figure 3). There were multiple hypo-pigmented areas over the right elbow and both knees with no loss of sensation (Figure 4).
Figure 1. A 28 year-old patient with leonine facies and diffuse nodular thickening of the face.

Figure 2. Destructive changes to the right hand including shortening of all the digits with loss of the nails. Left hand preserved.

Figure 3. Multiple denuded well-demarcated superficial ulcers present on both shins and ankles.

Figure 4. Multiple hypo-pigmented areas with no loss of sensation.

Laboratory findings: Punch biopsies were taken from the margin of a right lower limb ulcer and a right foot ulcer, which identified a severe histiocytic dermal reaction associated with a large number of intracellular and extracellular acid-fast bacteria (Figure 5). Pathological findings were consistent with lepromatous leprosy. A skin biopsy of the eyebrow was acid-fast bacilli (AFB) positive with Streptococcus pyogenes and methicillin resistant Staphylococcus aureus also identified. A nasal swab was negative for AFB. A Quantiferon Gold assay was negative along with negative results for HIV, Hepatitis B and C. A nasopharyngeal aspirate revealed Haemophilus influenzae and influenza A. The patient was treated with antibiotics for pneumonia. After lepromatous leprosy was confirmed, triple therapy was commenced including rifampicin 600mg monthly, clofazimine 50mg daily and dapsone 100mg daily. The patient was discharged home on day ten with initial daily follow-up by the chest clinic for direct observed treatment. The patient also had ongoing wound care management. After six months of treatment, the ulcers on his lower limbs had healed (Figure 6).
Figure 5. Wade Fite stain showing intracellular acid-fast bacteria.
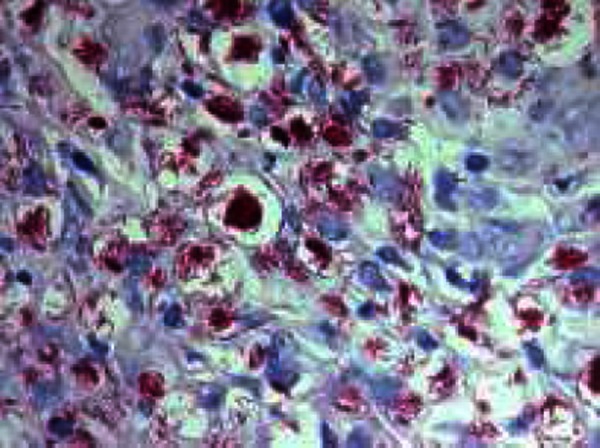
Figure 6. Healed lower limb ulcers.

Discussion
Leprosy is a slowly progressive disease with no reduction in life expectancy, as the viscera are largely preserved.1 Although a rare disease in developed countries today, there are still over 200,000 new cases of leprosy diagnosed each year worldwide.3 This case report is important because it identifies the possible delay in diagnosis of leprosy in Australia due to it being so rare. The patient in this case had presented to the same emergency department on several occasions prior to this admission. On this occasion the medical registrar on duty was from Sri Lanka and was able to make a spot diagnosis based on her clinical experience in Sri Lanka. This case report highlights the devastating effect leprosy has on the physical and emotional well-being of the affected individual and that there is a high likelihood of delayed diagnosis in Australia.
ACKNOWLEDGEMENTS
Dr Monika Rhunke, Dr Shiromali Malalasekera, Dr Myint Soe, Dr Ranjith Ralapanawa, Jean-Pierre Meyer
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
We declare no competing interests.
PATIENT CONSENT
The authors, Sally Barkla and Sunny Modi declare that:
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Barkla S, Modi S. Lepromatous Leprosy: A rare presentation in Australia. AMJ 2013, 6, 4, 175-177.http//dx.doi.org/10.4066/AMJ.2013.1604
References
- 1.Chimenos Küstner E, Pascual Cruz M, Pinol Dansis C, Vinals Iglesias H, Rodríguez de Rivera Campillo ME, López López J. Lepromatous leprosy: A review and case report. Med Oral Patol Oral Cir Bucal. 2006 Nov 1;11(6):E474–9. [PubMed] [Google Scholar]
- 2.Australian Bureau of Statistics, 1301.0 - Year Book Australia. 2009–10: Communicable Diseases. 2012 [Google Scholar]
- 3.World Health Organization. Global leprosy situation, 2012. Weekly epidemiological record. 2012;34(87):317–328. [Google Scholar]
- 4.Walker S, Lockwood D. Leprosy. Clin. Dermatol. Clin Dermatol. 2007;25(2):165–172. doi: 10.1016/j.clindermatol.2006.05.012. [DOI] [PubMed] [Google Scholar]


