Abstract
We report a case of a right radial pseudoaneurysm due to assault. The pseudoaneurysm was treated successfully with prolonged ultrasound-guided compression for more than 300 minutes over multiple sittings coupled with the use of a compression device. We believe that if initial compression fails, a prolonged ultrasound-guided compression repair coupled with a compression device can greatly improve the success rates and can negate the use of more invasive procedures to treat pseudoaneurysms.
Keywords: Pseudoaneurysm, Ultrasound-Guided Compression Repair (UGCR), Prolonged Compression, Radial Artery
Implications for Practice
What is known about such cases? Pseudoaneurysms are commonly seen in clinical practice, most often resulting from endovascular procedures or trauma.
What is the key finding reported in this case report? We present a case of pseudoaneurysm treated successfully by prolonged ultrasound-guided compression along with the use of a compression device.
What are the implications for future practice? Even if the first round of compression repair fails, in all cases of pseudoaneurysms, effort must be made in attempting a prolonged ultrasound-guided compression repair before resorting to the more invasive treatment options.
Background
A pseudoaneurysm, also termed a false aneurysm, is a leakage of arterial blood from an artery into the surrounding tissue with a persistent communication between the originating artery and the resultant adjacent cavity. Common causes of pseudoaneurysms include blunt and penetrating trauma and endovascular procedures.1
Ultrasound-guided compression repair (UGCR) is a simple, non-invasive and cost-effective method for repairing noncomplicated pseudoaneurysms, especially those arising from superficial vessels. Usually UGCR is tried only for one session and if the pseudoaneurysm does not heal, other more invasive methods are tried.2 We did not come across any literature that advocated a prolonged UGCR if the first session of UGCR fails. We report a case of a right radial artery pseudoaneurysm secondary to assault that was treated with a prolonged UGCR requiring more than 300 minutes coupled with the interval application of a compression device over a span of three days.
We feel that this report is relevant as pseudoaneurysm is a rather common clinical condition and multiple longer sessions of UGCR should be attempted even if the first round of compression fails before the use of more invasive treatment options, each of which has its own set of associated complications.
Case details
A 36-year-old male with a history of assault was referred to the Department of Radiology. He presented with a painful, pulsatile 5 x 5.5 cm swelling over his right arm below the cubital fossa.
A colour Doppler ultrasonography showed a pseudoaneurysm of size 3.8 x 4.2 cm with a neck size of 5 mm (Figure 1). The platelet count and coagulation profile was normal. The patient was not on any anticoagulants. A written informed consent was taken and compression of the pseudoaneurysm neck was done with the Doppler ultrasonography transducer for 40 minutes, however Colour Doppler done showed that the pseudoaneurysm had not been repaired. Nonetheless, it was noted that there was growing thrombosis and the pseudoaneurysm cavity had marginally decreased in size, this prompted us to believe that further sessions of UGCR would be beneficial. The patient received in total 180 minutes of UGCR with each session of compression lasting between 10-40 minutes subject to operator endurance. The patient was monitored via ultrasound for signs of distal thrombosis, following which the pseudoaneurysm had significantly reduced in size, but not completely obliterated. Hence the patient was asked to come again the next day (Figure 2). The patient was asked to report immediately to the hospital if he had any symptoms suggestive of distal ischemia or thrombosis. On day 2, UGCR was continued, this time for a total of 120 minutes. With each sitting the cavity progressively reduced with the evidence of growing thrombosis, but a small pseudoaneurysm cavity still persisted. The patient was sent home, this time with a compression device fashioned out of a plastic tube after checking the distal blood flow. When he returned on day 3, Doppler ultrasonography showed that the pseudoaneurysm cavity had obliterated Figure 3). We followed up with the patient for four weeks. There was no residual pain and the aneurysm remained obliterated.
Figure 1. Pseudoaneurysm prior to compression (Day 1).
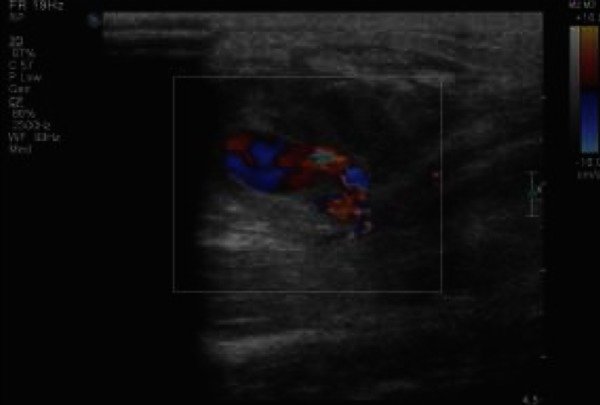
Figure 2. Pseudoaneurysm showing partially obliterated cavity prior to compression (Day 2).

Figure 3. Complete obliteration of pseudoaneurysm upon removal of compression device (Day 3).

Discussion
With the advent of modern imaging techniques such as ultrasound and CT angiography, the diagnosis of pseudoaneurysms has become more common. This allows early therapeutic intervention before complications of pseudoaneurysms can manifest.3,4 Moreover, pseudoaneurysms themselves have become more common due to the increased number of interventional procedures and the more frequent use of continued anticoagulation.5
There are a variety of modalities available for treatment of pseudoaneurysms. Surgical methods include bypass procedures, arterial ligation, and the partial or complete removal of the organ containing the pseudoaneurysm. Previously, surgery was the gold standard for treating pseudoaneurysms; however, traditional surgical treatment is highly invasive and is often associated with significantly higher morbidity. Now, surgical intervention is usually limited to complicated pseudoaneurysms such as infected pseudoaneurysms, when it leads to a significant mass effect, eg, when it is associated with distal ischemia or neuropathy, prolonged history and in cases where the non-surgical treatments failed.6,7
Endoluminal management includes embolisation and stenting. If the donor artery is expendable, embolisation of the donor artery alone is suitable, otherwise a stent graft placement or embolisation with a stent or balloon remodeling is required. Complications associated with endovascular techniques include intra-procedural rupture of the pseudoaneurysm and recanalisation of the embolised vessel. 8
Another modality is ultrasound-guided thrombin injection. After complete Doppler ultrasonography evaluation of the pseudoaneurysm is performed, thrombin is injected into the sac under ultrasound guidance with a sterile technique. The needle is positioned in the centre of the sac, and thrombin is injected at a constant rate while flow within the sac is monitored with Doppler Ultrasonography. Complications include thromboembolic events due to thrombin flowing into the arterial system leading to thrombosis of distal vessels and allergic reactions such as generalised urticaria and anaphylaxis.2,4 Contraindications to the procedure include known allergic reaction to thrombin, presence of infection, absence of a neck, large defect on the arterial wall, anastomotic aneurysms in bypasses and arteriovenous dialysis access.5
Compared to all of the above-mentioned methods, Ultra sound-guided compression repair is the most simple, cost effective and least invasive modality to treat pseudoaneurysms. Superficial pseudoaneurysms such as those affecting the femoral, axillary and radial arteries, that are not too large (<4cm) wherein compression using an ultrasound transducer achieves complete occlusion of the neck of the aneurysm preventing any inflow of blood into the aneurysmal sac are ideal cases to attempt UGCR.2 The risk factors for failure include a large size (> 4 cm) pseudoaneurysm and concomitant anticoagulant therapy. Thus, before the procedure, anticoagulants should be discontinued, if possible. Complications are rare, and failure rates of 15%–38% have been reported.5
Typical protocol includes an initial 10–40 minute compression of the pseudoaneurysmal neck.2 However, from our experience with the presented case, we feel that even if the initial attempt of compression fails to obliterate the pseudoaneurysm, a prolonged UGCR coupled with the use of a compression device can improve the success rate provided there is a progressive decrease in the size of the pseudoaneurysmal cavity with growing thrombosis after each session of UGCR. This we believe will reduce the cost of treatment and also potentially avoid the complications associated with the more invasive treatment options. The location and type of the pseudoaneurysm, along with cooperation of the patient and operator endurance are important factors in determining the success of ultrasoundguided compression of pseudoaneurysms.9 Only when prolonged compression aided by the use of interval compression with a compression device also fails (as evidenced by the failure of reduction of the pseudoaneurysm cavity size after a session of UGCR), should the more invasive treatment methods be applied.
Conclusion
Ultrasound-guided compression repair is the safest, simplest and most cost-effective method for treating pseudoaneurysms. We advocate trying a prolonged ultrasound-guided compression repair in all suitable cases over multiple sessions coupled with a compression device even if the first round of compression repair fails, provided there is a progressive decrease in the cavity size of the pseudoaneurysm with each session of compression; doing so can reduce patient morbidity and treatment costs. Only when the prolonged ultrasound guided compression fails should the more invasive treatment option be attempted.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
PATIENT CONSENT
The authors, Joseph V, Sambhaji C, Prakashini K declare that:
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Joseph V, Sambhaji C, Prakashini K. Radial artery pseudoaneurysm managed by prolonged ultrasound-guided compression repair and aided by interval application of compression device. AMJ 2013, 6, 4, 192-195.http//dx.doi.org/10.4066/AMJ.2013.1677
References
- 1.El AS, Guo W, Loveless T, Dhaliwal SS, Quereshy FA, Baur DA, Kaka NS. Pseudoaneurysm of the external carotid artery secondary to subcondylar fracture. Int J Oral Maxillofac Surg. 2011 Jun;40(6):644–6. doi: 10.1016/j.ijom.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Morgan R, Belli A. Current treatment methods for postcatheterization pseudoaneurysms. J Vasc Interv Radiol. 2003 Jun;14(6):697–710. doi: 10.1097/01.rvi.0000071089.76348.6a. [DOI] [PubMed] [Google Scholar]
- 3.Arata MA, Cope C. Principles used in the management of visceral aneurysms. Tech Vasc Intervent Radiol. 2000;3:124–129. [Google Scholar]
- 4.Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005 Oct 25;(1):S173–89. doi: 10.1148/rg.25si055503. [DOI] [PubMed] [Google Scholar]
- 5.Brophy DP, Sheiman RG, Amatulle P, Akbari CM. Iatrogenic femoral pseudoaneurysms: thrombin injection after failed US-guided compression. Radiology. 2000 Jan;214(1):278–82. doi: 10.1148/radiology.214.1.r00ja10278. [DOI] [PubMed] [Google Scholar]
- 6.Esfe ARG, Bozorg SMV, Yazdi HR. Pseudoaneurysm of a high origin radial artery treated by ultrasound-guided compression. Singapore Med J. 2009;50(7):e250. [PubMed] [Google Scholar]
- 7.Leone V, Misuri D, Console N. Radial artery pseudoaneurysm after a single arterial puncture for bloodgas analysis: a case report. Cases Journal. 2009;2:6890. doi: 10.4076/1757-1626-2-6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guillon R, Garcier JM, Abergel A, Mofid R, Garcia V, Chahid T, Ravel A, Pezet D, Boyer L. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc Intervent Radiol. 2003 May-Jun;26(3):256–60. doi: 10.1007/s00270-003-1948-y. [DOI] [PubMed] [Google Scholar]
- 9.Cheung YC, Wan YL. Peripheral arterial pseudoaneurysm treated by ultrasound-guided compression. Postgrad Med J. 1997;73:651–652. doi: 10.1136/pgmj.73.864.651. [DOI] [PMC free article] [PubMed] [Google Scholar]


