Abstract
Background:
Behavioral risk factors are responsible for a substantial portion of chronic disease. Educating patients is a professional responsibility of medical practitioners. However, it has been observed that physicians did not practice what they preach. To study whether medical colleges inculcate health-promoting lifestyle among medical students during their stay in medical colleges.
Methods:
A cross-sectional study conducted in two conveniently selected medical colleges in southern India. Fourth year MBBS students were included in the study. A pre-tested self-administered multiple choice type questionnaire was used to collect data. Information was sought on the behavioral factors, namely smoking, alcohol use, junk food consumption, and physical activity, before joining the medical college and at the time of the study. SPSS version 10.0 was used to analyze the data. Frequencies, proportions, chi-square test.
Results:
Out of 176 respondents, 94 (53%) were males and 82 (47%) were females. The number of smokers had increased from 24 (13.6%) to 46 (26.1%) and the number of alcohol consumers from 34 (19.3%) to 77 (43.8%) since they joined medical college. The number of students doing any physical activity declined from 76 (43.2%) to 43 (24.4%) and their food habits became unhealthier during the same period.
Conclusions:
The study reported an increase in health-risking behavior and a decline in health-promoting behavior among medical students during their stay in medical college.
Keywords: Lifestyle, medical colleges, medical students
INTRODUCTION
Chronic non-communicable diseases are assuming increasing importance among adult population in both developed and developing countries. The behavioral risk factors of smoking, nutrition, alcohol, and lack of physical activity (SNAP) are responsible for a substantial portion of chronic disease.[1] Public health interventions aimed at improving health often involve promoting healthy lifestyle by addressing these behavioral risk factors in general population. Giving advice and educating the patient are viewed as a professional responsibility by all general practitioners and are expected by the patients too.[2] However, researchers in many countries showed that medical students and graduates of medical colleges, as well as physicians, did not practice what they preach. High prevalence of smoking, drinking (alcohol), low level of physical activity, unsafe sex practices, and obesity among physicians were observed in studies conducted in Japan,[3] Hungary,[4] and Israel.[5] It is reported that 39.1% of physicians smoked in the presence of their patients, 34.7% did not think that they harmed themselves, and 45.7% did not consider that they harmed other people (NIH, 2003).[6] Given the significant potential for negative outcomes to physicians’ own health as well as the health and safety of their patients, examination of the acculturation process about development of related health-promoting/risking lifestyle patterns over the continuum of medical training is critical to the improvement of the health care delivery system. The aim of this cross-sectional study is to describe the changes in prevalence of health-promoting/risking lifestyle among medical students during their stay in the medical colleges.
METHODS
This cross-sectional study was conducted in two conveniently selected medical colleges in southern India. Two colleges were included in the study to avoid institutional bias. Ethical clearance was obtained from the institutional ethical committee and informed consent was obtained from the participants from both the colleges. The participating colleges were ensured that a complete confidentiality and anonymity shall be maintained. Fourth year medical students were selected for the study as they have spent over 3 years in the medical college. Inclusion criterion was all students of the regular batch of fourth year and exclusion criterion was all the irregular batch students as they may have spent more time in the medical college than the regular batch students. The purpose of the study and all the terms used in the questionnaire were explained to the students. The students were also ensured complete confidentiality and anonymity of the participants. A pre-tested self-administered multiple choice type questionnaire was used to collect data. Information was sought on the status of the students regarding the behavioral factors under study, namely smoking, alcohol use, junk food consumption, and physical activity, before joining the medical college and at the time of the study. The students who had reported smoking or using alcohol even once were taken as users. Those who were smoking or using alcohol before joining the medical college and have not done so after joining the college were taken as to have quitted the use. The criteria for physical activity were defined as those adults aged 18–64 who were doing at least 150 minutes of moderate-intensity aerobic physical activity throughout the week.[7] Junk foods were defined as any of various pre-packaged snack foods, high in calories but low in nutritional value.[8]
Statistical analysis
The data were analyzed using statistical package SPSS version 10.0. Frequencies, proportions, and chi-square test were the statistical methods used to interpret the findings.
RESULTS
There were a total of 185 students studying in the regular batch of fourth year MBBS in the medical colleges under study: 89 in college “A” and 96 in college “B.” Five students were absent from their class in the college “A” and four students were absent from their class in the college “B” on the day of study. All of the 176 students who were present at the time of study gave their consent to participate in study and filled up the questionnaire. Ninety-four (53%) among them were males and the remaining 82 (47%) were females. The study reported an increase in health-risking behaviors and a decline in health-promoting behaviors among the medical students during their stay in medical college [Figure 1].
Figure 1.
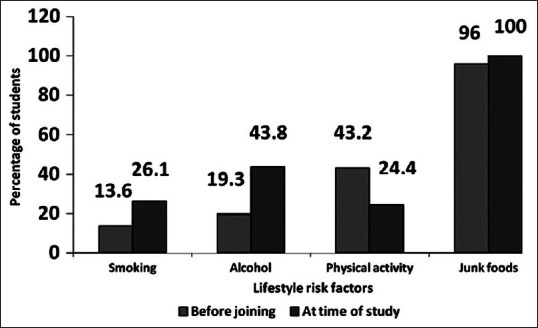
Lifestyle risk factors among fourth year medical students before joining the medical college and at the time of study
There was no statistically significant difference between the observations from the two colleges.
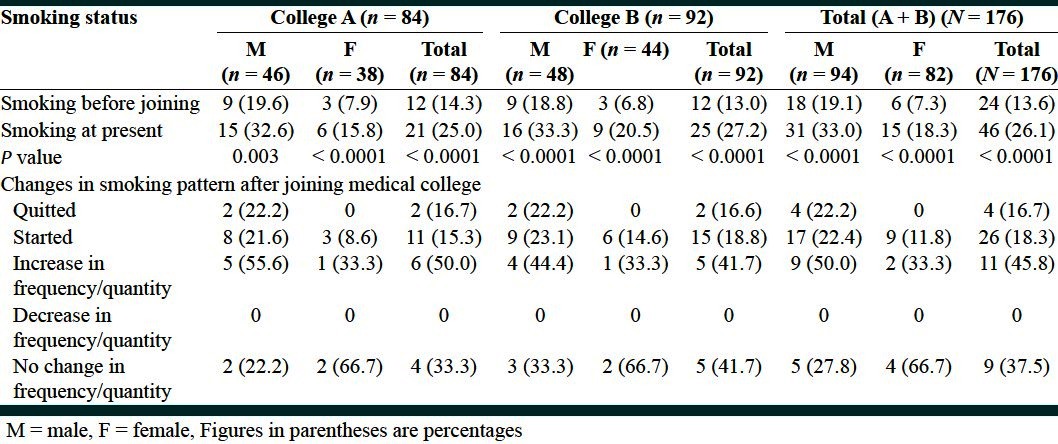
The study revealed that the number of smokers among medical students had almost doubled from 24 (13.6%) to 46 (26.1%) since they joined the medical college [Table 1]. A statistically significant increase was observed in the prevalence rate of smoking among males as well as females after joining the medical college. Though smoking was more prevalent among male medical students than females before joining the medical college as well as after 3 years of their stay in medical college, female medical students were getting into smoking faster than male medical students. Peer pressure was mentioned as the reason to get into smoking by majority [24 (48%)] of the smokers, followed by stress 14 (28%), desire to experiment 10 (20%), and freedom by 2 (4%) of the smokers (both females). Peer pressure was observed to be more prevalent among boys (54.3%) as compared to girls (33.3%); among girl students, stress (33.3%) was an equally important reason to start smoking.
Table 1.
Pattern of smoking among fourth year medical students
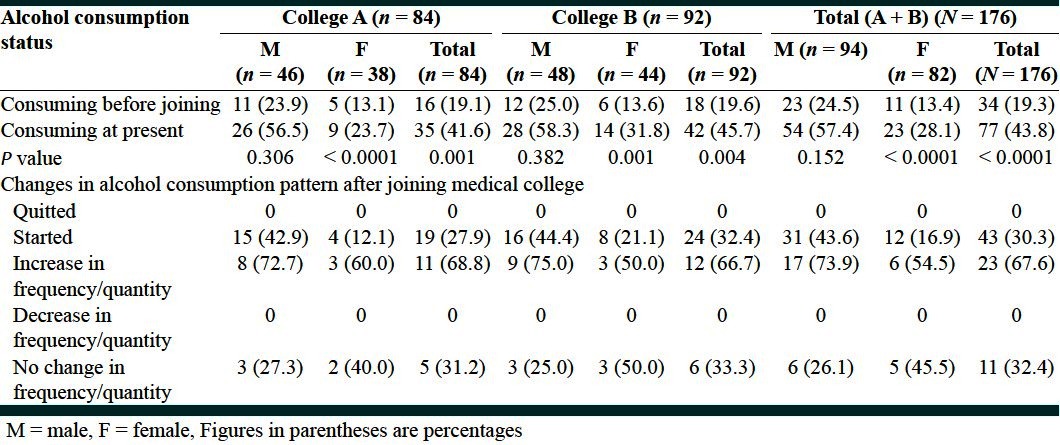
A statistically significant increase was observed in the prevalence of alcohol consumption among respondents since joining the medical college [Table 2]. Reasons to initiate alcohol consumption given by male and female students were quite different and this difference was statistically significant (P = 0.012). Majority of male consumers [29 (53.7%)] cited peer pressure as a reason to start consuming alcohol, followed by stress [11 (20.4%)], desire to experiment [8 (14.8%)] and freedom [6 (11.1%)]. Whereas, 6 (26.1%) and 5 (21.7%) of the female consumers mentioned freedom and to experiment as reasons for getting into alcohol consumption, respectively. Peer pressure was mentioned as the reason to start alcohol consumption by 10 (43.5%) female consumers and stress was the reason for only 2 (8.7%) females.
Table 2.
Pattern of alcohol consumption among fourth year medical students
A statistically significant decrease in the physical activity by medical students was observed since their joining medical college. Lesser proportion of females [17 (20.7%)] was having any physical activity as compared to 59 (43.2%) male students, and this proportion further declined to 9 (10.9%) during their stay in the medical college. It was observed that only 5 (5%) medical students stared any physical activity after joining the medical college, whereas 39 (51.9%) stopped and 27 (35.5%) reported decrease in their physical activity during the same period of time. Long working hours and lack of time was cited as the reason for stopping or decrease in their physical activity by all of the students.
At the time of study, 100% students reported eating junk foods. They also reported an increase in the quantity and frequency of eating junk food as well as irregularity in their eating habits after their joining medical college. All the students cited poor quality of food, lack of choice in available foods, and mess timings as the main causes for their unhealthy eating habits.
DISCUSSION
The focus on preventing chronic disease is increasing worldwide, which identifies the importance of promoting healthy lifestyles by addressing risk factors in general practice. However, it has been reported that the physicians vary in their attempts to motivate their patients to change risk behavior.[2] Physicians’ own behaviors and perceptions about lifestyle may have a direct impact on the advice that they provide to their patients. Physicians who live healthier lifestyles have been found to be more likely to discuss these lifestyles with their patients and to encourage their patients to behave in healthier ways.[9,10] The present study revealed an increase in health-risking behaviors and a decline in health-promoting behaviors among medical students during their stay in medical colleges. It was observed that the number of smokers among medical students had increased almost by twofold and the number of alcohol consumers by 2.5-fold since they joined their respective medical colleges, whereas the number of students doing any physical activity had reduced to half during the same period of time and food habits of all of the students had become unhealthier. These results are consistent with the observations made elsewhere that students were healthier prior to beginning medical school and that less healthy behaviors become evident by the time they begin residency.[11] It has been observed that if physicians do not engage in these healthy behaviors, they are less likely to encourage such behaviors in their patients,[9,12] and patients are less likely to listen to them even if they do talk about it.[13] Given the significant potential for negative outcomes to physicians’ own health as well as the health and safety of their patients, examination of the natural history of this acculturation process about physician self-care and lifestyle development is critical to the improvement of the health care delivery system.
Limitations of the study
This was a cross-sectional study based on recall by medical students; therefore, no inferences about causation may be made from these data.
CONCLUSION
Health and health risk behaviors as well as beliefs about self-care represent a significant part of the formation of professional identity for physicians which is not being given due attention at present. Therefore, it is recommended to develop such a system in our medical colleges that provides adequate education and support for the development of healthy lifestyle among medical students as part of their training process.
ACKNOWLEDGMENTS
I express my gratitude toward the group of interns from my institute for helping me in data collection and Ms. Neevan D’Souza for her help in statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mathers CD, Vos ET, Stevenson CE, Begg SJ. The Australian burden of disease study: Measuring the loss of health from diseases, injuries and risk factors. Med J Aus. 2000;172:592–6. doi: 10.5694/j.1326-5377.2000.tb124125.x. [DOI] [PubMed] [Google Scholar]
- 2.Ampt AJ, Amoroso C, Harris MF, McKenzie SH, Rose VK, Taggart JR. Attitudes, norms and controls influencing lifestyle risk factor management in general practice. BMC Fam Pract. 2009;10:1–23. doi: 10.1186/1471-2296-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohida T, Sakurai H, Mochizuki Y, Kamal AM, Takemura S, Minowa M, et al. Smoking prevalence and attitudes toward smoking among Japanese physicians. JAMA. 2001;285:2643–8. doi: 10.1001/jama.285.20.2643. [DOI] [PubMed] [Google Scholar]
- 4.Piko BF. Does knowledge count? Attitudes toward smoking among medical, nursing, and pharmacy students in Hungary. J Community Health. 2002;27:269–77. doi: 10.1023/a:1016330310931. [DOI] [PubMed] [Google Scholar]
- 5.Siegel-Itzkovich J. Lifestyles of medical students in Jerusalem are “shocking”. [Last accessed on 2011 Apr 28];Student British Medical Journal. 2002 10:445–6. Available from: http://archive.student.bmj.com/back_issues/1202/news/445a.html . [Google Scholar]
- 6.Khachkalyan T, Petrosyan V, Soghikian K. Association between health risk knowledge and risk behaviour among medical students and residents in Yerevan. Californian J Health Promot. 2006;4:197–206. [Google Scholar]
- 7.WHO. Physical activity and adults: Recommended levels of physical activity for adults aged 18 - 64 years. [Last accessed on 2011 Apr 28]. Available from: http://www.who.int/dietphysicalactivity/factsheet_adults/en/index.html .
- 8.Junk foods: Definition. The American Heritage Medical Dictionary Copyright. Houghton Mifflin Company. 2007. [Last accessed on 2011 April 28]. (Page number not available). Available from: http://medical.dictionary.thefreedictionary.com/junk+food .
- 9.Frank E, Rothenberg R, Lewis C, Belodoff BF. Correlates of physicians’ prevention-related practices. Findings from the women physicians’ health study. Arch Fam Med. 2000;9:359–67. doi: 10.1001/archfami.9.4.359. [DOI] [PubMed] [Google Scholar]
- 10.Lewis CE, Clancy C, Leake B, Schwartz JS. The counseling practices of internists. Ann Intern Med. 1991;114:54–8. doi: 10.7326/0003-4819-114-1-54. [DOI] [PubMed] [Google Scholar]
- 11.Hull SK, DiLalla LF, Dorsey JK. Prevalence of health-related behaviours among physicians and medical trainees. Acad Psychiatry. 2008;32:31–8. doi: 10.1176/appi.ap.32.1.31. [DOI] [PubMed] [Google Scholar]
- 12.Broquet KE, Rockey PH. Teaching residents and program directors about physician impairment. Acad Psychiatry. 2004;28:221–5. doi: 10.1176/appi.ap.28.3.221. [DOI] [PubMed] [Google Scholar]
- 13.Frank E, Breyan J, Elon L. Physician disclosure of healthy personal behaviours improves credibility and ability to motivate. Arch Fam Med. 2000;9:287–90. doi: 10.1001/archfami.9.3.287. [DOI] [PubMed] [Google Scholar]


