Abstract
Background:
Motivational interviewing (M.I.) is an option for modifying an individual's behavior. It is used as an educational method in recent years. The aim of our study was to indicate whether or not education, using lecture alone and lecture with M.I., would affect the performance of nursing personnel regarding their hand hygiene. If so, which of these two methods were most effective for this purpose?
Methods:
This was an interventional study conducted in Bahrami Pediatric Hospital in Tehran. The study population consisted of all nursing personnel in the hospital. Considering the responsibilities of different nurses and their educational status, we divided them into three classes. The participants of each class were randomly assigned to either the control or experiment groups training lecture alone or lecture with M.I., respectively. We used Independent-t, Paired-t, Mann-Whitney U and Wilcoxon signed ranks tests for analysis.
Results:
Education using lecture alone improved the hand hygiene performance of nursing personnel only in the first and third classes (P = 0.002 and P = 0.001, respectively). Similarly, lecture combined with M.I. improved the hand hygiene performance of personnel in the first and third classes (P < 0.001 and P = 0.004, respectively). The latter method was more effective compared to lecture alone in the first and third classes (P < 0.001 and P = 0.013, respectively).
Conclusions:
Education based on lecturing improves hand hygiene performance among nursing personnel. It will be more effective if combined with M.I.
Keywords: Hand washing, health education, interview, lectures, nursing staff
INTRODUCTION
According to the 2005 report of the World Health Organization (WHO), over 1.4 million people suffer from nosocomial infections worldwide. In developed countries, about 5-10% of patients admitted to hospitals contract nosocomial infections, which is 25% in developing countries. Studies conducted in countries with average income indicate that an annual sum of 8 billion dollars is spent every year to resolve nosocomial infections. Therefore, WHO has developed different strategies, most importantly hand hygiene as reflected in the motto, “Clean care is safer care, and clean hands are safer hands”.[1] Interventions such as educational programs influence the function of healthcare personnel. In order to improve the function of personnel, it is better to utilize cognitive, behavioral and emotional methods. On the other hand, it is established that hand hygiene is the most important procedure for preventing infection transmission; nevertheless, this simple procedure is largely ignored by healthcare personnel.[2,3] Compliance with the principles of hand hygiene is particularly important in pediatric hospitals.[4–6]
M.I. is an option for modifying an individual's behavior. It was developed by Miller to treat patients with alcoholism issues and then completed by Miler and Rollnick.[7] M.I. is a directive, client-oriented approach to improve an individual's internal motives for modifying behavior; it facilitates behavioral modification through helping the person identify his/her doubts regarding behavior modification and overcome them. Expressing empathy, developing discrepancy, avoiding argumentation, rolling with resistance, and supporting self-efficacy are the clinical principles of M.I.[8]
The present study attempted to indicate whether or not education, using lecture alone and lecture with M.I., would affect the performance of nursing personnel regarding their hand hygiene. If so, which of these two methods were most effective for this purpose?
METHODS
Study design and setting
This was an interventional study conducted in Bahrami Pediatric Hospital, affiliated to Tehran University of Medical Sciences in 2010. The objective of lecture-based education is to introduce the protocol of hand hygiene and its importance in controlling nosocomial infection to study units. The educational material dealing with hand hygiene was prepared by the researcher and confirmed by the physician in charge of hospital's infection control (subspecialist in pediatric infectious diseases and faculty member of our university's pediatric department) and a specialist in infectious disease (faculty member of our university's infectious disease department). Hand hygiene education was performed by an infection control nurse via a 2-h lecture; the lecture session was repeated a few times in such a way as to cover all the personnel working in different shifts. In addition to the lecture, individuals in the experiment group participated in M.I., conducted by a health psychology specialist (faculty member of the psychology department, University of Tabriz). Five sessions of interviewing were held, with a maximum of 15 participants and duration of 90 min.
Measurement
Data were collected using hand hygiene checklist, developed by the researchers based on the protocols of the WHO and Center for Disease Control (CDC), Feldman criteria, and Fulkerson activity classification criteria, in 5 sections. The first section contained 8 statements about the participants’ demographic data; the second section contained 6 statements about routine hand decontamination; the third section contained 10 statements about using alcohol rub products, the fourth section contained 12 statements about routine cases; and the fifth section contained 6 statements about evaluation of hand hygiene. Data were collected by the hospital's infection control supervisor who had received the required training about hand hygiene. Content validity of the tool was confirmed by infectious specialists. We used test re-test to evaluate the reliability of the tool on 30 nursing personnel. So, at first session, the observer completed checklist according to personnel's activities and scored them and 30 days later she repeated it on the same persons. In next step, we calculated correlation of data. The reliability was acceptable (r > 0.7). These 30 individuals were eliminated from the final sample.
Study sample
The study was conducted in Bahrami Pediatric Hospital and the study population consisted of all nursing personnel in the hospital. The participants were assigned to either the control or experiment groups using the table of random numbers. Considering the responsibilities of different nurses and their educational status, we divided them into three classes: The first one included nurses, operating room technicians, anesthesiology technicians and nurse-aids; the second one included head nurses; and the third one included assistant nurse-aids. Since direct observation and the personnel's awareness of the hand hygiene checklist could affect their function, the infection control supervisor completed the checklists without notifying the personnel and during the routine nursing activities. Prior to training with lecture alone and lecture with M.I., the supervisor completed the checklist for each participant in the experiment and control groups; after training, the checklists were completed again by the same person for all participants. It should be noted that in order to prevent information exchange between the two groups, participants in the control group were first educated about hand hygiene and their checklists were completed; subsequently, participants in the experiment groups underwent lecture and M.I. and then had their checklists completed. Once the data were collected, data pertaining to each of the three classes of the control and experiment groups were analyzed separately.
Ethical consideration
The informed consent was obtained from all participants. The study complied with current ethical considerations in accordance with the rules of the ethical review board of Tehran University of Medical Sciences.
Statistical analysis
We used Independent-t, Paired-t, Mann-Whitney U and Wilcoxon Signed Ranks tests for analysis. Alpha was considered lower than 5%.
RESULTS
A total of 128 individuals were selected for the study, with 64 in the experiment group and 64 in the control group. 12 (9.4%) were male and 116 (90.6%) were female.
Experiment group
The mean age (± standard deviation) of the participants was 35.83 ± 7.184 years. As for education, 6 (9.4%) were below diploma, 8 (12.5%) had high school diploma, 1 (1.6%) had an associate degree, and 49 (76.6%) had a bachelor's degree or higher. Regarding marital status, 11 (17.2%) were single and 53 (82.8%) were married. As for organizational position, there were 42 (65.6%) nurses, 3 (4.7%) nurse aids, 1 (1.6%) operating room technicians, 1 (1.6%) anesthesiology technicians, 5 (7.8%) head nurses, and 12 (18.8%) assistant nurse-aids.
Control group
The mean age (± standard deviation) of the participants was 34.58 ± 7.946 years. As for education, 6 (9.4%) were below diploma, 9 (14.1%) had high school diploma, 3 (4.7%) had an associate degree, and 46 (71.9%) had a bachelor's degree or higher. Regarding marital status, 10 (15.6%) were single and 54 (84.4%) were married. As for organizational position, there were 41 (64.8%) nurses, 2 (3.1%) nurse aids, 2 (3.1%) operating room technicians, 2 (3.1%) anesthesiology technicians, 5 (7.8%) head nurses, and 12 (18.8%) assistant nurse-aids.
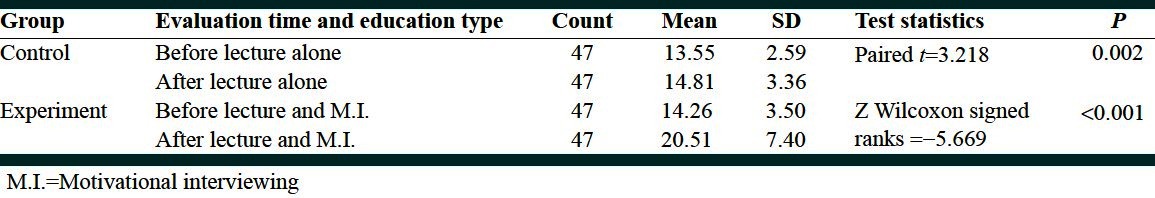
The mean ± standard deviation of hand hygiene scores of first class of participants was 13.55 ± 2.59 before intervention and 14.8 ± 3.36 after intervention in the control group, and 14.26 ± 3.50 before intervention and 20.51 ± 7.40 after intervention in the experiment group. The hand hygiene scores of first class of participants in the control and experiment groups were significantly different before and after intervention [Table 1].
Table 1.
Comparing hand hygiene scores before and after intervention in the two groups consisting of first class of participants
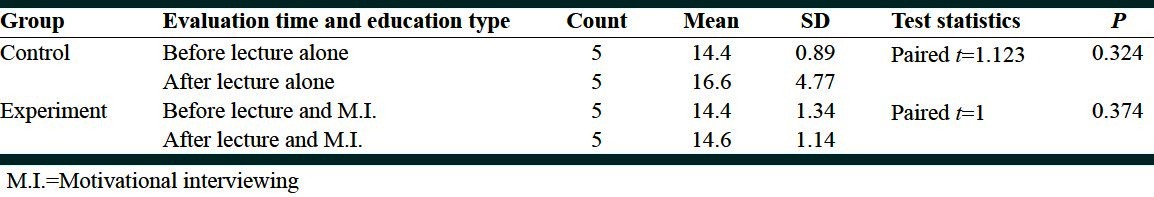
The mean (± standard deviation) of hand hygiene scores in second class of participants of the control group was 14.4 ± 0.89 before intervention and 16.6 ± 4.77 after intervention, whereas in the experiment group, it was 14.4 ± 1.34 before intervention and 14.6 ± 1.14 after intervention. The hand hygiene scores of second class of participants were not significantly different before and after intervention in head nurses of both control and experiment groups [Table 2].
Table 2.
Comparing hand hygiene scores before and after intervention in the two groups consisting of second class of participants
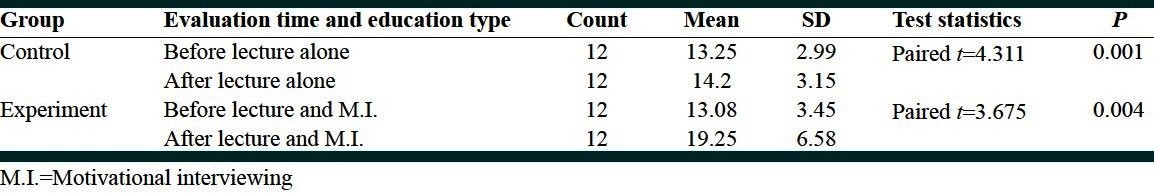
The mean (± standard deviation) of hand hygiene scores in third class of participants of the control group was 13.25 ± 2.99 before intervention and 14.2 ± 3.15 after intervention, whereas in the experiment group, it was 13.08 ± 3.45 before intervention and 19.25 ± 6.58 after intervention. The hand hygiene scores of third class of participants were significantly different before and after intervention in both control and experiment groups [Table 3].
Table 3.
Comparing hand hygiene scores before and after intervention in the two groups consisting of third class of participants
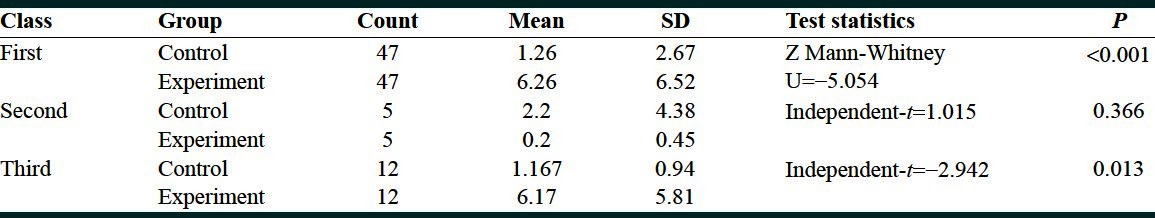
We compared the improvement in hygiene scores before and after the intervention (lecture alone and lecture with M.I. for the control and experiment groups, respectively) between first class of participants of the control and experiment groups, and we found a statistically significant difference (P < 0.001). Subsequently, we compared the improvement in hygiene scores before and after the intervention (lecture alone and lecture with M.I. for the control and experiment groups, respectively) between second class of participants of the control and experiment groups, and we found no statistically significant difference (P = 0.366). In next step, we compared the improvement in hygiene scores before and after the intervention (lecture alone and lecture with M.I. for the control and experiment groups, respectively) between third class of participants of the control and experiment groups, and we found a statistically significant difference (P = 0.013) [Table 4].
Table 4.
Comparing the improvement in hand hygiene scores before and after education between the two groups consisting of three classes of participants
DISCUSSION
In this study, we compared the hand hygiene performance of three classes of hospital personnel before and after educating them in two different methods. Education using lecture alone improved the hand hygiene performance of nursing personnel only in the first and third classes (P = 0.002 and P = 0.001, respectively). Similarly, lecture combined with M.I. improved the hand hygiene performance of personnel in the first and third classes (P < 0.001 and P = 0.004, respectively). It is noteworthy that the latter method (lecture combined with M.I.) was more effective compared to lecture alone in the first and third classes (P < 0.001 and P = 0.013, respectively). We did not observe a significant improvement in hand hygiene scores of nurses in the second class with either method (all P > 0.05), which is probably due to the small number of participants –5 in each of the control and experiment groups.
Education plays a pivotal role in establishment of hand hygiene and prevention of nosocomial infections. In addition, any plan for improving hand hygiene in healthcare personnel should focus on factors affecting the behavior of personnel regarding their hand hygiene; they should be trained about caring for patients while exposing him/her to the minimal risk of infection, and should be familiarized with the necessity of hand hygiene as an efficient method for reducing nosocomial infections. M.I. can be particularly helpful for this purpose. Hands of healthcare personnel can transmit pathogens from one patient to another or from the environment to patients.[9] Microorganisms are colonized on patients’ skin or the environment (medical tools) and they can be transmitted on hands of personnel. Unless hands are sufficiently washed and sanitized, these microorganisms will survive and may be transmitted to the next patient or the tools. Previous studies indicated that healthcare personnel carry the patients’ skin flora, as 102-103 colony forming units (CFUs) of Klebsiella had been isolated from skins of nurses who cared for patients.[10,11] Some studies reported that personnel might acquire and carry Gram negative bacilli, Staph. aureus, Enterococcus, or Clostridium difficile from patients’ normal skin. Repeated cultures indicated that 100% and 64% of healthcare personnel had carried Gram negative bacilli and Staph. aureus, respectively, at least once on their hands.[12–18] For this reason, the World Health Organization (WHO) has developed a number of strategies, with hand hygiene at the top, in order to ensure the protection of patients against infection in healthcare centers.[1]
Extensive studies have dealt with the issue of hand hygiene and the rate of compliance with recommended guidelines; the majority of these studies indicate that the healthcare personnel have a low rate of compliance with hand hygiene protocols–often below 50%.[19,20] Teaching hand hygiene to healthcare personnel may improve their hand washing techniques.[21] Hand hygiene guidelines and training healthcare personnel influence their function.[22] A study by Conrad et al., in 2010 demonstrated that short educational sessions of hand hygiene are negatively correlated with methicillin resistant Staphylococcus.[23] Lack of sufficient scientific information about the importance of hand hygiene by personnel will pose obstacles for achieving the goals of hand hygiene protocols, thus increasing the rate of nosocomial infections. In 2000, a Swiss university published the results of its policies implemented from 1993 to 1998 to promote the use of alcohol rub by healthcare personnel and preparation of educational materials and programs to improve hand hygiene and control nosocomial infections. These policies provided personal alcohol rub solutions for the personnel, containers of alcohol rub dispensers were placed next to patients’ beds for convenience, the personnel were encouraged to carry the bottles of sanitizing solution in their pockets, and educational posters and reminders were hung in the environment. As a result, the efficiency of educations rose from 48% in 1994 to 66% in 1997 (P < 0.001). Although hand washing with water and soap was still in use, the amount of alcohol rub used per 1000 patients/day increased from 3.5 L to 15.4 L (P < 0.001). These studies indicated that better educational methods will result in better acceptance by personnel, and eventually reducing the risk of transmission of pathogenic microorganisms and nosocomial infections. The approach to hygiene improvement should address the issue through a variety of aspects, as most authors believe this method to be optimal for improving personnel commitment.[1,24] A study by Won et al., in 2004 observed an improvement in commitment of personnel employed in a neonatal intensive care unit from 43% to 80% following hygiene improvement programs.[25]
M.I. is a method for modifying individuals’ behaviors.[26–30] It is particularly suitable for modifying the behavior of individuals who resist the change.[31] Dilorio et al., observed that M.I. improved the adherence of patients with AIDS to antiretroviral therapy in 2003.[32] LaBrie et al., demonstrated the effectiveness of M.I. in modifying the behavior of American students regarding their alcohol intake.[33]
Study limitations and strength
Our research had some limitations. We studied only nursing personnel of a subspecialty pediatric hospital in capital of our country. So, the external validity of study was not high. Furthermore, although we achieved a randomized controlled clinical trial, we did not have any blinding.
CONCLUSIONS
Our findings indicate that education based on lecturing improves hand hygiene performance among nursing personnel. Furthermore, we analyzed that education will be more effective if combined with M.I.
Footnotes
Source of Support: The Present Study was Financed from the Research Credits Allocated to Tehran University of Medical Sciences under Registry Number 8847-76-02-88 Dated December 9th, 2009
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva: WHO; 2006 . [Last cited on 2006 Sept 05]. WHO. WHO Guidelines for hand hygiene in health care (Advanced Draft) Available from: http://www.who.int/patient safety/challenge/en . [Google Scholar]
- 2.Akyol AD. Hand hygiene among nurses in Turkey: Opinions and practice. J Clin Nurs. 2007;16:431–7. doi: 10.1111/j.1365-2702.2005.01543.x. [DOI] [PubMed] [Google Scholar]
- 3.Creedon SA. Health care workers hand decontamination practices: Compliance with recommended guidelines. J Adv Nurs. 2005;51:208–16. doi: 10.1111/j.1365-2648.2005.03490.x. [DOI] [PubMed] [Google Scholar]
- 4.Salamati P, Rahbarimanesh AA, Yunesian M, Naseri M. Neonatal nosocomial infections in Bahrami children hospital. Indian J Pediatr. 2006;73:197–200. doi: 10.1007/BF02825479. [DOI] [PubMed] [Google Scholar]
- 5.Salamati P, Zargar M, Eghbalkhah A, Chaman R, Sotoudeh K, Navabi B, et al. Prediction of pediatric mortality in Bahrami children's hospital pediatric intensive care unit (PICU) based on pediatric index of mortality-2 (PIM2) J Isfahan Med Sch. 2010;28:1–10. [Google Scholar]
- 6.Barak M, Mamishi S, Siadati A, Salamati P, Khotaii GH, Mirzarahimi M. Risk factors and bacterial etiologies of nosocomial infections in NICU and PICU Wards of children's medical center and bahrami hospitals during 2008-2009. J Ardabil Univ Med Sci. 2011;2:113–20. Persian. [Google Scholar]
- 7.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- 8.Arborelius E, Eklund AB. Smoke-free pregnancy: Motivational interviewing, a guide for midwives. [Last cited on 2012 Jul 08]. Available from: http://www.motivationalinterview.net/clinical/Smoke.free_pregnancy_eng.pdf .
- 9.Bhalla A, Pultz NJ, Gries DM, Ray AJ, Eckstein EC, Aron DC, et al. Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect Control Hosp Epidemiol. 2004;25:164–7. doi: 10.1086/502369. [DOI] [PubMed] [Google Scholar]
- 10.Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Recommendations of the healthcare infection control practices advisory committee and the ICPAC/SHEA/APIC/IDSA Hand hygiene task force. Society for healthcare epidemiology of America/Association for professionals in infection Control/Infectious diseases society of America. MMWR Recomm Rep. 2002;51:1–45. [PubMed] [Google Scholar]
- 11.Casewell M, Phillips I. Hands as route of transmission for Klebsiella species. Br Med J. 1977;2:1315–7. doi: 10.1136/bmj.2.6098.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McBryde ES, Bradley LC, Whitby M, McElwain DL. An investigation of contact transmission of methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2004;58:104–8. doi: 10.1016/j.jhin.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 13.McFarland LV, Mulligan ME, Kwok RY, Stamm WE. Nosocomial acquisition of clostridium difficile infection. N Engl J Med. 1989;320:204–10. doi: 10.1056/NEJM198901263200402. [DOI] [PubMed] [Google Scholar]
- 14.Ojajarvi J. Effectiveness of hand washing and disinfection methods in removing transient bacteria after patient nursing. J Hyg (Lond) 1980;85:193–203. doi: 10.1017/s0022172400063221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pessoa-Silva CL, Dharan S, Hugonnet S, Touveneau S, Posfay-Barbe K, Pfister R, et al. Dynamics of bacterial hand contamination during routine neonatal care. Infect Control Hosp Epidemiol. 2004;25:192–7. doi: 10.1086/502376. [DOI] [PubMed] [Google Scholar]
- 16.Samore MH, Venkataraman L, DeGirolami PC, Levin E, Karchmer AW. Clinical and molecular epidemiology of sporadic and clustered cases of nosocomial Clostridium difficile diarrhea. Am J Med. 1996;100:32–40. doi: 10.1016/s0002-9343(96)90008-x. [DOI] [PubMed] [Google Scholar]
- 17.Sanderson PJ, Weissler S. Recovery of coliforms from the hands of nurses and patients: Activities leading to contamination. J Hosp Infect. 1992;21:85–93. doi: 10.1016/0195-6701(92)90027-j. [DOI] [PubMed] [Google Scholar]
- 18.Waters V, Larson E, Wu F, San Gabriel P, Hass J, Cimiotti J, et al. Molecular epidemiology of gram negative bacilli from infected neonates and health care workers’ hands in neonatal intensive care units. Clin Infect Dis. 2004;38:1682–7. doi: 10.1086/386331. [DOI] [PubMed] [Google Scholar]
- 19.Nova AM, Pi-Sunyer T, Sala M, Molins E, Castells X. Evaluation of hand hygiene adherence in a tertiary hospital. Am J Infect Control. 2007;35:676–83. doi: 10.1016/j.ajic.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Pittet D, Mourouga P, Perneger TV. Compliance with hand washing in a teaching hospital. Ann Intern Med. 1999;130:126–30. doi: 10.7326/0003-4819-130-2-199901190-00006. [DOI] [PubMed] [Google Scholar]
- 21.Lam BC, Lee J, Lau YL. Hand hygiene practices in a neonatal intensive care unit: A multimodal intervention and impact on nosocomial infection. Pediatrics. 2004;114:565–71. doi: 10.1542/peds.2004-1107. [DOI] [PubMed] [Google Scholar]
- 22.Rosenthal VD, McCormick RD, Guzman S, Villamayor C, Orellano PW. Effect of education and performance feedback on hand washing: The benefit of administrative support in Argentinean hospitals. Am J Infect Control. 2003;31:85–92. doi: 10.1067/mic.2003.63. [DOI] [PubMed] [Google Scholar]
- 23.Conrad A, Kaier K, Frank U, Dettenkofer M. Are short training sessions on hand hygiene effective in preventing hospital-acquired MRSA? A time-series analysis. Am J Infect Control. 2010;38:559–61. doi: 10.1016/j.ajic.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 24.lankford MG, Zemblower TR, Trick WE, Hacek DM, Noskin GA, Peterson LR. Influence of role models and hospital design on hand hygiene of health workers. Emerg Infect Dis. 2003;9:217–23. doi: 10.3201/eid0902.020249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Won SP, Chou HC, Hsieh WS, Chen CY, Huang SM, Tsou KI, et al. Hand washing program for the prevention of nosocomial infections in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2004;25:742–6. doi: 10.1086/502470. [DOI] [PubMed] [Google Scholar]
- 26.Blaakman S, Tremblay PJ, Halterman JS, Fagnano M, Borrelli B. Implementation of a community-based secondhand smoke reduction intervention for caregivers of urban children with asthma: Process evaluation, successes and challenges. Health Educ Res. 2013;28:141–52. doi: 10.1093/her/cys070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Mallakh P, Chlebowy DO, Wall MP, Myers JA, Cloud RN. Promoting nurse interventionist fidelity to motivational interviewing in a diabetes self-care intervention. Res Nurs Health. 2012;35:289–300. doi: 10.1002/nur.21472. [DOI] [PubMed] [Google Scholar]
- 28.Jackman K. Motivational interviewing with adolescents: An advanced practice nursing intervention for psychiatric settings. J Child Adolesc Psychiatr Nurs. 2012;25:4–8. doi: 10.1111/j.1744-6171.2011.00304.x. [DOI] [PubMed] [Google Scholar]
- 29.Drevenhorn E, Bengtson A, Nilsson PM, Nyberg P, Kjellgren KI. Consultation training of nurses for cardiovascular prevention-a randomized study of 2 years duration. Blood Press. 2012;21:293–9. doi: 10.3109/08037051.2012.680734. [DOI] [PubMed] [Google Scholar]
- 30.Karzenowski A, Puskar K. Motivational interviewing: A valuable tool for the psychiatric advanced practice nurse. Issues Ment Health Nurs. 2011;32:436–40. doi: 10.3109/01612840.2011.565907. [DOI] [PubMed] [Google Scholar]
- 31.Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: It sounds like something is changing. Health Psychol. 2002;21:444–51. [PubMed] [Google Scholar]
- 32.Dilorio C, Resnicow K, McDonnell M, Soet J, McCarty F, Yeager K. Using motivational interviewing to promote adherence to antiretroviral medications: A pilot study. J Assoc Nurses AIDS Care. 2003;14:52–62. doi: 10.1177/1055329002250996. [DOI] [PubMed] [Google Scholar]
- 33.LaBrie JW, Lamb TF, Pedersen ER, Quinlan T. A group motivational interviewing intervention reduces drinking and alcohol-related consequences in adjudicated college students. J Coll Stud Dev. 2006;47:267–80. [Google Scholar]


