Abstract
Background:
This study aimed to assess the salt intake of Iranian children, and to assess the correlation of urinary electrolytes excretion with blood pressure.
Methods:
This cross-sectional study was conducted in 2011-2012 among 3-10-year-old children, selected by multi-stage cluster sampling from urban and rural areas of Isfahan, Iran. The sodium (Na), potassium (K), and creatinine (Cr) were measured in a random sample of the children's first morning fasting urine. Three-day averages of dietary intakes were analyzed by the Nutritionist-4 software.
Results:
The mean (SD) of urinary Na was 177.17 (28.68) mEq/day without significant difference according to gender and living area. The mean (SD) dietary intakes of Na and K were 2017.76 (117.94) and 1119.06 (76.03) mg/day, respectively. Children of urban and rural areas consumed similar sources of salty foods (bread, cheese, and snacks) and had low intake of vegetables. No significant association was documented between urinary electrolytes excretions and blood pressure.
Conclusions:
This study, which to the best of our knowledge is the first of its kind in the Middle East and North Africa region, revealed that Iranian young children consume a large amount of sodium and small amount of potassium. The non-significant associations of electrolyte excretions with blood pressure may be because of the very young age group of participants. Given the development of preference to salt taste from early childhood, and the tracking of risk factors of chronic diseases from this age, reducing salt intake of young children should be emphasized.
Keywords: Blood pressure, prevention, salt intake, urine electrolytes
INTRODUCTION
Establishing food preferences and healthy eating habits in childhood have long-term health effects. Preferences for food tastes are learned and developed through exposure. Consuming salty foods is one of important issues in this regard. Although decreasing dietary sodium intake is highly recommended,[1] but still this point has received little attention for children.
Salt modifies the taste of foods and may make them enjoyable.[2] Therefore, families may provide salty foods for their children for increasing their food intake. Although limited experience exists on the short-term effects of dietary salt intake on blood pressure (BP), but establishment of dietary habits from early life, and tracking of BP from childhood to adulthood,[3] elucidate the importance of determining the salt intake of young children.
Troubles in collecting 24-hour urine and diet recall make sodium intake estimation more difficult.[4,5] Since 24-hour urine collection is troublesome in children, measuring spot urine sodium has been recommended.[6–8] Therefore, early morning spot urine has been used to estimate sodium excretion.[9] A systematic review on comparing 24-hour vs. partial urine collections for estimating population salt intake showed that most studies advocated spot urine sampling mostly because of its convenience and feasibility.[10–12] Although, 24-hour urine sampling is more accurate in comparison with spot urine sampling, the last method can be used in epidemiological studies.[10,13] Spot urine sodium-to-potassium ratio (Na/K) has been also used in evaluating dietary Na restriction in cirrhotic patients,[14] and in chronic kidney diseases patients to evaluate their Na intake.[7,15] Some studies reported high salt intake in young children of Western countries. Limited experience exists about other populations. Non-communicable diseases and their risk factors as high BP are an emerging global health problem, notably in developing countries.[16]
Among these populations, the situation of the Middle East and North Africa (MENA) region is of special concern because of the rapid nutrition transition and very high prevalence rates of non-communicable diseases.[17] However, limited data exist on the dietary salt intake in children of this region. This study was conducted in a representative sample of young Iranian children to estimate the salt intake and to assess its correlation with BP.
METHODS
This cross-sectional study was conducted in 2011-2012 among 3-10-year-old children living in urban and rural areas of Isfahan, Iran. It was approved by the Research and Ethics Committee of Isfahan University of Medical Sciences; written informed consent was obtained from parents of all participants. By considering α error of 0.05 and β error of 20%, the sample size was calculated as 110 in each area (urban/rural). Because of possible missing data, we increased the sample size to 120 in each area.
Children were selected by multistage random cluster sampling from households living in the study area. Those children with any chronic disease, any physical or mental disability, and history of any medication use, and/or those on special diet or any recent acute disease were not recruited to the study.
A team of trained physician and nurses conducted the study under standard protocols and by using calibrated instruments. Demographic characteristics as age, gender, parents’ education level and job, household number, and past medical history were recorded.
As it is well-documented that assessment of Na and K excretion in spot urine sample is as valid as measuring them in 24-hour-urine sample.[6,15] In this study, a random sample of the children's first morning fasting urine sample was collected. The urine Na and K were measured by flame method and the urine creatinine (Cr) by Jaffe's method.
Mothers were interviewed about the type and amount of food eaten by their children, using scales or household measures to gauge portion sizes. Three-day averages of intakes were analyzed by the Nutritionist-4 software (First Databank Inc., Hearst Corp., San Bruno, CA). Data entry was performed by a trained dietitian. Nutrient information was also obtained through food labels or recipes from participants.
Systolic and diastolic BP (SBP, DBP) were measured on the right arm, with the individual in a sitting position and at rest for at least 5 min, using standardized mercury sphygmomanometer and appropriate size cuff. Two measurements at two-minute intervals were recorded and the average was used for the statistical analysis.[18] The mean arterial pressure (MAP) was calculated by the following equation: MAP = 2/3 DBP + 1/3 SBP.
Statistical analysis
Data analyses were performed using Statistical Package for the Social Sciences (SPSS) (version 16:0, SPSS Inc., Chicago, IL) software. Continuous variables are reported as the mean, standard deviation (SD), and minimum, maximum, median, and interquartile range. The relationship of urinary excretion of Na and K with SBP, DBP, and MAP was assessed by regression analysis and Pearson correlation analysis. The significance level was set at P < 0.05.
RESULTS
Data of 241 children (51% girls, 50% urban) were complete and were included in the statistical analysis. BP and urinary excretion of Na, K, and Cr are presented in Table 1. The mean (SD) values of SBP and DBP were 102.05 (15.89) and 64.30 (14.23) mmHg, respectively. The mean (SD) of urinary Na was 177.17 (28.68) mEq/day without significant difference according to gender and living area. The corresponding figures were 170 and 96 mEq/day for its median and interquartile range.
Table 1.
Blood pressure and urinary excretion of sodium, potassium, and creatinine of children studied by gender and living area

Table 2 presents the daily intake of macronutrients, Na and K of children studied. As no significant difference was documented in terms of gender and living area, the findings are presented in the whole population studied. The mean (SD) of Na intake was 2017.76 (117.94) mg/day. In the whole population studied, the main sources of Na intake were bread, cheese and snacks.
Table 2.
Daily dietary intake of children based on 3-day food record
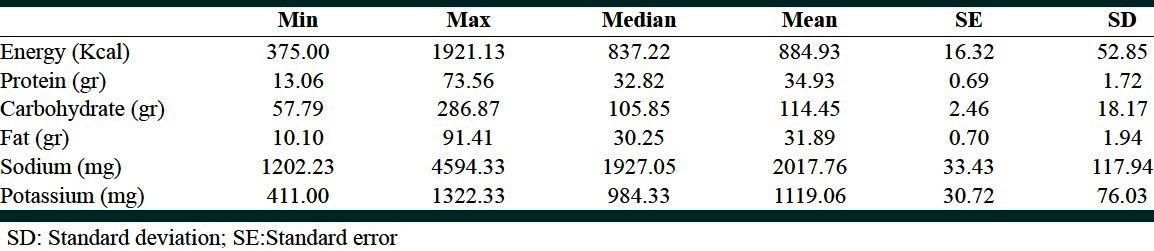
Figure 1 demonstrates the results of the regression analyses of Na/Cr and K/Cr with SBP, DBP, and MAP. None of the relationships was significant. Likewise, further analysis according to gender and living area revealed non-significant results.
Figure 1.
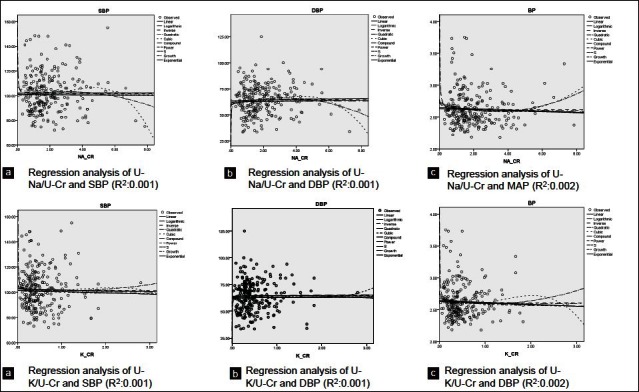
Regression analysis of urine sodium and potassium to creatinine ratios with systolic, diastolic, and mean arterial blood pressure. U-Na: Urine sodium, U-K: Urine potassium, U-Cr: Urine creatinine, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MAP: Mean arterial pressure
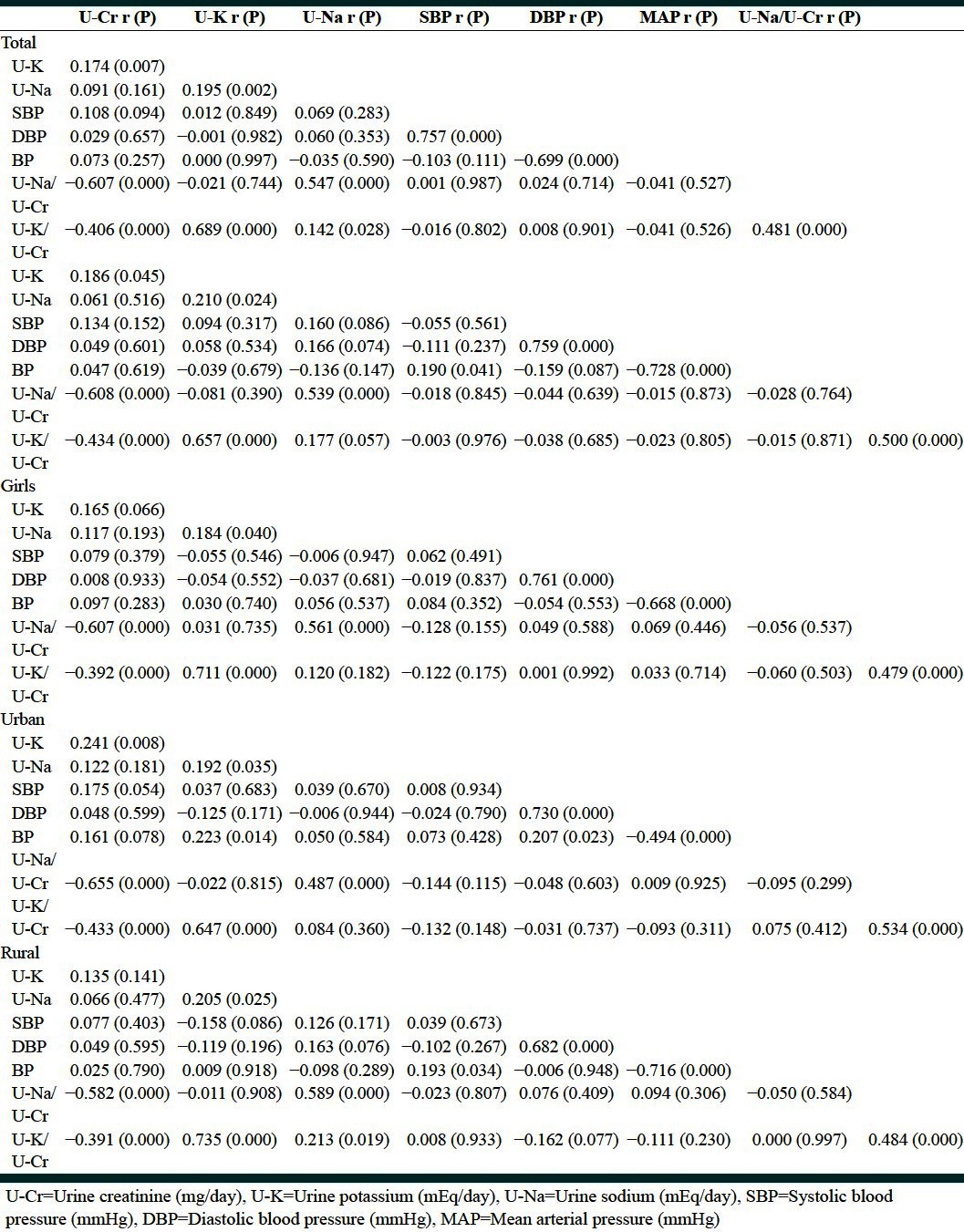
The association of variables studied determined by Pearson correlation analysis in total and according to gender and living area are presented in Table 3, and reveal no significant relationship between Na intake, urinary excretion of Na, K, and Cr with SBP, DBP, and MAP.
Table 3.
Pearson correlation coefficients of variables studied
DISCUSSION
This study, which to the best of our knowledge is the first of its kind in the MENA region, the urinary Na level was high among young children. Iranian young children consume a large amount of sodium and small amount of potassium both in urban and rural areas. Given the development of preference to salt taste from early life, and the tracking of risk factors of non-communicable diseases from this age, reducing salt intake of young children should be emphasized.
The recommended Na and K intake in children aged 3-10 years ranges from <1,500 to <1,900 mg/day and 3,000-3,800 mg/day,[19] whereas, in the current study, the mean intakes of Na and K were 2,017.76 mg/day and 1,119.06 mg/day, respectively. Our findings may be explained by the high salt content of bread, cheese, and snacks in Iran, as well as the low intake of vegetables by children. The tracking of nutrient intake from childhood to adulthood is well documented.[20–23]
Therefore, persistence of this pattern of nutrient intake by children can be a substantial determinant of dietary habits and chronic diseases in adulthood. Considering the importance of prehypertension and the increasing prevalence of essential hypertension in the pediatric age group,[24] controlling the salt intake of children should be considered as a priority at individual and public health levels.
Socioeconomic status is considered as one of most important determinants of diet quality in children and adolescents.[25,26] However, such association is inconsistent regarding salt intake; for instance a study in the UK revealed higher Na intake in individuals with lower socioeconomic status,[27] whereas, this finding was not confirmed in the US population.[28] Such experience is very limited in the pediatric age group. A recent study in Australia found that children of lower socioeconomic levels had greater dietary Na intake than their counterparts from a high socioeconomic background.[29]
We did not document significant differences between children of urban and rural areas; this may be because the main sources of salt intake, i.e., bread, cheese, and salty snacks as cheese puff and potato chips, are regularly used by all Iranian children and not limited to urban areas or a special socioeconomic class. The current finding on the high intake of salty foods and low intake of vegetables by children is consistent with our previous nationwide study among 6-18-year-old children,[30] and the current study confirms such situation in young children aged as young as 3 years. These findings underscore of the importance of increasing the awareness of families about healthy diet for their children, as well as the importance of reducing the salt content of food products by food industries.
Our findings are also consistent with a study conducted among 3-year-old Japanese children, who had high Na intake mainly by consuming snack, and low K intake by low intake of fruits and vegetables. This study also showed that presence of an older sibling influenced the dietary habit of the younger sibling. This confirms the role of family in establishment of dietary habits from early life.[31]
High salt intake in children is usually part of an unhealthy dietary pattern, for instance higher consumption of soft drinks.[32] A large study among Australian children revealed that each additional 1 g/day of salt intake was accompanied with 17 g/day higher intake of sugar-sweetened beverage, and in turn increased risk of overweight and obesity.[33] Higher Na intake was associated with higher systolic but not diastolic BP in American children aged 8-15 years.[34] An association between changes in BP and urinary Na/K ratio has been shown in Stanford Three Community Study.[35] In addition, the association between BP and urinary Na excretion in children has been reported by Cooper et al.[36] Nevertheless, Walker et al., demonstrated a negative correlation between DBP and urinary K.[37] We did find significant association between urinary electrolytes and BP; this may be mainly because of the very young age of participants. It is noteworthy to consider that in addition to elevated BP, high salt intake is also considered as a risk factor for many other health disorders as stroke, left ventricular hypertrophy, renal disease, renal stones, osteoporosis, the severity of asthma, and possibly stomach cancer.[1,38] It is well established that newborns distaste salt, but preference to salt taste develops and establishes at 2-3 years of age.[39] High Na content of children's foods and snacks is a universal problem, as reported recently for the high salt content of foods prepared for infants and children.[40] Reducing the Na intake and increasing the K intake of children is strongly recommended by the World Health Organization,[41] but still this issue deserves more attention from health policy-makers. Actually, reducing salt intake is recognized as a national health priority in Iran[42] but the high Na intake by very young children should also be considered by health authorities.
Study limitations and strengths
The main limitation of this study is its cross-sectional nature. The dietary intakes are subject to be not precise, because of the difficulties in filling food records, and accurate measurement of salt consumed, however, they can provide an estimate of the intake, in our study, the urine electrolytes confirmed the findings of children's dietary intakes. The novel aspects of our study are being the first of its kind in the MENA region, which can add to the international evidence on Na intake of children. The other strength of the study is the young age of participants.
CONCLUSIONS
This study revealed high Na consumption by young Iranian children. Although this was not significantly associated with their current BP, but establishment of this dietary habit, may have long-term health consequences. Childhood is the most important life period for development of food preferences and healthy eating habits, given the tracking of risk factors of chronic diseases from early life, reducing salt intake should be considered as a health priority.
ACKNOWLEDGMENTS
This study was conducted as a thesis funded by Isfahan University of Medical Sciences.
Footnotes
Source of Support: This study was conducted as a thesis funded by Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.He FJ, MacGregor GA. Reducing population salt intake worldwide: From evidence to implementation. Prog Cardiovasc Dis. 2010;52:363–82. doi: 10.1016/j.pcad.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Leshem M. Biobehavior of the human love of salt. Neurosci Biobehav Rev. 2009;33:1–17. doi: 10.1016/j.neubiorev.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Toschke AM, Kohl L, Mansmann U, von Kries R. Meta-analysis of blood pressure tracking from childhood to adulthood and implications for the design of intervention trial. Acta Paediatr. 2010;99:24–9. doi: 10.1111/j.1651-2227.2009.01544.x. [DOI] [PubMed] [Google Scholar]
- 4.Livingstone MB, Robson PJ, Wallace JM. Issues in dietary intake assessment of children and adolescents. Br J Nutr. 2004;92(Suppl 2):S213–22. doi: 10.1079/bjn20041169. [DOI] [PubMed] [Google Scholar]
- 5.Simons-Morton DG, Obarzanek E. Diet and blood pressure in children and adolescents. Pediatr Nephrol. 1997;11:244–9. doi: 10.1007/s004670050271. [DOI] [PubMed] [Google Scholar]
- 6.Subramanian S, Teo BW, Toh QC, Koh YY, Li J, Sethi S, et al. Spot urine tests in predicting 24-Hour urine sodium excretion in Asian patients. J Ren Nutr. 2013:S1051–2276. doi: 10.1053/j.jrn.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Kang SS, Kang EH, Kim SO, Lee MS, Hong CD, Kim SB. Use of mean spot urine sodium concentrations to estimate daily sodium intake in patients with chronic kidney disease. Nutrition. 2012;28:256–61. doi: 10.1016/j.nut.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Mann SJ, Gerber LM. Estimation of 24-hour sodium excretion from spot urine samples. J Clin Hypertens (Greenwich) 2010;12:174–80. doi: 10.1111/j.1751-7176.2009.00241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–38. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 10.Ji C, Sykes L, Paul C, Dary O, Legetic B, Campbell NR, et al. Systematic review of studies comparing 24-hour and spot urine collections for estimating population salt intake. Rev Panam Salud Publica. 2012;32:307–15. doi: 10.1590/s1020-49892012001000010. [DOI] [PubMed] [Google Scholar]
- 11.Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20:7–14. doi: 10.1111/j.1440-1681.1993.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103. doi: 10.1038/sj.jhh.1001307. [DOI] [PubMed] [Google Scholar]
- 13.Joint Health Surveys Unit. National Center for Social research. A survey of 24 hour and spot urinary sodium and potassium excretion in a representative sample of the Scottish population. [Last accessed 2012 Sept 20]. Available from: http://www.natcen.ac.uk/study/scottish-salt-intake .
- 14.El-Bokl MA, Senousy BE, El-Karmouty KZ, Mohammed lel K, Mohammed SM, Shabana SS, et al. Spot urinary sodium for assessing dietary sodium restriction in cirrhotic ascites. World J Gastroenterol. 2009;15:3631–5. doi: 10.3748/wjg.15.3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogura M, Kimura A, Takane K, Nakao M, Hamaguchi A, Terawaki H, et al. Estimation of salt intake from spot urine samples in patients with chronic kidney disease. BMC Nephrol. 2012;13:36. doi: 10.1186/1471-2369-13-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, et al. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–97. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- 17.Fahed AC, El-Hage-Sleiman AK, Farhat TI, Nemer GM. Diet, genetics, and disease: A focus on the Middle East and North Africa region. J Nutr Metab. 2012;2012:109037. doi: 10.1155/2012/109037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National high blood pressure education program working group on high blood pressure in children and adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. (2 Suppl 4th Report) [PubMed] [Google Scholar]
- 19.Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Lichtenstein AH, et al. Dietary recommendations for children and adolescents: A guide for practitioners. Pediatrics. 2006;117:544–59. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 20.Patterson E, Wärnberg J, Kearney J, Sjöström M. The tracking of dietary intakes of children and adolescents in Sweden over six years: The European Youth Heart Study. Int J Behav Nutr Phys Act. 2009;6:91. doi: 10.1186/1479-5868-6-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lake AA, Mathers JC, Rugg-Gunn AJ, Adamson AJ. Longitudinal change in food habits between adolescence (11-12 years) and adulthood (32-33 years): The ASH30 Study. J Public Health (Oxf) 2006;28:10–6. doi: 10.1093/pubmed/fdi082. [DOI] [PubMed] [Google Scholar]
- 22.Singer MR, Moore LL, Garrahie EJ, Ellison RC. The tracking of nutrient intake in young children: The Framingham Children's Study. Am J Public Health. 1995;85:1673–7. doi: 10.2105/ajph.85.12.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mikkilä V, Räsänen L, Raitakari OT, Pietinen P, Viikari J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: The cardiovascular risk in young finns study. Eur J Clin Nutr. 2004;58:1038–45. doi: 10.1038/sj.ejcn.1601929. [DOI] [PubMed] [Google Scholar]
- 24.Kelishadi R, Poursafa P, Keramatian K. Overweight, air and noise pollution: Universal risk factors for pediatric pre-hypertension. J Res Med Sci. 2011;16:1234–50. [PMC free article] [PubMed] [Google Scholar]
- 25.Ambrosini GL, Oddy WH, Robinson M, O’Sullivan TA, Hands BP, de Klerk NH, et al. Adolescent dietary patterns are associated with lifestyle and family psycho-social factors. Public Health Nutr. 2009;12:1807–15. doi: 10.1017/S1368980008004618. [DOI] [PubMed] [Google Scholar]
- 26.Utter J, Denny S, Crengle S, Ameratunga S, Clark T, Maddison R, et al. Socio-economic differences in eating-related attitudes, behaviours and enviornments of adolescents. Public Health Nutr. 2010;14:629–34. doi: 10.1017/S1368980010001898. [DOI] [PubMed] [Google Scholar]
- 27.Bates CJ, Prentice A, Cole TJ, van der Pols JC, Doyle W, Finch S, et al. Micronutrients: Highlights and research challenges from the 1994-5 national diet and nutrition survey of people aged 65 years and over. Br J Nutr. 1999;82:7–15. doi: 10.1017/s0007114599001063. [DOI] [PubMed] [Google Scholar]
- 28.Gerber AM, James SA, Ammerman AS, Keenan NL, Garrett JM, Strogatz DS, et al. Socioeconomic status and electrolyte intake in black adults: The pitt county study. Am J Public Health. 1991;81:1608–12. doi: 10.2105/ajph.81.12.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross-sectional study. BMJ Open. 2013:3. doi: 10.1136/bmjopen-2012-002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007;85:19–26. doi: 10.2471/BLT.06.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morinaga Y, Tsuchihashi T, Ohta Y, Matsumura K. Salt intake in 3-year-old Japanese children. Hypertens Res. 2011;34:836–9. doi: 10.1038/hr.2011.55. [DOI] [PubMed] [Google Scholar]
- 32.He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: A link to obesity? Hypertension. 2008;51:629–34. doi: 10.1161/HYPERTENSIONAHA.107.100990. [DOI] [PubMed] [Google Scholar]
- 33.Grimes CA, Riddell LJ, Campbell KJ, Nowson CA. Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics. 2013;131:14–21. doi: 10.1542/peds.2012-1628. [DOI] [PubMed] [Google Scholar]
- 34.Yang Q, Zhang Z, Kuklina EV, Fang J, Ayala C, Hong Y, et al. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611–9. doi: 10.1542/peds.2011-3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farquhar J.W, Wood P.D, Haskelt W.L, Williams P, Fortman S.P. Relationship of urinary sodium/potassium ratio to systolic blood pressure The Stanford three community study. Abstracts from the Eighteenth Conference on Cardiovascular Disease Epidemiology. 1978 [Google Scholar]
- 36.Cooper R, Soltero I, Liu K, Berkson D, Levinson S, Stamler J. The association between urinary sodium excretion and blood pressure in children. Circulation. 1980;62:97–104. doi: 10.1161/01.cir.62.1.97. [DOI] [PubMed] [Google Scholar]
- 37.Walker WG, Whelton PK, Satio H, Russell RP, Hermann J. Relation between blood pressure and renin, renin substrate, angiotensin II, aldosterone and urinary sodium and potassium in 574 ambulatory subjects. Hypertension. 1977;1:287–91. doi: 10.1161/01.hyp.1.3.287. [DOI] [PubMed] [Google Scholar]
- 38.Amiri M, Kelishadi R. Can salt hypothesis explain the trends of mortality from stroke and stomach cancer in Western Europe? Int J Prev Med. 2012;3:377–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Strazzullo P, Campanozzi A, Avallone S. Does salt intake in the first two years of life affect the development of cardiovascular disorders in adulthood? Nutr Metab Cardiovasc Dis. 2012;22:787–92. doi: 10.1016/j.numecd.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 40. [Last accessed on 2012 Sept 26]. Available from: http://newsroom.heart.org/news/most-pre-packaged-meals-snacks-for-toddlers-contain-too-much-salt .
- 41.World Health Organization Guideline: Sodium intake for adults and children. Geneva: WHO; 2012. [PubMed] [Google Scholar]
- 42.Fahimi S, Pharoah P. Reducing salt intake in Iran: Priorities and challenges. Arch Iran Med. 2012;15:110–2. [PubMed] [Google Scholar]


