CASE PRESENTATION
A 2-week-old female infant presented to the pediatric primary care office with her mother for a routine well-baby check. The mother had no concerns other than routine questions about growth, developmental milestones, and feeding. The infant was born full-term via normal, spontaneous vaginal delivery. Neither the mother nor the baby had any antenatal or perinatal complications. The mother’s prenatal serologies were unremarkable, and she was rubella immune. The parents said that no problems were noted when the infant was examined after birth. Hospital records were not available for review. The family history did not include any eye problems.
EXAMINATION
Upon examination, the infant appeared alert and in no obvious distress. Her length was 50 cm (21st percentile), her weight was 3.52 kg (26th percentile), and her head circumference was 35 cm (15th percentile). She had no apparent dysmorphic features. Her heart sounds were normal, and no cardiac murmurs were appreciated. The remainder of the systemic examination was within normal limits.
Ophthalmic examination revealed that the pupils were round and equally reactive to light, with no relative afferent pupillary defect. The infant reacted to light by blinking with either eye. The lids, lashes, conjunctiva, and sclera appeared normal. The red reflex was present and clear in the left eye but was absent in the right eye. Upon closer examination, the pupil in the left eye was clear, but the pupil in the right eye had a milky appearance (leukocoria).
The infant was sent to a pediatric ophthalmologist who evaluated her and confirmed the absent red reflex in the right eye. After dilating the pupils with 0.5% cyclopentolate, a central cataract measuring approximately 4 mm with a clear lens surrounding it (Figure) was found in the right eye. The fundus was difficult to visualize in the right eye but appeared normal with a clear vitreous and no masses in the retina. The left eye lens and fundus appeared normal. A diagnosis of a congenital cataract was confirmed by the ophthalmologist, and the infant was scheduled for cataract surgery 2 weeks later. The infant was fitted with an aphakic contact lens immediately after surgery, and the parents were given instruction regarding its insertion and removal. The parents also were instructed to place a patch over the left eye for 2 hours a day to prevent amblyopia.
FIGURE.
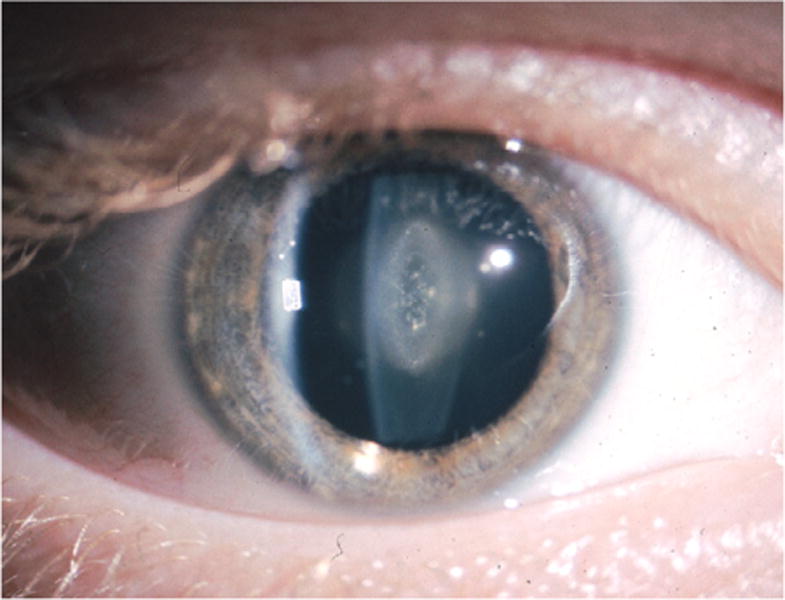
Slit beam view of the cataract through a dilated pupil showing a central, 4mm opacity in the crystalline lens. This figure appears in color online at www.jpedhc.org.
CASE STUDY QUESTIONS
What differential diagnoses should you consider in an infant with an absent red reflex in one eye?
What is the best evidence-based management for this 2-week-old infant?
What considerations are important in the follow-up of this patient?
CASE STUDY ANSWERS
1. What differential diagnoses should you consider in an infant with an absent red reflex in one eye?
Leukocoria or a white pupillary reflex is an ominous finding in infants. It can be caused by opacification of any of the structures that lie in the visual axis including the cornea, the lens, the vitreous, and the retina. The majority of these conditions are significant for visual impairment that may not be appreciated until the child is older. However, retinal conditions such as retinoblastoma (RB) can be life-threatening. Therefore screening for and evaluation of leukocoria should be performed at every well-baby and well-child visit. This screening can be performed very easily by testing for an intact red reflex using a direct ophthalmoscope (Russell, McDougall, & Dutton, 2011). Any dark opacity in the red reflex must be further investigated, which can be done by viewing the eye with magnification with or without dilation of the pupil. Dilation of the pupil is essential to rule out pathology such as RB, because it can be missed otherwise. Parents also must be counseled on leukocoria and should be instructed to look for a missing red reflex in photographs in one or both eyes when the child is looking at the camera.
Leukocoria or a white pupillary reflex is anominous finding in infants.
Corneal Conditions
Only a few corneal conditions can cause leukocoria. The most common is Peters anomaly, which is characterized by absence of the posterior stroma, Descemet’s membrane, and the endothelial layer of the central cornea (Harissi-Dagher & Colby, 2008). This absence results in a dense opacity in the center of the cornea and is associated with adhesion of the iris and sometimes of the lens to the scar. Glaucoma occurs in more than 50% of cases. Other less common corneal conditions causing leukocoria include congenital hereditary endothelial dystrophy, forceps injury, and mucopolysaccharidosis. Treatment of corneal conditions usually requires a corneal transplant to clear the visual axis and rehabilitate the vision. However, the outcomes are uniformly poor, especially in persons with Peters anomaly (Yang, Lambert, Drews-Botsch, & Stulting, 2009). Corneal conditions were not supported by the ophthalmic examination in this case.
Lenticular Conditions
A cataract is any opacification of the natural crystalline lens. Cataracts are called congenital or infantile if they occur within the first year of life, juvenile if they occur in the first decade, presenile if they occur before the age of 45 years, and senile if they occur after the age of 45 years. Congenital cataracts are a significant cause of preventable blindness in children, and some form of cataract may be seen in as many as one in every 250 live births (Krishnamurthy & Vanderveen, 2008). Infantile cataracts may occur as a result of inheritance, chromosomal anomalies, systemic syndromes, systemic diseases, perinatal illnesses (e.g., TORCH [toxoplasmosis, other diseases, rubella, cytomegalovirus, and herpes simplex virus] infections, especially rubella), trauma, or radiation (Mahalakshmi et al., 2010). Rubella cataracts are unique in that active virus can be isolated in the lens and removal of the lens can result in significant inflammation in the eye when the virus is released. Rubella cataracts are now rare because most persons in the United States receive rubella vaccinations.
Inherited cataracts are usually transmitted as an autosomal dominant trait and are nearly always bilateral; however, they may have significant asymmetry. The family history may not be available because the history frequently is not significant for visual conditions, and the parents may be unaware that they themselves have cataracts. Cataracts associated with systemic disease such as galactosemia, homocystinuria, or perinatal TORCH infections are also almost always bilateral. Anterior lenticonus is seen in patients with Alport syndrome, and posterior lenticonus is seen in patients with Lowe syndrome. Therefore bilateral cases should prompt a workup for systemic disease or an examination of the parents for undetected cataracts. Unilateral cataracts, on the other hand, are usually sporadic and are not associated with any systemic diseases or other anomalies, as is consistent with our case, in which the infant had a unilateral cataract and is otherwise healthy.
Pathophysiology
Cataracts vary significantly in their location and severity and, consequently, the degree of obstruction of vision. Sutural cataracts are opacities in the anterior and posterior ‘Y’ sutures that represent the early fetal lens fibers. These cataracts are usually innocuous, do not cause visual problems, and typically are found incidentally during an eye examination. Nuclear cataracts result from opacification of the center of the lens, as in our patient. They are considered to be visually significant if they are greater than 3 mm in diameter because they occlude the visual axis. Lamellar cataracts appear as an opaque layer in the middle of the lens with clear lens on either side (similar to one layer of an onion). These cataracts typically indicate an intrauterine insult at one stage of development that opacified the layer that developed at that stage. They usually are not visually significant. Anterior and posterior subcapsular cataracts, polar cataracts, and lenticonus are located centrally at the level of the capsule of the lens. As a general rule, posterior cataracts are more visually significant than anterior cataracts because they are located closer to the nodal point of the eye through which all light rays must pass to get to the retina.
Vitreous Conditions
Vitreous anomalies include persistent fetal vasculature, previously referred to as persistent hyperplastic primary vitreous. This condition results from the failure of the fetal hyaloid vasculature to regress at birth (Shastry, 2009) and results in an opaque, often vascularized membrane behind the lens. The lens may opacify rapidly in this condition, resulting in a shallow anterior chamber and glaucoma. Persistent fetal vasculature is invariably unilateral, and the affected eye is smaller than the other eye. Treatment consists of removal of the membranes and the cataract by a retina specialist. However, the visual prognosis is poor because the eye is usually malformed and amblyopic. Examination revealed no evidence of vitreous anomalies in our case.
Retinal Conditions
The most ominous pathology that causes leukocoria is RB, which is a malignant neoplasm of the retina. RB is the most common malignant ocular neoplasm of childhood and affects approximately 1 in 15,000 children (Houston, Murray, Wolfe, & Fernandes, 2011). It presents in the first year of life in bilateral and familial cases and between the ages of 1 and 3 years in sporadic cases. It is transmitted via an autosomal dominant inheritance pattern and maps to chromosome 13. Most cases present when the family notices a “cat’s eye reflex” or leukocoria in family photographs. Leukocoria is present because the tumor appears as a white mass within the retina and can grow to fill the entire vitreous cavity, resulting in a very poor prognosis as it spreads through the optic nerve to the brain. Calcification in the tumor is pathognomonic, and a computed tomography scan was historically the imaging modality of choice. However, patients with RB have an extremely high risk of secondary malignancies, and ultrasound or magnetic resonance imaging of the eye is preferable to decrease the radiation risk.
Treatment of RB depends on the size of the tumor and its laterality. Large, unilateral tumors are treated with enucleation (removal of the eye). Smaller tumors can be treated locally using photocoagulation, thermotherapy, or plaque therapy. Bilateral tumors are treated using chemoreduction (i.e., chemotherapy to reduce the tumor size) followed by local therapy. External beam radiation is seldom used now because of the disfiguration it causes and the higher risk of secondary malignancies in the irradiated area in persons with RB (Eng et al., 1993).
Retinopathy of prematurity (ROP) is another common cause of leukocoria. The normal retinal vasculature is not fully developed until 9 months of gestation or slightly later. If the baby is born significantly premature, the vessels do not develop in the peripheral retina and result in growth of abnormal vessels. These immature vessels and their associated fibrous tissue can lead to contraction and traction, resulting in retinal detachments. Gestational age less than 30 weeks and birth weight less than 1500 g are risk factors for the development of ROP. It is estimated that 65% to 70% of children who weigh less than 1250 g at birth will develop some degree of ROP (Reynolds, 2010). Supplemental oxygen is thought to increase the risk of retinopathy by constriction of the vessels. The retinal detachments cause the retina to become ischemic and yellow colored, thus causing leukocoria. Early diagnosis of ROP is essential to prevent severe visual loss. Premature infants with identified risk factors should receive eye examinations by an ophthalmologist. If detected early, the eye can be treated with a laser or cryotherapy to destroy the abnormal peripheral retina, thereby saving the central retina from damage.
Other Conditions
Rarer conditions include Coat’s disease, corneal scarring, toxocariasis, and optic disc coloboma (Vahedi et al., 2008). Coat’s disease is a condition with exudation of lipid into the retina and subretinal space. It occurs as a result of the presence of abnormal blood vessels in the retina, but the etiology of these vessels is unknown (Reichstein & Recchia, 2011). Corneal scarring can result from birth trauma from forceps delivery, corneal involvement in TORCH infections, and inherited disorders of metabolism such as Hurler syndrome, among others. Toxocariasis is caused by ingestion of the eggs of the dog tapeworm. This ingestion typically occurs in the late first decade, and the leukocoria occurs because of the formation of granulomas in the retina and vitreous. Optic disc colobomas are caused by incomplete closure of the optic fissure, which may be isolated or may be associated with an iris coloboma.
2. What is the best evidence-based management for this 2-week-old infant?
This infant presented with a unilateral cataract that was larger than 3 mm in size, and the evidence-based management for this case is removal of the cataract (Lloyd, Ashworth, Biswas, & Abadi, 2007). If they do not significantly obstruct the visual axis, small, less dense cataracts can be managed conservatively by using pharmacological dilation, which allows the child to see around the cataract and permits good vision until cataract surgery can be performed safely, but larger cataracts require urgent surgical management (Drummond & Hinz, 1994). Urgent management is required because the obscuration of vision from larger cataracts can disrupt the visual development and result in amblyopia (lazy eye; Lloyd et al., 2007). If amblyopia is allowed to go untreated, the vision continues to be poor even if the occluding pathology is removed. Amblyopia is much more severe in cases where the disruption is unilateral because the child can see well out of the uninvolved eye and thus ignores the affected eye. In bilateral cases, neither eye can see well, so the child is forced to use both eyes, which allows the child to develop some vision. Therefore this infant’s cataract needed to be removed within the first 6 weeks of age to allow her to see well. Surgery in these infants is not without significant risk, however, given their age and size.
Unfortunately, cataract surgery in children is very different from that in adults where the outcomes are uniformly good. Children have very robust inflammatory responses to eye surgery and can form a fibrin response after cataract surgery that potentially occludes the pupil and can obstruct vision and cause pupillary block glaucoma (Comer, Kim, Cline, & Lyons, 2011). Glaucoma occurs in about 10% to 20% of children after cataract surgery and may be difficult to treat. Fortunately, this infant had an uneventful outcome following surgery, but she will require close long-term monitoring for glaucoma.
Once the cataract is removed, visual rehabilitation is crucial. In children older than 1 year, the standard of care is now to implant an intraocular lens into the capsular bag after removing the cataract, because that approach provides superior visual outcomes (Lambert et al., 2010). However, in children younger than 1 year, intraocular lens implantation is not advised because of the inflammatory response caused by this procedure (Lambert et al., 2001). Therefore patients are left aphakic (without a lens), which does not allow the eye to focus well. Visual rehabilitation in these patients is performed with aphakic glasses in bilateral cases and with a contact lens in unilateral cases (Lindsay & Chi, 2010). Accordingly, this infant was left aphakic and fitted with a contact lens for visual rehabilitation. Treatment of her amblyopia consisted of patching the uninvolved eye to force the affected eye to develop vision.
Once a child has had cataract surgery, it is very important to support and counsel parents on the risk of amblyopia despite an excellent surgical outcome.
The long-term prognosis of bilateral cataracts treated early is good in cases without additional ocular morbidities. The outcomes of a unilateral cataract, however, are usually poor because of the difficulty in convincing parents of the importance of investing the time and money to correct the vision and the amblyopia. Once the child reaches 10 years of age, patching will no longer treat the amblyopia, and the visual deficit becomes permanent. This fact was emphasized to the infant’s parents in detail to improve compliance with the patching.
3. What considerations are important in the follow-up of this patient?
Once a child has had cataract surgery, it is very important to support and counsel parents on the risk of amblyopia despite an excellent surgical outcome. It should be explained that patching of the “good” eye is necessary to force the “bad” eye to develop vision. Children will resist covering the unaffected eye because they cannot see well with the affected eye and will cry and try to pull the patch off. Parents often give up trying to force the child to wear a patch and assume they can do the patching later in life when the child will be more compliant with patch treatment. However, it is essential for the parents to understand that waiting until the child is older is not an option because it will be too late to correct the amblyopia at that time. Rewarding children for wearing the patch by allowing them to do their favorite activities only while wearing the patch (e.g., playing video games and watching television) could encourage them to comply.
Another issue that requires compliance is use of contact lenses. Tremendous dedication is required of the parents to insert, remove, and disinfect the lenses. Use of contact lenses is also costly and time intensive because the specialized contact lenses that are needed are expensive and may not be covered by insurance. Improper care can result in infectious corneal ulcers and permanent loss of vision. Therefore counseling of the parents on lens hygiene should be performed repeatedly by the primary care provider.
CONCLUSION
Leukocoria in an infant or child is an ominous finding and, if detected, should initiate an urgent ophthalmological referral. Cataracts are the most common cause of leukocoria in children, and early diagnosis and management are usually associated with a favorable outcome. Unilateral cataracts such as the one in our patient must be removed earlier than bilateral ones because of the risk of more severe amblyopia with unilateral cataracts. Postoperatively, the eventual outcomes depend on early and successful correction of the vision using contact lenses and of pre-existing amblyopia using patching of the other eye. Both these therapies require immense dedication and time commitment from the parents, and high rates of noncompliance are typical. Therefore significant encouragement, education, and support by the primary care provider are essential to a good outcome.
Footnotes
Conflicts of interest: None to report.
Contributor Information
Sanjeev Y. Tuli, Associate Professor and Chief, Division of Ambulatory Pediatrics, Department of Pediatrics, University of Florida, Gainesville, FL.
Beverly P. Giordano, Advanced Registered Nurse Practitioner, Department of Pediatrics, University of Florida, Gainesville, FL.
Maria Kelly, Assistant Professor, Department of Pediatrics, University of Florida, Gainesville, FL.
Donald Fillipps, Assistant Professor, Department of Pediatrics, University of Florida, Gainesville, FL.
Sonal S. Tuli, Associate Professor and Residency Program Director, Department of Ophthalmology, University of Florida, Gainesville, FL.
References
- Comer RM, Kim P, Cline R, Lyons CJ. Cataract surgery in the first year of life: Aphakic glaucoma and visual outcomes. Canadian Journal of Ophthalmology. 2011;46:148–152. doi: 10.3129/i11-006. [DOI] [PubMed] [Google Scholar]
- Drummond GT, Hinz BJ. Management of monocular cataract with long-term dilation in children. Canadian Journal of Ophthalmology. 1994;29:227–230. [PubMed] [Google Scholar]
- Eng C, Li FP, Abramson DH, Ellsworth RM, Wong FL, Goldman MB, Boice JD., Jr Mortality from second tumors among long-term survivors of retinoblastoma. Journal of the National Cancer Institute. 1993;85:1121–1128. doi: 10.1093/jnci/85.14.1121. [DOI] [PubMed] [Google Scholar]
- Harissi-Dagher M, Colby K. Anterior segment dysgenesis: Peters anomaly and sclerocornea. International Ophthalmology Clinics. 2008;48:35–42. doi: 10.1097/IIO.0b013e318169526c. [DOI] [PubMed] [Google Scholar]
- Houston SK, Murray TG, Wolfe SQ, Fernandes CE. Current update on retinoblastoma. International Ophthalmology Clinics. 2011;51:77–91. doi: 10.1097/IIO.0b013e3182010f29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamurthy R, Vanderveen DK. Infantile cataracts. International Ophthalmology Clinics. 2008;48:175–192. doi: 10.1097/IIO.0b013e3181694b31. [DOI] [PubMed] [Google Scholar]
- Lambert SR, Buckley EG, Drews-Botsch C, DuBois L, Hartmann EE, Lynn MJ, Wilson ME. A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: Grading acuity and adverse events at age 1 year. Archives of Ophthalmology. 2010;128:810–818. doi: 10.1001/archophthalmol.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SR, Lynn M, Drews-Botsch C, Loupe D, Plager DA, Medow NB, Fawcett SL. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. Journal of AAPOS. 2001;5:70–75. doi: 10.1067/mpa.2001.111015. [DOI] [PubMed] [Google Scholar]
- Lindsay RG, Chi JT. Contact lens management of infantile aphakia. Clinical and Experimental Ophthalmology. 2010;93:3–14. doi: 10.1111/j.1444-0938.2009.00447.x. [DOI] [PubMed] [Google Scholar]
- Lloyd IC, Ashworth J, Biswas S, Abadi RV. Advances in the management of congenital and infantile cataract. Eye (Lond) 2007;21(1):301–1309. doi: 10.1038/sj.eye.6702845. [DOI] [PubMed] [Google Scholar]
- Mahalakshmi B, Therese KL, Devipriya U, Pushpalatha V, Margarita S, Madhavan HN. Infectious aetiology of congenital cataract based on TORCHES screening in a tertiary eye hospital in Chennai, Tamil Nadu, India. Indian Journal of Medical Research. 2010;131:559–564. [PubMed] [Google Scholar]
- Reichstein DA, Recchia FM. Coats disease and exudative retinopathy. International Ophthalmology Clinics. 2011;51:93–112. doi: 10.1097/IIO.0b013e318200de51. [DOI] [PubMed] [Google Scholar]
- Reynolds JD. Retinopathy of prematurity. International Ophthalmology Clinics. 2010;50:1–13. doi: 10.1097/IIO.0b013e3181f12ffd. [DOI] [PubMed] [Google Scholar]
- Russell HC, McDougall V, Dutton GN. Congenital cataract. British Medical Journal. 2011;342:d3075. doi: 10.1136/bmj.d3075. [DOI] [PubMed] [Google Scholar]
- Shastry BS. Persistent hyperplastic primary vitreous: Congenital malformation of the eye. Clinical and Experimental Ophthalmology. 2009;37:884–890. doi: 10.1111/j.1442-9071.2009.02150.x. [DOI] [PubMed] [Google Scholar]
- Vahedi A, Lumbroso-Le RL, Levy GC, Doz F, Aerts I, Desjardins L. Differential diagnosis of retinoblastoma: a retrospective study of 486 cases. Journal Francais d’Ophtalmologie. 2008;31:165–172. doi: 10.1016/s0181-5512(08)70349-8. [DOI] [PubMed] [Google Scholar]
- Yang LL, Lambert SR, Drews-Botsch C, Stulting RD. Long-term visual outcome of penetrating keratoplasty in infants and children with Peters anomaly. Journal of AAPOS. 2009;13:175–180. doi: 10.1016/j.jaapos.2008.10.007. [DOI] [PubMed] [Google Scholar]


