Abstract
Background
Full-field digital mammography (FFDM) has largely replaced screen-film mammography (SFM) for breast cancer screening, but how this affects downstream breast-related use and costs is unknown.
Objectives
To compare breast-related healthcare use and costs among Medicare beneficiaries undergoing SFM versus FFDM from 1999 to 2005.
Design
Retrospective cohort study.
Subjects
Medicare-enrolled women ages 66 and older with mammograms in Breast Cancer Surveillance Consortium registries.
Measures
Subsequent follow-up with additional imaging or breast biopsy within 12 months was ascertained through Medicare claims. Associated mean costs were estimated by screening modality and year, adjusting for confounding factors and clustering within mammography facilities using Generalized Estimating Equations.
Results
Among 138,199 women, 332,324 SFM and 22,407 FFDM mammograms were analyzed. Approximately 6.5% of SFM and 9.0% of FFDM had positive findings. In 2001 subsequent imaging was higher among FFDM versus SFM (127.5 vs. 97.4 follow-up mammography claims per 1000 index mammograms) whereas subsequent biopsy was lower among FFDM versus SFM (19.2 vs. 24.9 per 1000 index mammograms) with differences decreasing over time. From 2001 to 2004, mammography subsequent to FFDM had higher mean costs than SFM ($82.60 vs. $64.31 in 2001). The only cost differences between SFM and FFDM for ultrasound or biopsy were in 2001.
Conclusions
Subsequent breast-related healthcare use differed early in FFDM introduction, but diminished over time with differences attributable to higher recall rates for additional imaging and lower rates of biopsy in those undergoing FFDM vs. SFM. Remaining cost differences are due to higher reimbursement rates for FFDM vs. SFM.
Keywords: Mammography screening, Full Field Digital, Cost, Medicare, work-up, false positive, health services
Introduction
There is little controversy that the best approach for decreasing breast cancer morbidity and mortality among most women includes mammography screening for early detection.1,2 Mammography screening reduces breast cancer mortality by 15%-32% for women aged 40-69.2,3 Comparative effectiveness research (CER) has shown that full field digital mammography (FFDM) is superior to screen film mammography (SFM) in terms of cancer detection in pre- and peri- menopausal women, women less than 50 years and women with dense breasts, but found no overall difference between the modalities.4-6 Among women ages 65 years and older with non-dense breasts the Digital Mammography Imaging Screening Trial (DMIST) reported greater sensitivity of SFM compared to FFDM, though this difference was not statistically significant.7
Despite limited evidence of superior performance, FFDM use has diffused rapidly in the US; it is currently estimated to comprise 79% of all mammography machines8 and FFDM is anticipated to fully replace SFM over time. Currently Medicare reimburses screening SFM and FFDM at average rates of $78 and $129 respectively. The higher cost of FFDM is linked to the cost of purchasing and maintaining the digital machines as well as the increased time it takes to interpret FFDM9 due to computer manipulation time.10
While DMIST reported that FFDM is not cost-effective relative to SFM for women aged 50 years or older,11 the trial was not able to evaluate follow-up care costs between modalities because all women were screened with both modalities. The SFM and FFDM mammograms were interpreted independently by different radiologists and follow-up care was undertaken to pursue screening abnormalities detected with either modality. It is unknown whether downstream breast-related healthcare use and costs vary by initial screening modality (SFM vs. FFDM) once an abnormal finding is reported.
Understanding the downstream health service use following the introduction of digital mammography is an important part of documenting the health and economic impact of the transition to this new technology. Using data from the Breast Cancer Surveillance Consortium (BCSC) and linked Medicare claims data, we examined breast-related healthcare use and costs in the year following screening mammography among women ages 66 years and older over the period 1999 to 2005. We assessed differences in these outcomes when the initial screening modality was SFM compared to FFDM over time and by mammography result.
Methods
Data Sources
The BCSC is a national network of mammography registries organized to assess breast cancer screening practices and outcomes in the U.S.12,13 Data were obtained from four BCSC registries participating in a linkage of BCSC records and Medicare claims data: Carolina Mammography Registry; New Hampshire Mammography Network; San Francisco Mammography Registry; and Vermont Breast Cancer Surveillance System. Registries collected data from community radiology facilities including patient characteristics and clinical information at each mammogram. Radiologists’ assessments and recommendations were based on the American College of Radiology's Breast Imaging Reporting and Data System (BI-RADS®).14 Breast cancer diagnoses and tumor characteristics were obtained by linking BCSC data to hospital-based pathology services, regional Surveillance, Epidemiology, and End Results (SEER) programs, and state tumor registries. Data were pooled at the central Statistical Coordinating Center (SCC). Registries and the SCC received Institutional Review Board approval for active or passive consenting processes or a waiver of consent to enroll participants, link data, and perform analyses. All procedures were Health Insurance Portability and Accountability Act compliant, and registries and the SCC received a Federal Certificate of Confidentiality and other protections for the identities of women, physicians, and facilities.
Women receiving mammograms at one of the four registries participating in the Medicare linkage who were ages 65 and older and enrolled in Medicare between 1998 and 2006 were matched to the Center for Medicare and Medicaid Services’ (CMS) Medicare Program Master Enrollment file by unique identifiers (86.8% match rate). Medicare enrollment information for this period and Medicare claims data from MedPAR, Outpatient, and Carrier files were included in the database.
Participants
Women receiving a screening mammogram (determined by radiologist's indication)13 within the participating registries were included if they were at least age 66 years or older at the time of the screening mammogram, continuously enrolled in fee-for-service Medicare Parts A and B and not enrolled in a Medicare HMO for one year before or after the mammogram, and had no prior history of breast cancer. We limited the study to women at least 66 years of age at the time of screening mammogram and those with two years of continuous Medicare enrollment (one year before and one year after the screening mammogram) in order to ensure complete capture of claims data. We included the 96.5% of BCSC database mammograms with a corresponding Medicare claim within 7 days before or after the exam date recorded in the BCSC database.
Measures and definitions
We used standard BCSC definitions to assign mammogram outcome.13 A mammogram was considered positive if the BI-RADS® assessment following the initial screening mammogram (initial assessment) was: 0 (needs additional imaging evaluation); 4 (suspicious abnormality); 5 (highly suggestive of malignancy); or 3 (probably benign finding) with a recommendation for immediate follow-up. Mammograms were defined as true-positive (TP) or false-negative (FN) if a diagnosis of invasive carcinoma or ductal carcinoma in situ occurred within 1 year after the screening examination or before the next screening mammogram, whichever occurred first.13 Mammograms with no diagnosis of invasive carcinoma or ductal carcinoma in situ within 1 year of the screening mammogram or prior to the next mammogram were classified as false-positive (FP) or true-negative (TN).
Self-reported data on age, race, Hispanic ethnicity, personal history of breast cancer, family history of breast cancer in a first-degree relative, and previous mammography were collected at each mammogram. BI-RADS14 breast density was assigned by the interpreting radiologist.
We examined follow-up services related to the diagnostic work-up of mammograms as: mammography, ultrasound, or breast biopsy/other invasive breast procedure using claims identified on the basis of International Classification of Disease, Ninth Revision (ICD-9) procedure and diagnosis codes, Healthcare Common Procedure Coding System (HCPCS) codes, and diagnosis-related groups (see Table, Supplemental Digital Content 1). We also created a category of any follow-up which included any of the above services. For each follow-up type, we identified the total number of days on which a claim occurred in the Medicare files in the year subsequent to the index screening mammogram. Procedures of multiple types (e.g. mammography and ultrasound) occurring on the same day were counted separately whereas multiple claims for procedures of a single type (e.g. multiple mammography claims) were counted as a single visit. We also identified the number of unique days in which mammography, ultrasound or breast biopsy/other invasive breast procedure appeared in the Medicare files in the year preceding the index screening exam for adjustment purposes.
We calculated Medicare reimbursed amounts for each type of follow-up for the year before (for adjustment purposes) and after the index mammogram. Medicare reimbursement for professional and facility charges were based on the Resource Based Relative Value Scale methodology, which assigns costs on the basis of HCPCS, with regional modifiers to allow for differences in cost of medical care throughout the U.S.15 Inpatient service costs were based on the Diagnosis Related Groups (DRG). Because our goal was to examine the costs to Medicare for breast-related health care use, the analytic perspective taken was that of the Center for Medicare and Medicaid Services (CMS). Medicare pricing was relatively constant over the study time period; hence, due to the similarity between real and nominal dollars to CMS over this period, we report observed payments instead of indexing costs to a single year.
Statistical Analysis
We estimated the distribution of patient- and mammogram-level characteristics by index screening mammogram modality. We computed the count and proportion of screening mammograms with subsequent utilization for each follow-up type, overall and separately by year and modality of the index examination. Among screening mammograms with at least one claim for follow-up breast-related care, we estimated the mean and standard deviation of costs, overall and separately by year and modality of the index examination. These statistics were also computed stratified by TN and FP mammography outcomes. We limited the stratified results to those without a cancer endpoint because of the relatively small number of cancer cases and the difficulty in using claims to determine when diagnostic workup ends and cancer treatment begins. We estimated means rather than medians to allow for extrapolation of our findings to the population level (mean cost x number of women in population = total cost for population). In addition, we calculated and compared the sensitivity and specificity with 95% confidence intervals (95%CI) of SFM and FFDM over time.
We modeled the probability of subsequent breast-related follow-up and the total cost of follow-up by service type (mammography, ultrasound, breast biopsy/other invasive breast procedure, and any follow-up) as a function of modality and year of the index screening exam while adjusting for possible confounding factors and clustering within mammography facilities using Generalized Estimating Equations. Multivariable models were adjusted for age, race/ethnicity, breast density, first degree family history of breast cancer, breast-related use or cost in the prior year, screening interval, and BCSC registry. Cost models were estimated only among women who had any additional costs in the subsequent year and therefore estimate mean cost among women who received subsequent breast-related health care. Models were used to generate standardized estimates of the probability of use and the cost of follow-up in each year subsequent to FFDM and SFM via indirect standardization. Estimates were standardized to the distribution of patient characteristics represented by the total population of index mammograms. We report point estimates and 95% confidence intervals generated by these models.
Analyses were performed using R 2.10.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 332,324 SFM and 22,407 FFDM from 138,199 women from 139 mammography facilities (72 in North Carolina, 33 in New Hampshire, 18 in San Francisco and 16 in Vermont) were performed between 1999 and 2005 (Table 1). BCSC facilities first began performing FFDM in 2001 with 802 (1.6%) screens. By 2005 the number of FFDM screens increased to 8,640 (17.5%). The majority of SFM and FFDM were among white non-Hispanic women and among women ages 66-74 years. The majority of women had no first degree family history of breast cancer and were not using hormone therapy. Most women had scattered fibroglandular breast density. Positive findings were reported for 6.5% of SFM and 9.0% of FFDM. The cancer rate within one year of screening mammogram and prior to the next screening mammogram was 0.7% among SFM and 0.6% among FFDM screens. Due to few cancer events in the FFDM group, comparison of sensitivity between SFM and FFDM is inappropriate. The specificity of SFM and FFDM remained relatively constant during the study period, yet the specificity of FFDM is consistently lower than the specificity of SFM (in 2005 specificity was 91.6% (95%CI: 91.0, 92.2) versus 94.4% (95%CI: 94.1, 94.6) respectively).
Table 1.
Characteristics of the Index Screening Mammograms
| Characteristic | Screen-Film N=332,324 | Digital N=22,407 | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age group, years | ||||
| 66-74 | 193,029 | 58.1 | 13,059 | 58.3 |
| 75-84 | 122,220 | 36.8 | 8,040 | 35.9 |
| 85+ | 17,075 | 5.1 | 1,308 | 5.8 |
| Race/ethnicity | ||||
| White, non-hispanic | 262,332 | 85.8 | 19,151 | 90.4 |
| Black, non-hispanic | 25,900 | 8.5 | 474 | 2.2 |
| Asian | 10,527 | 3.4 | 1,152 | 5.4 |
| Am Indian/Alaska native | 1,490 | 0.5 | 23 | 0.1 |
| Hispanic | 5,481 | 1.8 | 393 | 1.9 |
| Missing | 26,594 | -- | 1,214 | -- |
| Family history of breast cancer | ||||
| Yes | 45,668 | 17.0 | 3,903 | 19.4 |
| No | 222,455 | 83.0 | 16,252 | 80.6 |
| Missing | 64,201 | -- | 2,252 | -- |
| Hormone therapy use | ||||
| Yes | 56,246 | 18.7 | 2,160 | 10.9 |
| No | 243,863 | 81.3 | 17,663 | 89.1 |
| Missing | 32,215 | -- | 2,584 | -- |
| BIRADS breast density | ||||
| 1 – Almost entirely fat | 30,050 | 10.4 | 2,134 | 10.2 |
| 2 – Scattered fibroangular tissue | 163,747 | 56.7 | 10,642 | 51.0 |
| 3 – Heterogenously dense | 86,741 | 30.0 | 7,716 | 37.0 |
| 4 – Extremely dense | 8,497 | 2.9 | 388 | 1.9 |
| Missing | 43,289 | -- | 1,527 | -- |
| Mammogram finding | ||||
| Negative | 310,853 | 93.5 | 20,394 | 91.0 |
| Positive | 21,471 | 6.5 | 2,013 | 9.0 |
| Months since previous mammogram | ||||
| 9-18 | 242,167 | 75.9 | 18,503 | 83.4 |
| 18-30 | 48,223 | 15.1 | 2,276 | 10.3 |
| 31-42 | 14,533 | 4.6 | 685 | 3.1 |
| >42 | 14,034 | 4.4 | 724 | 3.3 |
| Missing | 13,367 | -- | 219 | -- |
| Cancer within 1 year | ||||
| Yes | 2,315 | 0.7 | 139 | 0.6 |
| No | 330,009 | 99.3 | 22,268 | 99.4 |
| Year of mammogram | ||||
| 1999 | 44,055 | 13.3 | -- | -- |
| 2000 | 45,641 | 13.7 | -- | -- |
| 2001 | 49,139 | 14.8 | 802 | 3.6 |
| 2002 | 55,425 | 16.7 | 2,300 | 10.3 |
| 2003 | 51,843 | 15.6 | 4,513 | 20.1 |
| 2004 | 45,378 | 13.7 | 6,152 | 27.5 |
| 2005 | 40,843 | 12.3 | 8,640 | 38.6 |
Of the 49,941 screening mammograms performed in 2001, 9.5% of SFM and 13.7% of FFDM had a subsequent mammogram in the following year, 3.4% of SFM and 7.7% of FFDM had an ultrasound visit, and 2.2% of SFM and 2.2% of FFDM had a breast biopsy/invasive breast procedure (Table 2). Among index screening mammograms with a follow-up mammogram, approximately 97% of initial SFM were followed by SFM and 92% of initial FFDM were followed by FFDM. A higher proportion of FFDM had a subsequent mammogram or ultrasound compared with SFM in all years from 2001 to 2005. There was no difference in the proportion of SFM vs. FFDM with a breast biopsy/invasive procedure in the year after the screening mammogram.
Table 2.
Number of subsequent claims by year, screening modality, and visit type
| Year | Screen Type | Number of Screening Mammograms | Subsequent Visit | |||||
|---|---|---|---|---|---|---|---|---|
| Mammography | Ultrasound | Biopsy | ||||||
| N | % | N | % | N | % | |||
| 1999 | All | 44,055 | 3,945 | 9.0 | 1,164 | 2.6 | 896 | 2.0 |
| 2000 | All | 45,641 | 4,139 | 9.1 | 1,347 | 3.0 | 892 | 2.0 |
| 2001 | All | 49,941 | 4,769 | 9.5 | 1,728 | 3.5 | 1,114 | 2.2 |
| SFM | 49,139 | 4,659 | 9.5 | 1,666 | 3.4 | 1,096 | 2.2 | |
| FFDM | 802 | 110 | 13.7 | 62 | 7.7 | 18 | 2.2 | |
| 2002 | All | 57,725 | 5,630 | 9.8 | 2,130 | 3.7 | 1,395 | 2.4 |
| SFM | 55,425 | 5,337 | 9.6 | 1,998 | 3.6 | 1,349 | 2.4 | |
| FFDM | 2,300 | 293 | 12.7 | 132 | 5.7 | 46 | 2.0 | |
| 2003 | All | 56,356 | 5,116 | 9.1 | 190 | 3.4 | 1,385 | 2.5 |
| SFM | 51,843 | 4,530 | 8.7 | 1,676 | 3.2 | 1,280 | 2.5 | |
| FFDM | 4,513 | 586 | 12.9 | 254 | 5.6 | 116 | 2.6 | |
| 2004 | All | 51,530 | 4,669 | 9.1 | 1,777 | 3.4 | 1,155 | 2.2 |
| SFM | 45,378 | 4,037 | 8.9 | 1,504 | 3.3 | 1,039 | 2.3 | |
| FFDM | 6,152 | 632 | 10.3 | 273 | 4.4 | 105 | 1.7 | |
| 2005 | All | 49,483 | 4,389 | 8.9 | 1,739 | 3.5 | 1,136 | 2.3 |
| SFM | 40,843 | 3,466 | 8.5 | 1,359 | 3.3 | 943 | 2.3 | |
| FFDM | 8,640 | 923 | 10.7 | 380 | 4.4 | 193 | 2.2 | |
SFM= screen-film mammography; FFDM=full field digital mammography
The unadjusted number of subsequent claims (separately for mammography, ultrasound, and breast biopsy) per 1,000 index screening mammograms and the unadjusted mean costs in the following year by calendar year and screening modality are shown in Table 3. In 1999 for every 1,000 screening mammograms performed, Medicare received 107.5 claims for additional mammograms in the subsequent year. The number of claims for subsequent mammography was higher for FFDM compared to SFM from 2001 to 2005 but the gap narrowed over time. Similar patterns were seen for ultrasound claims in the year after initial screening mammography, but not for breast biopsies/other invasive procedures. For women with at least one subsequent mammography claim, the mean number of mammograms in the year following initial SFM and FFDM were similar (1.25 versus 1.27, respectively). In 1999 the mean cost to Medicare of subsequent mammography for SFM was $49.10. The mean cost of subsequent mammography claims increased over time for both SFM and FFDM. In 2001, the mean cost of subsequent mammography in the year following a SFM was $54.00 compared to $65.40 for FFDM. By 2005 the cost of subsequent mammography had increased to $111.60 for SFM and $131.70 for FFDM.
Table 3.
Unadjusted subsequent claims and mean cost (SD) by type of visit, year, and screening modality
| SUBSEQUENT CLAIMS | MEAN COST | |||||||
|---|---|---|---|---|---|---|---|---|
| Year | SFM | FFDM | SFM | FFDM | ||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| MAMMOGRAPHY | ||||||||
| 1999 | 107.5 | 369.2 | -- | 49.1 | 55.7 | -- | ||
| 2000 | 110.5 | 379.5 | -- | 49.8 | 53.0 | -- | ||
| 2001 | 118.3 | 400.3 | 175.8 | 477.0 | 54.0 | 57.2 | 65.4 | 50.5 |
| 2002 | 122.3 | 411.5 | 157.0 | 440.6 | 67.9 | 105.7 | 88.1 | 63.2 |
| 2003 | 111.8 | 397.2 | 163.8 | 466.0 | 79.2 | 105.4 | 100.1 | 82.3 |
| 2004 | 112.8 | 395.2 | 128.6 | 413.0 | 97.3 | 114.2 | 114.4 | 97.9 |
| 2005 | 107.9 | 389.4 | 138.2 | 440.3 | 111.6 | 127.8 | 131.7 | 120.7 |
| ULTRASOUND | ||||||||
| 1999 | 29.6 | 190.9 | -- | 15.6 | 38.4 | -- | ||
| 2000 | 32.8 | 198.0 | -- | 17.4 | 39.6 | -- | ||
| 2001 | 38.8 | 220.3 | 84.8 | 304.4 | 20.0 | 45.9 | 25.8 | 42.0 |
| 2002 | 41.7 | 230.1 | 71.7 | 317.1 | 21.2 | 45.7 | 22.2 | 50.7 |
| 2003 | 38.3 | 228.1 | 70.2 | 317.5 | 22.4 | 51.9 | 24.6 | 57.8 |
| 2004 | 38.1 | 220.3 | 52.5 | 262.6 | 24.7 | 53.1 | 26.3 | 58.4 |
| 2005 | 38.2 | 219.6 | 52.7 | 266.8 | 27.8 | 99.2 | 28.8 | 56.9 |
| BIOPSY | ||||||||
| 1999 | 25.8 | 194.9 | -- | 96.9 | 321.2 | -- | ||
| 2000 | 25.2 | 194.8 | -- | 98.7 | 333.2 | -- | ||
| 2001 | 28.9 | 208.9 | 27.4 | 191.6 | 114.2 | 431.7 | 37.24 | 129.1 |
| 2002 | 32.7 | 227.1 | 27.0 | 204.7 | 157.9 | 589.0 | 97.84 | 568.3 |
| 2003 | 32.0 | 219.3 | 31.2 | 223.1 | 184.8 | 599.0 | 87.45 | 297.7 |
| 2004 | 29.3 | 209.8 | 23.9 | 182.8 | 161.9 | 507.4 | 79.91 | 261.8 |
| 2005 | 29.6 | 209.4 | 27.0 | 189.0 | 152.5 | 494.5 | 90.43 | 269.5 |
| ANY Follow-Up | ||||||||
| 1999 | 162.8 | 567.7 | -- | 161.6 | 341.4 | -- | ||
| 2000 | 168.5 | 589.4 | -- | 165.9 | 355.5 | -- | ||
| 2001 | 186.0 | 641.7 | 288.0 | 772.9 | 188.3 | 456.3 | 128.4 | 152.3 |
| 2002 | 196.7 | 671.1 | 255.7 | 737.9 | 247.0 | 651.3 | 208.1 | 591.9 |
| 2003 | 182.1 | 659.2 | 265.2 | 808.5 | 286.4 | 659.6 | 212.2 | 339.3 |
| 2004 | 180.2 | 645.3 | 205.0 | 689.3 | 283.9 | 570.7 | 220.6 | 314.2 |
| 2005 | 175.7 | 644.2 | 217.8 | 710.4 | 291.9 | 571.5 | 250.9 | 347.5 |
SFM = screen-film mammography; FFDM = full field digital mammography; SD standard deviation
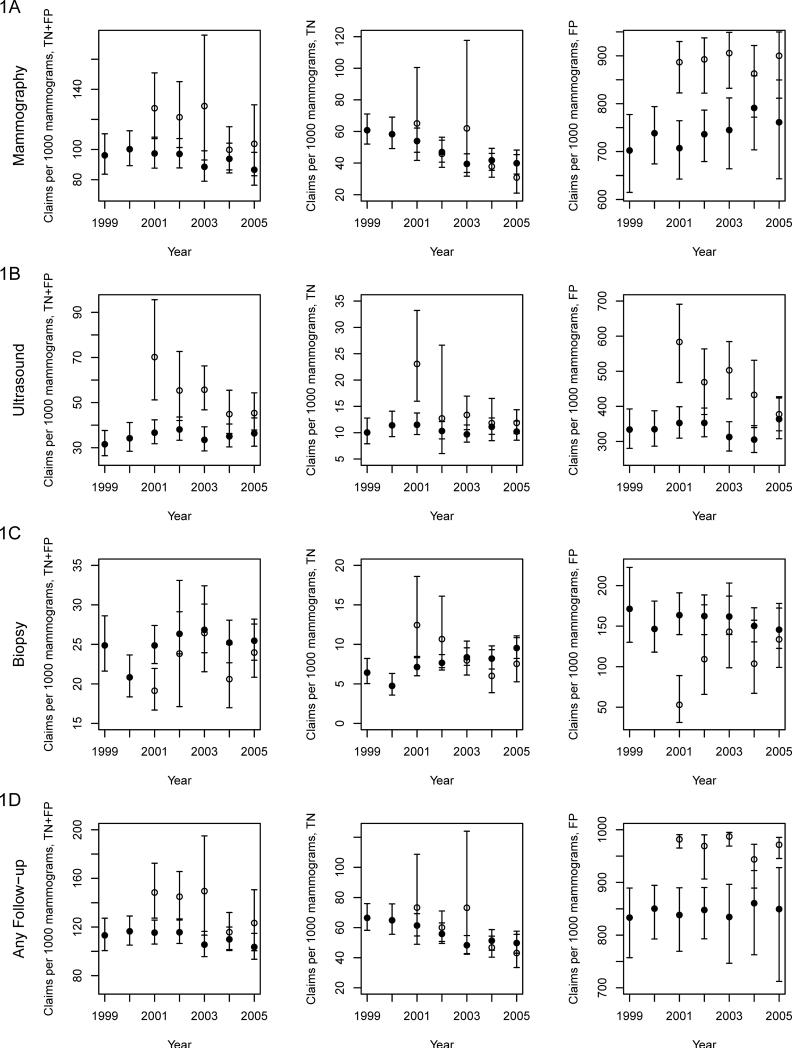
The adjusted number of screening mammograms with subsequent mammography was significantly higher for FFDM compared to SFM in 2001-2003 (p = 0.009, 0.03, and 0.03, respectively) (Figure 1A). No difference was observed in rates of subsequent mammography use between SFM and FFDM among women with TN index mammograms. However, among women with FP index mammograms, significant differences were observed across most years (p <0.05 for all years except 2004). Significantly more FFDM index mammograms received subsequent ultrasound compared to SFM in 2001-2003 (Figure 1B). The adjusted number of subsequent ultrasound claims decreased in 2002 for FFDM and by 2005 there was no difference between FFDM and SFM. For breast biopsies/other invasive procedures, the adjusted number of claims were significantly lower both overall and among TN and FP index mammograms for FFDM compared to SFM in 2001 (p < 0.05). No significant differences were observed in other years (Figure 1C). Patterns of adjusted subsequent use for any follow-up are similar to those observed for subsequent mammography because the majority of follow-up involved use of subsequent mammography (Figure 1D).
Figure 1.
Trends in the adjusted number of women with subsequent claims (separately for mammography (1A), ultrasound (1B), and breast biopsy (1C) and a combined total for any breast-related follow-up (1D)) per 1000 index mammograms, by mammogram result (true positive + false positive (TN+FP), TN, and FP) and screening modality. Full field digital mammography is indicated with white circles and screen film mammography is indicated with black circles.
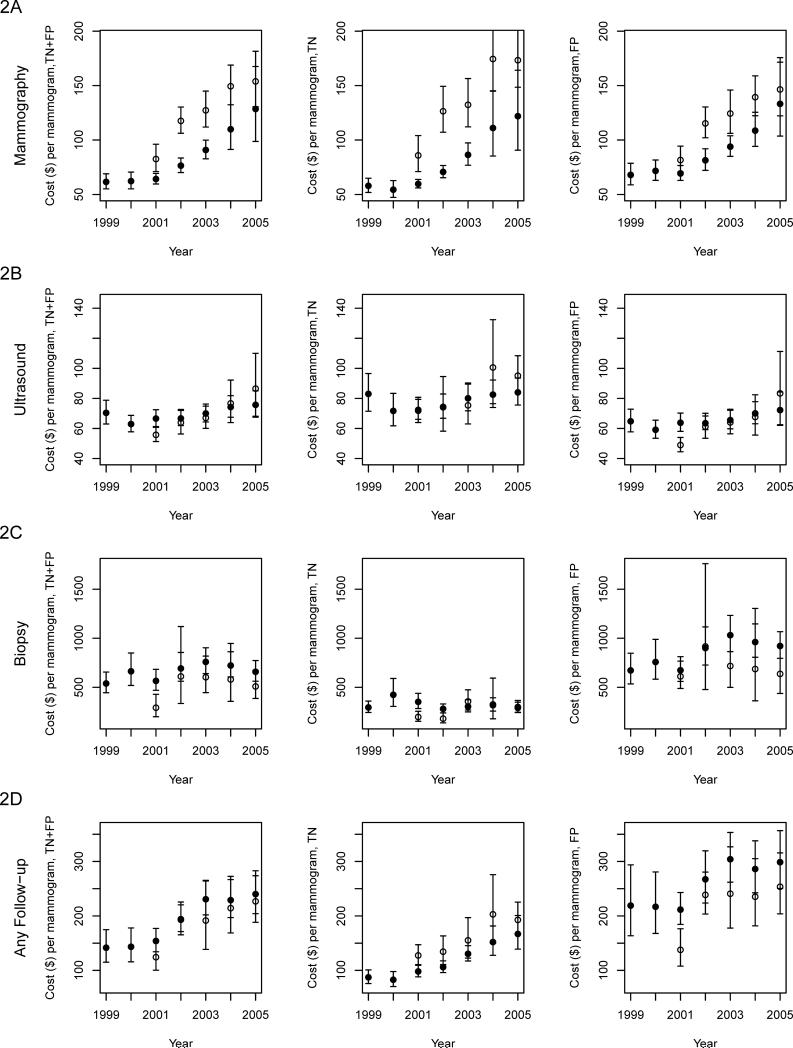
In adjusted analyses, the costs of subsequent mammography were higher among FFDM compared to SFM in 2001-2004. of modality, the costs increased over time (Figure 2A). Among women with subsequent ultrasound, costs differed significantly by screening modality only in 2001 ($66.65 for SFM vs. $55.81 for FFDM, p <0.0001) (Figure 2B). For women receiving follow-up biopsies/invasive breast procedures, differences in cost by screening modality were evident in 2001 ($566.47 for SFM vs. $292.64 for FFDM, p=0.002), and among women with TN results in 2001 and 2002 (Figure 2C). The costs of any follow-up were higher for FFDM versus SFM among women with a TN result in 2001 and 2002 but were lower for FFDM versus SFM among women with a FP result in 2001 (Figure 2D).
Figure 2.
Trends in the adjusted subsequent costs (separately for mammography (2A), ultrasound (2B), and breast biopsy (2C), and a combined total for any breast-related follow-up (2D)) per index mammogram with non-zero subsequent costs, by mammogram result (true positive + false positive (TN+FP), TN, and FP) and screening modality. Full field digital mammography is indicated with white circles and screen film mammography is indicated with black circles.
Discussion
Downstream mammography and ultrasound use in the year after a screening mammogram was more common among FFDM versus SFM in the year when FFDM first became available (2001), with differences decreasing over time after the initial introduction of FFDM. Increases in subsequent mammography and ultrasound following FFDM versus SFM were observed among women with FP mammograms, suggesting that differences in utilization were not only attributable to higher recall rates in the early years of FFDM but represent increased use of imaging among recalled women whose index modality was FFDM. These differences in the early years of FFDM decrease over time, which may indicate a learning curve associated with diffusion of new technology.16 Our analysis did not address the timing of transition to FFDM within each facility, but focused instead on overall trends in use of breast-related services and costs following mammography screening over years when FFDM became increasingly available.
Two previous studies from Norway suggest there is an important learning curve for FFDM. The Oslo I trial17 found higher recall rates with FFDM versus SFM (12% vs. 7%) and the Oslo II trial18 found higher cancer detection rates with FFDM compared to SFM. In these prior studies, the authors speculated that the higher recall rates seen with FFDM could be explained by a learning curve effect. In another BCSC study using data from 1996 to 2005, we examined the performance of 231 radiologists on SFM. Radiologists’ interpretations of screening mammograms improved over time with additional residency training and targeted continuing medical education proved beneficial in reducing the number of work-ups for benign lesions.19 We would expect to see a similar learning curve with regard to FFDM as radiologists read more FFDM screens and in fact, this pattern was observed.
Not surprisingly, we report higher follow-up mammography costs over time from 1999 to 2005. We found that higher costs of subsequent mammography for FFDM were partly attributable to a higher proportion of FFDM being followed up with additional FFDM while SFM tended to be followed by SFM. Since FFDM has a higher reimbursement rate than SFM, the conversion to FFDM is increasing not just the initial screening mammogram cost, but also the overall costs associated with screening. Higher healthcare costs were associated with downstream mammography for FFDM compared to SFM from 2001 to 2005, but not higher costs for ultrasound and breast biopsies or other invasive procedures. Higher downstream costs associated with FFDM could not be attributed to receipt of more mammography among those with FFDM since the mean number of mammograms in the year following initial SFM and FFDM were similar.
Increases in downstream healthcare use and cost among FP mammograms relative to TN mammograms were expected since abnormal mammogram screening results are followed with additional imaging (diagnostic mammogram, targeted breast ultrasound, or breast MRI)20,21 or breast biopsy/procedure. A 2010 study examining breast-related care costs in the year after a FP screening mammogram among women ages 40-80 years enrolled in an HMO in Washington state found breast-related healthcare costs following a FP mammogram were approximately $500 more than for TN mammograms.22 The DMIST also reported increased costs of subsequent breast-related care among FP and TP mammograms but DMIST was unable to examine differences by modality since all women had both SFM and FFDM.11 Our finding that diagnostic mammograms are done using the same modality as the screening mammogram in the vast majority of cases, supports this assumption made in the DMIST cost-effectiveness analysis.
Our study used Medicare administrative data that rely on billing codes to identify subsequent breast-related healthcare use; thus, it is possible that we might not capture all follow-up visits. There is no reason to believe that there was differential ascertainment of healthcare use for women receiving SFM versus FFDM, so our results are not biased with respect to differences in relative health care use related to screening modality. Trends and patterns in subsequent breast-related healthcare use and cost might be different among women younger than 66 years or among women with private health insurance. There were a small number of FFDM exams in 2001 but this number increased substantially during the five year study period.
The use and costs of downstream breast imaging increased substantially over time, with some of the observed increases in cost attributable to greater use of FFDM which is reimbursed at a higher rate than SFM. The ability to measure the downstream burden on the healthcare system following the diffusion of new technology is an important element in its evaluation over and above performance characteristics. These long-term effects (subsequent use and cost of health services) need to be quantified if they are going to be considered in CER aimed at understanding the implications of implementing new technology. In the case of FFDM, adoption is inevitable given the persistent increase in facilities with certified FFDM units, currently representing 80% of mammography facilities and 82% of all mammography units.23 Our study documents that early in the transition period, FFDM had higher downstream costs than SFM and that these were largely due to the higher reimbursement rate for FFDM compared with SFM.
Using digital mammography as a case study, we have shown how registry and administrative claims data may be used to examine the resource use and cost consequences of adopting a new screening modality. Our approach of combining registry and claims data may serve as a paradigm for assessing the real-life consequences of new screening technology adoption and diffusion. With the advent of new effective advanced imaging technologies for screening (e.g. spiral CT and lung cancer) it is important to consider claims-based analyses to uncover downstream cost consequences of technology adopotion.
Supplementary Material
Acknowledgments
Funding Source: This project was supported by the National Cancer Institute–funded Breast Cancer Surveillance Consortium cooperative agreement (grants U01CA63740, U01CA86076, U01CA86082, U01CA63736, U01CA70013, U01CA69976, U01CA63731, U01CA70040, HHSN261201100031C) and the National Cancer Institute–funded grant RC2CA148577. The collection of cancer data used in this study was supported in part by several state public health departments and cancer registries throughout the U.S. For a full description of these sources, please see: http://breastscreening.cancer.gov/work/acknowledgement.html. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cokkinides VBP, Siegel R, Ward EM, Thun MJ. Cancer Prevention and Early Detection: Facts & Figures 2008. American Cancer Society; Atlanta, GA: 2007. [Google Scholar]
- 2.Nelson HD, Fu R, Griffin JC, Nygren P, Smith ME, Humphrey L. Systematic review: comparative effectiveness of medications to reduce risk for primary breast cancer. Ann Intern Med. 2009 Nov 17;151(10):703–715. W-226–735. doi: 10.7326/0003-4819-151-10-200911170-00147. [DOI] [PubMed] [Google Scholar]
- 3.Nelson HDTK, Naik A, et al. Screening for Breast Cancer: Systematic Evidence Review Update for the U.S. Preventive Services Task Force. Evidence Review Update No. 74. Agency for Healthcare Research and Quality; Rockville, MD: 2009. [PubMed] [Google Scholar]
- 4.Berman CG. Recent advances in breast-specific imaging. Cancer Control. 2007 Oct;14(4):338–349. doi: 10.1177/107327480701400404. [DOI] [PubMed] [Google Scholar]
- 5.Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005 Oct 27;353(17):1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 6.Kerlikowske K, Hubbard RA, Miglioretti DL, et al. Comparative Effectiveness of Digital Versus Film-Screen Mammography in Community Practice in the United States: A Cohort Study. Ann Intern Med. 2011 Oct 18;155(8):493–502. doi: 10.7326/0003-4819-155-8-201110180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pisano ED, Hendrick RE, Yaffe MJ, et al. Diagnostic accuracy of digital versus film mammography: exploratory analysis of selected population subgroups in DMIST. Radiology. 2008 Feb;246(2):376–383. doi: 10.1148/radiol.2461070200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Food and Drug Administration [September 7, 2011];Mammography Quality Standards Act and Program. 2011 http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/default.htm.
- 9.Haygood TM, Wang J, Atkinson EN, et al. Timed efficiency of interpretation of digital and film-screen screening mammograms. AJR Am J Roentgenol. 2009 Jan;192(1):216–220. doi: 10.2214/AJR.07.3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haygood TM, Wang J, Lane D, et al. Why does it take longer to read digital than film-screen screening mammograms? A partial explanation. J Digit Imaging. 2010 Apr;23(2):170–180. doi: 10.1007/s10278-009-9177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tosteson AN, Stout NK, Fryback DG, et al. Cost-effectiveness of digital mammography breast cancer screening. Ann Intern Med. 2008 Jan 1;148(1):1–10. doi: 10.7326/0003-4819-148-1-200801010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR Am J Roentgenol. 1997 Oct;169(4):1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 13.Breast Cancer Surveillance Consortium [August 29, 2011]; http://breastscreening.cancer.gov/.
- 14.Breast Imaging Reporting and Data System (BI-RADS) Breast Imaging Atlas. American College of Radiology; Reston, VA: 2003. [Google Scholar]
- 15.Hsiao WC, Braun P, Dunn DL, et al. An overview of the development and refinement of the Resource-Based Relative Value Scale. The foundation for reform of U.S. physician payment. Med Care. 1992 Nov;30(11 Suppl):NS1–12. doi: 10.1097/00005650-199211001-00001. [DOI] [PubMed] [Google Scholar]
- 16.Reiner BI. Optimizing Technology Development and Adoption in Medical Imaging Using the Principles of Innovation Diffusion, Part I: Theoretical, Historical, and Contemporary Considerations. J Digit Imaging. 2011 Jun 28; doi: 10.1007/s10278-011-9397-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skaane P, Young K, Skjennald A. Population-based mammography screening: comparison of screen-film and full-field digital mammography with soft-copy reading--Oslo I study. Radiology. 2003 Dec;229(3):877–884. doi: 10.1148/radiol.2293021171. [DOI] [PubMed] [Google Scholar]
- 18.Skaane P, Skjennald A. Screen-film mammography versus full-field digital mammography with soft-copy reading: randomized trial in a population-based screening program--the Oslo II Study. Radiology. 2004 Jul;232(1):197–204. doi: 10.1148/radiol.2321031624. [DOI] [PubMed] [Google Scholar]
- 19.Miglioretti DL, Gard CC, Carney PA, et al. When radiologists perform best: the learning curve in screening mammogram interpretation. Radiology. 2009 Dec;253(3):632–640. doi: 10.1148/radiol.2533090070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flobbe K, Bosch AM, Kessels AG, et al. The additional diagnostic value of ultrasonography in the diagnosis of breast cancer. Arch Intern Med. 2003 May 26;163(10):1194–1199. doi: 10.1001/archinte.163.10.1194. [DOI] [PubMed] [Google Scholar]
- 21.Bedrosian I, Bedi D, Kuerer HM, et al. Impact of clinicopathological factors on sensitivity of axillary ultrasonography in the detection of axillary nodal metastases in patients with breast cancer. Ann Surg Oncol. 2003 Nov;10(9):1025–1030. doi: 10.1245/aso.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Chubak J, Boudreau DM, Fishman PA, Elmore JG. Cost of breast-related care in the year following false positive screening mammograms. Med Care. 2010 Sep;48(9):815–820. doi: 10.1097/MLR.0b013e3181e57918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Food and Drug Administration [November 28, 2011];Mammography Quality Standards Act and Program (MQSA) National Statistics. 2011 http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/FacilityScoreca rd/ucm113858.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.