Abstract
This study compares HIV-affected families and their non-HIV-affected neighbors’ behavioral health outcomes and family conflict. To compare two groups from the same neighborhoods at four points over 18 months, mothers with HIV (MLH) (N=167) and their school-age children (age 6 to 20) were recruited from clinical care settings in Los Angeles, CA and neighborhood control mothers (NCM) without HIV (N=204) were recruited from modal neighborhoods. In addition, children living at home who were 12 years and older were recruited. We assessed parenting behaviors, family conflict, mental health, sexual behavior, substance use, and HIV-related health behaviors over time. MLH perceived greater economic insecurity at baseline, less employment, and involvement in romantic relationships. MLH reported more emotional distress and substance use than NCM. MLH, however, reported lowered HIV transmission risk. The random regressions indicated that MLH exhibited higher levels and became significantly less depressed and less anxious over time than their non-HIV-affected neighbors. MLH also reported less initial family violence and conflict reasoning than NCM; violence decreased and conflict increased over time for MLH relative to NCM. Children of MLH decreased their marijuana use but hard drug users of MLH increased their risk, over time, compared to children of NCM. Moreover, children of MLH reported more internalizing behaviors than children of NCM. Even when compared to other families living in the same economically disadvantaged communities, MLH and their children continue to face challenges surrounding family conflict, and key behavioral health outcomes, especially with respect to substance use and mental health outcomes. These families, however, show much resilience and MLH report lowered levels of HIV transmission risk, their children report no greater levels of HIV transmission risk and levels of family violence were lower than reported by families in the same neighborhoods.
Keywords: HIV+ Mothers, Family interventions, Parenting behaviors, Sexual behavior, substance abuse
Introduction
The challenges facing Mothers Living with HIV (MLH) have changed dramatically over the last 20 years. Anti-retroviral medications (ARV) improve both the quality and the length of life for MLH (Vittinghoff et al., 1999). The course of the disease has changed substantially. MLH must still manage health and mental health stressors related to HIV, stop sex and drug use acts that potentially transmit HIV, and adhere to multiple medical regimens. Yet, these challenges are similar to other chronic diseases (Simms, Higginson, & Harding, 2012; Anderson, 2012).
HIV is concentrated among ethnic minority neighborhoods in America’s urban inner cities, particularly African-American and Latino. In these neighborhoods, poverty and discrimination heighten stress, potentially exacerbating the consequences of HIV (Brackis-Cott, Mellins, Dolezal, & Spiefel, 2007). However, the course of the disease has changed so substantially that the impact of HIV may be comparable to a range of other stressors experienced by non-HIV affected mothers in the same neighborhoods.
We hypothesized that MLH and their children may experience more stressors than their neighbors not living with HIV. Mothers living with HIV continue to experience many challenges in making decisions about disclosure, sexual relationships, coping with stigma, and parenting while ill (Armistead et al., 2001; Cederbaum, 2011; Ciesla & Roberts, 2001; Morrison et al., 2002; Richardson et al., 2001; Remien et al., 2006; Yi et al., 2006). Their children also face considerable stress, including living with their mother’s and their own substance abuse, behavior problems (including early sexual debut), and children were less likely to successfully achieve developmental milestones (Lee, Lester, & Rotheram-Borus, 2002; Mellins, Brackis-Cott, Dolezal, & Meyer-Bahlburg, 2005; Murphy, Marelich, & Hoffman, 2002; Rotheram-Borus, Lee, Gwadz, & Draimin, 2001; Forehand et al., 2002; Lester et al., 2006; Pilowsky, Zybert, Hsieh, Vlahov, & Susser, 2003; O’Sullivan, Dolezal, Brackis-Cott, Traeger, & Mellins, 2005; Jones, Foster, Zalot, Chester, & King, 2007). The advances and consistent funding obtained for HIV may have decreased these problems for U.S. families, making HIV not the greatest challenge they face (Gunrung, Taylor, Kemeny, & Myers, 2004). This paper aims to evaluate the adjustment of MLH and their children compared to families not affected by HIV who live in similar neighborhoods to assess the behavioral health and family dynamics of MLH and their children over time to assess the continuing burden of living with HIV.
Methods
Institutional Review Board approval was obtained from all clinics used as recruitment sites and voluntary informed consent was obtained from all MLH and their children. Two groups of mothers aged 21 to 69 years were recruited from the same neighborhoods in Los Angeles County between January 2005 and October 2006: 1) MLH and their school-age children, and 2) mothers without HIV and their school-age children.
MLH were recruited after being approached in clinic waiting rooms (n=7 medical settings), being referred by providers or peers to study staff, approaching members of the study staff after presentations to support groups, or after reading promotional posters/flyers posted at participating agencies. Referring healthcare providers secured consent to contact potential participants.
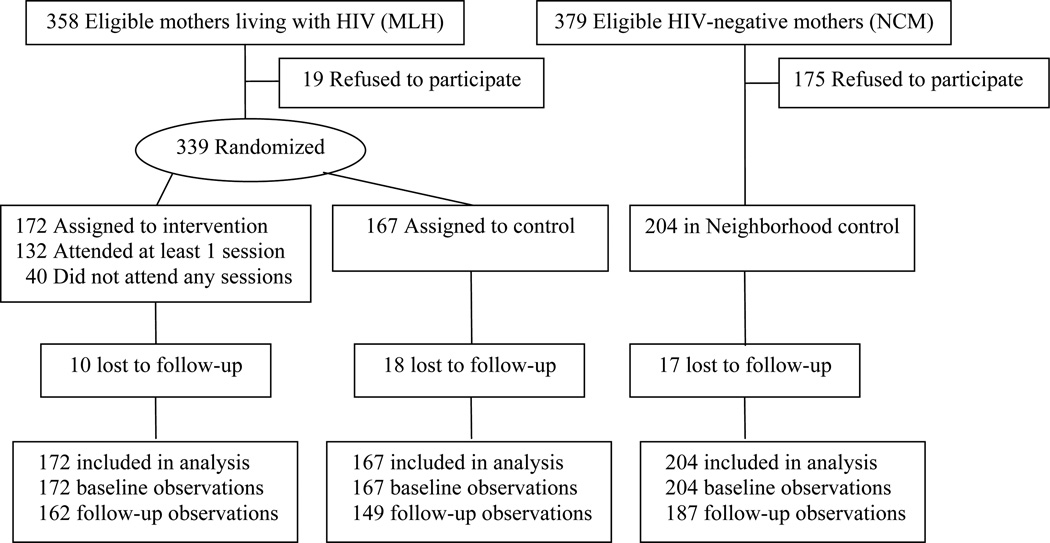
MLH were eligible for recruitment if they were mothers or primary female caregivers of at least one child between the age of 6 and 20 years and were enrolled in HIV-related clinical care. Of the 358 eligible MLH (Figure 1), 94% completed the baseline interview (n=339) (refusal rate: 6%). Only children over the age of 12 were invited to participate in the study, and 259 of their school-age children, aged 12 to 20 years, were enrolled. In prior work, we discussed in detail the challenges and lessons learned in recruiting MLH into behavioral interventions in Los Angeles (Rice, et al., 2009).
FIGURE 1.
Study Randomization Design & Participant Flow.
Randomization was conducted immediately following the baseline interview by telephoning a central data coordinator. In this article, we only included the MLH and their children who were randomized to the control condition (n=167 MLH; n=120 children). We have previously reported on the efficacy of the randomized controlled trial (RCT) in which the MLH participated (Rotheram-Borus et al., 2012).
As depicted in Table 1, the MLH who were recruited from clinical settings were primarily women of color, living in low income neighborhoods, who were struggling financially. In order to create an appropriate case-control group of women, the neighborhood control mothers (NCM) were recruited using street-intercept surveys. After 25% of the MLH sample was recruited, their addresses were mapped. Based on MLH address clustering, five modal neighborhoods were identified (Lester et al., 2010). Neighborhoods varied in ethnicity and socioeconomic status, based on census data. In these neighborhoods, screening and recruitment were conducted by systematically approaching women who did not appear elderly as they entered or left the grocery store. Women were asked whether they were over 18 years of age and a caretaker of at least one child between the ages of 6 and 20 years old. All eligible women were invited to participate in the study (n=379), yielding a baseline sample of 204 NCM who were assessed (refusal rate: 54%). Again, only children 12 years or older were invited to participate, and 160 of children aged 12 to 20 years did so. Thirteen children aged 14 to 19 from 6 NCM were enrolled in the study without their mother’s participation, but with parental consent. No NCM self-identified as HIV-positive.
TABLE 1.
Characteristics of Mothers Living with HIV (MLH) and Neighborhood Control Mothers (NCM) at Recruitment
| MLH | NCM | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| n = 167 | n = 204 | n = 371 | ||||||
| n | (%) | n | (%) | n | (%) | χ2df or tdfb | ||
| Sociodemographics | ||||||||
| Mean age (SD) | 39.6 | (8.2) | 39.5 | (8.8) | 39.5 | (8.5) | .99369 | |
| Ethnic group | 8.353 | * | ||||||
| Latino | 118 | (70.7) | 116 | (57.7) | 234 | (63.6) | ||
| White | 7 | (4.2) | 6 | (3.0) | 13 | (3.5) | ||
| African American | 39 | (23.4) | 73 | (36.3) | 112 | (30.4) | ||
| Other | 3 | (1.8) | 6 | (3.0) | 9 | (2.4) | ||
| Education | 7.751 | ** | ||||||
| Less than high school | 105 | (63.3) | 99 | (48.8) | 204 | (55.3) | ||
| High school or GED | 61 | (36.7) | 104 | (51.2) | 165 | (44.7) | ||
| Currently employed | 44 | (28.0) | 89 | (47.3) | 133 | (38.6) | 13.471 | ** |
| Financial status | 10.243 | * | ||||||
| Struggling to survive | 40 | (24.0) | 41 | (20.2) | 81 | (21.9) | ||
| Barely paying the bills | 65 | (38.9) | 61 | (30.0) | 126 | (34.1) | ||
| Have necessities | 49 | (29.3) | 64 | (31.5) | 113 | (30.5) | ||
| Comfortable | 13 | (7.8) | 37 | (18.2) | 50 | (13.5) | ||
| Mean number of children (SD) | 3.3 | (1.9) | 3.1 | (1.6) | 3.2 | (1.8) | 1.15368 | |
| Have romantic partner | 83 | (49.7) | 136 | (67.0) | 219 | (59.2) | 11.351 | ** |
| Married to romantic partner | 31 | (37.3) | 74 | (54.4) | 105 | (47.9) | 6.011 | * |
| Number of sexual partners during lifetime | 16.251 | ** | ||||||
| One | 34 | (21.1) | 81 | (41.1) | 105 | (32.1) | ||
| More than one | 127 | (78.9) | 116 | (58.9) | 243 | (67.9) | ||
| Number of sexual partners during past 6 months | 7.442 | * | ||||||
| None | 76 | (47.2) | 86 | (43.7) | 162 | (45.3) | ||
| One partner; protected sex only | 53 | (32.9) | 48 | (24.4) | 101 | (28.2) | ||
| One partner / unprotected discordant sexa | 32 | (19.9) | 63 | (32.0) | 95 | (26.6) | ||
| Mean number of unprotected discordant actsa | 1.0 | (3.6) | 10.1 | (40.7) | 6.0 | (30.6) | Wilcoxon | ** |
| Substance use | ||||||||
| Lifetime rates | ||||||||
| Alcohol | 98 | (60.1) | 125 | (63.1) | 223 | (61.8) | .341 | |
| Marijuana | 45 | (27.6) | 40 | (20.2) | 85 | (23.5) | 2.721 | |
| Hard drugs | 66 | (40.5) | 39 | (19.7) | 105 | (29.1) | 18.741 | ** |
| Rates during past 6 months | ||||||||
| Alcohol | 44 | (26.8) | 66 | (33.0) | 110 | (30.2) | 1.631 | |
| Marijuana | 14 | (8.5) | 7 | (3.5) | 21 | (5.8) | 4.201 | * |
| Hard drugs | 31 | (18.9) | 15 | (7.5) | 46 | (12.6) | 10.611 | ** |
| Number of days using during past 3 months | ||||||||
| Alcohol | 2.1 | (8.4) | 2.6 | (10.4) | 2.4 | (9.5) | Wilcoxon | |
| Marijuana | 2.9 | (14.4) | 1.0 | (9.0) | 1.8 | (11.8) | Wilcoxon | * |
| Hard drugs | 4.9 | (18.5) | 0.8 | (6.6) | 2.7 | (13.5) | Wilcoxon | ** |
| General health | ||||||||
| Have health insurance | 87 | (52.1) | 116 | (57.1) | 203 | (54.9) | .941 | |
| Mean number of visits to doctor during | ||||||||
| past year (SD) | 8.7 | (7.4) | 4.0 | (5.5) | 6.1 | (6.9) | Wilcoxon | ** |
| Mean percent of missed visits (SD) | 0.1 | (0.2) | 0.1 | (0.2) | 0.1 | (0.2) | Wilcoxon | ** |
| 100% Adherence to antiretrovirals | 95 | (72.5) | 95 | (72.5) | ||||
| Undetectable viral load | 97 | (63.4) | 97 | (63.4) | ||||
| Mental health, mean (SD) | ||||||||
| Higher life expectancy | 37.9 | (6.7) | 43.2 | (7.0) | 40.9 | (7.4) | 7.19347 | ** |
| Brief Symptom Inventory global distress | 0.7 | (0.6) | 0.4 | (0.4) | 0.5 | (0.5) | 6.97367 | ** |
| Family functioning, mean (SD) | ||||||||
| Conflict reasoning | 9.4 | (5.0) | 12.3 | (4.3) | 11.3 | (4.8) | 3.75143 | ** |
| Family cohesion | 7.1 | (2.3) | 5.7 | (1.3) | 6.3 | (2.0) | 7.09361 | ** |
| Expressiveness | 7.2 | (2.0) | 5.9 | (1.1) | 6.5 | (1.7) | 7.54361 | ** |
| Locus of control | 7.6 | (2.0) | 8.5 | (1.2) | 8.1 | (1.7) | 5.42357 | ** |
| Democratic style | 7.3 | (2.0) | 6.4 | (1.1) | 6.8 | (1.6) | 5.95361 | ** |
| Laissez-faire style | 7.6 | (1.7) | 8.5 | (1.2) | 8.1 | (1.5) | 5.30360 | ** |
| CBCL t-scores, mean (SD) | ||||||||
| Internalizing | 52.2 | (10.4) | 50.8 | (10.6) | 51.2 | (10.5) | .77159 | |
| Externalizing | 52.2 | (11.8) | 50.4 | (10.6) | 50.9 | (10.9) | .95162 | |
Abbreviations: χ2, chi-square statistic; t, t test statistic; Wilcoxon, Wilcoxon two-sample test; df, degrees of freedom.
Discordant partner has opposite HIV serostatus as mother in the study or serostatus was unknown.
Test statistics shown for comparison between MLH and neighborhood control.
P< 0.05;
P< 0.01
Retention
Most mothers (67%) and their adolescents (66%) were assessed across all four time points. Follow-up rates for mothers were 84% at 6 months, 81% at 12 months, and 75% at 18 months. The percentage of mothers with at least one follow-up (91%) and mothers lost to follow up (9%) did not significantly differ between the MLH and NCM cohorts. There were few differences between those lost to follow up and those retained except for two characteristics. MLH without a follow-up assessment were more likely to be African American versus reporting another ethnicity (56% versus 19%; Fisher’s Exact test, p < .01) and more likely to report financially struggling versus barely paying bills, having the necessities, or being comfortable (56% versus 20%, Fisher’s Exact test, p < .01). Differences on being African American vs. reporting another ethnicity (41% vs. 35%) and struggling to survive vs. barely paying the bills (24% vs. 20%) were not statistically significant.
Assessment Procedures
Using laptop computers, an ethnically diverse team of interviewers administered audio computer-assisted self-interviews to collect information from participants. Interviewer training included research ethics, emergency crisis protocols, intensive review of assessment protocols, and mock interviews. Quality assurance interviews were conducted initially with 20% of audio-taped interviews, which decreased to 10% over time. Interviewers met or exceeded expectations on 95% of tapes reviewed; remedial training was provided to interviewers when necessary. All participants were paid $30 (US) as an incentive for completing the baseline assessment and an additional $5 for each subsequent assessment. MLH were compensated for transportation costs and child care for the intervention sessions they attended. Adolescents were provided with gifts valuing less than $10 per session.
Measures
Recent events covered behaviors over the past 6 months.
Mothers' Sociodemographics included age, gender, ethnicity, years of education, employment, household members, income per household member, and marital status.
Conflict Tactics Scale, Form A (Strauss, 1979) measured the frequency from never to every time (0–6) of parent conflict with a child using 14 items, including overall conflict, reasoning, verbal aggression, and violence.
Parenting behaviors were assessed on a 30-item Adult Adolescent Parenting Inventory, Form A; (AAPI; Steele, 1970; Steele & Polluck, 1968) with subscales for appropriate expectations (α = 0.56), obedience (α = 0.68), and less role reversal (α = 0.79). Family Functioning (Bloom, 1985) was adapted to consist of 24 statements reflecting themes of cohesion (α =0.86), expressiveness (α = 0.75), conflict (α =0.54), sociability (α = 0.62), an external locus of control (α = 0.72), engagement (α = 0.52), a democratic style (α = 0.65), and laissez-faire style (α = 0.55).
Mental health was assessed by the Brief Symptom Inventory (BSI) (Derogatis, 1993) with scales for anxiety, depression, and a global distress index (all α >0.71). A logarithm to the base 2 transformation is applied after the addition of a small constant to normalize scores.
Sexual behavior was measured through self-reports obtained for the number of lifetime and recent sexual partners. Sero-discordant partners had unknown HIV serostatus or opposite serostatus from that of the mothers in the study.
Substance use as defined by lifetime and recent prevalence of using alcohol, marijuana, and hard drugs (barbiturates, cocaine or crack, hallucinogens, heroin, inhalants, opiates or painkillers) was measured (Wong, et al., 2008). Recent reports of use included the number of days using over the past 90 days grouped as: “never” (0), “used only once” (1), “less than one day a month” (2), “1 to 2 days a month” (3), “3 to 4 days a month” (9), “1 to 2 days a week” (12), “3 to 4 days a week” (36), “5 to 6 days a week” (60), or “every day or almost every day” (90).
Adolescents were assessed with measures similar to mothers: Demographics, Conflict Tactics, Family Functioning, AAPI, and BSI. The Child Behavior Checklist (CBCL) (Achenbach & Rescorla, 2001) was completed by MLH and NCM for children aged 6 to 18 years. Internalizing and externalizing symptom t-scores were calculated across 119 items.
School attendance, grade level, and most recent grade point average (GPA) were self-reported. Multiple problem behaviors (Rotheram-Borus et al., 2001) were summed as the presence (coded as "1") or absence (coded as "0") of recent unprotected sexual intercourse, contact with the criminal justice system, suicide attempts, hard drug use, and lifetime pregnancy.
Statistical Analysis
We calculated the needed sample size (n=200 MLH and NCM) to compare family adjustment measures and HIV-transmission behaviors between MLH in the intervention, control MLH and NCM using RMASS2 software (Hedecker, Gibbon, Waternaux, 1999). We assumed 80% power, a type I error of 0.05 for a two-sided test, 4 repeated measurements from baseline to 18 months at 6-month intervals, and an attrition rate of 5% between follow-ups.
Demographics and background characteristics were compared between MLH and NCM. Chi-square tests were applied to categorical measures and t tests were applied to continuous measures. Mental health symptoms were compared between adolescent boys and girls in the current study and non-patient normative samples using t tests (Derogatis, 1993).
Group analyses examined parent and adolescent outcomes over time using mixed-effect regression models using random intercepts and slopes from baseline to 18 months between MLH and NCM. Covariates included treatment assignment for the HIV-affected samples and time from the baseline assessment; interaction effects were examined for both linear and quadratic effects. Quadratic effects were identified at the time point where the zero slope occurred (-βlinear/2βquadratic) and the slope changed valence.
Linear regressions were applied to continuous outcomes (PROC MIXED) and logistic regressions were applied to binomial outcomes (PROC GLIMMIX). Zero-inflated Poisson models (NLMIXED) were applied to sexual behavior and substance use count data to account for the high proportion of zero counts; results are reported as two outcomes for the probability of engaging in the behavior (e.g. use or no use), and the frequency of engagement among those who engage in the behavior (e.g. frequency of use among users) (Hall, 2000). Random effects were included in the models to account for correlations between nested observations (e.g. repeated observations over time for a MLH). Linear regressions on adolescent outcomes included random intercepts for each adolescent’s mother.
RESULTS
MLH and their children
MLH were predominantly Latino (71%) or African-American (23%), 39 years of age, and had three children (Table 1). Typically, one child’s age was eligible for enrollment (64%; range 1–4). Almost two-thirds of MLH had less than a high school education and most were struggling to survive economically. Only one-third were employed and about half had health insurance.
MLH reported few HIV-transmission acts at baseline: 21% only had one sexual partner during their lifetime. Only 53% were currently sexually active, 20% had unprotected sex with sero-discordant partners, 27% used alcohol, and 19% used hard drugs.
The school-age children of MLH were 15 years old on average; 83% were in school, 17% were employed, and 29% had experienced sexual debut. Adolescents reported few problem behaviors: only 11% reported more than one problem act. On average, adolescents reported fewer mental health symptoms than normative samples of same-age peers at baseline; all comparisons were significantly different (t = −2.08 to −8.09, df = 878 for girls and 1646 for boys, all P< .05) except for female depression (t = −1.90, df = 878, P = 0.06) and anxiety (t = −1.39, df = 878, P = 0.16). Nine percent reported clinically significant internalizing or externalizing symptoms. Among the 40% who had been tested for HIV, 10% were HIV-positive.
Comparison of MLH and NCM at baseline
As shown in Table 1, MLH and NCM were similar in age, their number of children, and having health insurance. However, there were a few important differences between the two conditions. Compared to MLH, NCM were less likely to be Latino, reported higher socioeconomic status, were more likely to have a high school diploma or its equivalent and to be employed (all p<0.05). NCM were also more likely to have a romantic partner and to be married, but more likely to engage in risky sexual behavior compared to MLH (all p<0.05). In addition to what is presented in Table 1 at baseline, MLH not living with a partner were more likely to report “struggling to survive” versus “barely paying bills, having the necessities, or being comfortable” versus MLH living with a partner (32% vs. 10%; Chi-square = 10.51, df = 1, p < .01). This difference was not significant among NCM without and with a partner (21% versus 19%). Recent hard drug use was lower among NCM compared to MLH (7.5% vs. 19%; p<0.01).
Adolescents of NCM and MLH were similar in mean age, ethnicity, gender, employment, multiple problem behaviors, school enrollment, attendance, and grade level (Table 2), as well as numbers of CBCL internalizing and externalizing symptoms (Table 1).
TABLE 2.
Characteristics of Adolescents of Mothers Living with HIV (MLH) and Neighborhood Control Mothers (NCM) at Recruitment.
| MLH | NCM | Total | |||||
|---|---|---|---|---|---|---|---|
| n = 120 | n = 173 | n = 293 | |||||
| n | (%) | n | (%) | n | (%) | χ2df or tdfb | |
| Sociodemographics | |||||||
| Mean age (SD) | 15.0 | (2.5) | 15.3 | (2.4) | 15.2 | (2.4) | 1.20291 |
| Male gender | 47 | (39.2) | 78 | (45.1) | 125 | (42.7) | 1.021 |
| Currently attending school | 99 | (82.5) | 149 | (86.1) | 248 | (84.6) | .721 |
| Currently employed | 20 | (16.7) | 36 | (20.8) | 56 | (19.1) | .791 |
| Sexual behavior | |||||||
| Number of sexual partners during lifetime | .172 | ||||||
| None | 85 | (71.4) | 124 | (71.7) | 209 | (71.6) | |
| One | 11 | (9.2) | 18 | (10.4) | 29 | (9.9) | |
| More than one | 23 | (19.3) | 31 | (17.9) | 54 | (18.5) | |
| Number of sexual partners during past 6 months | 1.112 | ||||||
| None | 91 | (76.5) | 137 | (79.2) | 228 | (78.1) | |
| One partner; protected sex only | 19 | (16.0) | 28 | (16.2) | 47 | (16.1) | |
| One partner / unprotected discordant sexa | 9 | (7.6) | 8 | (4.6) | 17 | (5.8) | |
| Mean unprotected discordant actsa | 0.1 | (0.5) | 0.3 | (3.8) | 0.2 | (2.9) | Wilcoxon |
| Unprotected, discordant acts under | |||||||
| the influence of alcohol | 2 | (1.7) | 1 | (0.6) | 3 | (1.0) | Wilcoxon |
| Substance use | |||||||
| Lifetime rates | |||||||
| Alcohol | 46 | (38.7) | 59 | (34.1) | 105 | (36.0) | .631 |
| Marijuana | 31 | (26.1) | 42 | (24.3) | 73 | (25.0) | .121 |
| Hard drugs | 14 | (11.8) | 17 | (9.8) | 31 | (10.6) | .281 |
| Rates during past 6 months | |||||||
| Alcohol | 32 | (26.9) | 40 | (23.1) | 72 | (24.7) | .541 |
| Marijuana | 20 | (16.8) | 28 | (16.2) | 48 | (16.4) | .021 |
| Hard drugs | 9 | (7.6) | 10 | (5.8) | 19 | (6.5) | .371 |
| Number of days using during past 3 months | |||||||
| Alcohol | 1.8 | (6.8) | 0.9 | (4.9) | 1.3 | (5.8) | Wilcoxon |
| Marijuana | 5.9 | (20.7) | 3.2 | (14.6) | 4.3 | (17.3) | Wilcoxon |
| Hard drugs | 0.7 | (4.0) | 1.1 | (9.8) | .9 | (8.0) | Wilcoxon |
| Contact with the criminal justice system | |||||||
| Lifetime | 7 | (5.8) | 8 | (4.6) | 15 | (5.1) | .211 |
| Past 6 months | 3 | (2.5) | 5 | (2.9) | 8 | (2.7) | .041 |
| Pregnancy | |||||||
| Lifetime | 10 | (8.4) | 14 | (8.1) | 24 | (8.2) | .0091 |
| During the study | 19 | (16.7) | 16 | (10.4) | 35 | (13.1) | 2.271 |
| Suicide attempts, past 6 months | 3 | (2.5) | 2 | (1.2) | 5 | (1.7) | Fisher |
| Brief Symptom Inventory global distress, mean (SD) | .5 | (.4) | .5 | (.4) | .5 | (.4) | .75291 |
Abbreviations: Fisher, Fisher's Exact test was performed; χ2, chi-square statistic; t, ttest statistic; Wilcoxon, Wilcoxon two-sample test; df, degrees of freedom.
Discordant partner has opposite HIV serostatus as adolescent in the study or serostatus is unknown.
Test statistics shown for comparison between MLH and neighborhood control.
Note: None of differences between adolescents of MLH and Neighborhood Control Mothers were significantly different.
Regression results
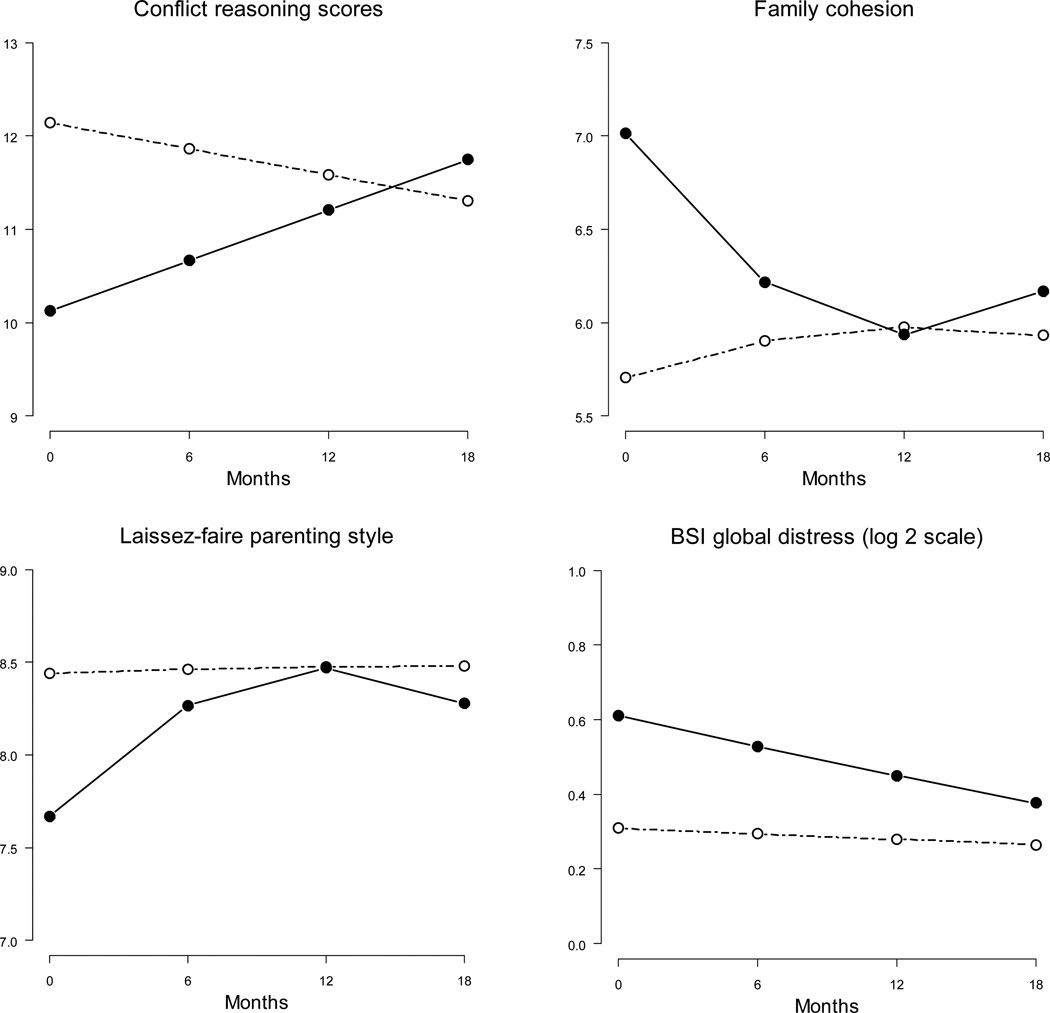
The frequency of parent-child role reversal, appropriate expectations, and empathy were similar on the AAPI across groups. MLH reported lower initial levels of conflict reasoning than NCM (Figure 2; t = −3.08, df = 212, p< 0.01) and less physical violence compared to NCM (t = −2.13, df = 212, p<0.01), but were similar on verbal aggression. At baseline, MLH self-reported higher levels of cohesion and expressiveness on family measures, more social interactions, a more democratic style of parenting, and a higher internal locus of control (t = 4.25 to 8.45, df = 522 to 533, all p< 0.01). MLH reported less conflict compared to NCM (t = −4.14, df = 532, p<0.01). At baseline, MLH’s style of parenting was to remain significantly more engaged during conflict, rather than the disengagement style of NCM (t = 4.02, df = 533, p<0.01).
FIGURE 2.
Plots of Estimated Means over 18 months for Mothers Living with HIV (•) and Neighborhood Control Mothers (ο).
Conflict reasoning, family cohesion, laissez-faire parenting style, and BSI global distress as rated by MLH and NCM mothers over time.
Compared to NCM over time, MLH reported higher levels of conflict reasoning (Figure 2; t = 2.56, df = 212, p=0.01) and lower levels of physical violence (t = −4.21, df = 212, p<0.01); verbal aggression was similar. Compared to the NCM, family cohesion of MLH decreased over 12 months, but then increased for 6 months (Figure 2; linear est. = −0.22, t = −6.93; quadratic est. = 0.0088, t = 5.40, df = 531, both p<0.01). Similar patterns were seen for expressiveness (linear est. = −0.19, t = −7.04; quadratic est. = 0.0070, t = 5.03, df = 531, both p<0.01), an internal locus of control (linear est. = −0.12, t = −4.65; quadratic est. = 0.0043, t = 3.06, df = 522, both p<0.01), and a democratic style (linear est. = −0.17, t = −5.85; quadratic est. = 0.0070, t = 4.73, df = 530, both p<0.01). A mirror image of the outcome trajectories is seen for laissez-faire parenting (Figure 2). Compared to NCM, the MLH increased in laissez-faire parenting until 12 months (linear est. = 0.13, t = 4.70, df = 527, p < 0.01), and decreased in laissez-faire parenting thereafter (quadratic est. = −0.0054, t = −3.76, df = 527, p < 0.001). MLH reported higher levels of conflict (t = 3.16, df = 532, p<0.01) and lower levels of both social interactions (t = −2.47, df = 533, p =0.01) and engagement (t = −2.83, df = 532, p<0.01) over time (not shown). NCM reported significantly fewer mental health symptoms on the logarithmic scale at baseline (all p<0.01); however, symptoms of MLH decreased significantly more over time (t = −4.82 to t = −4.42, df = 549, all p<0.01 for global distress, anxiety, and depression). Log-transformed global distress is shown in Figure 2.
Youth Over Time
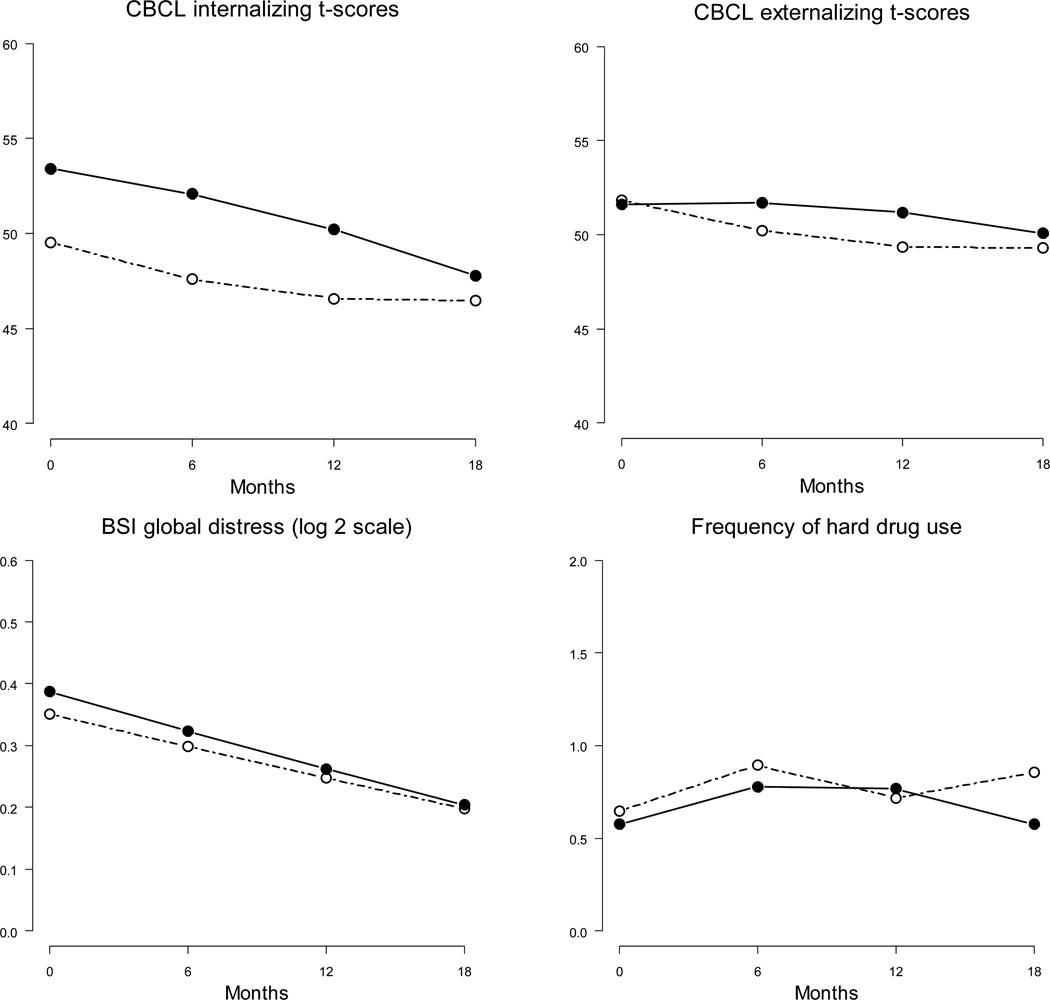
Estimated outcome trajectories are shown for several key outcomes in Figure 3. MLH’s children reported higher overall levels of CBCL internalizing symptoms across time compared to NCM youth (t = 2.11, df = 197, p = .04); MLH and NCM youth did not significantly differ on externalizing symptoms. Reports of CBCL internalizing and externalizing symptoms as reported by mothers did not differ between MLH and NCM. Global distress, anxiety, and depression were similar between MLH and NCM youth. MLH’s children initially increased, then decreased the likelihood of having unprotected sex over time compared to NCM’s children (linear est. = .23, t = 2.20; quadratic est. = −0.011, t = −2.12, df = 689, both p = 0.03). Among marijuana users, MLH youth decreased their frequency of use over time compared to NCM youth (t = −5.41, df = 292, p<0.01). Among hard drug users, MLH’s children increased the frequency of hard drug use over time compared to NCM’s children (t = 2.56, df = 292, p = 0.01). At 18 months, the school drop-out rate was similarly low at 4% across MLH and NCM youth.
FIGURE 3.
Plots of Estimated Means over 18 months for Adolescents by Mothers Living with HIV (•) and Neighborhood Control Mothers (ο).
CBCL t-scores, BSI global distress, and frequency of hard drug use among adolescents of MLH (•) and NCM (ο) over time.
Discussion
Even in an era of effective antiretroviral treatments and access to high quality HIV care in the United States for people living with HIV/AIDS, families living with HIV are burdened by their experience with the disease. Similar to prior work, we found that mothers living with HIV/AIDS face many challenges (Armistead et al., 2001; Cederbaum, 2011; Ciesla & Roberts, 2001; Morrison et al., 2002; Richardson et al., 2001; Remien et al., 2006; Yi et al., 2006). Like other studies, we found that families living with HIV/AIDS continued to struggle compared to non-infected mothers and their children (Murphy, Marelich, Dello Stritto, Swendeman, & Witkin, 2002; Rotheram-Borus et al., 2001; Lester et al., 2010). Our data allows us to examine the behavioral health outcomes of MLH, their adolescent children and how they assess their family dynamics, comparing them to families living in the same communities in Los Angeles.
MLH showed several indications of the stress of living with HIV. Fewer MLH than NCM were employed and reported more financial hardship. These results may be in part due to illness, but also because fewer MLH had romantic partners to whom they were married, and potentially had a smaller household income, while the number of children was similar across conditions. Moreover, MLH reported more emotional distress (declining over time) and lifetime and current substance use than NCM. It is interesting to note that sexual risk was lower among MLH than NCM and that even among MLH there were a large number of women with only one lifetime sex partner.
The largest differences, especially with respect to over time dynamics, between these two groups revolve around issues of family relationships. MLH reported higher levels of cohesion at baseline, but as one can see in Figure 2 those gains were lost over time. MLH reported lower conflict reasoning and less physical violence than NCM at baseline. Over time MLH reported increased levels of conflict and lowered levels of physical violence, social interactions and engagement over time, relative to NCM.
The adolescent children of these two groups of women were remarkably similar in many respects. There were no differences with respect to employment, school attendance, or juvenile justice involvement. Moreover, there were no differences in lifetime substance use, or baseline substance use, although MLH youth increased their use of hard drugs and decreased their use of marijuana over time relative to NCM youth. The most important difference for youth, however, emerged with the CBCL results. MLH youth reported more internalizing behaviors than NCM.
Like any study, there are limitations to this work. First, we lost families over time and, while the number was small, results may be impacted, especially if there is some undetected bias leading to their loss. Second, these data were not drawn from a random sample, because the original intention of the data was as control groups for an intervention. These data were drawn from a clinical sample of MLH enrolled as the control arm of an intervention trial and the neighborhood control consists of a convenience sample recruited outside grocery stores in the modal neighborhoods where the MLH lived. While a random sample would allow us to make larger claims about the general population, these data are still informative.
Even with the limitations presented by our sampling methods, a few important insights can be drawn. While the scope of HIV/AIDS in many countries around the world may outpace that of the United States, families living with HIV/AIDS are still suffering under the burden of their disease. In the United States, HIV/AIDS disproportionately affects women of color who live in poverty. These data remind us that women in those struggling communities have an added struggle with which to contend.
Acknowledgements
This study was supported by grant # R01MH068194 from the National Institute of Mental Health. Dr. Rotheram-Borus had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This work was also supported by the Center for HIV Identification, Prevention, and Treatment (CHIPTS) NIMH grant MH58107; the UCLA Center for AIDS Research (CFAR) grant 5P30AI028697; and the National Center for Advancing Translational Sciences through UCLA CSTI Grant UL1TR000124. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
REFERENCES
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Anderson J. Women and HIV: motherhood and more. Current Opinion in Infectious Diseases. 2012 Feb;25(1):58–65. doi: 10.1097/QCO.0b013e32834ef514. [DOI] [PubMed] [Google Scholar]
- Armistead L, Tannenbaum L, Forehand R, Morse E, Morse P. Disclosing HIV status: are mothers telling their children? Journal of Pediatric Psychology. 2001;26(1):11–20. doi: 10.1093/jpepsy/26.1.11. [DOI] [PubMed] [Google Scholar]
- Bloom BL. A factor analysis of self-report measures of family functioning. Family Processes. 1985;24:225–239. doi: 10.1111/j.1545-5300.1985.00225.x. [DOI] [PubMed] [Google Scholar]
- Brackis-Cott E, Mellins CA, Dolezal C, Spiegel D. The mental health risk of mothers and children: the role of maternal HIV infection. Journal of Early Adolescence. 2007;27(1):67–89. [Google Scholar]
- Cederbaum JA. The experience of sexual risk communication in African American families living with HIV. Journal of Adolescent Research. 2011 doi: 10.1177/0743558411417864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. American Journal of Psychiatry. 2001;158(5):725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. Minneapolis, MN: National Computer Systems, Inc; 1993. [Google Scholar]
- Forehand R, Jones DJ, Kotchick BA, Armistead L, Morse E, Simon Morse P, Stock M. Noninfected children of HIV-infected mothers: a 4-year longitudinal study of child psychosocial adjustment and parenting. Behavior Therapy. 2002;33(4):579–600. [Google Scholar]
- Gurung RAR, Taylor SE, Kemeny M, Myers H. HIV is not my biggest problem: the impact of HIV and chronic burden on depression in women at risk for AIDS. Journal of Social Psychology. 2004;23(4):490–511. [Google Scholar]
- Hall DB. Zero-inflated Poisson and binomial regression with random effects: a case study. Biometrics. 2000;56(4):1030–1039. doi: 10.1111/j.0006-341x.2000.01030.x. [DOI] [PubMed] [Google Scholar]
- Hedeker H, Gibbons R, Waternaux C. Sample size estimation for longitudinal designs with attrition: comparing time-related contrasts between two groups. Journal of Educational and Behavioral Statistics. 1999;24(1):70–93. [Google Scholar]
- Jones DJ, Foster SE, Zalot AA, Chester C, King A. Knowledge of maternal HIV/AIDS and child adjustment: the moderating role of children’s relationships with their mothers. AIDS & Behavior. 2007;11(3):409–420. doi: 10.1007/s10461-006-9188-1. [DOI] [PubMed] [Google Scholar]
- Lee MB, Lester P, Rotheram-Borus MJ. The relationship between adjustment of mothers with HIV and their adolescent daughters. Clinical Child Psychology and Psychiatry. 2002;7(1):71–84. [Google Scholar]
- Lester P, Rotheram-Borus MJ, Lee S-J, Comulada S, Cantwell S, Wu N, Lin YY. Rates and predictors of anxiety and depressive disorders in adolescents of parents with HIV. Vulnerable Children & Youth Studies. 2006;1(1):81–101. [Google Scholar]
- Lester P, Stein JA, Bursch B, Rice E, Green S, Penniman T, Rotheram-Borus MJ. Family-based processes associated with adolescent distress, substance use and risky sexual behavior in families affected by maternal HIV. J Clin Child Adolesc Psychol. 2010;39(3):328–340. doi: 10.1080/15374411003691677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Meyer-Bahlburg HFL. Behavioral risk in early adolescents with HIV+ mothers. Journal of Adolescent Health. 2005;36(4):342–351. doi: 10.1016/j.jadohealth.2004.02.038. [DOI] [PubMed] [Google Scholar]
- Morrison MF, Petitto JM, Ten Have T, Gettes BS, Chiappini RN, Weber AL, Brinker-Spence BS, Bauer RM, Douglas SD, Evans DL. Depressive and anxiety disorders in women with HIV infection. American Journal of Psychiatry. 2002;159(5):789–796. doi: 10.1176/appi.ajp.159.5.789. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Dello Stritto ME, Swendeman D, Witkin A. Mothers living with HIV/AIDS: mental, physical, and family functioning. AIDS Care. 2002;14(5):633–644. doi: 10.1080/0954012021000005461. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D. A longitudinal study of the impact on young children of maternal HIV serostatus disclosure. Journal of Clinical Child and Adolescent Psychology. 2002;7(1):55–70. [Google Scholar]
- O’Sullivan LF, Dolezal C, Brackis-Cott E, Traeger L, Mellins CA. Communication about HIV and risk behaviors among mothers living with HIV and their early adolescent children. Journal of Early Adolescence. 2005;25(2):148–167. [Google Scholar]
- Pilowsky DJ, Zybert PA, Hsieh PW, Vlahov D, Susser E. Children of HIV-positive drug-using parents. Journal of American Acadamy of Child Adolescent Psychiatry. 2003;42(8):950–956. doi: 10.1097/01.CHI.0000046888.27264.17. [DOI] [PubMed] [Google Scholar]
- Remien RM, Exner RH, Kertzner T, Ehrhardt AA, Rotheram-Borus MJ, Johnson MO, Weinhardt LS, Kittel LE, Goldstein RB, Pinto RM, Morin SF, Chesney MA, Lightfoot M, Gore-Felton C, Dodge B, Kelly JA The NIMH Healthy Living Project Team (Ehrhardt, A. A., P. I. NY Site) Depressive symptomatology among HIV-positive women in the era of HAART: a stress and coping model. American Journal of Community Psychology. 2006;38(3–4):275–285. doi: 10.1007/s10464-006-9083-y. [DOI] [PubMed] [Google Scholar]
- Richardson J, Barkan S, Cohen M, Back S, Fitzgerald G, Feldman J, Young M, Palacio H. Experience and covariates of depressive symptoms among a cohort of HIV infected women. Social Work in Health Care. 2001;32(4):93–111. doi: 10.1300/J010v32n04_05. [DOI] [PubMed] [Google Scholar]
- Rice E, Lester P, Flook L, Green S, Valladares E, Rotheram-Borus MJ. Lessons learned from “integrating” intensive family-based interventions into medical care settings for mothers living with HIV/AIDS and their adolescent children. AIDS and Behavior. 2009;13(5):1005–1011. doi: 10.1007/s10461-008-9417-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Lee MB, Gwadz M, Draimin B. An intervention for parents with AIDS and their adolescent children. American Journal of Public Health. 2001;91(8):1294–1302. doi: 10.2105/ajph.91.8.1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Rice E, Comulada WS, Best K, Elia C, Peters K, Valladares E. Intervention outcomes among HIV-affected families over 18 months. AIDS and Behavior. 2012;16:1265–1275. doi: 10.1007/s10461-011-0075-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simms V, Higginson IJ, Harding R. Integration of palliative care throughout HIV disease. The Lancet Infectious Diseases. 2012 Jun 8; doi: 10.1016/S1473-3099(12)70085-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Steele B. Violence in our society. The Pharos. 1970;33:42–48. [Google Scholar]
- Steele BF, Pollock CB. A psychiatric study of parents who abuse infants and small children. In: Kempe CH, Helfer RE, editors. The Battered Child. Chicago, IL: University of Chicago Press; 1968. pp. 89–133. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) scales. Journal of Marriage and Family. 1979;41:75–88. [Google Scholar]
- Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. American Journal of Epidemiology. 1999;150(3):306–311. doi: 10.1093/oxfordjournals.aje.a010003. [DOI] [PubMed] [Google Scholar]
- Wong FL, Rotheram-Borus MJ, Lightfoot M, Pequegnat W, Comulada WS, Cumberland W, Weinhardt LS, Remien RH, Chesney M, Johnson M. Effects of behavioral intervention on substance use among people living with HIV: The Healthy Living Project randomized controlled study. Addiction. 2008;103(7):1206–1214. doi: 10.1111/j.1360-0443.2008.02222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi MS, Mrus JM, Wade TJ, Ho ML, Hornung RW, Cotton S, Peterman AH, Puchalski CM, Tsevat J. Religion, spirituality, and depressive symptoms in patients with HIV/AIDS. Journal of General Internal Medicine. 2006;21(5):S21–S27. doi: 10.1111/j.1525-1497.2006.00643.x. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]