Abstract
Aims/Hypothesis
We assessed the effects of type 1 diabetes and type 2 diabetes on fecundability (as manifest by increased time-to-pregnancy (TTP)) in a large cohort of pregnant women.
Methods
This study is based on the Norwegian Mother and Child Cohort Study (MoBa). Members of this large cohort were enrolled early in pregnancy and asked about TTP and other factors. Among the 58,004 women included in the analysis, we identified 221 cases of type 1 diabetes and 88 cases of type 2 diabetes using the Medical Birth Registry of Norway. A logistic analog of the proportional probability model, a Cox-like discrete-time model, was used to compute fecundability odds ratios (FOR) and 95% CI for type 1 diabetes and type 2 diabetes, adjusted for maternal age and prepregnancy BMI.
Results
Compared with non-diabetic women, the adjusted FOR for women with type 1 diabetes was 0.76 (95% CI=0.64, 0.89) and the adjusted FOR for women with type 2 diabetes was 0.64 (95% CI=0.48, 0.84). These FORs did not change substantively and remained statistically significant after excluding women with irregular menstrual cycles and accounting for cycle length.
Conclusions/Interpretation
The results from the present study provide evidence of substantially decreased fecundability for women with type 1 and type 2 diabetes, even among those with normal menstrual cycles.
Keywords: Pregestational Diabetes, Type 1 Diabetes, Type 2 Diabetes, Fecundability, Pregnancy, Time-to-Pregnancy
Introduction
Women with type 1 diabetes may experience delayed onset of menarche, early menopause, and menstrual cycle irregularities [1]. For example, a study of Danish women reported a higher prevalence of menstrual irregularities among women with type 1 diabetes (21.6%) compared with controls (10.8%) [2]. Further, a study conducted in the United States found that women with type 1 diabetes had up to twice the frequency of menstrual irregularities compared with controls [3]. Menstrual cycle irregularities among women with type 2 diabetes have been less well studied. However, the Nurses Health Study reported an increased risk of developing type 2 diabetes among women with long cycles (relative risk (RR)=2.0, 95% CI=1.6, 2.7) or very irregular cycles (RR=1.5, 95% CI=1.3,1.8) [4].
Studies have also reported increased rates of spontaneous abortion among women with type 1 diabetes [5], and of perinatal mortality and birth defects among women with either type 1 or type 2 diabetes [6, 7].
Due to the reproductive abnormalities experienced by women with diabetes, a reduction in fecundability (the ability to conceive) is expected. Yet data that directly address the effects of diabetes on women’s fecundability or fertility are scarce[1]. In Sweden, the live birth rate among women with type 1 diabetes has been normal since 1985 [8]. Live birth rate, though, reflects fertility rather than fecundability. Because fecundability is the odds of conception (regardless of pregnancy outcome), live birth rate is a relatively insensitive measure of fecundability. For example, conceptions leading to spontaneous abortions are counted towards fecundability but are not reflected in live birth rate. Additionally, women’s family planning decisions can alter a population’s fertility rate (by lowering the number of live births), even if the population is fecund. Therefore, data regarding pregnancy attempts are necessary to make conclusions regarding fecundability. In the present study, we examined the effects of type 1 diabetes and type 2 diabetes on fecundability in a large study of pregnant women.
Methods
This study was based on the Norwegian Mother and Child Cohort Study (MoBa), conducted by the Norwegian Institute of Public Health [9]. A total of 235,577 women in Norway were invited to participate in MoBa. Women were enrolled from 1999–2008 and received an invitation to participate in MoBa through the mail with their notice of an appointment for a routine ultrasound, given to all women in Norway around week 17–18 of gestation. The participation rate was 38.5%, resulting in 90,697 women who participated in MoBa, and 106,977 pregnancies. Additional details can be found at www.fhi.no/morogbarn. MoBa was approved by The Regional Committee for Medical Research Ethics and the Norwegian Data Inspectorate. Informed consent was obtained from each participant.
Mothers completed a questionnaire around 17 weeks of gestation. Maternal demographics (age, height, prepregnancy weight, and education), lifestyle factors (physical activity, smoking, and alcohol use three months before pregnancy; frequency of intercourse one month before pregnancy), and maternal diseases (hypo- or hyperthyroidism, fallopian tube infection, endometriosis, and sexually transmitted diseases) were obtained from this questionnaire. Maternal prepregnancy body mass index (BMI) was constructed using the self-reported values from this questionnaire. The questionnaire also included questions related to reproductive history (cycle length, irregular cycles in the last year, parity, history of fertility treatments, and time-to-pregnancy (TTP)). Regarding TTP, women were first asked whether they planned their pregnancy. If they answered positively, they were asked a series of questions regarding how long it took them to achieve pregnancy including “how many months did you have regular intercourse without contraception before you became pregnant?” Women chose ‘<1 month’, ‘1–2 months’, or ‘3 months or more’. If they answered ‘3 months or more’, they were further prompted to list the number of months.
Data on MoBa pregnancies were linked with data in the Medical Birth Registry of Norway (MBRN). The MBRN data were collected by the physician or midwife attending the childbirth, who had access to the pregnancy medical record [10]. Data from the MBRN were used to ascertain women’s diabetes status (pregestational type 1 diabetes, pregestational type 2 diabetes, unspecified pregestational diabetes, or gestational diabetes).
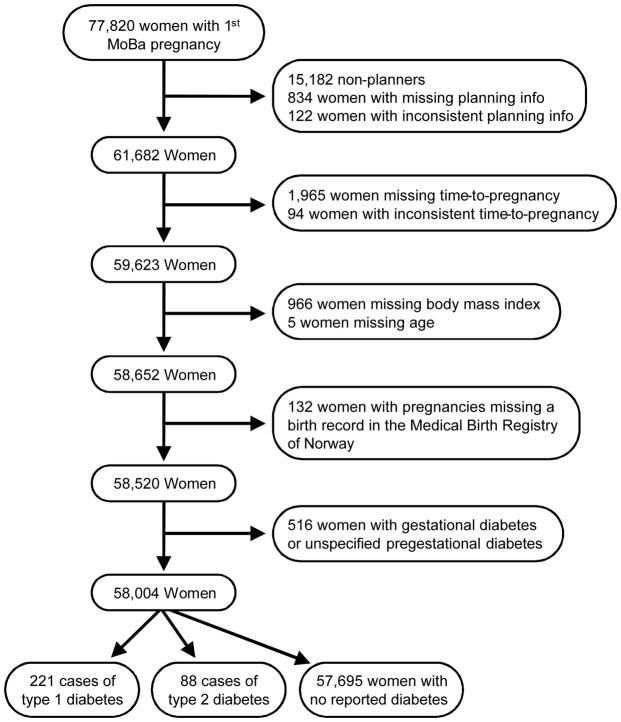
Eligibility for the present analysis was restricted to a woman’s first pregnancy registered with MoBa (that is, a woman’s first study pregnancy which may not be her first lifetime pregnancy). A total of 77,820 pregnancies were eligible. Further exclusions were made as shown in Figure 1. Thus, a total of 58,004 pregnancies, including 221 type 1 diabetic women and 88 type 2 diabetic women, were included in the analysis.
Figure 1.
Flow chart for subject inclusion based on MoBa Database Version 4.301, restricted to MoBa first pregnancies.
The logistic analog of the proportional probability model, a Cox-like discrete-time model [11], was used to estimate fecundability odds ratios (FOR) and 95% CIs for associations between type 1 diabetes or type 2 diabetes and fecundability (odds of conception). The equation for this model is given in the online appendix. This is a standard statistical method used in studies of fecundability [12] and was implemented using PROC LOGISTIC in SAS (SAS Institute Inc., Cary, NC). For each month that contributes to the analysis, the FOR measures the fecundability in the exposed (women with type 1 diabetes or type 2 diabetes) divided by the fecundability in the unexposed (women with no diabetes), conditional on not having conceived in any previous month. The FOR is the weighted average of the estimates across all contributing months. An FOR of less than one indicates reduced fecundability (increased TTP). The unit of analysis was the woman-month and each woman contributed up to 12 months to the analysis. Women’s reported TTP was used to construct an analysis dataset with multiple records per woman (one record for each month she was trying to conceive). As recommended for avoiding medical intervention bias, TTP was censored at 13 months because women are considered clinically infertile after 12 months of unsuccessful pregnancy attempts [13]. For example, if a woman reported getting pregnant after 14 months, only her first 12 (unsuccessful) months contributed to the analysis. Further, women who received infertility treatment at or before 12 months (2.0%) had their TTP censored at TTP-1 month. Thus, if a woman reported getting pregnant after nine months, and reported receiving fertility treatments, only her first (unsuccessful) eight months contributed to the analysis.
Maternal age and prepregnancy BMI (kg/m2) were assumed to be important confounders and included in the model a priori. Maternal age was modeled as a continuous variable while prepregnancy BMI was modeled using its cubic form and all lower order terms (BMI, BMI2, and BMI3, all continuous). We further considered as potential confounders variables that may be associated with both diabetes and fecundability, conditional on maternal age and prepregnancy BMI. These variables include: maternal education, physical activity, smoking and alcohol use, and frequency of intercourse. A backward selection method was used whereby the additional covariates were dropped from the full model and the change in the effect estimate for diabetes and fecundability was assessed in a step-wise manner. Because the effect estimates changed by less than 10% with each deletion, none of these variables were deemed confounders. To further evaluate the potential confounding effects of maternal diseases (fallopian tube infection, endometriosis, sexually transmitted disease, and hypo- or hyperthyroidism) without sacrificing degrees of freedom in the model, we examined the association between diabetes and fecundability after excluding women with these conditions (one at a time). Because the FORs for both type 1 and type 2 diabetes did not change, we concluded that these variables were not confounders. Interaction terms were fit to test effect modification between parity (yes/no) and diabetes, and age (continuous) and diabetes. To help determine whether interaction was present, we used an alpha level equal to 0.20 as a screening criterion. The p-values for interaction between parity and diabetes (p=0.61 for type 1 diabetes and p=0.68 for type 2 diabetes) and age and diabetes (p=0.44 for type 1 diabetes and p=0.65 for type 2 diabetes) all fell well above this cutoff, providing no support for interaction. All analyses were completed using SAS version 9.2 (SAS Institute Inc., Cary, NC).
We completed two additional sub-analyses. In the first, we recalculated FORs after excluding women who reported irregular menstrual cycles; in the second, we recalculated FORs after excluding women who reported irregular menstrual cycles and we based the TTP calculation on the estimated number of cycles it took to get pregnant (instead of the number of months). For the analysis using cycle lengths, those who reported cycle length greater than 60 days (0.2%) were excluded which also likely excluded women with polycystic ovary syndrome (PCOS).
Additional sensitivity analyses were conducted and the results are presented in Figure 1 of the online appendix. These sensitivity analyses assessed planning bias (bias resulting from excluding women who did not plan their pregnancy and who may have higher fecundability than planners [13, 14]), medical intervention bias (bias that may result if the exposure under study is associated with the probability that women will receive successful medical help for infertility [13, 14]), and wantedness bias (bias which occurs when women who did not plan their pregnancy respond that the pregnancy was in fact planned when asked about it in retrospect [13, 14]).
Results
A total of 61,682 first MoBa pregnancies were planned compared with 15,182 unplanned pregnancies (Figure 1). The distribution of diabetes among planners and non-planners was essentially the same (Table 1 in the online appendix). Planners were older, more educated, smoked less, and had more infertility treatments than non-planners (Table 1 in the online appendix). While 11.2% of women with no diabetes had a TTP of >12 months, 19.5% of women with type 1 diabetes and 29.6% of women with type 2 diabetes had a TTP of >12 months (Table 1). On average, women with type 2 diabetes were older than either women with type 1 diabetes or non-diabetic women at the time of their pregnancy. Also, on average, women with either type 1 diabetes or type 2 diabetes had a higher prepregnancy BMI compared with non-diabetic women. Women with either type 1 or type 2 diabetes were also more likely to have irregular menstrual cycles in the 12 months before pregnancy and to receive fertility treatments for their pregnancy compared with non-diabetic women.
Table 1.
Demographic factors among 58,004 women, by diabetes status
| Maternal Characteristics | No Diabetes N=57,695 % |
Type 1 Diabetes N=221 % |
Type 2 Diabetes N=88 % |
|---|---|---|---|
| Time-to-pregnancy (TTP) (mean, months) | 4.4 | 5.4 | 6.5 |
| Time-to-pregnancy (TTP) | |||
| <1 month | 23.0 | 20.8 | 17.1 |
| 1–2 months | 27.0 | 23.1 | 17.1 |
| 3 months | 12.2 | 10.9 | 12.5 |
| 4–12 months | 26.6 | 25.8 | 23.9 |
| >12 months | 11.2 | 19.5 | 29.6 |
| Age (mean) | 29.8 | 29.7 | 31.5 |
| Prepregnancy body mass index (kg/m2) (mean) | 24.1 | 26.3 | 28.5 |
| Smoking 3 months before pregnancy | |||
| Daily | 17.3 | 20.0 | 21.6 |
| Sometimes | 10.2 | 9.1 | 6.8 |
| None | 72.3 | 71.0 | 70.5 |
| Missing | 0.2 | 0.0 | 1.1 |
| Highest completed years of education | |||
| ≤12 years | 35.0 | 34.8 | 45.5 |
| 13–16 years | 40.7 | 47.5 | 40.9 |
| >16 years | 22.4 | 16.3 | 12.5 |
| Other | 2.1 | 1.4 | 1.1 |
| Irregular menstrual cycles 12 months before pregnancy | |||
| Yes | 21.1 | 24.4 | 21.6 |
| No | 78.7 | 74.7 | 78.4 |
| Missing | 0.3 | 0.9 | 0.0 |
| Infertility treatment for current pregnancy | |||
| Yes | 7.0 | 15.4 | 15.9 |
| No | 93.0 | 84.6 | 84.1 |
| Frequency of intercourse one month before pregnancy | |||
| >2 times per week | 48.5 | 51.1 | 45.5 |
| 1–2 times per week | 35.5 | 34.9 | 31.8 |
| <1 time per week | 14.7 | 12.2 | 19.3 |
| Missing | 1.4 | 1.8 | 3.4 |
| Parity | |||
| 0 | 52.4 | 59.3 | 42.1 |
| 1 | 31.3 | 32.1 | 29.6 |
| >1 | 16.4 | 8.6 | 28.4 |
The crude FOR for type 1 diabetes was 0.73 (95% CI=0.62, 0.86) and for type 2 diabetes was 0.53 (95% CI=0.41, 0.70). After adjustment for age and prepregnancy BMI, the estimates were slightly attenuated: women with type 1 diabetes had an FOR of 0.76 (95% CI=0.64, 0.89) and women with type 2 diabetes had an FOR of 0.64 (95% CI=0.48, 0.84) compared with women with no diabetes (Table 2). Based on our model, among women with average BMI (24.1 kg/m2 in our study population) and less than 25 years of age with no diabetes, the fecundability (expressed as a probability) was 26% versus a 21% fecundability for similar women with type 1 diabetes and a 18% fecundability for similar women with type 2 diabetes (data not shown).
Table 2.
Adjusted fecundability odds ratios (FOR) and 95% CIs associated with type 1 diabetes and type 2 diabetes
| Modela | Type 1 Diabetes
|
Type 2 Diabetes
|
||||||
|---|---|---|---|---|---|---|---|---|
| N | FOR | 95% CI | N | FOR | 95% CI | |||
| All women | ||||||||
| No Diabetes | 57,695 | 1.00 | 57,695 | 1.00 | ||||
| Diabetes | 221 | 0.76 | 0.64 | 0.89 | 88 | 0.64 | 0.48 | 0.84 |
| Excluding women reporting irregular menstrual cycles | ||||||||
| No Diabetes | 43,385 | 1.00 | 43,385 | 1.00 | ||||
| Diabetes | 165 | 0.80 | 0.66 | 0.97 | 69 | 0.71 | 0.52 | 0.96 |
| Excluding women reporting irregular menstrual cycles and using cycle length to calculate time-to-pregnancy | ||||||||
| No Diabetes | 43,987 | 1.00 | 43,987 | 1.00 | ||||
| Diabetes | 161 | 0.81 | 0.66 | 0.98 | 69 | 0.69 | 0.51 | 0.93 |
All models adjusted for prepregnancy BMI and maternal age (see methods)
Approximately 79% of women reported regular menstrual cycles, including 79% of women with no diabetes, 75% of women with type 1 diabetes and 78% of women with type 2 diabetes (Table 2). Once the analysis was restricted to these women, there was a slight attenuation in the FOR for either women with type 1 or type 2 diabetes. Accounting for cycle length had little effect on the results. The additional sensitivity analyses addressing planning, wantedness, and medical intervention biases suggested none had an important effect on results (See online appendix).
Discussion
In these data, the FOR among women with type 1 diabetes was reduced by 24% and among women with type 2 diabetes it was reduced by 36% compared with non-diabetic women. Examination of fecundability among women with diabetes has not been reported to our knowledge, probably because it requires a very large general population sample to include sufficient women with diabetes.
Although the mechanism through which diabetes affects fecundability is unknown, several have been proposed. Hyperglycemic mouse models have shown that that poor metabolic control during the periconception period may affect oocyte competence and decreased fecundability [15]. A recent review suggests that not only are women with type 2 diabetes less likely to obtain prepregnancy counseling than type 1 diabetics, but diabetic women who do not seek prepregnancy counseling have decreased metabolic control [16]. Although the present study was unable to assess differences in HbA1c levels among women with type 1 and type 2 diabetes, it is possible that poor metabolic control at the time of conception could account for the lower fecundability observed among the women with type 2 diabetes.
Type 1 and type 2 diabetes may affect fecundability through separate mechanisms. Because the preimplantation conceptus is sensitive to insulin, it may be directly affected by maternal insulin resistance. Using mouse models, Pinto et al. [17] demonstrated that excess insulin or insulin-like growth factor 1 leads to decreased levels of the pre-implantation glucose transporter (GLUT) 8. The decreasing levels of GLUT 8 increased apoptosis in blastocysts, increased rates of resorptions, and decreased pregnancy rates [17]. Although the mouse models in these studies used glucose levels that may not be directly applicable to humans, they provide insight into how insulin resistance may affect fecundability.
Lastly, alterations in the hypothalamic-pituitary-ovarian (HPO) axis could affect fecundability among both type 1 and type 2 diabetic women. Menstrual disturbances in diabetic women suggest alterations in the HPO axis [1]. Given the evidence supporting the association between diabetes and menstrual cycle irregularities, we explored the influence of cycle irregularity and cycle length on the associations described in the present study. After restricting the analysis to women with regular menstrual cycles, the FORs among women with type 1 diabetes mellitus and type 2 diabetes mellitus were attenuated but still statistically significant. We observed similar reductions in fecundability in both type 1 and type 2 diabetic women after accounting for cycle length. Past studies have documented large proportions of oligomenorrhea among women with pregestational diabetes [2–4, 18]. Although based on small numbers, we also observed a higher proportion of longer menstrual cycles among women with diabetes compared to women without diabetes (data not shown). It appears that regardless of menstrual disturbances (length or regularity), women with diabetes still experience a reduction in fecundability. These results, paired with observations regarding delayed menarche among type 1 diabetic women may suggest a hypothalamic contribution to reduced fecundability [1].
Our study population is drawn from a cohort with a relatively large number of women with pregestational diabetes. A recent study examined the validity of diabetes diagnosis in the MBRN by cross referencing MBRN diagnoses between March, 2004 and January, 2007 with medications dispensed for diabetes listed in the Norwegian Prescription Database (NorPD) [19]. The authors of this study reported good sensitivity (the proportion of accurately identified cases among all true cases) for type 1 diabetes (90%). The sensitivity of any type of diabetes (72%) (including type 1 diabetes, type 2 diabetes and gestational diabetes) was lower, possibly a result of the fact that the NorPD database does not capture cases of type 2 diabetes that do not require medication. Further, a separate study compared the MBRN diabetes diagnoses with medical records for 1998 and estimated that the positive predictive value of pregestational diabetes (including type 1 and type 2 diabetes) was 79.5% (95% CI=74.6%, 84.5%) [20]. The mean BMI among type 1 diabetic women was higher than those without diabetes, possibly indicating misclassification (i.e. some type 2 diabetic women may have been classified as having type 1 diabetes). However, a recent study based on Swedish medical records also reported similarly increased prepregnancy BMI among women with type 1 diabetes compared to women with no diabetes [21].
Although women were recruited during pregnancy, they were recruited early in pregnancy and are likely to have provided accurate reports of TTP and other covariates. Due to the pregnancy-based design of the MoBa study, sterile and extremely subfecund women were excluded from our sample. This may limit the generalizability of the results, but if diabetes is associated with decreased fecundability, bias resulting from including only the most fecund women in the sample will result in underestimation of the effect. Retrospective TTP studies are susceptible to planning, wantedness, and medical intervention biases [13, 14]; however, when sensitivity analyses were conducted, the overall results did not change.
In the present study, we found evidence of longer TTP among women with type 1 diabetes or type 2 diabetes compared with women with no diabetes. This relationship was present even after accounting for cycle length and cycle regularity. Though menstrual and reproductive problems have been documented for women with diabetes, no study has previously demonstrated reduced fecundability directly. The reduction we observed is similar in magnitude to the FOR of obese women in a recent study [22], and we controlled for the effect of BMI. Women with diabetes may be unaware of the difficulties achieving pregnancy, particularly if they have never experienced menstrual cycle disturbances. These findings have important implications regarding the potential medical treatment of women with diabetes who wish to have a child. Fertility drugs (commonly gonadotropins, gonadotropin releasing hormone (GnRH) agonists, and GnRH antagonists) are unlikely to affect the woman’s glycemic state [23]. Although current clinical management guidelines for women with pregestational diabetes discusses the role of preconception counseling for these women, the focus of these guidelines is on euglycemic control as it relates to achieving the best possible pregnancy outcome [24]. In the future, it may be useful to have clinically relevant markers of hyperglycemia among women with diabetes attempting pregnancy in order to aid in the elucidation of the mechanism by which diabetes affects fecundability. As with obese women or women with polycystic ovarian syndrome, protocols may be needed to better manage the care of women with diabetes who are planning a pregnancy.
Supplementary Material
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences. The Norwegian Mother and Child Cohort Study is supported by the Norwegian Ministry of Health, NIH/NIEHS (grant no N01-ES-85433), NIH/NINDS (grant no.1 UO1 NS 047537-01), and the Norwegian Research Council/FUGE (grant no. 151918/S10).
Abbreviations
- FOR
Fecundability Odds Ratio
- GLUT
Glucose Transporter
- HPO
Hypothalamic-Pituitary-Ovarian
- MBRN
Medical Birth Registry of Norway
- MoBa
Norwegian Mother and Child Cohort Study
- NorPD
Norwegian Prescription Database
- TTP
Time-to-Pregnancy
Footnotes
Duality of Interests The authors declare that there is no duality of interests associated with this manuscript.
The authors declare no potential conflicts of interest.
References
- 1.Livshits A, Seidman DS. Fertility issues in women with diabetes. Women’s Health. 2009;5:701–707. doi: 10.2217/whe.09.47. [DOI] [PubMed] [Google Scholar]
- 2.Kjaer K, Hagen C, Sando SH, Eshoj O. Epidemiology of menarche and menstrual disturbances in an unselected group of women with insulin-dependent diabetes mellitus compared to controls. Journal of Clinical Endocrinology and Metabolism. 1992;75:524–529. doi: 10.1210/jcem.75.2.1639955. [DOI] [PubMed] [Google Scholar]
- 3.Strotmeyer ES, Steenkiste AR, Foley TP, Jr, Berga SL, Dorman JS. Menstrual cycle differences between women with type 1 diabetes and women without diabetes. Diabetes Care. 2003;26:1016–1021. doi: 10.2337/diacare.26.4.1016. [DOI] [PubMed] [Google Scholar]
- 4.Solomon CG, Hu FB, Dunaif A, et al. Long or highly irregular menstrual cycles as a marker for risk of type 2 diabetes mellitus. Journal of the American Medical Association. 2001;286:2421–2426. doi: 10.1001/jama.286.19.2421. [DOI] [PubMed] [Google Scholar]
- 5.Lorenzen T, Pociot F, Johannesen J, et al. A population-based survey of frequencies of self-reported spontaneous and induced abortions in Danish women with Type 1 diabetes mellitus. Diabetic Med. 1999;16:472–476. doi: 10.1046/j.1464-5491.1999.00087.x. [DOI] [PubMed] [Google Scholar]
- 6.Melamed N, Hod M. Perinatal mortality in pregestational diabetes. International Journal of Gynecology and Obstetrics. 2009;104 doi: 10.1016/j.ijgo.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 7.Ramosarroyo MA, Rodriguezpinilla E, Cordero JF. Maternal Diabetes -the Risk for Specific Birth-Defects. Eur J Epidemiol. 1992;8:503–508. doi: 10.1007/BF00146367. [DOI] [PubMed] [Google Scholar]
- 8.Jonasson JM, Brismar K, Sparen P, et al. Fertility in women with type 1 diabetes -A population-based cohort study in Sweden. Diabetes Care. 2007;30:2271–2276. doi: 10.2337/dc06-2574. [DOI] [PubMed] [Google Scholar]
- 9.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C. Cohort profile: the Norwegian Mother and Child Cohort Study (MoBa) Int J Epidemiol. 2006;35:1146–1150. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- 10.Irgens LM. The Medical Birth Registry of Norway. Epidemiologicalresearch and surveillance throughout 30 years. Acta Obstet Gynecol Scand. 2000;79:435–439. [PubMed] [Google Scholar]
- 11.Weinberg CR, Baird DD, Rowland AS. Pitfalls inherent in retrospective time-to-event studies: The example of time to pregnancy. Statistics in Medicine. 1993;12:867–879. doi: 10.1002/sim.4780120906. [DOI] [PubMed] [Google Scholar]
- 12.Weinberg CR, Wilcox AJ. Methodologic Issues in Reproductive Epidemiology. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. Lippincott Williams & Wilkins; Philadelphia PA: 2008. pp. 620–640. [Google Scholar]
- 13.Weinberg CR, Baird DD, Wilcox AJ. Sources of bias in studies of time to pregnancy. Stat Med. 1994;13:671–681. doi: 10.1002/sim.4780130528. [DOI] [PubMed] [Google Scholar]
- 14.Joffe M, Key J, Best N, Keiding N, Scheike T, Jensen TK. Studying time to pregnancy by use of a retrospective design. American Journal of Epidemiology. 2005;162:115–124. doi: 10.1093/aje/kwi172. [DOI] [PubMed] [Google Scholar]
- 15.Sutton-McDowall ML, Gilchrist RB, Thompson JG. The pivotal role of glucose metabolism in determining oocyte developmental competence. Reproduction. 2010;139:685–695. doi: 10.1530/REP-09-0345. [DOI] [PubMed] [Google Scholar]
- 16.Slocum JM. Preconception counseling and type 2 diabetes. Diabetes Spectrum. 2007;20:117–123. [Google Scholar]
- 17.Pinto AB, Carayannopoulos MO, Hoehn A, Dowd L, Moley KH. Glucose transporter 8 expression and translocation are critical for murine blastocyst survival. Biology of Reproduction. 2002;66:1729–1733. doi: 10.1095/biolreprod66.6.1729. [DOI] [PubMed] [Google Scholar]
- 18.Yeshaya A, Orvieto R, Dicker D, Karp M, Ben-Rafael Z. Menstrual characteristics of women suffering from insulin-dependent diabetes mellitus. International Journal of Fertility and Menopausal Studies. 1995;40:269–273. [PubMed] [Google Scholar]
- 19.Engeland A, Bjørge T, Daltveit AK, Vollset SE, Furu K. Validation of disease registration in pregnant women in the Medical Birth Registry of Norway. Acta Obstetricia et Gynecologica Scandinavica. 2009;88:1083–1089. doi: 10.1080/00016340903128454. [DOI] [PubMed] [Google Scholar]
- 20.Stene LC, Eidem I, Vangen S, Geir J, Lorentz MI, Narve M. The validity of the diabetes mellitus diagnosis in the medical birth registry of Norway. Norsk Epidemiologi. 2007;17:165–174. [Google Scholar]
- 21.Persson M, Norman M, Hanson U. Obstetric and perinatal outcomes in type 1 diabetic pregnancies: A large, population-based study. Diabetes Care. 2009;32:2005–2009. doi: 10.2337/dc09-0656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Law DCG, Maclehose RF, Longnecker MP. Obesity and time to pregnancy. Human Reproduction. 2007;22:414–420. doi: 10.1093/humrep/del400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Physicians’ Desk Reference. Thomson PDR; Montvale, NJ: 2008. [Google Scholar]
- 24.ACOG Practice Bulletin #60: Pregestational Diabetes Mellitus. Obstetrics & Gynecology. 2005;105:675–685. doi: 10.1097/00006250-200503000-00049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.