Abstract
Objectives
Traditional clinical risk factors are associated with inflammation cross-sectionally, but associations of longitudinal variation in inflammatory biomarkers with corresponding changes in clinical risk factors are incompletely described. We sought to analyze clinical factors associated with change in inflammation in the community.
Methods
We studied 3013 Framingham Offspring (n = 2735) and Omni Cohort (n = 278) participants (mean age 59 years, 55% women, 9% ethnic/racial minority) who attended two consecutive examination cycles (mean 6.7 years apart). We selected ten inflammatory biomarkers representing distinctive biological functions: C-reactive protein (CRP), intercellular adhesion molecule-1, interleukin-6, isoprostanes, lipoprotein-associated phospholipase-2 (Lp-PLA2) activity, Lp-PLA2-mass, monocyte chemoattractant protein-1, osteoprotegerin, P-selectin, and tumor necrosis factor receptor II (TNFRII). We constructed multivariable-adjusted regression models to assess the relations of baseline, follow-up and change in clinical risk factors with change in biomarker concentrations over time.
Results
Baseline, follow-up and change in clinical risk factors explain a moderate amount of the variation in biomarker concentrations across 2 consecutive examinations (ranging from r2 = 0.28 [TNFRII] up to 0.52 [Lp-PLA2-mass]). In multivariable models, increasing body-mass index, smoking initiation, worsening lipid profile, and increasing waist size were associated with increasing concentrations of several biomarkers. Conversely, hypercholesterolemia therapy and hormone replacement cessation were associated with decreasing concentrations of biomarkers such as CRP, Lp-PLA2-mass and activity.
Conclusion
Cardiovascular risk factors have different patterns of association with longitudinal change in inflammatory biomarkers and explain modest amounts of variability in biomarker concentrations. Nevertheless, a substantial proportion of longitudinal change in inflammatory markers is not explained by traditional risk factors.
Keywords: Biological markers, Longitudinal studies, Inflammation
1. Introduction
Inflammation and CVD risk factors are closely interrelated. CVD risk factors, such as hypertension, and hypercholesterolemia are associated with higher circulating concentrations of inflammatory biomarkers. Conversely, chronic inflammation increasingly is recognized as a major contributor to the development and the progression of atherosclerosis, CVD risk factors [1, 2] and subsequent cardiovascular disease (CVD) [3, 4]. Prior studies have reported the relations of CVD risk factors to circulating inflammatory biomarkers assessed on a single occasion [5–7].Nevertheless, there are only a few observational studies available examining the longitudinal progression of circulating inflammatory biomarkers [8]. Understanding modulators of longitudinal progression in inflammation potentially may improve early recognition of atherosclerosis and enhance risk prediction of CVD beyond traditional clinical risk factors [4].
Recent studies reveal an alarming increasing prevalence of CVD risk factors globally [9–11]. As risk factors and inflammation are closely associated, both may contribute to increased CVD burden. We sought to investigate the risk factors related to the progression of 10 inflammatory biomarkers representing distinctive biological functions. We hypothesized that higher level of CVD risk factors is associated with greater systemic inflammation and, therefore, increased biomarker levels. Further, we postulated that adverse changes in clinical factors would be associated with accelerated inflammation. We tested these hypotheses in a large community-based sample.
2. Methods
2.1. Study sample
The study design and selection criteria of the Framingham Offspring Study and Framingham Omni Study have been described previously [12, 13]. Since enrollment in 1971 (Offspring) and 1994 (Omni), study participants have had regular follow-up every 4–8 years. Offspring Cohort participants who attended the seventh (n = 3,539, 1998–2001, of which n = 3334 had a clinical examination) and eighth examination cycles (n = 3021, 2004–2008, of which n = 2913 had a clinical examination), or Omni participants attending the second (n = 405, 1999–2001) and third (n = 298, 2007–2008), were eligible for the study if they had at least one biomarker measured at both examination cycles (separated by 3.7–8.7 years). We excluded participants for the following reasons: missing biomarker measurement (n = 136) and missing covariate data (n = 246). The Boston University Medical Center Institutional Review Board approved the study protocol. All participants provided informed consent at both examinations.
2.2. Clinical evaluations
The Framingham Heart Study clinical evaluations were standardized and consisted of a concise clinical history with emphasis on physician ascertainment of symptoms, lifestyle habits, medications, interim cardiovascular events and a focused cardiovascular physical examination. Research technicians measured height, weight and waist circumference. Body-mass index was calculated as weight measured in kilograms divided by the square of height in meters (kg/m2). Current smoking was defined as self-report of smoking cigarettes regularly in the year prior to examination. Moderate to heavy alcohol consumption was defined as having reported ≥14 drinks per week for men, and ≥7 drinks per week for women. Blood samples were drawn after an overnight fast.
2.3. Biomarkers measurements
Participants were fasting except for the Omni Cohort at their examination cycle two [14]. We processed, centrifuged and stored blood specimens at −80 °C until assays were performed. We selected 10 different biomarkers of vascular inflammation available in the Framingham Heart Study: C-reactive protein (CRP), soluble intercellular adhesion molecule-1 (sICAM-1), interleukin-6, urinary 8-epi-PGF2α isoprostanes (isoprostanes), lipoprotein-associated phospholipase-A2 (Lp-PLA2) activity, Lp-PLA2-mass, monocyte chemoattractant protein-1 (MCP-1), osteoprotegerin, P-selectin, and tumor necrosis receptor II (TNFRII). CRP was measured using particle enhanced immunonephelometry; sICAM-1, interleukin-6, isoprostanes, Lp-PLA2-mass and activity, MCP-1, P-Selectin, and TNFRII were assayed with ELISA. We performed standard quality control evaluations; all intra-assay coefficients of variation were <10%. The details of the assays and measurement of were described elsewhere [14–16] and the biomarkers measurement manuals can be found at the FHS website http://www.framinghamheartstudy.org/share/vascularprotocols.html.
2.4. Statistical analysis
All analyses were conducted using natural logarithmically-transformed biomarkers to normalize their skewed distributions. To facilitate interpretation of concentrations of biomarkers between the two consecutive examinations we calculated medians and quartiles of each biomarker on the original scale. Pearson correlations were estimated between biomarker concentrations from the two consecutive examinations. For each biomarker we defined the response variable as change in biomarker concentration between examinations. We fitted multivariable regression models of change versus baseline biomarker level as well as traditional clinical factors – baseline and changes between examinations for each biomarker. We standardized both the change in markers and continuous clinical variables to mean 0 and SD 1 to facilitate the comparison of estimated beta coefficients across biomarkers. We examined stepwise models with grouped variables for most covariates: for continuous measures we used baseline value and change in value; for binary traits we used baseline status and change in status. After selecting groups of variables for each biomarker, we ran backward elimination to remove some nonsignificant individual covariates from groups. We selected covariates typically available in the clinical setting and known to be associated with CVD. Candidate variables were smoking, alcohol use, systolic blood pressure, diastolic blood pressure, body-mass index, waist circumference, glucose level, total/high-density lipoprotein (HDL) cholesterol level, low-density lipoprotein (LDL) level, use of aspirin, hormone replacement therapy, treatment for hypertension, treatment for hypercholesterolemia, history of diabetes, and history of cardiovascular disease. To facilitate comparisons among markers, we standardized response and (continuous) predictor variables. Given multiple tests, we used a 50-fold Bonferroni correction and considered a two-sided p ≤ 0.001 as statistically significant in each analysis. With sample size 3000 and significance level 0.001, we had power 0.80 to detect association between clinical variables with change in ln(biomarker) if the true partial correlation was 0.076 or larger in absolute value; for isoprostanes, sample size was n = 2480 and the corresponding partial correlation was 0.083. All analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina).
3. Results
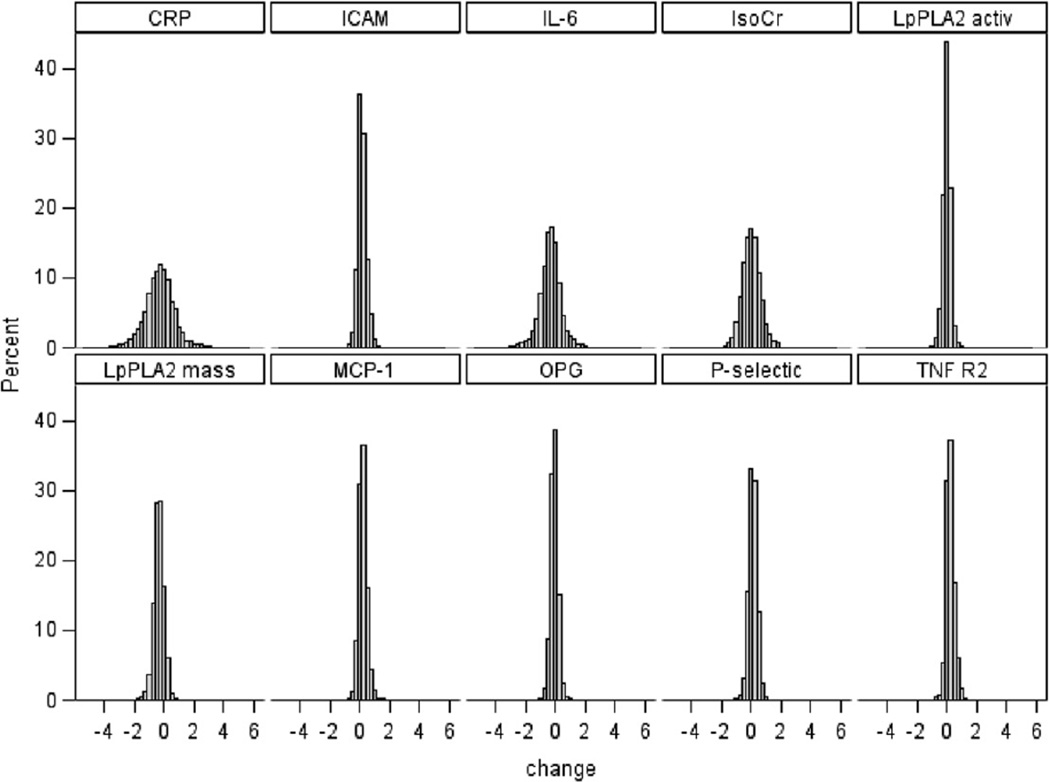
We examined 3013 participants (55% women, mean age 59 ± 9 years, 9% ethnic/racial minorities) from the Framingham Heart Study Offspring and Omni Cohorts (Table 1). Among participants who attended the index examination and who had biomarker and covariate data, 274 died before the close of examination 8 (mean age 69 years, 71% had hypertension, 30% had diabetes, 18% had CVD). Over the mean 6.7 year interval between baseline and follow-up examinations the prevalence of medication use (antihypertensive, lipid-lowering medication and aspirin) increased in both men and women. The only exception observed was hormone replacement therapy in women, which decreased. Fig. 1 illustrates the distribution of change of biomarkers on follow-up examination. Supplementary eFigure 1 compares the Box plots for change in log-transformed biomarkers after removing outliers. The median concentrations at baseline and at follow-up of each biomarker are shown in Table 2. The baseline and follow-up concentration of each biomarker were correlated; the lowest correlation was 0.32 for isoprostanes and the highest correlation was 0.66 for osteoprotegerin (eTable 1). By and large, the correlation between change in ln concentration of biomarkers was weak, except for interleukin-6 and CRP (r = 0.43) and Lp-PLA2 activity and mass (r = 0.55) (Table 3).
Table 1.
Participant characteristics.
| Men, n = 1353 |
Women, n = 1660 |
|||
|---|---|---|---|---|
| aBaseline | bFollow-up | aBaseline | bFollow-up | |
| Age, y | 59 ± 9 | 66 ± 9 | 59 ± 9 | 66 ± 9 |
| Cigarette smoking, % | 155(11) | 111(8) | 196(12) | 146(9) |
| Systolic blood pressure, mmHg | 127 ± 16 | 129 ± 17 | 125 ± 19 | 128 ± 18 |
| Diastolic blood pressure, mmHg | 76 ± 9 | 75 ± 10 | 73 ± 10 | 72 ± 10 |
| Body-mass index, kg/m2 | 28.8 ± 4.6 | 28.9 ± 4.8 | 27.6 ± 5.8 | 27.8 ± 5.9 |
| Waist circumference, in | 40 ± 5 | 41 ± 5 | 38 ± 6 | 39 ± 6 |
| Total/HDL cholesterol ratio | 4.5 ± 1.3 | 3.7 ± 1.1 | 3.6 ± 1.2 | 3.3 ± 1.0 |
| Triglycerides, mg/dL | 142 ± 95 | 119 ± 76 | 130 ± 81 | 116 ± 65 |
| Glucose, mg/dL | 107 ± 28 | 110 ± 26 | 99 ± 24 | 103 ± 21 |
| Diabetes, % | 187(14) | 245(18) | 152(9) | 190(11) |
| Hypertension treatment, % | 456(34) | 718(53) | 453(27) | 755(46) |
| Lipid-lowering medication, % | 313(23) | 665(49) | 256(15) | 627(38) |
| Hormone replacement therapy, % | 525(32) | 159(10) | ||
| Aspirin treatmentc, % | 509(38) | 714(53) | 370(22) | 591(36) |
| Prevalent cardiovascular disease,% | 97(7) | 145(11) | 39(2) | 71(4) |
Data are presented as mean ± standard deviation, or n(%).
Baseline examination is Offspring 7 and Omni 2.
Follow-up examination represents Offspring 8 and Omni 3.
Aspirin treatment ≥3 times week.
Fig. 1.
Histogram for changes in log biomarkers.
Table 2.
Summary for median concentration of biomarkers at baseline and follow-up examination.
| Variable | Baseline |
Follow-up |
||||
|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | |
| CRP, mg/L | 2.04 | 0.95 | 4.88 | 1.49 | 0.74 | 3.21 |
| sICAM-1, ng/mL | 238 | 207 | 279 | 271 | 230 | 336 |
| Interleukin-6, pg/mL | 2.54 | 1.72 | 4.09 | 1.77 | 1.18 | 2.87 |
| Isoprostanes, pg/mmol | 130 | 88 | 190 | 128 | 96 | 178 |
| Lp-PLA2 activity, nmol/mL/min | 138 | 116 | 163 | 136 | 114 | 160 |
| Lp-PLA2-mass, ng/mL | 278 | 223 | 351 | 200 | 170 | 229 |
| MCP-1, pg/mL | 305 | 244 | 375 | 364 | 299 | 441 |
| Osteoprotegerin, pmol/L | 5.21 | 4.31 | 6.22 | 4.72 | 3.90 | 5.70 |
| P-Selectin, ng/mL | 36.0 | 28.4 | 45.0 | 39.7 | 32.6 | 47.9 |
| TNFRII, pg/mL | 1918 | 1609 | 2310 | 2368 | 1913 | 3029 |
Table 3.
Correlation between change in log concentration of biomarkers.
| Change in log biomarker concentration | Change in log biomarker concentration |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CRP | Interleukin-6 | sICAM-1 | Isoprostanes | Lp-PLA2-mass | Lp-PLA2 activity | MCP-1 | Osteoprotegerin | P-selectin | TNFR2 | |
| CRP | 1.00 | |||||||||
| Interleukin-6 | 0.43† | 1.00 | ||||||||
| sICAM-1 | 0.12† | 0.05* | 1.00 | |||||||
| Isoprostanes | 0.02 | 0.01 | 0.07† | 1.00 | ||||||
| Lp-PLA2-mass | 0.06* | 0.03 | 0.04* | 0.01 | 1.00 | |||||
| Lp-PLA2 activity | 0.05* | 0.01 | 0.06* | −0.03 | 0.55† | 1.00 | ||||
| MCP-1 | 0.03 | 0.10† | 0.12† | 0.05* | 0.05* | 0.08† | 1.00 | |||
| Osteoprotegerin | 0.06† | 0.05* | 0.02 | 0.04 | 0.02 | −0.03 | 0.01 | 1.00 | ||
| P-selectin | 0.14† | 0.10† | 0.05* | 0.05* | 0.10† | 0.07† | 0.09† | 0.01 | 1.00 | |
| TNFR2 | 0.08† | 0.05* | 0.12† | 0.05* | 0.00 | 0.02 | 0.05* | −0.05* | 0.04* | 1.00 |
Notes:
p-value between 0.05 and 0.001;
p-value less than 0.001.
3.1. Clinical correlates of change of biomarkers
The results of the multivariable models of longitudinal change in biomarkers are shown in Table 4. Overall, we observed that the most consistent and strongest factor associated with change in biomarker levels was the baseline biomarker concentration (β = −0.736; SE = 0.015 for isoprostanes to β = −0.193; SE = 0.010 for TNFRII). Higher baseline biomarker concentration was associated with lower biomarker concentration at follow-up.
Table 4.
Clinical covariates of change in biomarkers concentration: results of 2-stage stepwise modeling.
| Covariates | CRP |
sICAM-1 |
Interleukin-6 |
Isoprostanes |
Lp-PLA2 activity |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | β | SE | β | SE | |
| Biomarker value, baseline | −0.494 | 0.018 | −0.464 | 0.020 | −0.544 | 0.017 | −0.736 | 0.015 | −0.493 | 0.018 |
| Age, baseline | 0.102 | 0.017 | 0.063 | 0.016 | 0.213 | 0.017 | ||||
| Omni Cohort | −0.377 | 0.060 | 0.287 | 0.062 | −0.187 | 0.046 | −0.190 | 0.049 | ||
| Interaction Omni* baseline | 0.341 | 0.052 | ||||||||
| Sex (female) | 0.127 | 0.032 | 0.234 | 0.028 | ||||||
| Total/HDL baseline | 0.091 | 0.021 | 0.356 | 0.019 | ||||||
| Change Total/HDL | 0.077 | 0.019 | 0.099 | 0.020 | 0.589 | 0.022 | ||||
| Smoke, baseline | 0.305 | 0.050 | 0.213 | 0.050 | 0.376 | 0.051 | 0.29 | 0.045 | ||
| Body-mass index, baseline | 0.131 | 0.018 | ||||||||
| Change in body-mass index | 0.200 | 0.017 | ||||||||
| Lipid therapy, baseline | −0.272 | 0.044 | ||||||||
| Lipid therapy, start | −0.212 | 0.044 | −0.321 | 0.037 | ||||||
| Hormone replacement therapy, baseline | ||||||||||
| Hormone replacement therapy, start | ||||||||||
| Hormone replacement therapy, stop | −0.281 | 0.051 | ||||||||
| Diastolic blood pressure, baseline | ||||||||||
| Change in diastolic blood pressure | ||||||||||
| Waist Circumference, baseline | 0.147 | 0.017 | ||||||||
| Change in Waist Circumference | 0.107 | 0.016 | ||||||||
| Triglycerides, baseline | ||||||||||
| Change triglycerides | −0.164 | 0.017 | ||||||||
| Diabetes, new-onset | ||||||||||
| Adjusted R-squared | 0.298 | 0.304 | 0.285 | 0.515 | 0.466 | |||||
| Lp-PLA2-mass |
MCP-1 |
Osteoprotegeri |
P-selectin |
TNFR2 |
||||||
| Est β | SE | Est β | SE | Est β | SE | Est β | SE | Est β | SE | |
| Biomarker value, baseline | −0.705 | 0.014 | −0.539 | 0.016 | −0.475 | 0.017 | −0.515 | 0.016 | −0.193 | 0.010 |
| Age, baseline | 0.064 | 0.016 | 0.278 | 0.018 | 0.12 | 0.011 | ||||
| Interaction age*baseline | 0.095 | 0.016 | ||||||||
| Omni Cohort | 0.315 | 0.057 | ||||||||
| Interaction Omni*baseline | 0.317 | 0.061 | ||||||||
| Sex (female) | ||||||||||
| Total/HDL, baseline | ||||||||||
| Change Total/HDL | 0.145 | 0.016 | 0.092 | 0.019 | 0.045 | 0.010 | ||||
| Smoke, baseline | 0.269 | 0.048 | 0.196 | 0.050 | ||||||
| Body-mass index, baseline | 0.044 | 0.010 | ||||||||
| Change in body-mass index | 0.078 | 0.015 | 0.040 | 0.010 | ||||||
| Lipid therapy, baseline | −0.296 | 0.037 | ||||||||
| Start lipid therapy | −0.320 | 0.035 | ||||||||
| Hormone replacement therapy, baseline | 0.095 | 0.024 | ||||||||
| Hormone replacement therapy Start | 0.109 | 0.026 | ||||||||
| Hormone replacement therapy, Stop | ||||||||||
| Diastolic blood pressure, baseline | −0.053 | 0.012 | ||||||||
| Change in diastolic blood pressure | −0.089 | 0.011 | ||||||||
| Waist circumference, baseline | ||||||||||
| Change in Waist circumference | 0.077 | 0.015 | ||||||||
| Triglyceride, baseline | 0.061 | 0.014 | ||||||||
| Change in triglyceride | 0.092 | 0.022 | ||||||||
| Diabetes, new-onset | 0.324 | 0.051 | ||||||||
| Adjusted R-squared | 0.520 | 0.297 | 0.311 | 0.309 | 0.280 | |||||
We accounted for demographic factors (age, sex, cohort status) in all models. For most biomarkers, the changes in biomarker concentrations were similar for men and women. However, sICAM-1 and isoprostanes serially increased more in women compared to men (β = 0.127, SE = 0.132; β = 0.234, SE = 0.028, respectively). Older age at the baseline examination was associated with increasing concentrations of biomarkers for six of the biomarkers, including CRP, interleukin-6, sICAM-1, MCP-1, osteoprotegerin and TNFRII, with osteoprotegerin increasing the most with older participant age (β = 0.278, SE = 0.018).
Anthropometric factors and smoking status also were associated with longitudinal changes in biomarker concentrations. For instance, for waist circumference the baseline (interleukin-6) and serial increase (interleukin-6, P-selectin) were associated with higher inflammatory markers at follow-up. Similarly, both baseline (CRP and TNFRII) and serial increases (CRP, MCP-1, and TNFRII) in body-mass index also were associated with increasing concentrations in biomarkers. Smoking at the baseline examination was associated with increased concentration of many of the biomarkers (CRP, interleukin-6, sICAM-1, isoprostanes, Lp-PLA2-mass, and osteoprotegerin) at follow-up.
Lipid concentrations and lipid treatment were associated with longitudinal changes in several biomarkers. Baseline (sICAM-1, Lp-PLA2 activity), and increasing total/HDL ratio (CRP, sICAM-1, Lp-PLA2 activity and mass, P-selectin and TNFRII) or higher baseline triglycerides (P-selectin) were associated with increasing concentrations of the biomarkers at follow-up. Conversely, lipid-lowering treatment either at the index examination or on follow-up was associated with decreased concentration of CRP and Lp-PLA2 activity and mass (Table 4).
A few risk factors were only associated with one or two biomarker levels. For instance, baseline and change in diastolic blood pressure were associated with declining TNFRII concentrations. Similarly, baseline and starting hormone replacement therapy were associated with increasing mean TNFRII concentrations. New diabetes was associated with increasing osteoprotegerin concentrations.
Despite the cross-sectional associations with isoprostanes, interleukin-6 and TNFRII (eTable 3), heavy alcohol consumption, and antihypertensive treatment were not associated with change in biomarkers. Prevalent CVD and aspirin use also were not associated with change in inflammatory biomarker concentrations.
The adjusted R-squared depicts the amount of variability in the change in biomarker concentrations explained by baseline biomarker levels and baseline and change in clinical risk factors. We observed that the clinical risk factors explained a moderate amount of variability of the change in biomarker concentrations between two consecutive examinations. Change in TNFRII over follow-up had the least amount of variability explained by the clinical factors (r2 = 0.280), and serial Lp-PLA2-mass had the highest (r2 = 0.52).
4. Discussion
In our large community-based sample we observed the following main findings. First, not surprisingly, for each biomarker, baseline inflammatory biomarker concentration explained the largest amount of variability in longitudinal change in its level. The baseline concentration was the only factor associated with serial change in every biomarker. Mean baseline concentrations were negatively associated with biomarker change. Second, older age at baseline was associated with increased follow-up concentration in the majority of biomarkers (CRP, interleukin-6, sICAM-1, MCP-1, osteoprotegerin and isoprostanes). Third, anthropometric factors were associated with progressive increases in mean inflammatory biomarker concentrations including baseline body-mass index (CRP, TNFRII) and waist circumference (interleukin-6), as well as serial increases in body-mass index (CRP, MCP-1 and TNFRII) and increase in waist circumference (interleukin-6, P-selectin). Fourth, smoking at the baseline examination was associated with longitudinal increases in more than half of the biomarkers (CRP, interleukin-6, sICAM-1, isoprostanes, Lp-PLA2-mass, and osteoprotegerin). Fifth, except for MCP-1 and osteoprotegerin, high lipid levels (or worsening of lipid profile on follow-up) also were commonly associated with increasing concentrations of biomarkers over time, as opposed to lipid medications that were associated with declining concentrations of biomarkers. Finally, CVD risk factors explained only a moderate amount of the longitudinal change in a panel of inflammatory biomarkers.
By exponentiating beta coefficients from multivariable models, we can estimate the expected change of the ratio of biomarker concentration of follow-up over the baseline concentration. For example, for CRP, corresponding with analysis of raw data (not shown), holding all the clinical covariates constant (assuming no change in clinical covariates statistically associated with change of CRP), participants who stopped hormone replacement therapy would have an estimated relative ~30% decrease in CRP concentrations, relative to individuals who did not stop hormone replacement therapy. Similarly, participants who were smokers at baseline had a ~35% increase in CRP concentrations, as compared to individuals who were not smokers, assuming no change in other clinical covariates.
As shown in Table 3, we observed weak-to-modest correlations of baseline levels of biomarkers and change in concentration of biomarkers on follow-up. A priori, we expected only weak correlations between biomarkers at baseline, as we selected the biomarkers to represent different biological pathways. Interestingly, the lack of a stronger correlation of change in biomarkers over time suggests that factors associated with change of inflammation are specific to each individual marker, which is further supported by the data in Table 3.
There are several potential explanations for the observed lower concentrations of several biomarkers on follow-up examination. One possible explanation is that there was a substantial increase in medical therapies for hypertension, hypercholesterolemia and prevention of CVD with aspirin from our index examination to the follow-up examination. Participants with higher concentrations of biomarkers at baseline had higher risk profiles, thus were more likely to receive new or more intensive drug therapies. Another potential explanation for lower concentrations on follow-up is regression to the mean.
The inflammatory biomarkers we report have been related to incident CVD events. For instance, CRP, interleukin-6, sICAM-1, isoprostanes and P-selectin have been related to new-onset MI; Lp-PLA2 and osteoprotegerin have been related to incident heart failure; CRP has been related to incident stroke, and CRP, sICAM-1 and osteoprotegerin have been associated with incident atrial fibrillation and progression of peripheral arterial disease [7, 17–30]. Whereas prior reports have focused on relating CVD risk factors cross-sectionally to inflammatory biomarkers, we sought to examine the relation of changing risk factors to progression of systemic inflammation. Identifying elements that promote systemic inflammation may offer insights into the development of CVD, thus suggesting targets for CVD prevention.
Despite the low prevalence of smoking behavior in our cohort, a central finding of our study is that smoking behavior is fundamentally associated with systemic inflammation [31, 32]. Cigarette smoking was associated with inflammatory biomarkers cross-sectionally at both examinations (all biomarkers except TNFRII, and MCP-1 at the follow-up examination, eTable 3). Similarly smoking at baseline was associated with longitudinal increases in most of the biomarkers (all but Lp-PLA2 activity, MCP-1, P-selectin and TNFRII). Although our data are observational and only 2% of participants stopped smoking between the two consecutive examinations, the associations suggest that one beneficial mechanism of smoking cessation may be declining levels of systemic inflammation.
Cross-sectional and longitudinal human and experimental data have consistently demonstrated that measures of adiposity are associated with inflammatory biomarkers [33–38]. Considering the obesity epidemic, the associations between weight gain and inflammation are concerning. Weight gain, reflected by both increases in body-mass index or increases in waist circumference, was associated with rising concentrations in multiple inflammatory biomarkers.
Our data are in line with literature suggesting that worsening of lipid profile is associated with increased burden of inflammation and the treatment with lipid-lowering medications is associated with lower concentrations of inflammatory biomarkers. For instance, experimental data show that mice fed with high-fat diets have higher levels of P-selectin and Lp-PLA2-mass [39, 40]. Large observational and experimental studies have suggested that the presence of hyperlipidemia is associated with inflammation and atherosclerosis [41, 42]. Recent interventional trials have shown the effect of lipid-lowering medications on biomarkers of inflammation, suggesting a causal link between lipid treatment and reduction of inflammation [43].
There are several possible explanations as to why our data reflected that blood pressure measures had little association with progression of inflammatory biomarkers. We only observed that baseline and increasing diastolic blood pressure were associated with declining TNFRII concentrations. It should be noted that the longitudinal change in blood pressure was very mild (a mean increase of 2–3 mmHg, Table 1). In addition, the relation of blood pressure to change in concentration of biomarkers may have been accounted for by other clinical factors in the stepwise exclusion model. The associations of increase in blood pressure with higher inflammation may have been counterbalanced by the increase in hypertension treatment between the two examinations. It is also possible that blood pressure and hypertension treatment are not associated with increased inflammation; however, this is less likely given cross-sectional and longitudinal data supporting such a relation [44, 45].
Whereas clinical factors explained between 28% (TNFRII) and 52% (Lp-PLA2-mass) of the variability in inflammatory markers, much of the variability in cross-sectional and longitudinal changes in systemic inflammation remains unexplained. There are many potential contributors to the unexplained variability in measures of systemic inflammation. We acknowledge that measurement variability may play a role. In addition, although we examined baseline and change in multiple clinical covariates, there are additional factors we did not include in our models, such as physical activity and psychosocial factors. The substantial unexplained variation in inflammatory marker concentrations suggests that there are individual and unique components in the development of CVD. Focusing on unknown factors related to inflammation may lead to the discovery of modifiable factors of inflammation and CVD incidence. Finally, we and other investigators have noted that genetic factors contribute to some of the inter-individual variation in systemic inflammatory markers [15, 46].
Cardiovascular risk factors have been associated cross-sectionally with concentrations of inflammatory biomarkers in many prior publications [33, 47–50], which we confirmed in our cross-sectional evaluations of the two consecutive examination cycles (eTable 2). Although our group and others have examined serial CRP measurements, to the best of our knowledge, this is the largest longitudinal study of factors associated with the progression of multiple inflammatory biomarkers in a community-based cohort [8, 51]. Additionally, the study was conducted with routinely and rigorously ascertained biomarkers and clinical risk factors.
The present study has several limitations. We cannot infer causal relations between the covariates and the change in biomarkers given the observational nature of the study. Second, due to the numerous covariates and biomarkers examined in our study, we acknowledge multiple statistical testing, which we addressed by employing a Bonferroni correction for a p-value of 0.0001 (0.05 divided by 15 covariates). Third, because we needed to account for multiple testing, we also acknowledge that in a larger data set, additional clinical covariates may have been associated with longitudinal change in inflammatory biomarkers for all but isoprostanes we had 80% power to detect a true partial correlation of 0.076 or larger in absolute value between clinical variables with change in ln(biomarker). Fourth, the time interval between examinations (~7 years) was intermediate and we measured the panel of biomarkers on only two occasions; we may have failed to detect factors associated with change in systemic inflammation over shorter or longer time frames. Fifth, concerns regarding the generalizability of the data must be acknowledged. Our sample was middle-aged to elderly at baseline; we may not be able to extrapolate these findings to other age groups. The small sample size, the mixed ethnic/racial composition of the Omni Cohort and the non-fasting collection on the first examination cycle markedly limited our ability to identify the relation between ethnic/racial variation and longitudinal changes in inflammatory biomarkers. The different patterns of change in concentration of inflammatory biomarkers between the Omni and Offspring Cohorts may reflect the difference in blood collection on the Omni’s baseline examination, rather than true biological effects. Given the small sample sizes, ethnic/racial variation, and differences in technique, we acknowledge our Omni data are hypothesis generating. Further studies are necessary to clarify the relations between ethnic/racial variation and change in biomarkers over time.
In our longitudinal community-based study, we describe the clinical covariates associated with change in inflammatory biomarkers over follow-up. Given the potential for the use of serial biomarker measurements in clinical practice, it is imperative to appreciate the factors involved with their change. Thus, it is important to highlight that traditional clinical risk factors explained a moderate amount of change in the inflammatory biomarkers. The relations between cigarette smoking, lipids and lipid therapies, and anthropometry and longitudinal progression of systemic inflammation provide indirect support for preventive cardiovascular risk factor modification. However, much of the variability in biomarker concentrations remains unexplained. Further studies are necessary to enhance our knowledge of the mechanisms responsible for, and therapies that will effectively protect against, the progression of systemic inflammation.
Supplementary Material
Acknowledgments
Grants
Work supported by the following NIH grants: NHLBI core contact N01-HC 25195; RO1HL064753, RO1HL076784, RO1AG028321 (EJB). Dr. Rienstra is supported by a grant from the Netherlands Organization for Scientific Research (Rubicon Grant 825.09.020).
The authors would like to thank Moira Pride for her support and help preparing the biomarkers manual.
Footnotes
Conflict of interest
Lp-PLA2 activity measurements were provided by GlaxoSmithKline and mass measurements by diaDexus at no cost to the FHS.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.atherosclerosis.2013.01.019.
References
- 1.Wilson PW, Nam BH, Pencina M, et al. C-reactive protein and risk of cardiovascular disease in men and women from the Framingham Heart Study. Arch Intern Med. 2005;165:2473–2478. doi: 10.1001/archinte.165.21.2473. [DOI] [PubMed] [Google Scholar]
- 2.Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers and the risk of incident hypertension. Hypertension. 2007;49:432–438. doi: 10.1161/01.HYP.0000256956.61872.aa. [DOI] [PubMed] [Google Scholar]
- 3.Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–874. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]
- 4.Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation. 2006;113:2335–2362. doi: 10.1161/CIRCULATIONAHA.104.482570. [DOI] [PubMed] [Google Scholar]
- 5.Koenig W, Sund M, Frohlich M, et al. C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99:237–242. doi: 10.1161/01.cir.99.2.237. [DOI] [PubMed] [Google Scholar]
- 6.Kugiyama K, Ota Y, Takazoe K, et al. Circulating levels of secretory type II phospholipase A(2) predict coronary events in patients with coronary artery disease. Circulation. 1999;100:1280–1284. doi: 10.1161/01.cir.100.12.1280. [DOI] [PubMed] [Google Scholar]
- 7.Pradhan AD, Rifai N, Ridker PM. Soluble intercellular adhesion molecule-1, soluble vascular adhesion molecule-1, and the development of symptomatic peripheral arterial disease in men. Circulation. 2002;106:820–825. doi: 10.1161/01.cir.0000025636.03561.ee. [DOI] [PubMed] [Google Scholar]
- 8.Chen TH, Gona P, Sutherland PA, et al. Long-term C-reactive protein variability and prediction of metabolic risk. Am J Med. 2009;122:53–61. doi: 10.1016/j.amjmed.2008.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farzadfar F, Finucane MM, Danaei G, et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet. 2011;377:578–586. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- 10.Danaei G, Finucane MM, Lin JK, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 11.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kannel WB, Feinleib M, McNamara PM, et al. An investigation of coronary heart disease in families. The Framingham Offspring Study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 13.Splansky GL, Corey D, Yang Q, et al. The third generation cohort of the national heart, lung, and blood institute’s Framingham heart study: design, recruitment, and initial examination. Am J Epidemiol. 2007;165:1328–1335. doi: 10.1093/aje/kwm021. [DOI] [PubMed] [Google Scholar]
- 14.Schnabel R, Larson MG, Dupuis J, et al. Relations of inflammatory biomarkers and common genetic variants with arterial stiffness and wave reflection. Hypertension. 2008;51:1651–1657. doi: 10.1161/HYPERTENSIONAHA.107.105668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnabel RB, Lunetta KL, Larson MG, et al. The relation of genetic and environmental factors to systemic inflammatory biomarker concentrations. Circ Cardiovasc Genet. 2009;2:229–237. doi: 10.1161/CIRCGENETICS.108.804245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schnabel R, Larson MG, Dupuis J, et al. Relations of inflammatory biomarkers and common genetic variants with arterial stiffness and wave reflection. Hypertension. 2008 doi: 10.1161/HYPERTENSIONAHA.107.105668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schnabel RB, Larson MG, Yamamoto JF, et al. Relation of multiple inflammatory biomarkers to incident atrial fibrillation. Am J Cardiol. 2009;104:92–96. doi: 10.1016/j.amjcard.2009.02.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ridker PM, Rifai N, Stampfer MJ, et al. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101:1767–1772. doi: 10.1161/01.cir.101.15.1767. [DOI] [PubMed] [Google Scholar]
- 19.Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108:3006–3010. doi: 10.1161/01.CIR.0000103131.70301.4F. [DOI] [PubMed] [Google Scholar]
- 20.Ridker PM, Cushman M, Stampfer MJ, et al. Plasma concentration of C-reactive protein and risk of developing peripheral vascular disease. Circulation. 1998;97:425–428. doi: 10.1161/01.cir.97.5.425. [DOI] [PubMed] [Google Scholar]
- 21.Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 22.Hwang SJ, Ballantyne CM, Sharrett AR, et al. Circulating adhesion molecules VCAM-1, sICAM-1, and E-selectin in carotid atherosclerosis and incident coronary heart disease cases: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 1997;96:4219–4225. doi: 10.1161/01.cir.96.12.4219. [DOI] [PubMed] [Google Scholar]
- 23.Schwedhelm E, Bartling A, Lenzen H, et al. Urinary 8-iso-prostaglandin F2alpha as a risk marker in patients with coronary heart disease: a matched case-control study. Circulation. 2004;109:843–848. doi: 10.1161/01.CIR.0000116761.93647.30. [DOI] [PubMed] [Google Scholar]
- 24.Packard CJ, O’Reilly DS, Caslake MJ, et al. Lipoprotein-associated phospholipase A2 as an independent predictor of coronary heart disease. West of Scotland Coronary Prevention Study Group. N Engl J Med. 2000;343:1148–1155. doi: 10.1056/NEJM200010193431603. [DOI] [PubMed] [Google Scholar]
- 25.Omland T, Ueland T, Jansson AM, et al. Circulating osteoprotegerin levels and long-term prognosis in patients with acute coronary syndromes. J Am Coll Cardiol. 2008;51:627–633. doi: 10.1016/j.jacc.2007.09.058. [DOI] [PubMed] [Google Scholar]
- 26.Ridker PM, Buring JE, Rifai N. Soluble P-selectin and the risk of future cardiovascular events. Circulation. 2001;103:491–495. doi: 10.1161/01.cir.103.4.491. [DOI] [PubMed] [Google Scholar]
- 27.Suzuki T, Solomon C, Jenny NS, et al. Lipoprotein-associated phospholipase A(2) and risk of congestive heart failure in older adults: the Cardiovascular Health Study. Circ Heart Fail. 2009;2:429–436. doi: 10.1161/CIRCHEARTFAILURE.108.839613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ueland T, Jemtland R, Godang K, et al. Prognostic value of osteoprotegerin in heart failure after acute myocardial infarction. J Am Coll Cardiol. 2004;44:1970–1976. doi: 10.1016/j.jacc.2004.06.076. [DOI] [PubMed] [Google Scholar]
- 29.Nambi V, Hoogeveen RC, Chambless L, et al. Lipoprotein-associated phospholipase A2 and high-sensitivity C-reactive protein improve the stratification of ischemic stroke risk in the Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 2009;40:376–381. doi: 10.1161/STROKEAHA.107.513259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vasan RS, Sullivan LM, Roubenoff R, et al. Inflammatory markers and risk of heart failure in elderly subjects without prior myocardial infarction: the Framingham Heart Study. Circulation. 2003;107:1486–1491. doi: 10.1161/01.cir.0000057810.48709.f6. [DOI] [PubMed] [Google Scholar]
- 31.Halvorsen B, Lund Sagen E, Ueland T, et al. Effect of smoking cessation on markers of inflammation and endothelial cell activation among individuals with high risk for cardiovascular disease. Scand J Clin Lab Invest. 2007;67:604–611. doi: 10.1080/00365510701283878. [DOI] [PubMed] [Google Scholar]
- 32.Levitzky YS, Guo CY, Rong J, et al. Relation of smoking status to a panel of inflammatory markers: the Framingham Offspring. Atherosclerosis. 2008;201:217–224. doi: 10.1016/j.atherosclerosis.2007.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pou KM, Massaro JM, Hoffmann U, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116:1234–1241. doi: 10.1161/CIRCULATIONAHA.107.710509. [DOI] [PubMed] [Google Scholar]
- 34.Park HS, Park JY, Yu R. Relationship of obesity and visceral adiposity with serum concentrations of CRP, TNF-alpha and IL-6. Diabetes Res Clin Pract. 2005;69:29–35. doi: 10.1016/j.diabres.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 35.Festa A, D’Agostino R, Jr, Williams K, et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord. 2001;25:1407–1415. doi: 10.1038/sj.ijo.0801792. [DOI] [PubMed] [Google Scholar]
- 36.Robker RL, Collins RG, Beaudet AL, et al. Leukocyte migration in adipose tissue of mice null for sICAM-1 andMac-1 adhesion receptors. Obes Res. 2004;12:936–940. doi: 10.1038/oby.2004.114. [DOI] [PubMed] [Google Scholar]
- 37.Esposito K, Pontillo A, Di Palo C, et al. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. J Am Med Assoc. 2003;289:1799–1804. doi: 10.1001/jama.289.14.1799. [DOI] [PubMed] [Google Scholar]
- 38.Selvin E, Paynter NP, Erlinger TP. The effect of weight loss on C-reactive protein: a systematic review. Arch Intern Med. 2007;167:31–39. doi: 10.1001/archinte.167.1.31. [DOI] [PubMed] [Google Scholar]
- 39.Sakai A, Kume N, Nishi E, et al. P-selectin and vascular cell adhesion molecule-1 are focally expressed in aortas of hypercholesterolemic rabbits before intimal accumulation of macrophages and T lymphocytes. Arterioscler Thromb Vasc Biol. 1997;17:310–316. doi: 10.1161/01.atv.17.2.310. [DOI] [PubMed] [Google Scholar]
- 40.Ivandic B, Castellani LW, Wang XP, et al. Role of group II secretory phospholipase A2 in atherosclerosis: 1. Increased atherogenesis and altered lipoproteins in transgenic mice expressing group IIa phospholipase A2. Arterioscler Thromb Vasc Biol. 1999;19:1284–1290. doi: 10.1161/01.atv.19.5.1284. [DOI] [PubMed] [Google Scholar]
- 41.Li H, Cybulsky MI, Gimbrone MA, Jr, et al. An atherogenic diet rapidly induces VCAM-1, a cytokine-regulatable mononuclear leukocyte adhesion molecule, in rabbit aortic endothelium. Arterioscler Thromb. 1993;13:197–204. doi: 10.1161/01.atv.13.2.197. [DOI] [PubMed] [Google Scholar]
- 42.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 43.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N.Engl.J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 44.Bautista LE. Inflammation, endothelial dysfunction, and the risk of high blood pressure: epidemiologic and biological evidence. J Hum Hypertens. 2003;17:223–230. doi: 10.1038/sj.jhh.1001537. [DOI] [PubMed] [Google Scholar]
- 45.Ridker PM, Danielson E, Rifai N, et al. Valsartan, blood pressure reduction, and C-reactive protein: primary report of the Val-MARC trial. Hypertension. 2006;48:73–79. doi: 10.1161/01.HYP.0000226046.58883.32. [DOI] [PubMed] [Google Scholar]
- 46.Dehghan A, Dupuis J, Barbalic M, et al. Meta-analysis of genome-wide association studies in >80 000 subjects identifies multiple loci for C-reactive protein levels. Circulation. 2011;123:731–738. doi: 10.1161/CIRCULATIONAHA.110.948570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ridker PM, Hennekens CH, Rifai N, et al. Hormone replacement therapy and increased plasma concentration of C-reactive protein. Circulation. 1999;100:713–716. doi: 10.1161/01.cir.100.7.713. [DOI] [PubMed] [Google Scholar]
- 48.van der Vaart H, Postma DS, Timens W, et al. Acute effects of cigarette smoke on inflammation and oxidative stress: a review. Thorax. 2004;59:713–721. doi: 10.1136/thx.2003.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keaney JF, Jr, Larson MG, Vasan RS, et al. Obesity and systemic oxidative stress: clinical correlates of oxidative stress in the Framingham Study. Arterioscler Thromb Vasc Biol. 2003;23:434–439. doi: 10.1161/01.ATV.0000058402.34138.11. [DOI] [PubMed] [Google Scholar]
- 50.Murabito JM, Keyes MJ, Guo CY, et al. Cross-sectional relations of multiple inflammatory biomarkers to peripheral arterial disease: the Framingham Offspring Study. Atherosclerosis. 2009;203:509–514. doi: 10.1016/j.atherosclerosis.2008.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Currie CJ, Poole CD, Conway P. Evaluation of the association between the first observation and the longitudinal change in C-reactive protein, and all-cause mortality. Heart. 2008;94:457–462. doi: 10.1136/hrt.2007.118794. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.