Abstract
Background:
Renal transplantation is the preferred therapy to extend life expectancy and quality of life for patients with chronic kidney disease. There are many barriers in the process of live kidney donation that prevent the timely progression from organ requirement to transplantation, including the progression of the live donor through a medical evaluation. We assess how easily patients complete the donor workup, how often the medical evaluation identifies significant incidental findings, and which surgical procedure is planned for organ retrieval.
Methods:
We reviewed our donor database and the minutes from our multidisciplinary rounds from 2002 to 2008 to assess how medical, radiological and psychological findings were used to decide on the candidacy of potential donors.
Results:
Half (50.2%) of patients did not pass the initial health screen. Of the 467 patients who progressed beyond the health screen to the computed tomographic angiogram evaluation, 48 (10.3%) were excluded as donors and 419 (89.7%) were accepted. Of those accepted, 136 (32.5%) were conditional on further medical workup. Of the patients accepted (n=419), 375 (89.5%) were planned for laparoscopic left-sided approach.
Conclusions:
The vast majority of patients who passed the initial health screen for kidney donation will be accepted as donors, but about one-third will require further workup. It is rare to identify life-threatening disease on screening computerized tomographic angiograph for kidney donor workup.
Introduction
Living-donor renal transplantation is the preferred treatment for end-stage renal disease; it is established as a safe procedure with excellent graft survival.1,2 Recent long-term prospective data suggest that overall survival and risk of developing chronic kidney disease in kidney donors is similar to the general population. In addition, kidney donors experience excellent quality of life.1 Although living donors represent more than half of the renal transplants performed in North America, there is still a wide gap between the need and availability of transplantable organs. Transplant centres are using several strategies to increase organ availability, including broadening medical acceptance criteria. A 2007 survey of transplant centres demonstrated that older, more obese, hypertensive and non-related patients are more likely to be accepted as donors compared to the previous decade.3–5 Long-term health outcomes for extended-criteria donors are less clear.4 In an attempt to make the donor screening process consistent, several consensus statements outlining the medical and psychosocial evaluation exist.6 However, discrepancies between practices of donor sites persist.3,4,7
The use of computed tomographic angiography (CTA) to assess the quality of donor kidneys and the renal vasculature is part of the donor workup.3,5,8 There are inherent risks associated with the medical and radiological evaluation itself, including incidental pathological findings and the emotional impact of being turned down for donation.7 One review of 1600 potential donors demonstrated that 49% were excluded for medical and ethical reasons.2
In our study, the medical and psychological workup and surgical planning for potential kidney donors at our institution was reviewed. To limit the radiation and contrast exposure for patients unlikely to be accepted as donors, CTA is limited to patients having passed the two-step preliminary health screen (Fig. 1). In this process, potential donors are first interviewed to screen for any contraindications to kidney donation, including a history of cancer, heart disease, diabetes, hepatitis or hypertension. Our centre has a body mass index (BMI) limit of 35 for donor nephrectomy. Donors and recipients must also have matching blood groups to pass the first step, unless seeking paired exchange, which has been available at our centre since 2004. The second step includes counselling by nephrology and social work, routine serologic and urinary tests, cardiac examinations and abdominal ultrasound.
Fig. 1.
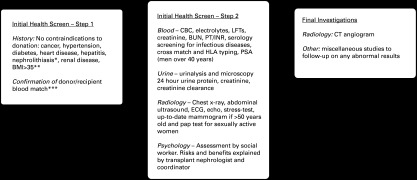
Flow diagram depicting the screening process for living-related kidney donation at St. Michael’s Hospital. *Patients with incidental, asymptomatic stones <5 mm on imaging are eligible only if >30 years old, normal metabolic workup and no recurrent stones. **Patients with a body mass index >35 are allowed to proceed to computerized tomographic angiograph only if a weight-loss plan is ongoing and successful. ***Blood type incompatible pairs can be considered for the national paired exchange program.
We report the likelihood of accepting potential donors after progressing to the final radiological portion of the workup, and the type of operation planned for their donor nephrectomy. We are interested in providing potential donors, recipients and transplant programs accurate data regarding the chance that they will be accepted immediately, pending other investigations, or rejected based on their medical and radiological workup.
Methods
The St. Michael’s kidney donor database was used to identify the total number of patients who came forward as potential donors, but who did not progress beyond the 2-step health screen from 2007 to 2008. Records on potential donors failing the screen do not exist prior to 2007.
To evaluate the progress of patients who passed the health screen, a retrospective review of the documented minutes from donor “CTA rounds” was conducted from March 2002 to December 2008. Members of our multidisciplinary kidney donor team, including transplant nephrologists, donor and recipient urologists, radiologists and transplant coordinators, meet at these monthly rounds to review patient appropriateness for kidney donation based on medical, psychological and final radiological workup. Reasons for exclusion, delay or acceptance for kidney donation, and the proposed organ retrieval surgical technique (right or left, laparoscopic or open, with or without vascular reconstruction) were recorded from the transcribed CTA round minutes. Several patients were discussed at more than one meeting, so care was taken to document each patient only once. Any discrepancies between entries or missing data were clarified by chart review.
The reasons for donor exclusion were grouped by urologic, medical, surgical and psychosocial domains. The reasons for donor delay were also tabulated and separated into several similar categories. The presumed need for re-imaging was addressed by combining all patients with incidentally discovered masses with patients where the radiology service suggested further imaging for any reason.
Results
In 2007 and 2008 combined, 241 patients presented as possible kidney donors. Of these, 121 were rejected due to results from the 2-step health screen and did not receive a CTA (50.2%). There were 467 prospective kidney donors that proceeded to CTA rounds from March 2002 to December 2008. The female to male ratio was about 2:1. The annual median number of patients reviewed at rounds was 71.
Overall, 48 patients (10.3%) were deemed unsuitable for donor nephrectomy at CTA rounds. Three quarters of these rejections were based on urologic concerns demonstrated on CTA, which included stones, complex renal vasculature, renal anatomic variability and incidental urologic malignancy (Fig. 2). Medical and other surgical causes were less common sources for donor rejection. Elevated BMI and other complex medical issues, such as newly diagnosed hypertension and metabolic syndrome, comprised 18.7% of the rejections.
Fig. 2.
Flow chart outlining the number of patients accepted and rejected as kidney donors after being reviewed at computerized tomographic angiograph rounds. The reasons for donor rejection are categorized.
In total, 419 (89.7%) prospective kidney donors were accepted into the SMH kidney donation program and planned for donor nephrectomy after complete workup. Based on renal vasculature and anatomy, patients were scheduled for either laparoscopic or open donor nephrectomy. Left laparoscopic nephrectomy was the most common procedure selected for prospective donors (89.5%) (Fig. 3). Of the patients selected for laparoscopic nephrectomy, 66 (16.8%) would require planned intraoperative vascular reconstruction for multiple renal arteries.
Fig. 3.
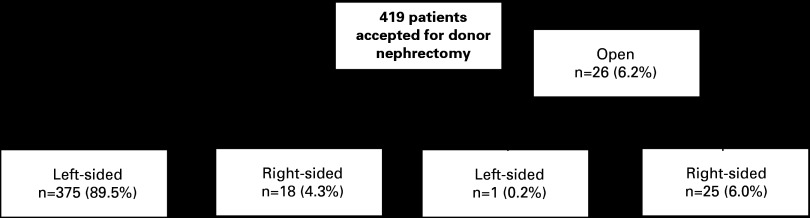
Planned surgical approach for donor nephrectomy of 419 patients accepted as live renal donors from 2002 to 2008 based on computerized tomographic angiograph anatomy.
Of the 419 patients accepted for donor nephrectomy, 136 (32.5%) acceptances pended further workup (Table 1). Detailed urologic workup was the most common cause of deferral (46.3%), and was most often performed for small stones, microscopic hematuria, incidental renal and adrenal masses and small kidneys. Other common reasons for nephrectomy deferral were social concerns, medicine consultation, incidental liver cysts and abnormal electrocardiograms.
Table 1.
Causes for deferral of live kidney donation based on computerized tomographic angiograph findings for 136 patients
| Reason for deferral | Most common causes |
|---|---|
| Urologic 63 patients |
|
| Medical 41 patients |
|
| Other surgical 20 patients |
|
| Psychosocial 9 patients Radiology review 3 patients |
Based on causes for deferral and rejection, we estimate that 52/467 (11.1%) patients would require further imaging following their full donor screen.
Discussion
Our 7-year review demonstrates the usual progression of patients through the process of kidney donor evaluation. At our centre, a key step in the evaluation of potential donors occurs at CTA rounds, where specialists from our multi-disciplinary live-renal donor team meet to discuss donor eligibility. In our series, although about half of potential donors did not pass initial screen, only 1 in 10 patients were rejected as donors afterwards. Additionally, in two-thirds of cases no concerning incidental findings were encountered and further testing was not required.
Women were twice as likely as men to come forward as potential donors in our cohort. This gender difference is greater than previously published.10 Gender differences are also present in transplant recipients, where men are more likely to receive a living-related donation. It is unclear exactly what is driving the disparity, although physician gender-bias has been suggested.11 It is possible that because women are commonly the emotional and physical caregivers in families, they are more likely to support a partner by donating an organ. This is an area deserving further study.
There were 4 patients in our cohort (0.8%) with incidentally identified malignancies requiring intervention. Their specific diagnoses were prostate cancer, renal cell carcinoma, schwannoma and lung cancer. The prognosis for these patients is unknown, and we cannot assume that incidental, early detection improved their survival. However, we demonstrated that the likelihood of identifying life-threatening disease on screening CTA is very low. We hope that this statistic can be shared with potential donors who may be anxious in this regard.
Reflecting the preferences of our surgeons to extract a longer renal vein for transplantation, left laparoscopic donor nephrectomy was performed for 89.5% of patients. Also, our practice prioritized laparoscopic surgery over open surgery first and then left-sided over right-sided second. For example, a laparoscopic left nephrectomy would be performed over a right-sided approach even if vascular reconstruction were required on the left side. Surprisingly, there were still 25 patients (6% of overall accepted patients) with planned open, right-sided nephrectomy. Most of these cases were performed open due to complex bilateral renal vasculature, commonly multiple left-sided arteries that bifurcated near the aorta in addition to multiple right-sided vessels. Interestingly, in the last 3 years of our study period (2006–2008), only 4 patients were planned for right-sided retrieval, likely due to improved laparoscopic techniques over time. As demonstrated in our review, vascular reconstruction is a common undertaking by our transplant urologists (17% of patients). Kidneys with more than 3 renal arteries were not deemed suitable for transplantation.
Our dataset from 2002 to 2008 was a time of evolution in acceptance-criteria for live renal donors in many programs. Exclusion criteria for donation at our centre includes diabetes, impaired glucose tolerance, proteinuria, BMI >35 or hypertension. We do allow patients with asymptomatic, small nephrolithiasis to donate. A survey performed by Mandelbrot and colleagues in 2007 demonstrated that 50% of programs use a BMI cutoff of 35. While 50% of programs allowed donation for hypertensive patients controlled on 1 medication, some programs allow patients on 2 or more antihypertensive medications. A quarter of programs exclude patients with a history of renal stones, while another quarter accept these patients without requiring a metabolic workup.3 Our study results should be generalizable because our acceptance criteria are similar to many other programs.
In light of these broadening criteria, we expected to find an increase in our acceptance rate compared to older data. However, our overall acceptance rate for the 2 years of our study, where data was available on patients rejected during the 2-step screen, was 50.2%. This is unchanged from historic levels in the literature and is perhaps reflective of contemporary aggressive donor recruitment strategies.2 With broadening acceptance criteria for living donation, our program now considers donors with increased comorbidity who would previously not have been offered an initial health screen.
Maizlin and colleagues examined the economic impact of extra-renal findings during kidney donor CT evaluation.9 In their series, 49 (28%) patients required further imaging, which represented a mean increased cost of $35 for each screened patient. Our re-imaging rate was lower (11.1%), likely because our cohort received full abdominal ultrasound prior to CTA, while the comparison cohort only underwent renal ultrasound.
There are limitations to our study that affect its external validity. Our surgeons performed laparoscopic donor nephrectomy in all cases when possible. This may not be relevant to non-laparoscopic transplant programs. In addition, most of the information collected for the study was collected from CTA round-minutes. Thus, the quality of our data is restricted by the possibility of transcription error and transcription omission. In addition, direct comparison to other studies is difficult because rejections in other series are not tabulated both prior to and following CTA rounds.2 Finally, the variation between donor acceptability between kidney donation programs in Canada limits the generalizability of our data. Interestingly, this inconsistency has prompted the Canadian Blood Services Living Donor Advisory Committee to seek common guidelines for living donor acceptance criteria because proposed paired exchanges and chains have been delayed due to the resources required to approve donors worked up at different sites.
However, despite these limitations we feel that this study is important because it reflects our real experience evaluating potential donors. We hope that this can be a resource for kidney donor centres and potential kidney donors by making the donation process more transparent and aligning the expectations of patients with the experience of 467 patients who were previously in their position. In most cases, the task of finding a donor is left to the chronically ill recipient.5,12 By making the donation process more transparent, we hope that patients in need of transplant organs will be more likely to ask friends and family to donate, and that more potential donors will come forward.
Conclusion
Most patients who pass the initial health screen for potential kidney donation will be accepted as donors, but about one-third will require further workup. Most patients will undergo left laparoscopic donor nephrectomy. There is a very small chance that a life-threatening finding will be identified on CTA during workup for living related kidney donation.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation. N Engl J Med. 2009;360:459–69. doi: 10.1056/NEJMoa0804883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wafa EW, Donia AF, Ali-El-Dein B, et al. Evaluation and selection of potential live kidney donors. J Urol. 2004;171:1424–7. doi: 10.1097/01.ju.0000116431.65651.58. [DOI] [PubMed] [Google Scholar]
- 3.Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of living kidney donors: A survey of US transplant centres. Am J Transplant. 2007;7:2333–43. doi: 10.1111/j.1600-6143.2007.01932.x. [DOI] [PubMed] [Google Scholar]
- 4.Iordanous Y, Seymour N, Yound A, et al. Recipient Outcomes for Expanded Criteria Living Kidney Donors: The Disconnect Between Current Evidence and Practice. Am J Transplant. 2009;9:1558–73. doi: 10.1111/j.1600-6143.2009.02671.x. [DOI] [PubMed] [Google Scholar]
- 5.Davis CL, Delmonico FL. Living-Donor Kidney Transplantation: A review of the current practices for the live donor. J Am Soc Nephrol. 2005;16:2098–110. doi: 10.1681/ASN.2004100824. [DOI] [PubMed] [Google Scholar]
- 6.A Report of the Amsterdam Forum On the Care of the Live Kidney Donor: Data and Medical Guidelines. Transplantation. 2005;79:S53–S66. doi: 10.1097/01.TP.0000157343.27949.9F. [DOI] [PubMed] [Google Scholar]
- 7.Rodrigue JR, Pavlakis M, Danovitch GM, et al. Evaluating living kidney donors: Relationship types, psychosocial criteria, and consent process at US transplant programs. Am J Transplant. 2007;7:2326–32. doi: 10.1111/j.1600-6143.2007.01921.x. [DOI] [PubMed] [Google Scholar]
- 8.Hanninen EL, Denecke T, Stelter L, et al. Preoperative evaluation of living kidney donors using multirow detector computed tomography: comparison with digital subtraction angiography and intraoperative findings. Transpl Int. 2005;18:1134. doi: 10.1111/j.1432-2277.2005.00196.x. [DOI] [PubMed] [Google Scholar]
- 9.Maizlin ZV, Barnard SA, Gourlay WA, et al. Economic and ethical impact of extrarenal findings on potential living kidney donor assessment with computed tomography angiography. Transpl Int. 2007;20:338–42. doi: 10.1111/j.1432-2277.2006.00443.x. [DOI] [PubMed] [Google Scholar]
- 10.Kayler LK, Meier-Kriesche HU, Punch JD, et al. Gender imbalance in living donor renal transplantation. Transplantation. 2002;73:248–52. doi: 10.1097/00007890-200201270-00017. [DOI] [PubMed] [Google Scholar]
- 11.Jindal RM, Ryan JJ, Sajjad I, et al. Kidney Transplantation and Gender Disparity. Am J Nephrol. 2005;25:474–83. doi: 10.1159/000087920. [DOI] [PubMed] [Google Scholar]
- 12.Reese PP, Shea JA, Berns JS, et al. Recruitment of live donors by candidates for kidney transplantation. Clin J Am Soc Nephrol. 2008;3:1152–9. doi: 10.2215/CJN.03660807. [DOI] [PMC free article] [PubMed] [Google Scholar]