Abstract
Cancer education seminars for Appalachian populations were conducted to: (1) increase knowledge of existing cancer disparities, (2) disseminate findings from Appalachian community-based participatory research (CBPR) projects, and (3) foster CBPR capacity building among community members by promoting social networking. Evaluation of the seminars was completed by: (1) using pre–post-surveys to assess changes in knowledge and attitudes at three regional and one national seminar and (2) measuring a change in the social network patterns of participants at a national seminar by analyzing the names of individuals known at the beginning and at the end of the seminar by each participant. Among participants, there was a significant increase in knowledge of Appalachian cancer disparities at two seminars [national, t(145)=3.41, p=0.001; Pennsylvania, t(189)=3.00, p=0.003] and a change in attitudes about Appalachia at one seminar [Ohio t(193)=−2.80, p=0.006]. Social network analysis, operationally defined for this study as familiarity with individuals attending the conference, showed participation in the national seminar fostered capacity building for future CBPR by the development of new network ties. Findings indicate that short-term outcomes of the seminars were accomplished. Future educational seminars should consider using social network analysis as a new evaluation methodology.
Keywords: Appalachian region, Health disparities, Cancer
Introduction
Appalachia is a region of the USA that includes 420 counties in 13 states [1]. It follows the Appalachian mountains and extends more than 1,000 mi from southern New York to northern Mississippi [1]. A large percentage (42%) of the region’s population lives in rural areas compared to 20% of the population in the U.S. Appalachia, which once was dependent on mining, forestry, agriculture, and industry, and has developed a more diversified economy, but remains economically distressed with a higher percent of residents living in poverty, unemployed, and have lower educational attainment compared to national rates [1, 2]. In addition, residents of Appalachia have limited access to health services and experience many health disparities. A significant disparity among residents of Appalachia is the elevated cancer incidence, prevalence, and mortality rates (lung, colorectal, and cervical cancers) [3–8]. Contributing to the elevated cancer rates are many factors included in the various levels of the social determinants of health framework [9]. Examples of these factors are individual risk factors (e.g., decreased cancer screening rates, increased tobacco use), social context (e.g., social cohesion), social condition (e.g., culture), and institutional context (e.g., health care system) [10–15].
Measurement of contextual and social variables at multiple levels, such as the environment, neighborhood, community, and social network, is important to include in research that attempts to understand the mechanisms responsible for the cancer disparities among residents of Appalachia. To address the complex nature of this problem, community-based participatory research (CBPR) strategies have been used as the keystone for working in underserved Appalachian communities to address cancer risk factors (e.g., cancer screening rates, physical inactivity, and uptake of the HPV vaccine) [15–18]. The Appalachia Community Cancer Network (ACCN), one of the National Cancer Institute Community Network Program sites, has a mission to reduce cancer disparities in Appalachia through community participation in education, training, and research. The ACCN has established relationships with community leaders, researchers, clinicians, public health professionals, health and human service agencies, and universities across central Appalachia to accomplish its mission. To address ACCN’s mission, a series of seminars for community members and individuals interested in cancer disparities in Appalachia entitled “Addressing Health Disparities in Appalachia” were conducted in collaboration with ACCN’s partner institutions: the University of Kentucky, The Ohio State University, Pennsylvania State University, Virginia Polytechnic Institute, and West Virginia University.
The seminar series consisted of three regional and one national seminar. The educational objectives of the seminars were to increase knowledge of existing cancer disparities in Appalachia and to disseminate research findings from CBPR projects conducted in Appalachia. An additional objective of the national seminar was to foster capacity building among Appalachian community members for CBPR by promoting networking at the seminars. Evaluation of the Appalachian cancer disparities seminars was conducted to assess changes in knowledge and attitudes by analyzing pre–post-surveys of participants attending the four seminars. In addition, at the national seminar, a social network analysis was conducted among the participants prior to and at the end of the meeting to evaluate potentially new patterns of collaboration for future CBPR research. The purpose of the evaluation of the seminars was to determine if the short-term outcomes of the seminars would assist ACCN in reaching its long-term goal of reducing cancer disparities in Appalachia.
Methods
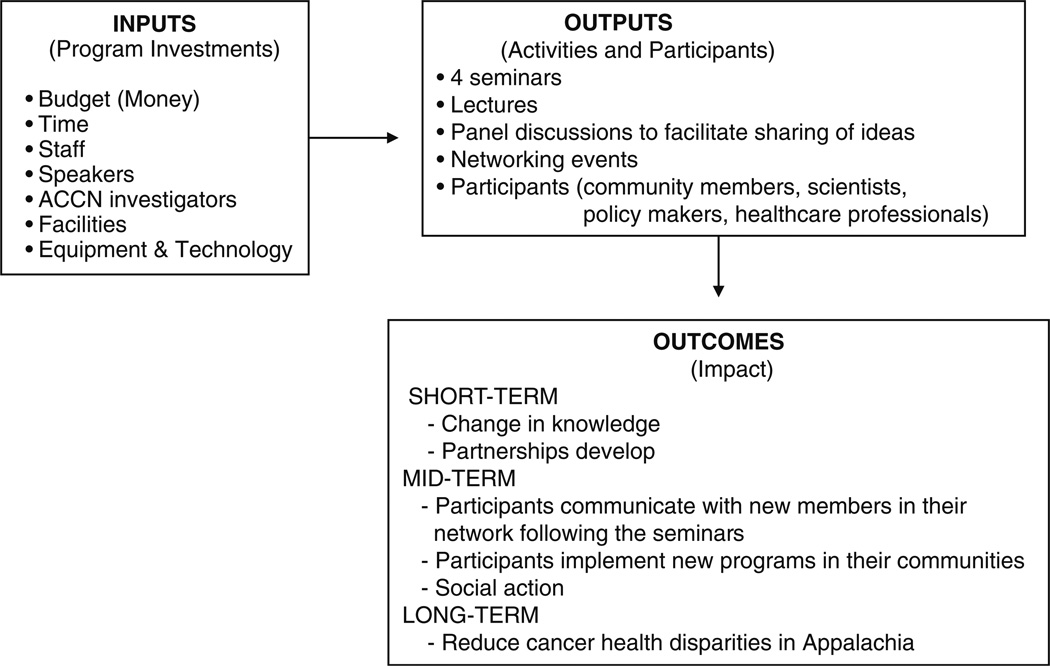
The process used for evaluation of the seminars is displayed in a logic model (Fig. 1). A pre–post-evaluation of all participants was conducted for each seminar. Three 1-day regional seminars were held in Kentucky (n=22), Ohio (n=120), and Pennsylvania (n=92). A 2.5-day national seminar was conducted in West Virginia (n=138). The seminars were conducted from October 2008 to September 2009 and were hosted by one of the ACCN-affiliated institutions. The seminars were supported by an NIH conference grant that allowed all participants to receive free registration. ACCN staff members and ACCN-affiliated, community-based cancer coalition members advertised the seminars to public health professionals, cancer control advocates, community leaders, cancer survivors, and other community members involved in eliminating health disparities in Appalachia. Advertising the seminars was accomplished by posting flyers in local Appalachia community locations (health departments, libraries, etc.) and by sending seminar information by fax and email to different community groups and agencies.
Fig. 1.
Logic model for Appalachia cancer health disparities seminars
The seminars were designed to draw attention to the cancer disparities that exist in Appalachia and to highlight the CBPR projects and evidence-based educational programs being conducted by academic and community partnerships in Appalachia. Each seminar used a common agenda format including speakers who were academic researchers, junior investigators, and community members from local cancer coalitions. Panel discussions were featured to facilitate sharing ideas with the members of the audience. In addition to presentations directed at cancer disparities and interventions to reduce cancer, the seminars also addressed Appalachian identity, the impact of culture and heritage on cancer disparities in Appalachia, and the importance of storytelling in Appalachia. Although the content of all seminars was comparable, the regional seminars featured local researchers and community members compared to the national seminar which featured researchers, community members, and cancer-related issues associated with the entire Appalachian region.
Individuals preregistered for the seminars on-line or by calling a toll-free telephone number. After preregistering for a seminar, individuals received a subject identification number and were requested to complete a web-based pre-seminar survey using SurveyMonkey®. The short survey developed for this seminar series (and not tested for reliability or validity) included: demographic characteristics, knowledge (10 true/false items) and attitudes (10 items on a five-point Likert scale: strongly disagree to strongly agree) about cancer and cancer disparities in Appalachia, and one open-ended question that asked participants to describe the unique qualities of people living in Appalachia that best represent the overall spirit of this population. The identical pre–post-surveys took approximately 5 to 10 min to complete. Individuals who registered on the day of the seminar completed a pre-seminar paper survey and received a subject identification number. At the end of the seminar, individuals completed a short post-seminar paper survey that included their subject ID number, knowledge and attitudes about cancer and cancer disparities in Appalachia, as well as a speaker evaluation form. All paper surveys were structured for TeleForm electronic scanning, were completed on site, and were scanned and verified after completion of the seminars. The option of completing the pre-seminar survey on-line was designed to increase response rates and reduce costs. A mixed mode pre–post-survey design may cause measurement error that impacts the ability to measure change over time [19]. To minimize this error, all questions on the pre- and post-surveys were presented in the same format and order. The participants did not receive any incentive for completing the pre–post-surveys.
A unique feature of the evaluation of the national seminar was inclusion of a social network component, operationally defined for this study as familiarity with individuals attending the conference. Individuals attending the national seminar were provided with a list of all preregistered attendees categorized by state of residence. At the beginning of the seminar, participants were asked to review the list of attendees and indicate each person they knew prior to attending the seminar. At the end of the seminar, participants were asked to complete the same form and to mark additional people they met and talked to at the 2.5-day seminar. Special events to improve networking at the seminar included a special poster presentation event, randomly assigned seating during meals, and an “Appalachia Cancer Jeopardy” game during an evening session. The social network analysis included in this study was based on the identification of the names on the pre- and post-surveys.
An ACCN report, “The Cancer Burden in Appalachia—2009,” was distributed at the national seminar, and approximately 1 month later, an email request was sent to all participants requesting their assessment of the report and its usefulness [20]. The evaluation plan for the seminar series was approved by the institutional review board of The Ohio State University.
Summary statistics (means, percentages) were used to describe the participants. Participants were assigned knowledge scores pre- and post-seminar using the number of correct responses out of 10 true/false questions. Attitude scores were also assigned using the sum of the 10 Likert scale items mentioned above. Due to an administrative error, participants from the Ohio seminar were excluded from the knowledge analysis.
Since some participants failed to complete a pre- or posttest survey, simple paired t tests could not be used to test for pre–post-difference in knowledge and attitudes. Instead, knowledge and attitudes data were analyzed using repeated measures models fit using restricted maximum likelihood (SAS PROC MIXED REPEATED statement), which provide unbiased estimates of pre–post-differences assuming that the data are missing at random [21]. Our models included fixed effects for seminar, time (pre-/post-), and a seminar-by-time interaction. When analyzing the knowledge data, an unstructured variance–covariance matrix was used to model the residual errors while a compound symmetric matrix was used when analyzing the attitudes data. If the seminar-by-time interaction was significant (based on an F test evaluated at α=0.05), we performed separate tests of post–pre-differences for each seminar using t tests of linear contrasts of our model parameters evaluated under a Bonferroni-corrected significance level (α=0.0167 for knowledge and 0.0125 for attitudes), otherwise we evaluated the main effect of time using a single t test evaluated at α=0.05. The Kenward–Roger method was used to calculate the denominator degrees of freedom for both the F and t tests [22]. Since the knowledge and attitudes data were left skewed, we performed a power transformation of each outcome to remove skewness (fifth power for knowledge, cubed for attitudes following the methods of Box–Cox) [23]. Reported p values are based on these power transformations, though the pre- and posttest means and standard errors we report are based on running the models on the original scale. All analyses were conducted using SAS Version 9.2 (SAS Inc., Cary, NC).
The social network data were analyzed to determine visual changes in network patterns [24]. The written comments submitted by the seminar attendees to the one open-ended question on the survey (“Describe the qualities that best represent the overall spirit of the people living in Appalachia”) were categorized into repeated themes.
Results
Participants
Participants (n=335) attending the four seminars were predominantly college educated (83.9%), non-Hispanic (97.3%), white (80.3%), and female (74.6%, Table 1). Only 14% of the participants reported living in an urban setting. The occupation of the participants included academic researchers (29.0%), healthcare providers (15.8%), public health professionals (15.2%), and members of community agencies (13.4%).
Table 1.
Demographic characteristics of seminar participants (n=335)
| Characteristic | N (%) |
|---|---|
| Age, mean+SD (years) | 46.8+12.6 |
| Gender (female) | 250 (74.6) |
| Ethnicity (Hispanic) | 9 (2.7) |
| Race | |
| White | 269 (80.3) |
| African American | 26 (7.8) |
| Asian | 6 (1.8) |
| Native American/Alaskan | 3 (0.9) |
| Other | 6 (1.8) |
| Marital status | |
| Single | 50 (14.9) |
| Married/living together | 211 (63.0) |
| Divorced/widowed | 43 (12.8) |
| Education | |
| Less than high school | 1 (0.3) |
| High school | 27 (8.1) |
| College | 100 (29.9) |
| Graduate/professional school | 181 (54.0) |
| Residence | |
| Urban | 47 (14.0) |
| Suburban | 106 (31.6) |
| Rural | 133 (39.7) |
| Occupation | |
| Academic researchers | 97 (29.0) |
| ACCN member | 36 (10.8) |
| Cancer survivor | 5 (1.5) |
| Community agency | 45 (13.4) |
| Community resident | 6 (1.8) |
| Healthcare provider | 53 (15.8) |
| Public health official | 51 (15.2) |
Numbers do not always add up to 100% because of missing data
Pre–Posttest
Prior to the seminars, 309 (92%) participants answered the knowledge questions (true/false) and 291 (87%) participants completed the attitude items (Likert scale). After the seminars, 211 (63%) participants completed the knowledge questions and 202 (60%) participants completed the attitude items. Assessment of change in knowledge (Table 2) was limited to data from Kentucky, West Virginia, and Pennsylvania seminars and was found to differ by seminar (F(2, 148)=3.60, p=0.030). There was no change in knowledge following the Kentucky seminar, however knowledge improved following the national and Pennsylvania seminars (Table 3). Change in attitudes also differed by seminar (F(3, 218)=4.75, p=0.003), with a significant change only occurring following the Ohio seminar (Table 3).
Table 2.
Appalachia knowledge questions used in pre–post tests
| Pretest |
Posttest |
|||
|---|---|---|---|---|
| N | N correct (%) | N | N correct (%) | |
| 1. There are less medical clinics and hospitals in Appalachia compared to non-Appalachia regions. | 309 | 263 (85.1) | 211 | 198 (93.8) |
| 2. Women living in Appalachia die of cancer at the same rate as women living in non-Appalachia.a | 184 | 152 (82.6) | 195 | 176 (90.3) |
| 3. Human papillomavirus is rare among women living in Appalachia.a | 184 | 154 (83.7) | 195 | 188 (96.4) |
| 4. Cancer mortality rates are higher in Appalachia compared to non-Appalachia. | 309 | 268 (86.7) | 211 | 205 (97.2) |
| 5. Tobacco use among residents of Appalachia is equal to residents of non-Appalachia. | 309 | 266 (86.1) | 211 | 203 (96.2) |
| 6. Breast cancer mortality rates are higher in Appalachia compared to non-Appalachia. | 309 | 38 (12.3) | 211 | 20 (9.5) |
| 7. Residents in Appalachia use cancer screening tests at the same rate as residents of non-Appalachia. | 309 | 280 (90.6) | 211 | 200 (94.8) |
| 8. Limited public transportation is currently a problem in Appalachiaa. | 184 | 177 (96.2) | 195 | 181 (92.8) |
| 9. There is a high rate of obesity among residents of Appalachia. | 309 | 268 (86.7) | 211 | 195 (92.4) |
| 10. Lung cancer mortality rates are higher in Appalachia compared to non-Appalachia. | 309 | 265 (85.8) | 211 | 196 (92.9) |
Not asked in KY (pre and post) and OH (pre) due to an administrative error
Table 3.
Model-based estimates of mean (SE) knowledge and attitude scores by seminar
| Seminar | Knowledge |
Attitudes |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre- | Post- | ta | df | p value | Pre- | Post- | ta | df | p value | |
| Kentucky | 9.2 (0.4) | 9.0 (0.2) | −1.16 | 128 | 0.247 | 36.8 (0.9) | 38.0 (1.1) | 1.29 | 193 | 0.200 |
| Ohio | –b | –b | –b | –b | –b | 36.3 (0.4) | 35.1 (0.5) | −2.80 | 193 | 0.006 |
| Pennsylvania | 7.5 (0.2) | 8.5 (0.1) | 3.00 | 189 | 0.003 | 35.1 (0.5) | 35.9 (0.5) | 1.60 | 263 | 0.111 |
| National | 8.0 (0.2) | 8.7 (0.1) | 3.41 | 145 | 0.001 | 34.8 (0.4) | 35.6 (0.6) | 1.50 | 216 | 0.134 |
t test of post–pre-difference
Ohio was omitted from the knowledge analysis, administrative error
Description of Appalachian Residents
The comments from the participants included statements about the overall spirit of people living in Appalachia including the following terms: family oriented, independent, proud, community connected, hardworking, friendly, patriotic, resistant to change, deep rooted in culture, and hospitable but cautious of “outsiders.” One participant summed up the residents of Appalachia as “filled with beautiful contradictions.”
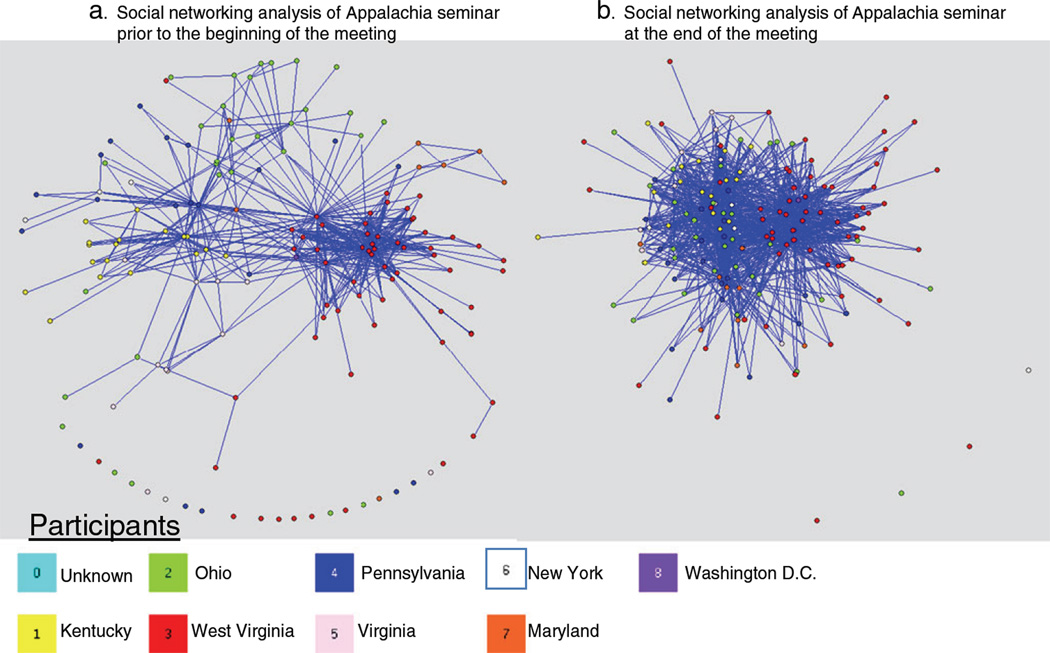
Social Network Analysis
This analysis consisted of measuring and mapping the normally invisible relationships between people. In the social network analysis, the nodes were the national seminar participants (color-coded circles based on participant’s state of residence) and the lines were the ties between the different participants. The pre-meeting social network map (Fig. 2a) demonstrated that most individuals knew colleagues from the same state, with a few participants having cross-state connections. The post-meeting map (Fig. 2b) showed a significant increase in the number of cross-state connections.
Fig. 2.
a Social networking analysis of Appalachia seminar prior to the beginning of the meeting. b Social networking analysis of Appalachia seminar at the end of the meeting
Cancer Burden in Appalachia—2009 Report
Approximately 1 month after the national seminar, an email request was sent to the 138 participants asking them to complete a short web-based survey (SurveyMonkey®) about the ACCN cancer disparities report that was distributed at the meeting. The survey completion rate was 48.6% (n=67). Of those completing the survey, 75% (n=50) reported looking at the report after the meeting and 45% (n=30) reported using the document during the month following the WV seminar. Participants (n=63; 94%) reported that they planned to use the report in the future for grant writing, for presentations, program planning, and to share with the local media. Among participants reporting already using the ACCN report, 100% thought the information was easy to locate and 90% were satisfied with the information.
Discussion
Evaluation of a seminar focusing on cancer health disparities in Appalachia was conducted to determine the ability of the educational seminars to accomplish three objectives: (1) increase knowledge of existing cancer disparities in Appalachia, (2) disseminate research findings from CBPR projects conducted in Appalachia, and (3) foster CBPR capacity building by promoting networking among participants of the seminars. Results of the evaluation suggest that the objectives, or short-term outcomes, of the educational seminars were accomplished.
Typically, educational seminars directed at health care professionals and community members are evaluated for attendance, satisfaction with the speakers and the overall program. In addition to these standard measures, the evaluation of the Appalachia cancer disparities seminars also included measuring changes in knowledge, attitudes, and the unique feature of measuring the change in social networks among participants of a national seminar. By planning activities within the seminar agenda to promote networking, we hoped that participants would gain an awareness of assets within each other’s communities and become aware of potential new collaborators to address the cancer health disparities in their communities.
Key principles of CBPR include community members participating in the planning, implementation, data collection and interpretation, and the dissemination of community-based programs [25]. The Appalachia cancer disparities seminars provided an opportunity for community members to participate in these tenets of CBPR by including community members in the planning of the seminars, as speakers who reported findings from projects that they conducted in their communities, having community members exchange ideas during panel discussions, and having free exchanges with community members in the audience and at social networking events. This component of the seminars was positively received by the seminar participants as documented in the post-seminar evaluation.
Based on comments from community members attending the seminars, a second more community-friendly ACCN report was developed, “Addressing the Cancer Burden in Appalachian Communities-2010” [26]. The 2010 ACCN report provided more information on cancer risk factors and risk reduction, a glossary of terms, and step-by-step instructions for completing a community assessment.
Although the short-term objective of promoting networking among the seminar attendees was accomplished at the seminar, assessment of the long-term effects of the networking at the meeting is beyond the scope of this evaluation. The networking events at the seminar, however, focused on the process instead of the seminar’s content, providing the opportunity for seminar attendees to develop new partnerships. It takes time to build trustworthy and effective partnerships to address the mutual goal of reducing cancer disparities among the residents of Appalachia. Capacity building is an important step to build the infrastructure for future CBPR projects to reduce cancer disparities, improves community empowerment, provides a better likelihood for sustainability of interventions, and is a critical step for policy advocacy [27–29].
This study is not without limitations. Limitations include that the pre–post-surveys were developed specifically for the seminars, and although questions were reviewed by content experts, the surveys were not tested for reliability or validity. Thus, because the test was newly developed, interpretation of the meaning of the test performance is limited, given the absence of comparative data. The majority of participants in this study were college graduates and are not representative of the residents of Appalachia who are most affected by cancer health disparities. In addition, surveys were not completed by all seminar attendees and a mixed mode administration of the surveys may have introduced measurement error in the analysis. Planning innovative strategies to increase response rates from program participants should be developed for future educational seminars and programs. The limitations of this study might limit the ability to generalize its findings to other populations
Among participants attending an Appalachia cancer disparities seminar, an evaluation found improved knowledge, dissemination of findings from CBPR projects and evidence-based educational programs, and changes in the social network of participants that potentially will increase CBPR projects conducted in Appalachia to address the cancer burden among its residents. This evaluation included the unique methodology of mapping the social network of the participants to document changes and including these methods in program evaluation should be assessed by others in the future.
Acknowledgments
The authors which to acknowledge the support from the following grants: National Center for Minority Health and Health Disparities (R24MD002785) and the National Cancer Institute 5 U01 CA114622 (ACCN), 5 P30CA16058-31 (The Ohio State University Comprehensive Cancer Center), UL1RR025755 from the National Center For Research Resources, and K07 CA 107079 (MLK).
Contributor Information
Mira L. Katz, Email: mira.katz@osumc.edu, College of Public Health, The Ohio State University, Suite 525, 1590 North High Street, Columbus, OH 43201, USA; Comprehensive Cancer Center, The Ohio State University, Columbus, OH 43201, USA.
Michael L. Pennell, College of Public Health, The Ohio State University, Suite 525, 1590 North High Street, Columbus, OH 43201, USA
Mark B. Dignan, College of Medicine, University of Kentucky, Lexington, KY 40504, USA
Electra D. Paskett, Comprehensive Cancer Center, The Ohio State University, Columbus, OH 43201, USA College of Medicine, The Ohio State University, Columbus, OH 43201, USA.
References
- 1.Appalachia Regional Commission (ARC) [Accessed April 2011]; http://www.arc.gov/index.asp.
- 2.Abramson R, Haskell J. Encyclopedia of Appalachia. Knoxville: The University of Tennessee Press; 2006. [Google Scholar]
- 3.Friedrich MJ. Lung cancer death rates in Appalachia, 1994–1998 Program aims to reduce cancer burden in Appalachia. J Natl Cancer Inst. 2002;94(16):1190. [PubMed] [Google Scholar]
- 4.Haung B, Wyatt SW, Tucker TC, Bottorff D, Lengerich E, Hall HI. Cancer death rates—Appalachia, 1994–1998. Breast and cervical cancer screening among Appalachian women. MMWR Morb Mortal Wkly Rep. 2002;51(24):527–529. [PubMed] [Google Scholar]
- 5.Armstrong LR, Thompson T, Hall HI, Coughlin SS, Steele B, Rogers JD. Colorectal carcinoma mortality among Appalachian men and women, 1969–1999. Cancer. 2004;101(12):2851–2858. doi: 10.1002/cncr.20667. [DOI] [PubMed] [Google Scholar]
- 6.Lengerich EJ, Tucker TC, Powell RK, et al. Cancer incidence in Kentucky, Pennsylvania, and West Virginia: disparities in Appalachia. J Rural Heal. 2005;21(1):39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 7.Wingo PA, Tucker TC, Jamison PM, et al. Cancer in Appalachia, 2001–2003. Cancer. 2008;112(1):181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]
- 8.Hopenhayn C, King JB, Christian A, Huang B, Christian WJ. Variability of cervical cancer rates across 5 Appalachian states, 1998–2003. Cancer. 2008;113(10 Suppl):2974–2980. doi: 10.1002/cncr.23749. [DOI] [PubMed] [Google Scholar]
- 9.Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, Lurie N, Rebbeck T, Goodwin J, Flack J, Srinivasan S, Kerner J, Heurtin-Roberts S, Abeles R, Tyson FL, Patmios G, Hiatt RA. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98:1608–1615. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher J, Engelhardt H, Stephens J, et al. Cancer-related disparities among residents of Appalachia Ohio. J Health Dispar Res Pract. 2008;2(2):61–74. [Google Scholar]
- 11.Wewers ME, Ahijevych KL, Chen MS, Dresbach S, Kihm KE, Kuun PA. Tobacco use characteristics among rural Ohio Appalachians. J Community Health. 2000;25(5):377–388. doi: 10.1023/a:1005127917122. [DOI] [PubMed] [Google Scholar]
- 12.Yabroff KR, Lawrence WF, King JC, et al. Geographic disparities in cervical cancer mortality: what are the roles of risk factor prevalence, screening, and use of recommended treatment? J Rural Health. 2005;21(2):149–157. doi: 10.1111/j.1748-0361.2005.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 13.Paskett ED, McLaughlin JM, Reiter PL, et al. Psychosocial predictors of adherence to risk-appropriate cervical cancer screening guidelines: a cross sectional study of women in Ohio Appalachia participating in the Community Awareness Resources and Education (CARE) project. Prev Med. 2010;50:74–80. doi: 10.1016/j.ypmed.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wewers ME, Katz M, Fickle D, Paskett ED. Risky behaviors among Ohio Appalachian adults. Prev Chronic Dis. 2006;3(4):A127. [PMC free article] [PubMed] [Google Scholar]
- 15.Behringer B, Mabe KH, Dorgan KA, Hutson SP. Local implementation of cancer control activities in rural Appalachia, 2006. Prev Chronic Dis. 2009;6(1):A34. [PMC free article] [PubMed] [Google Scholar]
- 16.Hutson SP, Dorgan KA, Phillips AN, Behringer B. The mountains hold things in: the use of community research review work groups to address cancer disparities in Appalachia. Oncol Nurs Forum. 2007;34(6):1133–1139. doi: 10.1188/07.ONF.1133-1139. [DOI] [PubMed] [Google Scholar]
- 17.Behringer B. Health care services in Appalachia. In: R Couto, NK Simpson, G Harris., editors. Sowing seeds in the mountains: community-based coalitions for cancer prevention and control NIH Publication No 94-3779. National Institutes of Health: Bethesda; 1994. pp. 62–80. [Google Scholar]
- 18.Katz ML, Reiter PL, Kluhsman BS, Kennedy S, Dwyer S, Schoenberg N, Johnson A, Ely G, Roberto KA, Lengerich EJ, Brown P, Paskett ED, Dignan M. Human papillomavirus (HPV) vaccine availability, recommendations, cost, and policies among health departments in seven Appalachian states. Vaccine. 2009;27:3195–3200. doi: 10.1016/j.vaccine.2009.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dillman DA, Smyth JD, Christian LM. The tailored design method. 3rd edn. Wiley: Hoboken; 2009. Internet, mail, and mixed-mode surveys. [Google Scholar]
- 20.Appalachia Community Cancer Network. [Accessed November 2010];The cancer burden in Appalachia. 2009 http://www.accnweb.com/
- 21.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 22.Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- 23.Box GEP, Cox DR. An analysis of transformations. J R Stat Soc. 1964;26:211–252. [Google Scholar]
- 24.Pajek A. [Accessed October 2009];program for large network analysis. http://vlado.fmf.uni-lj.si/pub/networks/pajek/
- 25.Israel BA, Eng E, Schulz AJ, Parker EA. Wiley: San Francisco; 2005. Methods in community-based participatory research for health. [Google Scholar]
- 26.Appalachia Community Cancer Network. [Accessed November 2010];Addressing the cancer burden in Appalachian communities. 2010 http://www.accnweb.com/.
- 27.Simmons A, Reynolds RC, Swinburn B. Defining community capacity building: is it possible? Prev Med. 2011;52:193–199. doi: 10.1016/j.ypmed.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, Reyes AG, Clement J, Burris A. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100:2094–2102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dankwa-Mullan I, Rhe KB, Williams K, Sanchez I, Sy FS, Stinson N, Ruffin J. The science of eliminating health disparities: summary and analysis of the NIH Summit recommendations. Am J Public Health. 2010;100:S12–S18. doi: 10.2105/AJPH.2010.191619. [DOI] [PMC free article] [PubMed] [Google Scholar]