Abstract
Background
No data have been available on severe allergic reactions in Finland.
Materials and Methods
We summarize the data accumulated from 2000 to 2007 in the national register established at the Skin and Allergy Hospital of the Helsinki University Central Hospital, where physicians voluntarily report on patients with severe allergic reactions.
Results
During the period, the 530 reported cases of severe allergic reactions represented an annual frequency of 0.001%. Of the patients, 66% were adults and 56% were female, with a median age of 27 years. Food was the causative agent in 53% of the cases, drugs in 26%, allergen preparations in 12%, and insects in 8%. Dermatologic symptoms were reported in 85%, respiratory in 76%, cardiovascular in 50%, gastrointestinal in 33%, and eye/nose symptoms in 18%. The reaction was a life-threatening anaphylactic shock in 26% of the cases, with no deaths reported. Patients were treated with intramuscular adrenaline in 75% of the cases. Not only nuts and seeds, but also fruit and vegetables were the most important allergens for the adults. Nuts were also important allergens for children, along with milk, egg, and wheat. In addition, many "exotic" allergens were identified: patent blue, carmine dye, yeast, buckwheat, and macrogol.
Conclusions
Severe allergic reactions are underreported, but a register reflects the real-life situation and helps to identify new causative agents. It also contributes to improvements in first aid treatment practice.
Keywords: allergen preparation, anaphylaxis, drug, food, insect, register
Anaphylaxis is an immunoglobulin E (IgE)-or non- IgE-mediated, severe, life-threatening systemic allergic reaction, with a rapid onset and multiple organ system involvement [1,2]. Independent of the mechanism, the first aid treatment of choice is intramuscular adrenaline. Because of the risk of recurrent severe reaction, the causative allergen must be recognized and avoided when possible.
To our knowledge, nationwide anaphylaxis registers or similar organizations exist at least in Denmark, France-Belgium, Germany-Austria-Switzerland, Italy, the Netherlands, Norway, Sweden, the United Kingdom and Ireland, and also in the United States (Table 1) [3-7]. Maintaining a comprehensive anaphylaxis register involves several difficulties, for example, the lack of internationally accepted clinical definition of anaphylaxis has made it difficult to diagnose an anaphylactic reaction (Table 2).
Table 1.
Anaphylaxis Registers and Anaphylaxis Organizations
| Country | Register Type and Contact Address | Responsible Informant/Organization |
|---|---|---|
| Several | The Food Allergy and Anaphylaxis Alliance | Since 1999, allergy network groups from the United States, United Kingdom, Canada, Quebec, New Zealand, Italy, Australia, and the Netherlands. |
| A voluntary registry for peanut and tree nut allergy (United States, since 1997) | ||
| Denmark | Danish Anaesthesia Allergy Centre | Clinicians may refer their patients to Danish Anaesthesia Allergy Centre for further investigation |
| Finland | National anaphylaxis register | 1-Page anaphylaxis form to be filled by physician |
| France and Belgium | French Allergy Vigilance Network (Available at: www.cicbaa.org) | 1-Page declaration of severe allergic accident to be filled in mainly by French and Belgian allergists |
| The Study Group on Anaphylaxis during Anaesthesia (GERAP) | ||
| Germany, Austria, and Switzerland | Deutscher Allergie-und Asthmabund (Available at: www.anaphylaxie.net) | Patient organization reports from clinicians |
| Norway | The Norwegian National Reporting System and Register of Severe Allergic Reactions to Food (Food Allergy Register) | Government-funded system, 1-page reporting form from physicians, IgE and allergen analysis service |
| Sweden | Swedish system for reporting severe and fatal reactions caused by food | National system for reporting by the medical profession |
| United Kingdom | The United Kingdom anaphylaxis register | Since 1992 for fatal anaphylactic reactions in the United Kingdom |
FAAA indicates Food Allergy and Anaphylaxis Alliance.
Table 2.
Difficulties in Maintaining an Anaphylaxis Register
| Problem | Solution | Suggestion |
|---|---|---|
| 1. Lack of definition of anaphylaxis: anaphylactic reaction vs anaphylactic shock | Clinical diagnosis [17] | Combination of circulatory, dermatologic, respiratory, gastrointestinal symptoms |
| 2. Not all reactions are reported | Improvement of knowledge and vigilance system | FAAA Ga2len network |
| 3. Not all allergens are considered | Exchange of register information | FAAA Ga2len network |
| 4. Allergen not identified | More resources, better organized testing | All anaphylaxis patients should be seen by an allergologist |
FAAA indicates Food Allergy and Anaphylaxis Alliance.
No data reveal actual frequency of severe allergic reactions in Finland. The literature has reported incidence figures of 7.9 to 21 anaphylaxis cases per 100,000 person-years,[8-10] along with increasing allergy prevalence and hospital admission figures during the past decade [11-13]. In the United States, approximately 30,000 cases of food anaphylaxis occur annually, 150 to 200 of which are fatal [14]. In the United Kingdom, the incidence of fatal reactions is one in 3 million person-years, and its National Anaphylaxis Campaign was set up in 1994 for guidance and information on allergens and allergic reactions [15-17].
In 2000, the Finnish register of severe allergic reactions was established at the Skin and Allergy Hospital of the Helsinki University Central Hospital, where physicians--mostly allergologists--voluntarily report patients with severe allergic reactions independently of the causative agent. A 1-page questionnaire form is available on the Internet.
Materials and methods
We summarize the first 530 cases reported to the register between 2000 and 2007. Our results are based on the anonymous patient data provided by the physicians in the questionnaire form evaluated by an allergy specialist.
Any adverse reactions from vaccines that were reported to the National Public Health Institute are absent from the present article.
Results
Reports on severe allergic reactions
A total of 530 cases of severe allergic reactions were reported between 2000 and 2007 throughout the country, mostly (65%) from the Helsinki capital area, which represents 25% of the entire population of 5.2 million. This represents an annual incidence of 0.001%.
Patients
Of the 530 cases, 348 (66%) were adults and 182 (34%) were children younger than 16 years. Females accounted for 295 (56%). Median age was 27 years; range was from 2 months to 92 years. Two peaks in age distribution were for children younger than 5 years and young adults aged 25 to 35 years.
A previously diagnosed allergy occurred in 91%; skin disorders were present in 43%, allergic rhinoconjunctivitis in 43%, asthma in 33%, and gastrointestinal disorders in 6%. A previous anaphylaxis affected 23%.
The reactions were regarded as severe anaphylactic shock reactions in 26% of the cases, with a systolic blood pressure in adults less than 90 mm Hg or with severe respiratory symptoms such as bronchospasm and upper airway angioedema [18]. Other severe allergic reactions included nonshock reactions with symptoms in at least two of the following organs: skin, respiratory tract, cardiovascular system, or gastrointestinal tract [18].
Symptoms and treatment
In 74% of the cases, the first symptoms predicting severe allergic reaction appeared less than 30 minutes after contact with the inciting allergen.
Skin symptoms were most commonly reported, in 85%, followed by respiratory (76%), cardiovascular (50%), and gastrointestinal (33%) symptoms.
Most frequently, corticosteroids were used for treatment, in 84%, followed by adrenaline in 75%, and antihistamine in 67%. Of the adrenaline-treated patients, 10% used a ready-to-use adrenaline autoinjector.
Allergens and exposure
Foods were the causative agent in 279 (53%) cases, drugs and medical interventions in 136 (26%), allergen preparations for diagnostic work and immunotherapy in 64 (12%), and insects in 40 (8%) (Figure 1). In 13 patients (2%), other causes were noted, and only 6 cases (1%) were idiopathic or without any recognizable cause (Table 3). In 7 cases, both food and a drug were suspect causative agents. An additional known or suspected factor in 29 cases (5%) was exercise.
Figure 1.
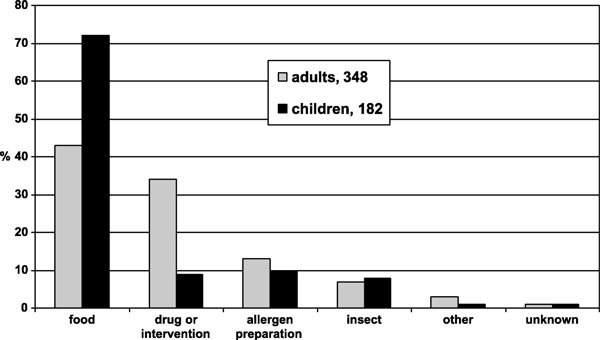
Causes for severe allergic reactions (%) in adults and in children between 2000 and 2007 in Finland.
Table 3.
Allergens Causing Severe Allergic Reactions in Finland
| Allergen | Adults | Children | Examples of Specific Agents |
|---|---|---|---|
| Foods | 148 | 131 | |
| Nuts/seeds | 38 | 21 | |
| Tree nuts | 21 | 10 | Hazel (n = 5), cashew (n = 3), walnut (n = 3), almond (n = 3; marzipan, n = 1), pistachio (n = 2) |
| Seeds | 12 | 3 | Sesame (n = 5; tahini, n = 3), pine (n = 3), flaxseed (n = 2), mustard |
| Peanut | 5 | 8 | Cooked peanut taken as beans |
| Fruit | 19 | 12 | Kiwi (n = 8), apple (n = 5), banana (n = 5), grape (n = 3), mango (n = 4), lychee, jackfruit, plum (n = 2), red currant |
| Vegetables | 11 | 5 | Celery (n = 5), carrot (n = 4), parsnip (n = 2), pea (n = 5), melon |
| Grains | 17 | 26 | Wheat (n = 32), buckwheat (n = 5), corn, oat, rye, barley |
| Milk | 7 | 31 | Cow milk (n = 36), goat milk (n = 2) |
| Egg | 1 | 23 | |
| Fish/shellfish | 14 | 9 | Tuna (high histamine; n = 5), perch, shrimp (n = 8), roe |
| Soy | 6 | 3 | Alpro soy drink (n = 4) |
| Other foods | 30 | 14 | Baked roll (n = 9), wine (n = 3), carmine red (n = 2), sweet (n = 2), yeast |
| Several foods | 111 | 1 | Milk-egg-wheat, a whole meal |
| Drugs | 120 | 16 | |
| Antibiotics | 35 | 5 | |
| Cephalosporin | 12 | 2 | Cefuroxime (n = 10), cefalexin (n = 2) |
| Penicillin | 11 | 1 | Phenoxymethyl penicillin (n = 9), filling agent macrogol (polyethylene glycol) |
| Other antibiotics | 12 | 2 | Amoxicillin (n = 5), macrolide (n = 4), fluoroquinolone (n = 2), trimethoprim (n = 2), tetracycline (n = 2), nitrofurantoin, chloramphenicol, metronidazole |
| Painkillers | 28 | 10 | |
| ASA | 8 | 1 | |
| Ibuprofen | 5 | 3 | Alone (n = 5) or with other drugs (n = 2) |
| Paracetamol | 2 | 1 | 1 in a combination product |
| Other pain killers | 11 | 2 | Diclofenac (n = 4), naproxen (n = 6), coxib (n = 3), mefenamic acid |
| General anesthetics | 25 | 0 | |
| Rocuronium | 17 | Alone (n = 14) or with other anesthetics (n = 3) | |
| Patent blue | 3 | ||
| Other anesthetics | 5 | Several (antibiotic, propofol, fentanyl), gelatin | |
| Local anesthetics | 10 | 0 | Lidocaine (vasovagal reaction), methylprednisolone of the product |
| Radiocontrast media | 9 | 0 | Iodobromide (n = 4), ioversol, ioxaglate, iomeprol (n = 2), iodixanol |
| Other drugs | 22 | 2 | Infliximab (n = 2), pollen product, insulin protamine, povidone, borophenylalanine, aurothiomalate, methylprednisolone (n = 3), angiotensin-converting enzyme inhibitor, reteplase, tetanus-diphtheria vaccine, antispasmodic, chlorhexidine |
| Allergen preparations | 46 | 18 | |
| SIT | 37 | 17 | |
| Timothy | 32 | 13 | Alone (n = 42) or with birch or grass mix |
| Other allergen | 5 | 4 | Birch (n = 6), cat (n = 2), dog, wasp |
| SPT | 9 | 1 | Egg, fish, penicillin, mould, carmine, chironomid, several allergens |
| Insects | 25 | 15 | |
| Wasp | 19 | 14 | |
| Other insects | 6 | 1 | Bee (n = 2), mosquito, chironomid, unknown (n = 2) |
| Other causes | 11 | 2 | Chemical, latex, viper bite, fragrance, algae, rabbit, plant, other (n = 5) |
| Not known | 4 | 2 | |
| All | 348 | 182 | In some cases, several causes were present |
Hospitals and other health care settings were the most common venues for severe allergic reactions overall (33%), followed by the home (30%), hobbies (14%), restaurants (7%), day care/schools (7%), and work places (6%).
Food
Food (n = 279) was the most common cause of severe allergic reaction (53%). Of these patients, 53% were adults, 64% of whom were females, but most (60%) of the children were boys. The home was the most common place for food reaction (36%).
Food was responsible for 72% of the reactions in children, but for only 43% in adults. An association with exercise was documented in 8% with food-related reactions. Food caused 46% of the most severe shock reactions, including peanut/tree nuts/seeds (n = 17), grains (n = 11), milk (n = 10), fruit/vegetable (n = 8), egg (n = 6), fish/shellfish (n = 2), soy, and yeast among others.
An allergen-containing food was accidentally given to 53 patients, 60% of whom were children. These included milk, wheat, egg, fish, nuts, and seeds. Most episodes (77%) took place outside the home.
Most food-related reactions were from peanuts, tree nuts, and seeds (21%), 36% of which occurred in children (Table 3). One adult experienced anaphylaxis after eating home-delivered Thai food that contained soft-treated peanuts, which the patient assumed were beans. Tree nuts were involved in 53% of the nut/seed cases. Hidden or nonrecognized nuts were the causative agent in bread and in ice cream. Two other patients (1 child and 1 adult) had anaphylaxis after eating tahini sauce not recognized by the patients as being a sesame seed product.
Fruits and vegetables were reported in 16% of the food anaphylaxis cases, of which kiwi, apple, and celery were the most common allergens. In 2 birch pollen-allergic adults, even the first ingestion of an exotic fruit such as jackfruit or lychee when abroad resulted in severe anaphylactic reactions.
Regarding grains, reports numbered 14% of the cases, 72% of which were from wheat. One wheat-allergic child had a severe reaction after eating gluten-free pasta, and another child after eating a wheat-free bun made of buckwheat to which the child had developed an allergy during a 3-year wheat-free diet. Buckwheat in a blin was unexpectedly allergenic to 1 adult patient, whereas another adult experienced anaphylaxis from a bun in which the marzipan was dyed with a red color from cochineal insects (carmine, E120).
Milk was the causative agent in 14% of the food-related anaphylaxis cases. Heavy exercise together with milk protein-containing pills caused a severe reaction in a milk-allergic adult to whom the terms casein and whey were unknown. The patient had an adrenaline autoinjector, but she did not dare use it. One adult experienced anaphylaxis from cow's milk feta cheese, but she tolerated goat's milk feta, whereas another adult experienced anaphylaxis from goat cheese without a cow's milk allergy (Figure 2).
Figure 2.
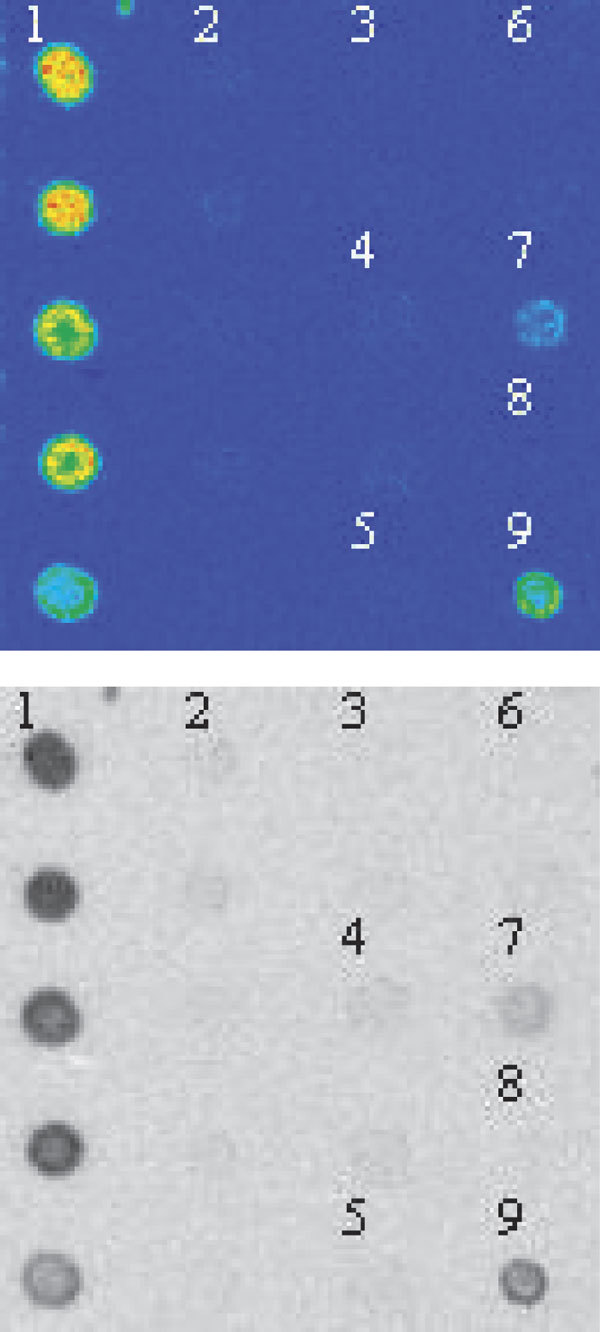
In-house immunospot method demonstrates serum IgE to the inner part of the goat cheese delivered by the patient with anaphylaxis,[1]but not to cow's milk [8]. Other examples are the mouldy surface of the goat cheese,[2] cow milk casein,[3] sheep milk casein,[4] carrageen used in the cheese,[5] cacao also suspected as an allergen,[6] egg white,[7] and goat cheese from the laboratory repertory [9].
Egg was reported in 9% of the food reactions, all but one in children, and 7 of which were accidents outside the home. In 1 case, a hidden allergen was suspected.
Fish or seafood was reported in 8% of the cases. Fish nuggets were given to a child instead of chicken nuggets (the Finnish word for fish is kala, for chicken, kana). Five reports were toxic reactions from tuna fish in which a high histamine content was suspected as the causative agent because no fish allergy was evident. Eight cases were from shrimp and one from roe in the absence of fish allergy [19].
Soy was reported or suspected in 9 cases, 4 of which occurred in birch pollen-allergic patients after a soy drink. A skin prick test with native soy bean was positive, whereas a commercial serum soy-specific IgE test was negative, indicating the missing labile cross-reactive soy allergen (Gly m 4) [20]. In other cases, soy was suspected as a hidden allergen in the food offered in day care centers.
Yeast used as a flavoring agent in a spaghetti sauce repeatedly caused severe anaphylactic reactions in a mould-sensitive patient [21].
Drinks were reported in 11 cases (4%), mostly (73%) in adults. Reported drinks included red and white wine, beer, long drink, cider, juice, and glühwein. One patient repeatedly experienced anaphylaxis when dancing the tango after drinking a beer.
Drugs, Allergen Preparations, and Other Interventions
Drugs (n = 136), allergen preparations (n = 64), and other medical interventions such as food provocation tests (n = 22) were reported in 222 cases (42%), mostly (75%) in adults (Table 3).
Antibiotics in 29% and painkillers in 24% were the most commonly reported in drug-related reactions. Cephalosporins and penicillins comprised 58% of the antibiotics, whereas acetylsalicylic acid (ASA) and ibuprofen accounted for 45% of painkillers. In 4 cases, ASA in a combination product was not recognized by the patient as such.
In 68% of the operation-related reactions, a neuromuscular blocking agent (rocuronium) was suspected as the causative agent either alone or with other anesthetic agents. Three cases were caused by the patent blue dye (E 131) used to locate sentinel lymph nodes. One reaction was caused by chlorhexidine used as skin disinfectant [22]. Local anesthetics were reported in 8 cases, in one of which methylprednisolone used simultaneously proved to be the anaphylactic agent based on positive intradermal testing. Nine cases were from contrast media and one from iodinated povidone (Betadine).
In a drug, the active ingredient is not always the agent causing harm. One case of penicillin anaphylaxis was caused by macrogol (polyethylene glycol) used as an excipient in the tablet vehicle [23].
Allergen preparations were the causative agent in 64 cases (12%), 18 of which occurred in children. Ten reports with mild reactions were from skin prick testing with fish, egg, penicillin, moulds, pollens, animals, chironomid, or carmine dye (E120). Carmine IgE was positive in in-house immunospot test but remained negative in the commercial IgE test, which, however, was improved in collaboration with our laboratory.
Of all reports, 54 (10%) concerned specific immunotherapy (SIT). In 83% of the reactions, timothy grass was the causative allergen, either alone or with other pollen allergens. Nine patients were on a maintenance dose; some for several years.
Of the severe anaphylactic shock reactions, 45% were caused by drugs, allergen preparations, and other interventions, such as operations (n = 16), painkillers (n = 13; ASA, coxib, naproxen, ibuprofen), β-lactams (n = 11), timothy SIT (n = 5), x-ray contrast media (n = 5), infliximab, sodium aurothiomalate, and a natural remedy (pollen) among others.
Insects and Other Agents
Insects were reported in 8% of the cases, 63% of which were in adults. Wasps (92%) were by far the most commonly reported. Insects caused 9% of the severe shock reactions.
Discussion
Based on our study, during the 8 years, 530 severe allergic reactions were reported to the Finnish register for an annual incidence of 0.001%. Reactions are undoubtedly underreported, with higher figures per population reported elsewhere [10].
From the reactions, 26% were life-threatening circulatory or respiratory shock reactions. Adrenaline was the first aid treatment for 75%, but corticosteroids were more frequent: 84% of all cases. In a Swiss study, 48% of the anaphylaxis patients with circulatory symptoms received adrenaline,[9] whereas in an Italian study, only 6% of the patients did [24]. Finnish health care is thus reasonably well prepared to use adrenaline appropriately, but still with room for improvement.
In 5% of our cases, a late-phase reaction occurred compared with late reactions reported in 2% to 20% of cases elsewhere [13,25].
Food, drugs, and insects alternate globally as the most common causes of anaphylaxis [9,11,13,18,26]. In an overview from 1 referral clinic, 59% of the anaphylactic cases were considered idiopathic [27]. In our register, food was the most commonly reported cause (53%), and only 1% of the cases were without a known or highly suspect cause. Fruits, vegetables, nuts, and seeds were the most common causes for food reactions in adults. Similarly, fresh fruits and vegetables have been the most important allergens in adult anaphylaxis in Italy [24]. Thirteen (5%) of the food reactions involved peanut, a common cause for fatal anaphylaxis in the United States and United Kingdom, where the Anaphylaxis Campaign has also reported an increasing frequency/number of sesame anaphylaxis [14,28]. Two of our patients experienced anaphylaxis from sesame sauce tahini. Fish and shellfish were rather seldom reported (8%) but are common causes of anaphylaxis in Italy, Asia, and the United States [13,14,24,27]. No deaths from food are known in Finland.
Diagnostics and other interventions are not without risks [8-10,13,15,28,29]. Of our cases, 42% were from drugs, operations, diagnostics, and other interventions. In line with the reports of neuromuscular blocking agents as the most frequently implicated anesthetic drug, rocuronium was the causative agent in 68% of the surgical anaphylaxis cases [10,29,30].
Severe allergic reactions from allergy diagnostics (skin test and food/drug challenge test) and allergy treatment (SIT) comprised 18% of the cases, and a high frequency of SIT anaphylaxis has been reported only by Mehl et al. [26] Timothy pollen SIT, but not birch pollen SIT, seems to be associated with a relatively high risk for severe reactions, a fact practitioners giving SIT in Finland have been warned about.
Insects are important anaphylactic allergens in Switzerland and in the United Kingdom but account for only 8% of the reports in Finland, wasps being the most frequently reported [8,9]. Because commercial skin prick and serum IgE tests are not always sufficiently sensitive and specific to identify the sensitizing insect, for SIT assessment in our hospital, an in-house immunospot method with several venom samples differentiates between wasps and honey bees [21]. No deaths were reported, although such fatalities are estimated to occur approximately every second year in Finland.
We found only 1 report on severe reaction from latex, an important allergen in France and the United States [10,18,25,27,30].
To avoid is to identify. Our register has been proven to be valuable for identifying causes for severe allergic reactions in Finland. Thus far, poorly recognized allergens and allergen sources have been detected, such as patent blue, carmine, yeast, buckwheat, soy drink, and macrogol. In addition, hidden allergens have been demonstrated in food and drugs. In France, hidden allergens have accounted for 13% of severe anaphylactic reactions [10].
Our register has also contributed to first aid treatment practice by highlighting the importance of intramuscular adrenaline as first-line treatment.
All patients experiencing a severe allergic reaction should be sent to an allergologist who will evaluate the causative agent, provide guidance for avoidance and prevention, and also consider SIT. The patient, family members, and caregivers must be instructed on how to use an adrenaline autoinjector.
Acknowledgements
This article is associated with the Finnish Allergy Programme 2008-2018 and the World Health Organization Global Alliance against Chronic Respiratory Diseases Project.
References
- Johansson SG, Hourihane JO, Bousquet J, Bruijnzeel-Koomen C, Dreborg S, Haahtela T. et al. A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy. 2001;1:813–824. doi: 10.1034/j.1398-9995.2001.t01-1-00001.x. [DOI] [PubMed] [Google Scholar]
- Simons FER. Anaphylaxis. J Allergy Clin Immunol. 2008;1:S402–S407. doi: 10.1016/j.jaci.2007.08.061. [DOI] [PubMed] [Google Scholar]
- Sicherer SH, Mundoz-Furlong A, Sampson HA. Prevalence of peanut and tree nut allergy in the United States determined by means of a random digit dial telephone survey: a 5-year follow-up study. J Allergy Clin Immunol. 2003;1:1203–1207. doi: 10.1016/S0091-6749(03)02026-8. [DOI] [PubMed] [Google Scholar]
- Løvik M, Namork E, Fæste C, Egaas E. The Norwegian national reporting system and register of severe allergic reactions to food. Norsk Epidemiologi. 2004;1:155–160. [Google Scholar]
- Foucard T, Malmheden Yman I. A study on severe food reactions in Sweden--is soy protein an underestimated cause of food anaphylaxis? Allergy. 1999;1:261–265. doi: 10.1034/j.1398-9995.1999.00924.x. [DOI] [PubMed] [Google Scholar]
- Foucard T, Malmheden Yman I. Food-induced anaphylaxis. Pediatr Allergy Immunol. 2001;1(suppl 14):97–101. doi: 10.1034/j.1399-3038.2001.121421.x. [DOI] [PubMed] [Google Scholar]
- Colver AF, Nevantaus H, Macdougall CF, Cant AJ. Severe food-allergic reactions in children across the UK and Ireland, 1998-2000. Acta Pædiatrica. 2005;1:689–695. doi: 10.1111/j.1651-2227.2005.tb01966.x. [DOI] [PubMed] [Google Scholar]
- Peng MM, Jick H. A population-based study of the incidence, cause, and severity of anaphylaxis in the United Kingdom. Arch Intern Med. 2004;1:317–319. doi: 10.1001/archinte.164.3.317. [DOI] [PubMed] [Google Scholar]
- Helbling A, Hurni T, Müller UR, Pichler WJ. Incidence of anaphylaxis with circulatory symptoms: a study over a 3-year period comprising 940 000 inhabitants of the Swiss Canton Bern. Clin Exp Allergy. 2004;1:285–290. doi: 10.1111/j.1365-2222.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- Moneret-Vautrin DA, Morisset M, Flabbee J, Beaudoin E, Kanny G. Epidemiology of life-threatening and lethal anaphylaxis: a review. Allergy. 2005;1:443–451. doi: 10.1111/j.1398-9995.2005.00785.x. [DOI] [PubMed] [Google Scholar]
- Gupta R, Sheikh A, Strachan D, Anderson HR. Increasing hospital admissions for systemic allergic disorders in England: analysis of national admissions data. BMJ. 2003;1:1142–1143. doi: 10.1136/bmj.327.7424.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R, Sheikh A, Strachan DP, Anderson HR. Time trends in allergic disorders in the UK. Thorax. 2007;1:91–96. doi: 10.1136/thx.2004.038844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jirapongsananuruk O, Bunsawansong W, Piyaphanee N, Visitsunthorn N, Thongngarm T, Vichyanond P. Features of patients with anaphylaxis admitted to a university hospital. Ann Allergy Asthma Immunol. 2007;1:157–162. doi: 10.1016/S1081-1206(10)60689-8. [DOI] [PubMed] [Google Scholar]
- Sampson HA. Anaphylaxis and emergency treatment. Pediatrics. 2003;1:1601–1608. [PubMed] [Google Scholar]
- Pumphrey R. Anaphylaxis: can we tell who is at risk of the fatal reaction? Curr Opin Allergy Clin Immunol. 2004;1:285–290. doi: 10.1097/01.all.0000136762.89313.0b. [DOI] [PubMed] [Google Scholar]
- Pumphrey RSH. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;1:1144–1150. doi: 10.1046/j.1365-2222.2000.00864.x. [DOI] [PubMed] [Google Scholar]
- Uguz A, Lack G, Pumphrey R, Ewan P, Warner J, Dick J. et al. Allergic reactions in the community: a questionnaire survey of members of the anaphylaxis campaign. Clin Exp Allergy. 2005;1:746–750. doi: 10.1111/j.1365-2222.2005.02257.x. [DOI] [PubMed] [Google Scholar]
- Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson AN Jr, Bock SA, Brown SGA. et al. Second symposium on the definition and management of anaphylaxis: summary report-Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;1:391–397. doi: 10.1016/j.jaci.2005.12.1303. [DOI] [PubMed] [Google Scholar]
- Mäkinen-Kiljunen S, Kiistala R, Varjonen E. Severe reactions from roe without concomitant fish allergy. Ann Allergy Asthma Immunol. 2003;1:413–416. doi: 10.1016/S1081-1206(10)61691-2. [DOI] [PubMed] [Google Scholar]
- Süss A, Rytter M, Sticherling M, Simon JC. Anaphylaktische Reaktion auf ein Sojagetränk bei drei Patienten mit Birkenpollenallergie. JDDG. 2005;1:895–897. doi: 10.1111/j.1610-0387.2005.05749.x. [DOI] [PubMed] [Google Scholar]
- Airola K, Petman L, Mäkinen-Kiljunen S. Clustered sensitivity to fungi: anaphylactic reactions caused by ingestive allergy to yeasts. Ann Allergy Asthma Immunol. 2006;1:294–297. doi: 10.1016/S1081-1206(10)60792-2. [DOI] [PubMed] [Google Scholar]
- Aalto-Korte K, Mäkinen-Kiljunen S. Symptoms of immediate chlorhexidine hypersensitivity in patients with a positive prick test. Contact Dermatitis. 2006;1:173–177. doi: 10.1111/j.1600-0536.2006.00900.x. [DOI] [PubMed] [Google Scholar]
- Hyry H, Vuorio E, Varjonen E, Skyttä J, Mäkinen-Kiljunen S. Two cases of anaphylaxis to macrogol 600 after ingestion of drug tablets. Allergy. 2006;1:1021. doi: 10.1111/j.1398-9995.2006.01083.x. [DOI] [PubMed] [Google Scholar]
- Pastorello EA, Rivolta F, Bianchi M, Mauro M, Pravettoni V. Incidence of anaphylaxis in the emergency department of a general hospital in Milan. J Chrom B. 2001;1:11–17. doi: 10.1016/S0378-4347(01)00067-6. [DOI] [PubMed] [Google Scholar]
- Ellis AK, Day JH. Incidence and characteristics of biphasic anaphylaxis: a prospective evaluation of 103 patients. Ann Allergy Asthma Immunol. 2007;1:64–69. doi: 10.1016/S1081-1206(10)60861-7. [DOI] [PubMed] [Google Scholar]
- Mehl A, Wahn Y, Niggemann B. Anaphylactic reactions in children--a questionnaire-based survey in Germany. Allergy. 2005;1:1440–1445. doi: 10.1111/j.1398-9995.2005.00909.x. [DOI] [PubMed] [Google Scholar]
- Webb LM, Liebermann P. Anaphylaxis: a review of 601 cases. Ann Allergy Asthma Immunol. 2006;1:39–43. doi: 10.1016/S1081-1206(10)61367-1. [DOI] [PubMed] [Google Scholar]
- Derby CJ, Gowland MH, Hourihane JOB. Sesame allergy in Britain: a questionnaire survey of members of the Anaphylaxis Campaign. Pediatr Allergy Immunol. 2005;1:171–175. doi: 10.1111/j.1399-3038.2005.00232.x. [DOI] [PubMed] [Google Scholar]
- Thong BY-H, Chan Y. Anaphylaxis during surgical and interventional procedures. Ann Allergy Asthma Immunol. 2004;1:619–628. doi: 10.1016/S1081-1206(10)61427-5. [DOI] [PubMed] [Google Scholar]
- Karila C, Brunet-Langot D, Labbez F, Jacqmarcq O, Ponvert C, Paupe J. et al. Anaphylaxis during anesthesia: results of a 12-year survey at a French pediatric center. Allergy. 2005;1:828–834. doi: 10.1111/j.1398-9995.2005.00787.x. [DOI] [PubMed] [Google Scholar]


