Abstract
Objective
To identify serum biomarkers of papillary thyroid cancer.
Methods
Prospective analysis was performed of banked tumor and serum specimens from 99 patients with thyroid masses. Enzyme-linked immunosorbent assay (ELISA) was employed to measure levels of five serum proteins previously demonstrated to be up-regulated in papillary thyroid cancer (PTC): angiopoietin-1 (Ang-1), cytokeratin 19 (CK-19), tissue inhibitor of metalloproteinase-1 (TIMP-1), chitinase 3 like-1 (YKL-40), and galectin-3 (GAL-3). Serum levels were compared between patients with PTC and those with benign tumors.
Results
A total of 99 patients were enrolled in the study (27 men, 72 women), with a median age of 54 years. Forty-three patients had PTC and 58 cases were benign tumors. There were no statistically significant differences when comparing all five different biomarkers between PTC and other benign thyroid tumors. The p-values were 0.94, 0.48, 0.72, 0.48, and 0.90 for YKL-40, Gal-3, CK19, TIMP-1, and Ang-1, respectively.
Conclusion
Serum levels of four of the five proteins were elevated in patients with thyroid masses relative to normal values. However, the difference between benign and PTC was not significant. Two of the markers (Gal-3 & TIMP-1) displayed a greater potential difference, which may warrant further investigation. This study suggests that other serum markers should be sought. This is the first study to investigate potential serum biomarkers based on over-expressed proteins in thyroid cancer versus benign pathology.
Keywords: Thyroid, Cancer, Papillary, Serum biomarkers
Introduction
Papillary thyroid cancer (PTC) is one of the few cancers whose incidence is on the rise. It is considered the most rapidly increasing of all cancers in Canada [1]. Incidence has increased by 6.8% per year in males and 8.8% per year in females since 1998 in Canada with similar results noted in Europe and the United States [1]. Risk factors for thyroid cancers include prior radiation, family history and genetics. Treatment by surgery and radio-iodine therapy is highly effective; however, due to the difficulty in accurate diagnosis of thyroid cancer, surgery is often performed on benign nodules. Benign thyroid masses such goiter, follicular adenomas and cysts are approximately ten times more common than thyroid cancers [2]. Pre-operative diagnostic tests such as U/S, CT scan, and fine needle aspirate (FNA) often do not provide a definitive diagnosis. In these indeterminate cases, diagnostic hemithyroidectomy surgery is often performed and up to 75% of these patients have benign disease [3].
Research into the use of genomic techniques for improved diagnosis has focused on transcript profiling of well-differentiated thyroid cancer [4]. Genes that appear to be up-regulated in these studies are numerous. Jazab et al. demonstrated in a group of 16 patients with PTC increased gene expression for lectin, galactoside-binding, soluble, 3 (LGALS3) which codes for galectin-3 (Gal-3) protein, tissue inhibitor of metalloproteinases 1 (TIMP1), and chitinase 3-like 1 (CHI3L1) which is also known as YKL-40 [5]. Baris et al. noted high expression of adenosine deaminase (ADA), eukaryotic translation initiation factor 2 subunit 2 (EIF2S2), TIMP1, cyclin D1 (CCND1), cadherin-3 (CDH3) and collagen, type VIII, alpha 1 (COL8A1) in PTC [6]. Niedźwiecki et al. explored the role of angiopoietin 1 and 2 in thyroid cancers, showing a negative correlation of angiopoietin-1 (Ang-1) with state of malignancy [7]. Based on a review of these and other published studies using gene expression analysis, we concluded that YKL-40, Gal-3, cytokeratin 19 (CK19), TIMP-1 and Ang-1 were consistently found to be upregulated.
An alternative approach to tumor transcript profiling is protein profiling of serum. The main advantages of this approach are that it is minimally invasive, relatively safe and can be performed repeatedly. This could provide the basis for a useful test for screening, diagnosis, treatment and followup. However, the high complexity of serum makes identification of biomarkers challenging. Relative to healthy controls, the levels of serum vascular endothelial growth factor (VEGF) and matrix metallopeptidase 9 (MMP-9) are elevated in late-stage PTC; however, as the levels of these markers do not differentiate between goiter and early stage PTC, they are not useful for improving diagnosis [8]. Levels of biotinidase, clusterin, cysteine-rich, angiogenic inducer, 61 (CYR61), enolase 1, nucleolin and prothymosin alpha (PTMA) have been compared between PTC patients and healthy controls but no comparison was made with patients with benign nodules [9]. In spite of these advances, there are currently no validated serum markers for the diagnosis of PTC or for risk stratification of thyroid masses.
Our objective was to identify potential serum markers in subjects with PTC. We hypothesized that markers that have been shown to be highly expressed in PTC tumor tissue, especially those that are secreted or present at the cell surface, would also be elevated in serum, and thus measurable by serum enzyme-linked immunosorbent assay (ELISA) analysis.
Materials & methods
Subjects
This was a prospective study. All patients provided informed consent and the study was approved by the local Hospital Ethics Committee. All patients ≥ 18 years old and undergoing hemi-thyroidectomy or total thyroidectomy from July 2009 to June 2011 were enrolled initially in the study. Patients with human immunodeficiency virus or viral hepatitis were not included in the study for investigator handling safety reasons. After post-operative pathological evaluation, all patients with thyroid cancer other than PTC were excluded. Patients were then divided into two main groups based on their diagnosis: 1) PTC group and 2) control group. The control group included all patients with benign thyroid pathology. All specimens were then bar-coded and patient identifiers removed in order to protect their anonymity and also to blind the operators conducting the ELISA analysis.
Specimen collections (serum & tissue)
In the operating room prior to induction of general anesthesia, 2 red top vials of blood were drawn from all patients. The tubes were left at room temperature for 20-30 minutes to clot and then centrifuged at 3000 rpm for 10 minutes. If serum separation from erythrocytes was incomplete, the centrifugation step was repeated. The serum was aliquoted into 5-8 300 μl microcentrifuge tubes in order to limit the number of freeze-thaw cycles to one. At the same time, immediately upon completion of the procedure, the thyroid specimen was processed by a single study pathologist (M.B.). A representative portion of the mass was also preserved in ribonucleic acid stabilizing reagent (RNAlater, Ambion) for future analysis. Both serum and tissue specimens were subsequently stored in a freezer at -80°C.
Enzyme-linked immunosorbent assay
All the collected serum specimens were analyzed by ELISA according to the manufacturers’ instructions. ELISA kits for Ang-1 (catalog number DANG10), TIMP-1 (catalog number DTM100) and Gal-3 (catalog number DGAL30) were from the Research and Diagnostics (R&D) Systems, Inc., Minneapolis, MN, USA. The kit for YKL-40 (catalog number Microvue YKL-40 8020 (QI)) was made by Quidel Corp., San Diego, CA, USA. The CK19 ELISA kit (catalog number CSB-E09180H) was from CUSABIO, (http://www.cusabio.com). All ELISA washing steps were performed using a BioTek Elx50 microplate strip washer programmed as required. All readings were made on a Spectramax 384 Plus plate reader (Molecular Devices, Sunnyvale, CA, USA) using the SoftMax Pro software package. All samples, standards and blanks were analyzed in duplicate.
Statistical analysis
P values for the comparison of the means of the PTC and control groups for each of the 5 serum proteins were determined using t-tests. Random forest classification was performed using the R package random Forest. The random forest analysis was carried out with parameters ntree, mtry and nodesize set to 50 000, 3 and 1 respectively. Normal values for each of the 5 serum proteins were taken from references as indicated [10-14].
Results
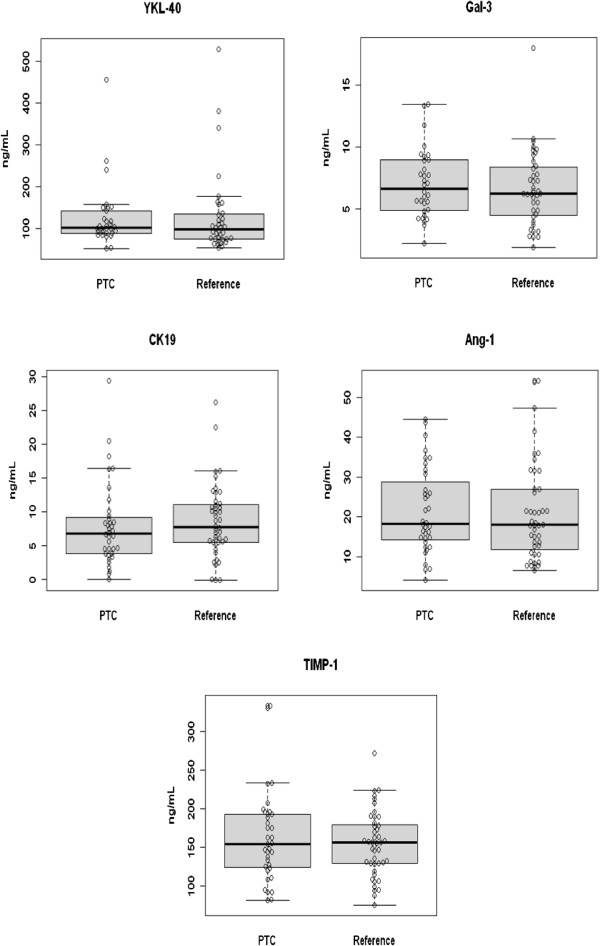
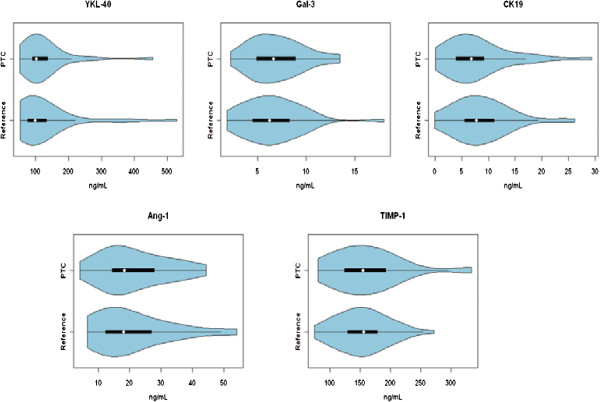
A total of 99 patients were enrolled in the study (42 PTC & 57 benign). The patients’ characteristics are summarized in Tables 1 &2. Each of the five potential serum markers were measured by ELISA and the levels were compared between PTC patients and the control group, consisting of all benign thyroid conditions. As can be seen in Table 3 & Figure 1, no significant differences were detected for any of the proteins measured. Therefore, the serum levels of these proteins are not diagnostic using univariate statistical analysis. The serum levels of these markers were also plotted using violin plots (Figure 2). In these plots the width of the image is proportional to the number of patients at each serum value. This can aid in the identification of smaller subsets of patients with elevated levels in cases where the mean is dominated by the bulk of the patient values. However, again in this case, no significant sub-groups are apparent.
Table 1.
Patients characteristics
| |
Age |
Sex |
|||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean | Median | Male | Female | Total | |
|
PTC |
19 |
78 |
52.9 |
54 |
17 |
25 |
42 |
|
Benign |
30 |
81 |
53.7 |
54 |
10 |
47 |
57 |
| All | 19 | 81 | 53.4 | 54 | 27 | 72 | 99 |
Table 2.
PTC patients’ and tumor characteristics
| # | Sex | Age | Dx* | Procedure | Level 6 (yes = 1, no = 0) | Level 6 nodes (positive/total) | Lateral neck (yes = 1, no = 0) | Neck nodes (positive/total) | Tumor diameter (cm) | LVI* (yes = 1, no = 0) | ETE* (yes = 1, no = 0) | Multicentricity (yes = 1, no = 0) | Number of foci |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
1 |
M |
42 |
MP* |
Hemi *(Lt) |
1 |
0/3 |
0 |
_ |
0.1 |
0 |
0 |
0 |
1 |
|
2 |
F |
53 |
PTC* |
Total Thyroid* |
1 |
1/12 |
0 |
_ |
0.7 |
0 |
1 |
0 |
1 |
|
3 |
F |
38 |
MP |
Hemi (Rt) |
0 |
0 |
0 |
_ |
0.3 |
0 |
0 |
1 |
2 |
|
4 |
F |
69 |
PTC |
Hemi (Lt) |
1 |
6/16 |
1 |
4/98 |
0.2 |
0 |
0 |
1 |
3 |
|
5 |
M |
59 |
MP |
Total Thyroid |
1 |
0/17 |
0 |
_ |
0.2 |
0 |
0 |
0 |
1 |
|
6 |
M |
55 |
PTC |
Total Thyroid |
1 |
0/7 |
0 |
_ |
0.3 |
0 |
0 |
1 |
5 |
|
7 |
F |
35 |
PTC |
Total Thyroid |
1 |
0/18 |
0 |
_ |
5.5 |
0 |
0 |
1 |
7 |
|
8 |
F |
42 |
MP |
Hemi (Rt) |
0 |
0 |
0 |
_ |
0.2 |
0 |
0 |
1 |
2 |
|
9 |
F |
36 |
PTC |
Hemi (Rt) |
0 |
0 |
0 |
_ |
3 |
0 |
0 |
1 |
6 |
|
10 |
M |
46 |
PTC |
Hemi (Lt) |
0 |
0 |
0 |
_ |
6.5 |
1 |
0 |
1 |
2 |
|
11 |
F |
19 |
PTC |
Total Thyroid |
1 |
3/4 |
1 |
10/37 |
7 |
1 |
1 |
1 |
+* |
|
12 |
M |
63 |
PTC |
Total Thyroid |
1 |
0/7 |
0 |
- |
1 |
0 |
0 |
0 |
1 |
|
13 |
M |
57 |
PTC |
Total Thyroid |
1 |
4/13 |
0 |
- |
2 |
1 |
1 |
0 |
1 |
|
14 |
M |
67 |
PTC |
Total Thyroid |
1 |
0/2 |
0 |
_ |
1.3 |
0 |
0 |
1 |
4 |
|
15 |
M |
40 |
PTC |
Total Thyroid |
1 |
11/15 |
1 |
13/44 |
0.5 |
1 |
0 |
1 |
10 |
|
16 |
M |
66 |
MP |
Hemi (Lt) |
1 |
0/1 |
0 |
_ |
2.5 |
0 |
0 |
0 |
1 |
|
17 |
F |
53 |
PTC |
Total Thyroid |
1 |
0/5 |
0 |
_ |
4 |
0 |
0 |
1 |
2 |
|
18 |
M |
77 |
PTC |
Total Thyroid |
0 |
0 |
0 |
_ |
0.3 |
0 |
0 |
1 |
3 |
|
19 |
F |
56 |
PTC |
Hemi (Lt) |
0 |
0 |
0 |
_ |
1.7 |
0 |
0 |
0 |
1 |
|
20 |
F |
47 |
PTC |
Hemi (Rt) |
0 |
0 |
0 |
_ |
1.1 |
0 |
0 |
1 |
3 |
|
21 |
F |
58 |
PTC |
Total Thyroid |
1 |
0/6 |
0 |
_ |
1.6 |
0 |
0 |
1 |
2 |
|
22 |
F |
56 |
PTC |
Total Thyroid |
1 |
0/20 |
0 |
_ |
2 |
1 |
1 |
1 |
2 |
|
23 |
M |
53 |
PTC |
Total Thyroid |
1 |
7/18 |
1 |
11/46 |
1.8 |
0 |
1 |
1 |
+ |
|
24 |
F |
75 |
PTC |
Total Thyroid |
1 |
0/13 |
0 |
_ |
0.5 |
0 |
0 |
1 |
2 |
|
25 |
F |
35 |
PTC |
Hemi (Lt) |
0 |
0 |
0 |
_ |
1.3 |
0 |
0 |
1 |
3 |
|
26 |
F |
41 |
PTC |
Total Thyroid |
1 |
3/12 |
0 |
_ |
1.7 |
0 |
0 |
1 |
10 |
|
27 |
F |
62 |
PTC |
Total Thyroid |
1 |
0/13 |
0 |
_ |
2.2 |
0 |
0 |
0 |
1 |
|
28 |
M |
42 |
PTC |
Total Thyroid |
1 |
4/6 |
0 |
_ |
1.7 |
1 |
1 |
0 |
1 |
|
29 |
F |
72 |
PTC |
Hemi (Rt) |
0 |
0 |
0 |
_ |
1.5 |
0 |
0 |
0 |
1 |
|
30 |
M |
37 |
PTC |
Total Thyroid |
1 |
0/11 |
0 |
_ |
4.5 |
0 |
0 |
0 |
1 |
|
31 |
M |
72 |
PTC |
Total Thyroid |
1 |
7/9 |
1 |
9/18 |
2.5 |
1 |
1 |
1 |
+ |
|
32 |
F |
37 |
PTC |
Total Thyroid |
1 |
0/9 |
0 |
_ |
1.5 |
0 |
0 |
0 |
1 |
|
33 |
F |
40 |
PTC |
Total Thyroid |
1 |
0/6 |
0 |
_ |
0.9 |
0 |
0 |
1 |
4 |
|
34 |
F |
40 |
PTC |
Total Thyroid |
1 |
7/8 |
0 |
_ |
4 |
1 |
0 |
1 |
2 |
|
35 |
F |
35 |
PTC |
Total Thyroid |
1 |
1/13 |
|
|
1.o |
|
0 |
0 |
1 |
|
36 |
M |
78 |
PTC |
Hemi (Rt) |
0 |
0 |
0 |
_ |
8 |
0 |
0 |
0 |
1 |
|
37 |
F |
61 |
MP |
Hemi (Rt) |
0 |
0 |
0 |
_ |
<0.1 |
0 |
0 |
0 |
1 |
|
38 |
M |
77 |
MP |
Total Thyroid |
0 |
0 |
0 |
_ |
0.4 |
0 |
0 |
0 |
1 |
|
39 |
F |
70 |
MP |
Hemi (Rt) |
0 |
0 |
0 |
_ |
0.2 |
0 |
0 |
1 |
2 |
|
40 |
M |
56 |
PTC |
Total Thyroid |
1 |
2/3 |
1 |
0 |
2.5 |
1 |
1 |
0 |
1 |
|
41 |
F |
49 |
MP |
Hemi (Lt) |
0 |
0 |
0 |
_ |
0.1 |
0 |
0 |
0 |
1 |
| 42 | F | 56 | MP | Hemi (Rt) | 0 | 0 | 0 | _ | 0.1 | 0 | 0 | 0 | 1 |
* Dx: Diagnosis, ETE: Extra thyroid extension, Hemi: Hemithyroidectomy, Lt: Left, LVI: Lymphovascular Invasion, MP: Micropapillary, PTC: Papillary Thyroid Cancer, Rt: Right, Total thyroid: Total thyroidectomy, +: Innumerable.
Table 3.
Tumor marker serum measurement values
| YKL-40 | Gal-3 | CK-19 | Ang-1 | TIMP-1 | |
|---|---|---|---|---|---|
|
PTC |
129 ± 77 |
7.07 ± 2.79 |
8.1 ± 6.1 |
21 ± 11 |
162 ± 60 |
|
Reference |
129 ± 99 |
6.6 ± 3.0 |
8.6 ± 5.4 |
21 ± 12 |
154 ± 42 |
|
P-value |
0.995 |
0.488 |
0.730 |
0.483 |
0.910 |
| Normala | 43 ± 25 [10] | 2.2 [11] | 1.4 +0.3 [12] | 58 ± 5 [13] | 95 + 26 [14] |
* All concentrations in ng/ml, a Values taken from references as indicated.
Figure 1.
Boxplot of serum marker levels in the PTC and reference group, which consists of all benign conditions. Boxes contain 25th and 75th percentile.
Figure 2.
Violin plot of serum marker levels in the PTC and reference group, which consists of all benign conditions. Width of the object is proportional to the number of patients with a particular serum concentration.
The potential markers were also analyzed using multivariate statistical analysis. Specifically, the data were analyzed using random forest analysis using R [15]. In this technique, approximately two thirds of the samples were chosen at random to generate a classification tree. At each tree node a random subset of variables (mtry) was selected with the variable responsible for the largest split used to split the node. This process was iterated ntree number of times to create an ensemble of classification trees in which sample prediction is accomplished through a majority vote. As in the case of the univariate analysis, the multivariate analysis using random forest did not reveal any serum markers that were significant for diagnosis. In Figure 3, the box plot shows that the margin, which is a measure of the ability to distinguish the two groups using the serum marker levels, is close to zero. This indicates poor predictive ability. Similarly, the plot on the right of Figure 3 shows little separation for the PTC and reference groups.
Figure 3.

Boxplot of the margin of prediction (positive values indicate correct classification). Multi-dimensional scaling plot of the random forest proximity measure.
Discussion
Up to this date the gold standard for the diagnosis of thyroid cancer remains pathological evaluation of surgically obtained thyroid tissue. Since the introduction of FNA in the 1970s the preoperative diagnostic accuracy of thyroid nodules has greatly improved [16]. However, FNA still has significant limitation in the diagnosis of thyroid nodules with an overall sensitivity and specificity from 65-98% and 72-100%, respectively [17]. Microarray technology has significantly improved the understanding of cancer pathophysiology as well by providing valuable clinical information. This has yielded multiple genes that have been demonstrated to be up-regulated in PTC. Certain genes encode secretory proteins that with the use of commercially available ELISA kits are measurable in serum. In 2001, Huang et al. published the first study describing genes that are up-regulated in PTC based on microarray [18]. Comparing 8 pairs of normal and PTC thyroid tissue resulted in the detection of 24 genes that were up-regulated in PTC [18]. In the present study we measured serum levels of YKL-40, Gal-3, CK19, TIMP-1 and Ang-1 proteins using a commercially available ELISA kit.
Tissue inhibitor of metalloproteinase-1 (TIMP-1)
As its name suggests, TIMP-1 inhibits a variety of metalloproteinases. Its expression is dependent on BRAF and NF-κB using in vitro models, where it also influences proliferation [19]. High expression of TIMP-1 is indicative of an invasive phenotype. In 2000, Maeta et al. investigated the expression of both the TIMPs and matrix metalloproteinases (MMPs) in PTC, which were up-regulated relative to normal tissue [20]. Similar results were also obtained by others and confirmed at the protein level [21-25]. Serum levels in thyroid cancer patients have not been previously measured; however, levels in pancreatic cancer patients and, to a lower extent in chronic pancreatitis, have been shown to have diagnostic potential [26]. In metastatic breast cancer patients, elevated serum TIMP-1 levels were shown to correlate with poor response to therapy and lower overall survival [27]. In our study the TIMP-1 levels in PTC and control samples were 162 ng/ml and 154 ng/ml, respectively. The serum level did not show any significant difference despite the strong evidence in the literature for elevated gene and protein expression of TIMP-1. This is the first study to demonstrate equivalent levels of serum TIMP-1 in patients with PTC and benign thyroid nodules.
Chitinase 3-like 1 (YKL-40)
Chitiniase 3-like 1 has been found to be up-regulated in PTC [18] and in numerous other cancers where it appears to promote angiogenesis [28]. The serum levels of this protein, which is also known as YKL-40, have not been studied in PTC patients. However, it has been found to be elevated in the serum of patients suffering from various other cancers although it is also elevated in various inflammatory conditions [29]. The mean concentration of YKL-40 in both PTC and control samples was 129 ng/mL, which is higher than the level reported in healthy controls (43 ng/ml) [10].
Lectin, galactoside-binding, soluble, 3 (LGALS3), galectin – 3 (Gal-3)
Galectins are a family of carbohydrate-binding proteins with a high affinity for β-galactoside. Gal-3 is implicated in cell growth and differentiation, cell adhesion, angiogenesis, tumor progression, apoptosis and metastasis and has been detected in many human tumors and cell lines, including thyroid, colon and breast. It has been identified in a number of different tumors, and Xu et al. reported that it is expressed preferentially in papillary and follicular carcinoma at a high level and in medullary carcinoma at a variable level [30]. Bartolazzi et al. used monoclonal antibodies to Gal-3 on 1009 archival tissues and 226 fresh specimens and reported 99% sensitivity and 98% specificity in discriminating benign from malignant lesions [31]. However, a recent study on PTC has observed that there was a decreased intensity of Gal-3 expression at the invasive edges of the tumors during tumor progression [32]. In 2010 Htwe et al. showed a significant (p = 0.001) stronger expression of Gal-3 in the advancing follicular cells at the periphery of thyroid cancer lesions, which was more pronounced in PTC than follicular carcinoma of the thyroid [33]. In our study the mean value of Gal-3 in PTC and control samples were 7.07 and 6.6 ng/ml, respectively, and the p-value was 0.48. These results are consistent with those of Saussez et al. who observed elevated Gal-3 levels in patients with PTC but found significant overlap with Gal-3 levels in patients with benign conditions [11].
Cytokeratin 19 (CK19)
Cytokeratins are filamentous proteins that participate in the integrity and cytoskeleton of the cells. CK19 has the lowest molecular weight of all the cytokeratins. It is normally expressed in ductal epithelium (bile ducts, pancreas, and renal collecting tubules) and in the mucosa of the gastrointestinal tract. The differential expression of cytokeratins has been evaluated in various thyroid lesions. Among various cytokeratins, CK19 has shown diffuse and strong cytoplasmic staining in PTC, which makes it useful in the diagnosis of PTC [34-39]. High molecular weight cytokeratin has also been found to be significantly increased in PTC and has been reported to be helpful in distinguishing it from other benign and malignant thyroid nodules [37,40]. In 2007, Park et al. had showed that CK19 immunoreactivity of follicular adenoma was higher than previously reported cases, and because of its low specificity this may limit its utility as a diagnostic marker [41]. Our serum protein measurement didn’t show any significant difference between PTC and benign thyroid pathology.
Angiopoietin-1 (Ang-1)
Angiopoietins (Ang1 and Ang2) are structurally related growth factors, and contribute to angiogenesis upon binding to Tie2 receptor [42]. Ang1 is known as a Tie2 agonist capable of inducing EC migration and proliferation [43-46]. Interaction of angiopoietins with vascular endothelial growth factors (VEGF) in different kinds of tumor tissue is important for tumor growth and possible local invasion or distant metastasis [47-49]. In 2006, Niedźwiceki et al. measured serum levels of Ang-1 using ELISA and showed statistically significant lower concentrations of Ang-1 in patients with thyroid cancers versus patients without thyroid pathology [7]. In contrast, in 2011, Hsueh et al. demonstrated the expression of Ang-1, Ang-2, and Tie-2 in normal benign and PTC tissues and significantly high expression of Ang-1 in metastatic PTC cases [50]. Based on their results they also concluded that Ang-1, Ang-2, Tei-2 receptor, and VEGF play important roles in progression of clinical stages of PTC [50]. Our measurements were consistent with those of Niedźwiceki et al. [7] levels of Ang-1 were lower in PTC compared to normal. However, there was no difference between serum Ang-1 levels in PTC and the benign nodule group.
Despite significant evidence in the literature for elevation of these markers in tumor tissue, the same is not true for serum. Underlying theories why serum values of these markers were not consistent with the tissue values are unknown at this stage. In tumor tissue, the availability of adjacent normal tissue facilitates identification of markers. No such internal control is possible for serum analysis; therefore, in the case of serum markers, there must be a very large difference in concentration in order for the marker to be useful for diagnostic purposes.
Conclusion
Although the results of this study did not demonstrate a statistically significant difference in serum levels of YKL-40, Gal-3, CK19, TIMP-1 and Ang-1 between PTC patients and those with benign conditions, it does demonstrate the potential feasibility of a blood-based diagnostic test. It also demonstrates that although there may be up-regulation of several of these gene products in PTC tissue, this may not be representative of overexpression of the proteins in serum.
With the rising incidence of thyroid cancer the need for an accurate diagnostic test is becoming paramount and development of such a test may significantly reduce patient morbidity and unnecessary surgery in benign thyroid disease. Obviously further study is required.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FM, AS, & KI: Ethics approval, patient enrollment, blood and tissue collection and serum extraction. SD selected candidates for ELISA and assays were performed by JG at the National Research Council. SMT & JT: staff head & neck surgeons. MB: pathologist. DP, AL, & TE: data acquisition and tracking. All authors read and approved the final manuscript.
Contributor Information
Fawaz M Makki, Email: f50_fawaz@hotmail.com.
S Mark Taylor, Email: Smtaylorwashu@yahoo.com.
Ali Shahnavaz, Email: ali_shahnavaz@hotmail.com.
Andrew Leslie, Email: Andrew.Leslie@nrc-cnrc.gc.ca.
Jeffrey Gallant, Email: Jeffrey.Gallant@nrc-cnrc.gc.ca.
Susan Douglas, Email: Susan.Douglas@nrc-cnrc.gc.ca.
Evelyn Teh, Email: Evelyn.Teh@nrc-cnrc.gc.ca.
Jonathan Trites, Email: jonathan.trites@cdha.nshealth.ca.
Martin Bullock, Email: martin.bullock@cdha.nshealth.ca.
Karen Inglis, Email: karen.inglis@cdha.nshealth.ca.
Devanand M Pinto, Email: devanand.pinto@nrc-cnrc.gc.ca.
Robert D Hart, Email: drrobhart@hotmail.com.
References
- Chappell H, Pritwish D, Dryer D, Ellison L, Logan H, MacIntyre M. Canadian cancer Society’s steering committee on cancer statistics. Toronto, ON: Canadian Cancer Society; 2011. [Google Scholar]
- Meinhold CL, Ron E, Schonfeld SJ, Alexander BH, Freedman DM, Linet MS. Nonradiation risk factors for thyroid cancer in the US radiologic technologists study. Am J Epidemiol. 2010;171(2):242–252. doi: 10.1093/aje/kwp354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiseman S, Baliski C, Irvine R, Anderson D, Wilkins G, Filipenko D. Hemithyroidectomy: the optimal initial surgical approach for individuals undergoing surgery for a cytological diagnosis of follicular neoplasm. Ann Surg Oncol. 2006;13(3):425–432. doi: 10.1245/ASO.2006.03.089. [DOI] [PubMed] [Google Scholar]
- Griffith OL, Melck A, Jones SJM, Wiseman SM. Meta-analysis and meta-review of thyroid cancer gene expression profiling studies identifies important diagnostic biomarkers. J Clin Oncol. 2006;24(31):5043–5051. doi: 10.1200/JCO.2006.06.7330. [DOI] [PubMed] [Google Scholar]
- Jarzab B, Wiench M, Fujarewicz K, Simek K, Jarzab M, Oczko-Wojciechowska M. Gene expression profile of papillary thyroid cancer: sources of variability and diagnostic implications. Cancer Res. 2005;65(4):1587–1597. doi: 10.1158/0008-5472.CAN-04-3078. [DOI] [PubMed] [Google Scholar]
- Baris O, Mirebeau-Prunier D, Savagner F, Rodien P, Ballester B, Loriod B. Gene profiling reveals specific oncogenic mechanisms and signaling pathways in oncocytic and papillary thyroid carcinoma. Oncogene. 2005;24(25):4155–4161. doi: 10.1038/sj.onc.1208578. [DOI] [PubMed] [Google Scholar]
- Niedzwiecki S, Stepien T, Kopec K, Kuzdak K, Komorowski J, Krupinski R. Angiopoietin 1 (Ang-1), angiopoietin 2 (Ang-2) and Tie-2 (a receptor tyrosine kinase) concentrations in peripheral blood of patients with thyroid cancers. Cytokine. 2006;36(36):291–295. doi: 10.1016/j.cyto.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Lin SY, Wang YY, Sheu WH-H. Preoperative plasma concentrations of vascular endothelial growth factor and matrix metalloproteinase 9 are associated with stage progression in papillary thyroid cancer. Clin Endocrinol. 2003;58(4):513–518. doi: 10.1046/j.1365-2265.2003.01749.x. [DOI] [PubMed] [Google Scholar]
- Kashat L, So AK-C, Masui O, Wang XS, Cao J, Meng X. Secretome-based identification and characterization of potential biomarkers in thyroid cancer. J Proteome Res. 2010;9(11):5757–5769. doi: 10.1021/pr100529t. [DOI] [PubMed] [Google Scholar]
- Johansen JS, Lottenburger T, Nielsen HJ, Jensen JEB, Svendsen MN, Kollerup G. Diurnal, weekly, and long-time variation in serum concentrations of YKL-40 in healthy subjects. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2603–2608. doi: 10.1158/1055-9965.EPI-07-2766. [DOI] [PubMed] [Google Scholar]
- Saussez SGD, Chantrain G, Pattou F, Carnaille B, André S, Gabius HJ, Laurent G. Serum galectin-1 and galectin-3 levels in benign and malignant nodular thyroid disease. Thyroid. 2008;18(7):705–712. doi: 10.1089/thy.2007.0361. [DOI] [PubMed] [Google Scholar]
- Uenishi T, Kubo S, Hirohashi K, Tanaka H, Shuto T, Yamamoto T. Cytokeratin-19 fragments in serum (CYFRA 21-1) as a marker in primary liver cancer. Br J Cancer. 2003;88(12):1894–1899. doi: 10.1038/sj.bjc.6601026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukasz A, Hellpap J, Horn R, Kielstein J, David S, Haller H. Circulating angiopoietin-1 and angiopoietin-2 in critically ill patients: development and clinical application of two new immunoassays. Critical Care. 2008;12(4):R94. doi: 10.1186/cc6966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noji Y, Kajinami K, Kawashiri M, Todo Y, Horita T, Nohara A. Circulating matrix metalloproteinases and their inhibitors in premature coronary atherosclerosis. Clin Chem Lab Med. 2001;39(5):380–384. doi: 10.1515/CCLM.2001.060. [DOI] [PubMed] [Google Scholar]
- Breiman L. Random forests. Machine Learning: Springer Netherlands; 2001. pp. 5–32. [Google Scholar]
- Kundel AZR, Kato M, Moo TA, Zhu B, Scognamiglio T, Fahey TJ 3rd. Comparison of microarray analysis of fine needle aspirates and tissue specimen in thyroid nodule diagnosis. Diagn Mol Pathol. 2010;19(1):9–14. doi: 10.1097/PDM.0b013e3181ae870c. [DOI] [PubMed] [Google Scholar]
- Gharib H, Goellner JR. Fine-needle aspiration biopsy of the thyroid: an appraisal. Ann Intern Med. 1993;118(4):282–289. doi: 10.7326/0003-4819-118-4-199302150-00007. [DOI] [PubMed] [Google Scholar]
- Huang Y, Prasad M, Lemon WJ, Hampel H, Wright FA, Kornacker K. Gene expression in papillary thyroid carcinoma reveals highly consistent profiles. Proc Natl Acad Sci USA. 2001;98(26):15044–15049. doi: 10.1073/pnas.251547398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bommarito A, Richiusa P, Carissimi E, Pizzolanti G, Rodolico V, Zito G. BRAFV600E mutation, TIMP-1 up-regulation and NF-KB activation: closing the loop on the papillary thyroid cancer trilogy. Endocr Relat Cancer. 2011;18(6):669–685. doi: 10.1530/ERC-11-0076. [DOI] [PubMed] [Google Scholar]
- Maeta H, Ohgi S, Terada T. Protein expression of matrix metalloproteinases 2 and 9 and tissue inhibitors of metalloproteinase 1 and 2 in papillary thyroid carcinomas. Virchows Archiv. 2001;438(2):121–128. doi: 10.1007/s004280000286. [DOI] [PubMed] [Google Scholar]
- Korem S, Resnick MB, Kraiem Z. Similar and divergent patterns in the regulation of matrix metalloproteinase-1 (MMP-1) and tissue inhibitor of MMP-1 gene expression in benign and malignant human thyroid cells. J Clin Endocrinol Metab. 1999;84(9):3322–3327. doi: 10.1210/jc.84.9.3322. [DOI] [PubMed] [Google Scholar]
- Shi Y, Parhar RS, Zou M, Hammami MM, Akhtar M, Lum Z-P. Tissue inhibitor of metalloproteinases-1 (TIMP-1) mRNA is elevated in advanced stages of thyroid carcinoma. Br J Cancer. 1999;79(7-8):1234–1239. doi: 10.1038/sj.bjc.6690198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraiem ZKS. Matrix metalloproteinases and the thyroid. Thyroid. 2000;10:1061–1069. doi: 10.1089/thy.2000.10.1061. [DOI] [PubMed] [Google Scholar]
- Komorowski JPZ, Jankiewicz-Wika J, Stepien H. Matrix metalloproteinases, tissue inhibitors of matrix metalloproteinases and angiogenic cytokines in peripheral blood of patients with thyroid cancer. Thyroid. 2000;12:655–662. doi: 10.1089/105072502760258622. [DOI] [PubMed] [Google Scholar]
- Patel A, Straight A, Mann H, Duffy E, Fenton C, Dinauer C. Matrix metalloproteinase (MMP) expression by differentiated thyroid carcinoma of children and adolescents. J Endocrinol Invest. 2002;25(5):403–408. doi: 10.1007/BF03344028. [DOI] [PubMed] [Google Scholar]
- Pan S, Chen R, Crispin DA, May D, Stevens T, McIntosh MW. Protein alterations associated with pancreatic cancer and chronic pancreatitis found in human plasma using global quantitative proteomics profiling. J. Proteome Res. 2011;10(5):2359–2376. doi: 10.1021/pr101148r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton A, Leitzel K, Chaudri-Ross HA, Evans DB, Ali SM, Demers L. Serum TIMP-1 and response to the aromatase inhibitor letrozole versus tamoxifen in metastatic breast cancer. J Clin Oncol. 2008;26(16):2653–2658. doi: 10.1200/JCO.2007.15.4336. [DOI] [PubMed] [Google Scholar]
- Shao R, Hamel K, Petersen L, Cao QJ, Arenas RB, Bigelow C. YKL-40, a secreted glycoprotein, promotes tumor angiogenesis. Oncogene. 2009;28(50):4456–4468. doi: 10.1038/onc.2009.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffman FD. Chitinase 3-Like-1 (CHI3L1): A putative disease marker at the interface of proteomics and glycomics. Crit Rev Clin Lab Sci. 2008;45(6):531–562. doi: 10.1080/10408360802334743. [DOI] [PubMed] [Google Scholar]
- Xu XC N-NA, Lotan R. Differential expression of galectin 1 and galectin-3 in thyroid tumors: potential diagnostic implications. Am J Pathol. 1995;147(3):815–822. [PMC free article] [PubMed] [Google Scholar]
- Bartolazzi A, Gasbarri A, Papotti M, Bussolati G, Lucante T, Khan A. Application of an immunodiagnostic method for improving preoperative diagnosis of nodular thyroid lesions. The Lancet. 2001;357(9269):1644–1650. doi: 10.1016/S0140-6736(00)04817-0. [DOI] [PubMed] [Google Scholar]
- Türköz HK OH, Yurdakul Z, Ozcan D. Galectin-3 expression in tumor progression and metastasis of papillary thyroid carcinoma. Endocr Pathol. 2008;19(2):92–96. doi: 10.1007/s12022-008-9033-3. [DOI] [PubMed] [Google Scholar]
- Htwe TTKN, Wong J, Jahanfar S, Mansur MA. Differential expression of galectin-3 in advancing thyroid cancer cells: a clue toward understanding tumour progression and metastasis. Singapore Med J. 2010;51(11):856–859. [PubMed] [Google Scholar]
- Prasad ML, Pellegata NS, Huang Y, Nagaraja HN, Chapelle A, Kloos RT. Galectin-3, fibronectin-1, CITED-1, HBME1 and cytokeratin-19 immunohistochemistry is useful for the differential diagnosis of thyroid tumors. Mod Pathol. 2005;18(1):48–57. doi: 10.1038/modpathol.3800235. [DOI] [PubMed] [Google Scholar]
- De Matos PS, Ferreira AP, De Oliveira Facuri F, Assumpção LVM, Metze K, Ward LS. Usefulness of HBME-1, cytokeratin 19 and galectin-3 immunostaining in the diagnosis of thyroid malignancy. Histopathol. 2005;47(4):391–401. doi: 10.1111/j.1365-2559.2005.02221.x. [DOI] [PubMed] [Google Scholar]
- Park MIKD. Usefulness of galectin-3, cytokeratin 19, p53, and Ki-67 for the differential diagnosis of thyroid tumors. Korean J Pathol. 2006;40:86–92. [Google Scholar]
- Raphael S, McKeown-Eyssen G, Asa S. High-molecular-weight cytokeratin and cytokeratin-19 in the diagnosis of thyroid tumors. Mod Pathol. 1994;7(3):295–300. [PubMed] [Google Scholar]
- Miettinen M, Kovatich AJ, Karkkainen P. Keratin subsets in papillary and follicular thyroid lesions. Virchows Archiv. 1997;431(6):407–413. doi: 10.1007/s004280050117. [DOI] [PubMed] [Google Scholar]
- Sahoo S, Hoda SA, Rosai J, DeLellis RA. Cytokeratin 19 immunoreactivity in the diagnosis of papillary thyroid carcinoma. Am J Clin Pathol. 2001;116(5):696–702. doi: 10.1309/6D9D-7JCM-X4T5-NNJY. [DOI] [PubMed] [Google Scholar]
- de Araujo VC, de Sousa SO, Carvalho YR, de Araujo NS. Application of immunohistochemistry to the diagnosis of salivary gland tumors. Appl Immunohistochem Mol Morphol. 2000;8(3):195–202. doi: 10.1097/00022744-200009000-00005. [DOI] [PubMed] [Google Scholar]
- Park YJ KS, Kim DC, Kim H, Choe G, Park do J, Jang HC, Park SH, Cho BY, Park SY. Diagnostic value of galectin-3, HBME-1, cytokeratin 19, high molecular weight cytokeratin, cyclin D1 and p27(kip1) in the differential diagnosis of thyroid nodules. Korean Medical Sciences. 2007;22(4):621–628. doi: 10.3346/jkms.2007.22.4.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asahara DCT, Takahashi T, Fujikawa K, Kearney M, Magner M, Yancopoulos GD, Isner JM. Tie2 receptor ligands, angiopoietin-1 and angiopoietin-2, modulate VEGF-induced postnatal neovascularization. Circ Res. 1998;83:233–240. doi: 10.1161/01.RES.83.3.233. [DOI] [PubMed] [Google Scholar]
- TI Koblizek CW, Yancopoulos GD, Deutsch U, Risau W. Angiopoietin-1 induces sprouting angiogenesis in vitro. Curr Biology. 1998;8:529–532. doi: 10.1016/S0960-9822(98)70205-2. [DOI] [PubMed] [Google Scholar]
- Kanda S, Miyata Y, Mochizuki Y, Matsuyama T, Kanetake H. Angiopoietin 1 is mitogenic for cultured endothelial cells. Cancer Res. 2005;65(15):6820–6827. doi: 10.1158/0008-5472.CAN-05-0522. [DOI] [PubMed] [Google Scholar]
- Thurston G, Suri C, Smith K, McClain J, Sato TN, Yancopoulos GD. Leakage-resistant blood vessels in mice transgenically overexpressing angiopoietin-1. Science. 1999;286(5449):2511–2514. doi: 10.1126/science.286.5449.2511. [DOI] [PubMed] [Google Scholar]
- Witzenbichler B, Maisonpierre PC, Jones P, Yancopoulos GD, Isner JM. Chemotactic Properties of angiopoietin-1 and -2, ligands for the endothelial-specific receptor tyrosine kinase Tie2. J Biol Chem. 1998;273(29):18514–18521. doi: 10.1074/jbc.273.29.18514. [DOI] [PubMed] [Google Scholar]
- Park JH, Park KJ, Kim YS, Sheen SS, Lee KS, Lee HN. Serum angiopoietin-2 as a clinical marker for lung cancer. Chest. 2007;132(1):200–206. doi: 10.1378/chest.06-2915. [DOI] [PubMed] [Google Scholar]
- Yalcin M, Dyskin E, Lansing L, Bharali DJ, Mousa SS, Bridoux A. Tetraiodothyroacetic acid (Tetrac) and nanoparticulate Tetrac arrest growth of medullary carcinoma of the thyroid. J Clin Endocrinol Metab. 2010;95(4):1972–1980. doi: 10.1210/jc.2009-1926. [DOI] [PubMed] [Google Scholar]
- Wray CJ, Rilo HL, Ahmad SA. Colon cancer angiogenesis and antiangiogenic therapy. Expert Op Invest Drugs. 2004;13(6):631–641. doi: 10.1517/13543784.13.6.631. [DOI] [PubMed] [Google Scholar]
- Hsueh C, Lin J-D, Wu I-C, Chao T-C, Yu J-S, Liou M-J. Vascular endothelial growth factors and angiopoietins in presentations and prognosis of papillary thyroid carcinoma. J Surg Oncol. 2011;103(5):395–399. doi: 10.1002/jso.21844. [DOI] [PubMed] [Google Scholar]