Abstract
Objectives
There is conflicting evidence on the efficacy of Traditional Chinese Acupuncture (TCA), and the role of placebo effects elicited by acupuncturists’ behavior has not been elucidated. We conducted a 3-month randomized clinical trial in patients with knee osteoarthritis to compare the efficacy of TCA to sham acupuncture, and examine the effects of acupuncturists’ communication style.
Methods
Acupuncturists were trained to interact in one of two communication styles: ‘high’ or ‘neutral’ expectations. Patients were randomized to one of 3 groups: waiting list, ‘high’ or ‘neutral’, and nested within style, TCA or sham acupuncture over 6 weeks. Sham acupuncture was performed in non-meridian points, with shallow needles and minimal stimulation. Primary outcome measures were: Joint-specific Multidimensional Assessment of Pain (J-MAP), Western Ontario McMaster Osteoarthritis Index (WOMAC), and satisfaction.
Results
455 patients who received treatment (TCA or sham) and 72 controls were included. No statistically significant differences were observed between TCA or sham acupuncture, but both groups had significant reductions in J-MAP and WOMAC pain compared to the waiting group (-1.1, -1.0, and -0.1, p<0.001; -13.7, -14, -1.7, p<0.001). Statistically significant differences were observed in J-MAP pain reduction and satisfaction, favoring the ‘high’ expectations group. Fifty-two percent and 43% in the TCA and sham groups thought they had received TCA (kappa=0.05), suggesting successful blinding.
Conclusion
TCA was not superior to sham acupuncture. However, acupuncturists’ style had significant effects on pain reduction and satisfaction, suggesting that the analgesic benefits of acupuncture can be partially mediated through placebo effects related to the acupuncturist's behavior.
Acupuncture is a mainstay in Traditional Chinese Medicine. Health is attained through the flow of vital energy Qi through specific body paths called meridians; disease is caused by obstructions to this flow (1). In traditional Chinese acupuncture (TCA), needles are inserted at points along meridians to unblock these obstructions. In the past, acupuncture was mostly administered using manual needle manipulation. Increasingly, most acupuncturists, including those providing TCA, use electroacupuncture to increase stimulation.
There is conflicting evidence regarding the efficacy of acupuncture in knee osteoarthritis (OA)(2-5). Moreover, no study has systematically assessed the potential bias from the interactions of participants with acupuncturists. Only two randomized clinical trials (RCTs) in a recent systematic review described any attempts to limit the interactions between acupuncturists and participants (3, 6, 7). Neither achieved successful blinding. Placebo effects can be enhanced by expectations of improvement and it is conceivable that patient-provider interactions result in increased benefits if the provider has a confident attitude (8, 9).
To further evaluate the contribution of provider communication style to therapeutic responses we conducted a RCT of acupuncture for OA of the knee with a nested factorial design allowing us to evaluate the comparative effects of TCA and sham acupuncture while controlling for the effect of the acupuncturists’ communication styles.
PATIENTS AND METHODS
Design
We conducted a nested two-stage RCT to determine the effects of practitioner behavior on patients’ response to TCA or sham acupuncture in OA of the knee, and to evaluate the difference in therapeutic efficacy between these two modalities. Six acupuncturists trained in traditional Chinese medicine, licensed by the Texas State Board of Medical Examiners, were recruited through the American College of Acupuncture & Oriental Medicine (ACAOM). To ensure uniformity, all were Chinese, male, and had at least two years of clinical experience.
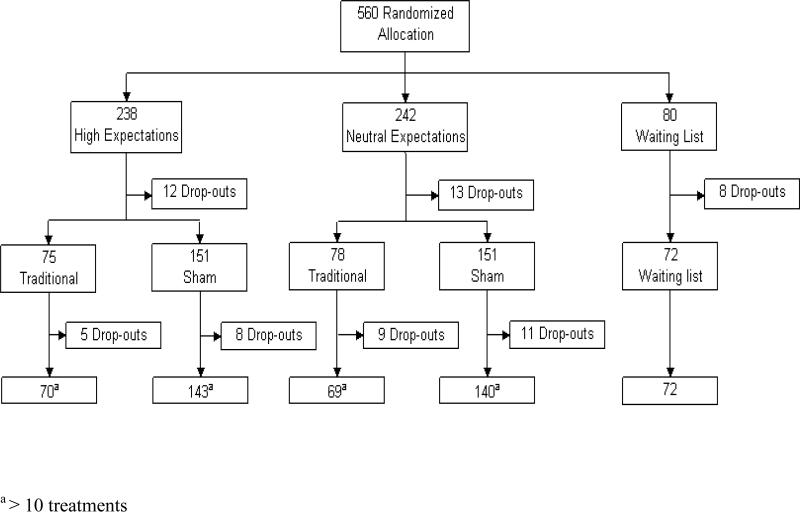
After completing a baseline assessment, patients were randomized to one of three groups, waiting list, high expectations or neutral expectations style, and were given an appointment with an acupuncturist trained in the assigned communication style (see below) (Figure 1). During the initial 30’ visit the acupuncturist examined the subject in the traditional Chinese medicine fashion (e.g. documenting pulse), giving information and answering questions with the corresponding communication style. Participants were then randomized again to receive TCA or sham acupuncture. The study was approved by our Institutional Review Board. Participants were told that the study compared traditional vs. non-traditional acupuncture. The words ‘sham’ or ‘placebo’ were not used in the information materials or consent forms.
Figure 1. Study Design.
For the first half of the trial half of the acupuncturists were randomly allocated to the high expectations communication style and the other half to the neutral style. In the second half the acupuncturists switched communication styles.
Randomization
Randomization was computer-generated with unequal blocks, stratified initially according to communication style. Patients allocated to either style were then randomized to one of the acupuncturists trained to interact in that style (acupuncturist nested within style). Finally, for each acupuncturist, patients were randomized to receive either TCA or sham acupuncture (treatment nested within acupuncturist). Opaque, sealed envelopes kept at a central location were used for allocation. Our hypothesis was that TCA would be more effective than sham acupuncture, so to better evaluate the effects of communication style on placebo effects we oversampled the sham arm, to allow us to conduct subgroup analyses in this group if results between both arms (TCA and sham) were found to be different.
Participants
Five hundred and sixty subjects, 50 years old or greater, with knee OA according to the American College of Rheumatology criteria (10) participated in the trial. All patients had a radiological diagnosis of OA. Additional inclusion criteria were: (i) pain in the knee in the preceding two weeks ≥3/10; (ii) no prior treatment with acupuncture; (iii) stable treatment with nonsteroidal anti-inflammatory (NSAIDS) and analgesics in previous month; (iv) if receiving glucosamine, stable dosage for the past 2 months; (v) no intraarticular injections in the knee in the previous 2 months.
Communication style intervention
Because the individual communication patterns of each acupuncturist could be different in the first half of the study, the acupuncturists were randomized, three to interact with a high expectations style and the other three in a more uncertain, neutral fashion. In the second half of the study, the high expectations acupuncturists were retrained to act neutrally and viceversa. One acupuncturist had to leave the study towards the end of the first half of the trial, so in order to maintain a balanced design, only 4 acupuncturists participated in the second half.
High expectations. Acupuncturists conveyed high expectations of improvement, using positive utterances such as “I think this will work for you,” “I've had a lot of success with treating knee pain,” “Most of my patients get better.” A high expectations brochure was developed and given to patients. The research coordinator assisting with these patients was also trained to interact with a high expectations style.
Neutral expectations. Acupuncturists conveyed uncertainty with utterances such as “It may or may not work for you,” “It really depends on the patient,” We're uncertain, and that's why we are doing the study.” and words like “uncertain”. A neutral expectations brochure was given to patients. The research coordinator for this group was trained to interact with a neutral style.
Training materials were developed for each style. Before the trial started, acupuncturists participated in two 2-day training sessions including didactic instruction, one-on-one coaching, and group role play to practice the assigned style, with video-recording to provide feedback. After completion of the first half of the trial acupuncturists were retrained.
Acupuncture intervention
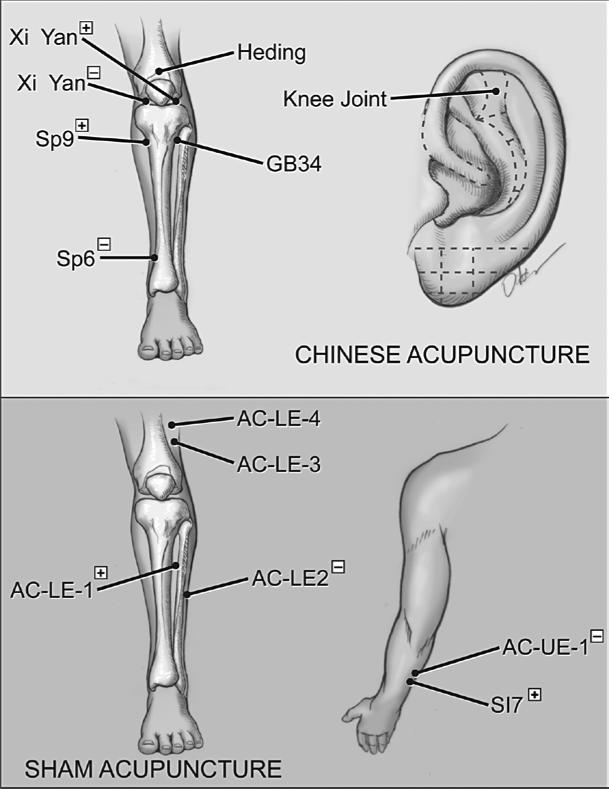
We chose electroacupuncture as the modality of choice because it is the most commonly used method nowadays. We used transcutaneous electrical nerve stimulation (TENS) equipment. In clinical settings, TCA is often performed by choosing points for each patient. To standardize our methods, a panel consisting of the acupuncturists determined the procedure and specific points to be used equally for all patients in each of the two arms: TCA points on the basis of clinical practice, and sham points outside relevant meridians (Figure 2). Before the trial started we tested both the TCA and sham protocols in 9 volunteers; 7 received both treatments, but only one correctly distinguished between the two.
Figure 2. Acupuncture points.
TCA. The following points were selected: Xi Yan, He Ding, GB 34, SP 6, SP 9, Ear-Knee, 1-2 tender Ashi points proximal to the knee. Filiform needles, 34 gauge, 1 or 1.5 cun, were used except for Ear- Knee in which 36 gauge, 0.5 cun, needles were used. The depth of insertion was 0.2-1.2 cun depending on tolerance. TENS was applied to outer Xi Yan (positive) and inner Xi Yan (negative), and SP 9 (positive) and SP 6 (negative).
Sham acupuncture. Needles were inserted at sham points not relevant to the knee, located in between meridians: AC-LE-1, 1.0 cun below and 0.5 cun lateral to ST 36; AC-LE-2,1.0 cun lateral and 1.0 cun above ST 40; AC-LE-3, above the superior-lateral border of the patella, 1.0 cun lateral to the stomach meridian; AC-LE-4, 4.0 cun above the superior-lateral border of the patella, 1.0 cun lateral to the stomach meridian. An arm point, SI 7 was used along with AC-UE-1, located in the middle of SI 5 and SI 8 points. The needles used in the sham procedure were thinner, shorter, and less deeply inserted than in TCA: 36 gauge, 1.0 cun needles 0.2-0.5 cun deep. The TENS unit was connected to SI 7 (positive) and AC-UE-1 (negative), and AC-LE-1 (positive) and AC-LE-2 (negative).
Labeled boxes with disposable Millennia needles were created for each arm. The depth of needles was shallower for sham acupuncture. For TCA, TENS was set to emit a dense disperse (DD) wave impulse at 50Hz, dispersing at 15Hz, 20 cycles/minute. Voltage was increased slowly from 5V to 60V until maximal tolerance was achieved. Patients rested for 20’ with continuing TENS. For sham, instead of DD, a 40Hz adjustable (ADJ) wave was used. Voltage was increased until the patient could feel it and then immediately turned off. Patients rested for 20’ with the needles retained, but without TENS stimulation.
All procedures, needling techniques and communication styles, were thoroughly outlined in the training manual and reviewed at training sessions. During the trial research assistants were instructed to enter the room randomly while patients were being treated to ensure that the needles were placed correctly with respect to the meridians. While they did not enter the treatment rooms on all occasions, acupuncturists were aware that the assistants would periodically check for accuracy in needle placement. The initial interaction between participants and acupuncturists took place before the participant was randomly allocated to TCA or sham; therefore the acupuncturist was unaware of what type of treatment the participant would receive. All visits were audiorecorded and feedback on performance was given at follow-up sessions. Audiorecordings at the baseline, mid-point and final sessions were rated on strength of expectations communication on a 0-10 cm visual analogue scale (VAS) by graduate students in the Department of Communication Sciences at Texas A&M University, unaware of treatment allocation. Acupuncturists did not know which sessions were rated.
Outcome measures
Outcome measures were collected at baseline, 4 weeks, 6 weeks (end of treatment) and 3 months. The primary outcomes determined a priori were:
Joint-Specific Multidimensional Assessment of Pain (J-MAP) measuring the intensity, frequency and quality of pain (11); Responses range from 1 to 7 with higher values indicating more pain (Cronbach's α=0.93). Respondents rated each knee separately. The score was the average of both knees if the pain was bilateral and they had received treatment in both knees. For unilateral symptoms, only the J-MAP for the relevant knee was used.
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale (12), scaled from 0 to 100, with higher values indicating more pain.
Satisfaction with Knee Procedure (SKIP), a 6-item satisfaction scale with the following agree/disagree statements: I would recommend acupuncture to my family if they needed care for the same problem; I feel acupuncture is worthwhile for my knee arthritis; All things considered, my perceptions of acupuncture are generally negative; I feel I was helped by the acupuncture; I am dissatisfied with the functioning of my knees after acupuncture; and Undergoing acupuncture was a waste of time. Scores range from 1 to 5 with higher scores indicating greater satisfaction. Cronbach's α for our sample was 0.91.
Secondary outcomes included: WOMAC function (12); 12-Item Short-Form Health Survey (SF12), physical and mental component summary scores (PCS and MCS) (13); 10cm VAS for pain; range of motion (ROM); Timed Up and Go Test (TUG)(14). We also estimated the proportion of patients who achieved at least 20%, 50% and 70% improvement in WOMAC scores which has been shown to be clinically relevant (15).
Questionnaires were self-administered; ROM and TUG were measured by a blinded research assistant.
We took several steps to minimize bias: (i) We did not use the words ‘sham’ or ‘placebo’ and stated our objective as a comparison between traditional and non-traditional acupuncture; (ii) Participants could not have received acupuncture previously; (iii) Clinic procedures were implemented to avoid minimal contact and interaction between participants; individuals with close relationships to participants were excluded; (iv) The research assistant conducting the follow-up assessments was blinded; (v) Although the statisticians could not be blinded because of unequal sample sizes, the other investigators were blinded to the allocation groups until the analysis was complete; (vi) At 3 months patients were asked whether they thought they had received TCA or non-traditional acupuncture;
Statistical analysis
Repeated measures ANOVA was used to assess changes over time for treatment and style. Individual growth curve analysis was used to examine change over time for each individual (16). A linear model was used, with intercept and time as random effects, treatment and style modeled as fixed effects, and interaction terms for time with treatment, time with style, and style with treatment.
The analysis was conducted as intent-to treat carrying the last observation forward for dropouts. Our power calculations were based on an unbalanced design (1:2:4): 80 waiting list, 160 TCA and 320 sham. This sample size yielded a power in excess of 0.99 (α=0.01) for ANOVA of the pain scales. All analyses were performed using SAS v.9.1.3.
RESULTS
Five-hundred-and-sixty patients were randomized: 238 to the high expectations group, 242 patients to the neutral expectations group, and 80 to the waiting list group. Numbers were slightly unbalanced because one of the acupuncturists left before the end of the first arm. Twenty-five patients withdrew before treatment; 8 patients in the waiting list did not return for reassessment. The analyses included 527 patients: 455 who received TCA or sham and 72 controls. Thirty-three patients did not complete at least 10 acupuncture treatments. No differences were observed in dropout rates between TCA and sham groups (9.2% vs. 6.3%, p>0.20) or high vs. neutral communication groups (5.7% vs. 8.7%, p>0.20). Most patients (72%) received acupuncture in both knees.
Baseline characteristics are shown in Table 1. P-values are shown for differences in proportions (X2 test) or differences in means (F-test) among all groups. No statistically significant differences were observed.
Table 1.
Baseline demographic and clinical characteristics
| High Expectations | Neutral Expectations | |||||
|---|---|---|---|---|---|---|
| TCA N=75 | Sham N=151 | TCA N=78 | Sham N=151 | Waiting List N=72 | p+ | |
| GENDER, females –n (%) | 51 (68.0%) | 97 (64.2%) | 50 (64.1%) | 98 (64.9%) | 42 (58.3%) | > 0.20 |
| AGE | 63.5 (10.4) | 65.3 (9.0) | 65.5 (7.8) | 63.7 (9.1) | 64.1 (9.6) | > 0.20 |
| ETHNICITY – n (%) Whites | 52 (69.3%) | 103 (68.2%) | 55 (70.5%) | 101 (66.9%) | 47 (65.3%) | > 0.20 |
| African American | 16 (21.3%) | 23 (15.2%) | 13 (16.7%) | 31 (20.5%) | 15 (20.8%) | |
| Hispanic | 4 (5.3%) | 14 (9.3%) | 8 (10.3%) | 14 (9.3%) | 5 (6.9%) | |
| Other | 3 (4.0%) | 11 (7.3%) | 2 (2.6%) | 5 (3.3%) | 5 (6.9%) | |
| EDUCATIONAL LEVEL – n (%) | ||||||
| Less than high school | 2 (2.7%) | 5 (3.3%) | 3 (3.8%) | 3 (2.0%) | 2 (2.8%) | > 0.20 |
| High School diploma/some college | 34 (45.3%) | 79 (52.3%) | 35 (44.9%) | 72 (48.0%) | 35 (48.6%) | |
| College degree | 39 (52.0%) | 67 (44.4%) | 40 (51.3%) | 75 (50%) | 35 (48.6%) | |
| DURATION OF KNEE PAIN, years | 10.0 (11.7) | 8.4(9.6) | 8.4(7.9) | 8.8 (10.4) | 11.5 (12.4) | 0.14 |
| J-MAP | 4.4 (1.2) | 4.3 (1.3) | 4.5 (1.3) | 4.6 (1.2) | 4.3 (1.2) | 0.12 |
| WOMAC Pain | 43.3 (18.2) | 44.8 (18.7) | 45.6 (18.6) | 45.2 (17.8) | 44.1 (15.2) | > 0.20 |
| WOMAC Function | 41.5 (19.3) | 45.1 (18.5) | 44.2 (18.8) | 44.1 (17.6) | 40.1 (16.5) | > 0.20 |
| VAS Pain | 57.3 (21.0) | 57.1 (24.0) | 59.3 (23.6) | 57.6 (23.0) | 54.6 (21.3) | > 0.20 |
| SF12 PCS | 35.4 (9.7) | 33.6 (8.1) | 34.6 (10.0) | 33.4 (9.3) | 35.3 (8.4) | > 0.20 |
| SF12 MCS | 51.7 (10.1) | 53.6 (9.3) | 52.8 (8.8) | 53.2 (9.3) | 53.7 (10.7) | > 0.20 |
| TUG, seconds | 14.3 (9.0) | 13.6 (4.8) | 13.6 (5.3) | 13.2 (6.1) | 12.3 (3.3) | 0.17 |
| ROM, degrees of flexion | 104.1 (14.5) | 105.3 (12.4) | 107.3 (12.9) | 106.0 (13.7) | 105.7 (13.0) | > 0.20 |
| MEDICATIONS: NSAIDs | 41 (54.7%) | 79 (52.3%) | 44 (56.4%) | 69 (45.7%) | 34 (37.2%) | > 0.20 |
| Analgesics | 29 (38.7%) | 50 (33.1%) | 35 (43.6%) | 54 (35.8%) | 21 (29.2%) | > 0.20 |
| Glucosamine | 20 (26.7%) | 33 (21.8%) | 22 (28.2%) | 51 (33.4%) | 18 (25.0%) | 0.12 |
Continuous variables shown as mean (SD). WOMAC: Western Ontario Western Ontario and McMaster Universities Osteoarthritis Index; J-MAP: Joint-Specific Multidimensional Assessment of Pain SF12 PCS: Physical Component Summary; SF12 MCS: Mental Component Summary; VAS: Visual Analogue Scale; TUG: Timed Get Up and Go; ROM: Range of Motion; NSAIDS: Nonsteroidal Anti-inflammatory Drugs. X2 p-value for difference in proportion between style groups or F-test p-value for difference in means between style groups (high/neutral/waiting list) as appropriate
No differences were observed between the TCA and sham groups (Table 2). Patients receiving either form of therapy showed improvement for most outcome measures compared to the waiting list group.
Table 2.
Outcome measures by acupuncture treatment group
| Baseline | 4 weeks | 6 weeks | 3 months | Baseline | 3 months | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TCA | Sham | TCA | Sham | TCA | Sham | TCA | Sham | p+ | Waiting list | p++ | ||
| J-MAP | 4.4 (1.3) | 4.4 (1.3) | 3.3 (1.3) | 3.4 (1.3) | 3.1 (1.3) | 3.3 (1.4) | 3.3 (1.4) | 3.4 (1.5) | >0.20 | 4.3 (1.2) | 4.2 (1.3) | 0.0003* |
| WOMAC Pain | 44.5 (18.4) | 45.0 (18.2) | 31.8 (17.5) | 32.6 (17.2) | 28.1 (18.4) | 28.9 (18.6) | 30.8 (17.9) | 31.0 (19.1) | >0.20 | 44.1 (15.2) | 42.4 (16.8) | 0.0002* |
| WOMAC Function | 42.9 (19.0) | 44.6 (18.1) | 32.3 (17.7) | 34.1 (17.1) | 29.5 (17.8) | 31.4 (18.5) | 31.2 (17.9) | 32.1 (18.3) | >0.20 | 40.1 (16.5) | 41.7 (18.0) | 0.0003* |
| SKIP | n/a | n/a | 4.15 (0.68) | 4.10 (0.68) | 4.13 (0.80) | 4.04 (0.79) | 4.00 (0.85) | 3.95 (0.78) | >0.20 | n/a | n/a | n/a |
| VAS Pain | 58.3 (22.3) | 57.4 (23.5) | 34.8 (25.9) | 38.2 (25.4) | 29.0 (26.3) | 32.5 (27.8) | 36.2 (28.5) | 36.7 (29.0) | >0.20 | 54.6 (21.3) | 53.2 (24.3) | 0.0001* |
| SF12 PCS | 35.0 (9.9) | 33.5 (8.7) | 38.5 (10.0) | 37.7 (9.1) | 40.5 (10.0) | 39.0 (9.9) | 39.5 (9.7) | 38.7 (10.1) | >0.20 | 35.3 (8.4) | 35.8 (8.9) | 0.11 |
| SF12 MCS | 52.3 (9.4) | 53.4 (9.3) | 53.9 (8.3) | 54.2 (8.9) | 53.4 (7.9) | 54.0 (8.7) | 54.1 (8.2) | 53.2 (8.9) | >0.20 | 53.7 (10.7) | 51.6 (9.8) | 0.11 |
| TUG, seconds | 13.9 (7.3) | 13.4 (5.5) | n/a | n/a | 12.2 (4.3) | 12.2 (5.0) | 11.9 (4.1) | 12.1 (5.4) | >0.20 | 12.3 (3.3) | 12.2 (3.5) | >0.20 |
| ROM, degrees | 105.7 (13.7) | 105.7 (13.1) | n/a | n/a | 106.1 (12.8) | 106.7 (13.1) | 106.2 (12.1) | 106.5 (12.6) | >0.20 | 105.7 (13.0) | 104.9 (13.7) | > 0.20 |
J-MAP: Joint-Specific Multidimensional Assessment of Pain; WOMAC: Western Ontario Western Ontario and McMaster Universities Osteoarthritis Index; SKIP: Satisfaction with Knee Procedure; SF12 PCS: Physical Component Summary; SF12 MCS: Mental Component Summary; VAS: Visual Analogue Scale; TUG: Timed Get Up and Go; ROM: Range of Motion
Improvement is seen as positive differences for SKIP; SF12 PCS, MCS, and ROM, and negative differences for J-MAP, WOMAC and TUG
P values for repeated measures models testing for difference in means across time excluding waiting list group
P values including waiting list group
statistically significant (p<= 0.05).
Cells in table represent mean (standard deviation)
n/a : not administered
Patient-provider interactions were audiotaped and rated blindly. Mean ratings for acupuncturists in the high expectations group were higher than those in the neutral group (p<0.0001). Patients in the high expectations communication style had statistically significant improvements in pain (J-MAP and VAS), and satisfaction (SKIP) compared to the neutral group, with effect sizes of respectively 0.25 and 0.22 at 3 months (Table 3). Patients receiving either communication style showed statistically significant improvement for most outcome measures compared to the waiting list group. No significant two-way interactions between treatment and style were found in the models. The effect of treatment and style on patients over time was examined using individual growth curve analysis. The time parameter was statistically significant for all measures, indicating that patients improved over the course of the study, equally for both treatments (TCA and sham). For J-MAP and SKIP, communication style was statistically significant (p=0.02, and p=0.01) favoring the high expectations group. For treatment (TCA vs. sham) none of the outcomes showed a significant effect. No interactions were observed between time and style, or time and treatment.
Table 3.
Outcome measures by communication style group
| Baseline | 4 weeks | 6 weeks | 3 months | Baseline | 3 months | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High | Neutral | High | Neutral | High | Neutral | High | Neutral | p | Waiting list | p++ | ||
| J-MAP | 4.3 (1.3) | 4.5 (1.2) | 3.2 (1.2) | 3.5 (1.4) | 3.0 (1.3) | 3.4 (1.4) | 3.2 (1.4) | 3.6 (1.5) | 0.006* | 4.3 (1.2) | 4.2 (1.3) | < 0.0001* |
| WOMAC Pain | 44.3 (18.5) | 45.3 (18.0) | 31.5 (16.9) | 33.1 (17.7) | 27.3 (18.1) | 30.0 (18.9) | 29.9 (19.1) | 31.9 (18.3) | >0.20 | 44.1 (15.2) | 42.4 (16.8) | 0.0001* |
| WOMAC Function | 43.9 (18.8) | 44.2 (18.0) | 33.0 (17.3) | 34.0 (17.3) | 30.0 (18.2) | 31.5 (18.4) | 31.3 (18.3) | 32.3 (18.0) | >0.20 | 40.1 (16.5) | 41.7 (18.0) | 0.0003* |
| SKIP | n/a | n/a | 4.22 (0.65) | 4.01 (0.69) | 4.13 (0.78) | 4.01 (0.79) | 4.06 (0.78) | 3.88 (0.82) | 0.004* | n/a | n/a | n/a |
| VAS Pain | 57.2 (23.0) | 58.2 (23.2) | 34.4 (24.3) | 39.6 (26.5) | 29.1 (26.4) | 33.5 (28.2) | 34.9 (28.3) | 38.1 (29.3) | 0.06 | 54.6 (21.3) | 53.2 (24.3) | < 0.0001* |
| SF12 PCS | 34.2 (8.7) | 33.8 (9.5) | 38.2 (8.5) | 37.7 (10.3) | 40.2 (9.5) | 38.9 (10.3) | 39.6 (9.2) | 38.4 (10.6) | >0.20 | 35.3 (8.4) | 35.8 (8.9) | 0.10 |
| SF12 MCS | 53.0 (9.6) | 53.1 (9.1) | 53.9 (8.6) | 54.4 (8.8) | 53.7 (8.1) | 54.0 (8.8) | 53.0 (8.6) | 54.0 (8.8) | >0.20 | 53.7 (10.7) | 51.6 (9.8) | 0.07 |
| TUG, seconds | 13.8 (6.5) | 13.3 (5.8) | n/a | n/a | 12.3 (4.2) | 12.0 (5.3) | 12.2 (4.3) | 11.9 (5.6) | >0.20 | 12.3 (3.3) | 12.2 (3.5) | > 0.20 |
| ROM, degrees | 104.9 (13.1) | 106.5 (13.5) | n/a | n/a | 105.6 (13.5) | 107.5 (12.4) | 105.8 (12.6) | 107.0 (12.2) | 0.18 | 105.7 (13.0) | 104.9 (13.7) | > 0.20 |
J-MAP: Joint-Specific Multidimensional Assessment of Pain; WOMAC: Western Ontario Western Ontario and McMaster Universities Osteoarthritis Index; SKIP: Satisfaction with Knee Procedure; SF12 PCS: Physical Component Summary; SF12 MCS: Mental Component Summary; VAS: Visual Analogue Scale; TUG: Timed Get Up and Go; ROM: Range of Motion
Improvement is seen as positive differences for SKIP; SF12 PCS, MCS, and ROM, and negative differences for J-MAP, WOMAC and TUG
+ P values for repeated measures models testing for difference in means across time excluding waiting list group
P values including waiting list group
statistically significant (p<= 0.05).
Cells in table represent mean (standard deviation). n/a: not administered
We also examined differences in treatment and style by categorizing the WOMAC pain and function scales according to 20%, 50% and 70% improvement. No statistically significant differences or trends were observed for treatment. For style, trends were observed favoring the high expectations group for 50% WOMAC improvement. For pain at 6 weeks 41.2% in the high expectations group achieved 50% improvement compared to 33.6% in the neutral group (p=0.10); at 3 months, 50% improvement was reported by 35.4% patients in the high expectations group, and 27.5% in the neutral group (p=0.07). For WOMAC function, a trend was observed at 4 weeks, with 24.3% and 17.0% respectively in the high and neutral style groups reporting 50% improvement (p=0.05).
At the end of the study we asked participants which treatment they thought they had received with three possible responses: TCA, non-traditional acupuncture, or not sure. No significant differences were observed: 52% in the TCA group and 43% in the sham thought they had received TCA (weighted kappa=0.05, p=0.23), showing successful blinding.
Few adverse events were observed: 26 patients (7.2% TCA vs. 4.9% sham) had exacerbation of knee pain; 22 (5.8% TCA vs. 4.6% sham) had bruising at needle site; 3 (<1% each TCA and sham) reported muscle cramps, 1 (TCA) headache, and 1 (TCA) infection at needle site.
DISCUSSION
This is the first study designed to compare the efficacy of TCA with sham acupuncture in OA of the knee while experimentally controlling and measuring the effects of provider-patient interactions in the response to acupuncture. There were two major findings. First, acupuncture as practiced traditionally, following the Chinese method of meridian needle insertion was not superior to the sham procedure. Second, the communication intervention had a small but significant effect on pain and satisfaction with treatment, demonstrating a placebo effect related to the clinicians’ communication style. Effect sizes were small, 0.25 and 0.22 respectively.
There is considerable interest in the use of acupuncture as a relatively safe intervention for the management of knee OA. Unfortunately, the quality of many trials has been poor (17-19). In many instances, sham procedures have not been adequate to mask the ‘true’ intervention (18). Specifically, the use of retractable non-penetrating needles may not adequately blind subjects (6, 20). Two recent systematic reviews have examined the efficacy of acupuncture in this condition (3, 4). White et al (4) identified 13 trials, of which 5 were considered to be of enough quality to be included in a meta-analysis (6, 7, 21-23). Although a statistically significant effect was observed favoring acupuncture over sham, these findings were mostly due to the results of two trials (6, 21), which used sham procedures with retractable needles. In one trial blinding was not successfully achieved (6), and in the other, it was not reported (21). Another 2007 meta-analysis (3) concluded that the effects of acupuncture for knee OA were clinically irrelevant when compared to sham therapy, but found statistically and clinically significant benefits when compared to usual care or waiting list controls, as we observed in our study. Similarly, in this review, trials that used non-penetrating needling procedures showed clinically small but statistically significant beneficial effects (6, 21, 24). The studies using superficial but penetrating needling at non-acupuncture points as sham showed no benefit or modest efficacy for traditional acupuncture (7, 25). Our study used a sham procedure with superficial needling in non-meridian points and minimal electric stimulation. While the procedure was minimally invasive, it was sufficient to allow successful blinding, as compared to some recent studies where blinding was unsuccessful. Our sham procedure may have had an analgesic effect from superficial needling such as release of endorphins, yet, this effect is also observed with oral pain placebo. Meridian point insertion following TCA practices did not have an additional effect. Furthermore, using continuous electrical stimulation in the TCA group (compared to a few seconds in the sham group) was also ineffective. Whereas the improvement observed in both TCA and sham groups is due to needling (deep or superficial) or to the placebo effects of participating in a study with frequent contact with research staff, cannot be easily established. A recent large trial of acupuncture for low back pain reported no differences between individualized acupuncture tailoring needling sites, a standardized approach using specific points, and simulated non-penetrating acupuncture (26). In a systematic review of three-armed trials of acupuncture for pain, a small difference was observed between traditional and placebo acupuncture, and a moderate difference between placebo acupuncture and no acupuncture (27). The authors questioned the importance of meridians and specific acupuncture points emphasized by TCA, and concluded that the analgesic effect of acupuncture is small and may result from incomplete blinding. Moreover, an acupuncturist may unintentionally convey different signals to the patient depending on whether TCA or sham acupuncture is administered. In addition to their training in behavioral styles, in our trial, the interactions of acupuncturists with patients were audiotaped to ensure adherence to protocol.
In our study, patients in the high expectations group showed a clinically small, but statistically significant improvement in knee pain and satisfaction (J-MAP, VAS and SKIP), compared with those in the neutral group. No significant differences were observed in WOMAC scores when using interval change as an outcome (12); however, we found borderline trends favoring the high expectations group when the WOMAC pain and function scores were dichotomized to identify those patients with at least 50% improvement, an approach previously recommended (15). A difference between the J-MAP and the WOMAC is that the first one asks about pain intensity and frequency in general (e.g. how intense was your knee pain), while the WOMAC elicits pain with specific activities (e.g. pain going up or down the stairs). We also evaluated each knee separately with the J-MAP, while the WOMAC assessed both knees simultaneously.
Expectancies play a role in patients’ perception of outcome and placebo responses are enhanced in patients with high expectations for improvement (28-31). These expectations can be modeled according to the behavior and communication style of the provider interacting with the patient. A recent study evaluated the role of provider communication style in patients treated for irritable bowel syndrome with sham acupuncture in a single blind trial (9). Patients were assigned to 3 groups: waiting list, placebo acupuncture with ‘limited’ communication (<5’ with the provider), and placebo-acupuncture with ‘augmented’ interaction (45’ visit with provider communicating in a warm, empathic manner). A statistically significant incremental response was observed, with patients in the ‘augmented’ group experiencing the most improvement.
The effects of TCA and sham needling appear to be mediated by similar neurochemical and neurophysiologic pathways (32-35). Release of endorphins and other neuropeptides has been documented both with placebo responses and acupuncture treatment, with or without electrical stimulation. Functional magnetic resonance imaging (fMRI) studies have shown broad activation and deactivation in central nervous (30, 33, 36). Kong et al used non-penetrating needles as a sham procedure to evaluate fMRI changes in response to expectations about acupuncture in 16 subjects receiving thermal stimulation (36). Investigators manipulated the subjects’ expectancy about acupuncture by explaining how pain relief might be achieved. Participants had higher pain relief and more prominent fMRI activation when their expectancies of relief were enhanced. These findings, in conjunction with other evidence, support the important neurophysiological changes that can modulate pain relief centrally through placebo effects based enhanced by expectancies.
Our study had some limitations. Firstly, we cannot make inferences with respect to the use of less invasive placebo, such as non-penetrating needles, which could have resulted in different results. Secondly, while we audiorecorded the verbal interactions between patients and acupuncturists, non-verbal communication may also be important in the setting of acupuncture and placebo responses, and we were unable to measure this. Finally, although we made efforts to blind the study in as much as was possible with the established procedures, some patients may have been aware of what treatment they were receiving (TCA or sham); yet, no differential responses were observed among groups, when patients were specifically asked what therapy they thought they had received.
This is the first study examining TCA and sham acupuncture in knee OA that also included experimental manipulation of the acupuncturists’ communication style. In summary, TCA was not superior to sham acupuncture, and needling of meridian points was not more effective than use of sham points. Continuous electrical stimulus or increased needle penetration in the TCA group did not improve response. Acupuncturists’ communication style had a small but statistically significant effect in pain reduction and satisfaction suggesting that the perceived benefits of acupuncture may be partially mediated through placebo effects related to the acupuncturists’ behavior.
Acknowledgements
Supported by the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS R01 AR49999). Dr. Suarez-Almazor holds a K24 career award from NIAMS, and is the Director of the Houston Center for Education and Research on Therapeutics supported by the Agency for Health Research and Quality (U18HS016093). This trial was registered at clinicaltrials.gov (NCT00059345). We are grateful to the members of the research team who contributed to this work. They are Stacey Havelka, BA, Sonya Patel, MSOM, Andrea Price, BS, and Elizabeth Simmons, RN. We are also grateful to Michael Kallen, PhD for his contributions to the analysis of this work.
References
- 1.Ernst E, White A. Acupuncture: A Scientific Appraisal. 1st ed Butterworth-Heinemann; 1999. [Google Scholar]
- 2.Kwon YD, Pittler MH, Ernst E. Acupuncture for peripheral joint osteoarthritis: a systematic review and meta-analysis. Rheumatology (Oxford) 2006;45(11):1331–7. doi: 10.1093/rheumatology/kel207. [DOI] [PubMed] [Google Scholar]
- 3.Manheimer E, Linde K, Lao L, Bouter LM, Berman BM. Meta-analysis: acupuncture for osteoarthritis of the knee. Ann Intern Med. 2007;146(12):868–77. doi: 10.7326/0003-4819-146-12-200706190-00008. [DOI] [PubMed] [Google Scholar]
- 4.White A, Foster NE, Cummings M, Barlas P. Acupuncture treatment for chronic knee pain: a systematic review. Rheumatology (Oxford) 2007;46(3):384–90. doi: 10.1093/rheumatology/kel413. [DOI] [PubMed] [Google Scholar]
- 5.Ezzo J, Hadhazy V, Birch S, Lao L, Kaplan G, Hochberg M, et al. Acupuncture for osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2001;44(4):819–25. doi: 10.1002/1529-0131(200104)44:4<819::AID-ANR138>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 6.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141(12):901–10. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 7.Scharf HP, Mansmann U, Streitberger K, Witte S, Kramer J, Maier C, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann.Intern.Med. 2006;145(1):12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 8.Street RL, Jr., Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336(7651):999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altman RD. Criteria for classification of clinical osteoarthritis. J Rheumatol Suppl. 1991;27:10–2. [PubMed] [Google Scholar]
- 11.O'Malley KJ, Suarez-Almazor M, Aniol J, Richardson P, Kuykendall DH, Moseley JB, Jr., et al. Joint-specific multidimensional assessment of pain (J-MAP): factor structure, reliability, validity, and responsiveness in patients with knee osteoarthritis. J Rheumatol. 2003;30(3):534–43. [PubMed] [Google Scholar]
- 12.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 13.Ware J, Kosinski M, Turner-Bowker D, Gandek B. How to Score Version 2 of the SF-12 Health Survey Lincoln. Quality Metric Incorporated; RI: 2002. [Google Scholar]
- 14.Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken LN, Eisma WH. The Timed “up and go” test: reliability and validity in persons with unilateral lower limb amputation. Arch Phys Med Rehabil. 1999;80(7):825–8. doi: 10.1016/s0003-9993(99)90234-4. [DOI] [PubMed] [Google Scholar]
- 15.Bellamy N, Bell MJ, Goldsmith CH, Pericak D, Walker V, Raynauld JP, et al. Evaluation of WOMAC 20, 50, 70 response criteria in patients treated with hylan G-F 20 for knee osteoarthritis. Ann Rheum Dis. 2005;64(6):881–5. doi: 10.1136/ard.2004.026443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Sage; Newbury Park, CA: 2002. [Google Scholar]
- 17.Manheimer E, Ezzo J, Hadhazy V, Berman B. Published reports of acupuncture trials showed important limitations. J Clin Epidemiol. 2006;59(2):107–13. doi: 10.1016/j.jclinepi.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 18.White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complement Ther Med. 2001;9(4):237–45. doi: 10.1054/ctim.2001.0489. [DOI] [PubMed] [Google Scholar]
- 19.Vas J, White A. Evidence from RCTs on optimal acupuncture treatment for knee osteoarthritis--an exploratory review. Acupunct Med. 2007;25(1-2):29–35. doi: 10.1136/aim.25.1-2.29. [DOI] [PubMed] [Google Scholar]
- 20.White P, Lewith G, Hopwood V, Prescott P. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over pilot trial. Pain. 2003;106(3):401–9. doi: 10.1016/j.pain.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Vas J, Mendez C, Perea-Milla E, Vega E, Panadero MD, Leon JM, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ. 2004;329(7476):1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366(9480):136–43. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 23.Takeda W, Wessel J. Acupuncture for the treatment of pain of osteoarthritic knees. Arthritis Care Res. 1994;7(3):118–122. doi: 10.1002/art.1790070304. [DOI] [PubMed] [Google Scholar]
- 24.Sangdee C, Teekachunhatean S, Sananpanich K, Sugandhavesa N, Chiewchantanakit S, Pojchamarnwiputh S, et al. Electroacupuncture versus diclofenac in symptomatic treatment of osteoarthritis of the knee: a randomized controlled trial. BMC Complement Altern.Med. 2002;2:3. doi: 10.1186/1472-6882-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomized arm. Arthritis Rheum. 2006;54(11):3485–93. doi: 10.1002/art.22154. [DOI] [PubMed] [Google Scholar]
- 26.Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169(9):858–66. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madsen MV, Gotzsche PC, Hrobjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. 2009;338:a3115. doi: 10.1136/bmj.a3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128(3):264–71. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Myers SS, Phillips RS, Davis RB, Cherkin DC, Legedza A, Kaptchuk TJ, et al. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 2008;23(2):148–53. doi: 10.1007/s11606-007-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25(4):1161–7. doi: 10.1016/j.neuroimage.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Bausell RB, Lao L, Bergman S, Lee WL, Berman BM. Is acupuncture analgesia an expectancy effect? Preliminary evidence based on participants’ perceived assignments in two placebo-controlled trials. Eval Health Prof. 2005;28(1):9–26. doi: 10.1177/0163278704273081. [DOI] [PubMed] [Google Scholar]
- 32.Han JS. Acupuncture and endorphins. Neurosci Lett. 2004;361(1-3):258–61. doi: 10.1016/j.neulet.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 33.Lewith GT, White PJ, Pariente J. Investigating Acupuncture Using Brain Imaging Techniques: The Current State of Play. eCAM. 2005;2(3):315–319. doi: 10.1093/ecam/neh110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Craggs JG, Price DD, Perlstein WM, Verne GN, Robinson ME. The dynamic mechanisms of placebo induced analgesia: Evidence of sustained and transient regional involvement. Pain. 2008;139(3):660–9. doi: 10.1016/j.pain.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol. 2008;59:565–90. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]
- 36.Kong J, Gollub RL, Rosman IS, Webb JM, Vangel MG, Kirsch I, et al. Brain Activity Associated with Expectancy-Enhanced Placebo Analgesia as Measured by Functional Magnetic Resonance Imaging. J. Neurosci. 2006;26(2):381–8. doi: 10.1523/JNEUROSCI.3556-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]