Abstract
The Clinical Trials Network (CTN) represents a major initiative intended to bridge the gap between research and practice in substance abuse treatment by implementing a range of studies evaluating behavioral, pharmacologic, and combined treatments in community-based drug abuse treatment programs across the country. This article describes the development of CTN protocols evaluating the effectiveness of Motivational Enhancement Therapy and Motivational Interviewing. Design, training, and implementation challenges associated with conducting a clinical trial of brief behavioral treatments in community programs are discussed. Issues requiring attention included the diversity in treatments offered across sites, heterogeneity in the study sample, and training of clinicians drawn from the staff of community programs to deliver the study treatments.
Keywords: Substance abuse treatment, Randomized clinical trials, Behavioral therapies, Motivational interviewing
1. Introduction
A major challenge in the substance abuse treatment field is the integration of practice and research. As described in detail in a landmark report by the Institute of Medicine (Institute of Medicine, 1998), there are a number of treatments, both behavioral and pharmacologic, that have strong empirical support from clinical trials that have not been implemented in clinical practice (McLellan & McKay, 1998). To address in part the need to develop new treatments, rigorously evaluate their efficacy, and then disseminate scientifically validated treatments to the clinical community, NIDA has articulated a Stage Model of Behavioral Therapies Research (Onken, Blaine, & Battjes, 1997), encompassing three progressive stages: Stage I consists of initial development of and pilot/feasibility testing for new and untested treatments; Stage II consists principally of randomized controlled clinical trials to evaluate efficacy of treatments that have shown promise or efficacy in initial studies; and Stage III is intended to address issues of transportability of treatments whose efficacy has been demonstrated in at least two Stage II trials (Rounsaville, Carroll, & Onken, 2001).
The Clinical Trials Network (CTN) was initiated by NIDA in 1999 to bridge the gap between research and practice by building a research infrastructure of partnerships of researchers and community treatment programs (CTPs) to conduct a wide range of Stage III research evaluating behavioral, pharmacologic, and combined treatments in community settings. Chief among the challenges faced by the CTN in developing protocols is achieving appropriate balance between internal validity (e.g., designs that emphasize experimental control and ability to rule out alternate explanations of findings) and external validity (e.g., designs emphasizing generalizability of findings and the degree to which research-supported treatments can be implemented in community programs). That is, research focusing on internal validity issues places a high value on experimental control and, thus, requires design features such as random assignment to experimental and control conditions, reduced variability in treatment delivery (e.g., through the use of manuals), close monitoring of treatment delivery, and independent evaluation of outcome (e.g., use of objective measures such as urinalyses). In contrast, studies focusing on external validity issues usually tolerate less control to enhance the generalizability of findings.
This article will describe the development of one CTN protocol evaluating a behavioral treatment, motivational interviewing, and will focus on two principal issues: (1) the challenges confronted in developing and implementing the protocol and how these challenges shaped the protocol design, and (2) the clinical issues involved in training and supervision of the “real world” therapists who delivered the study treatments.
2. Rationale for evaluating MET/MI in the CTN
Early dropout, partial treatment attendance, and early relapse are common occurrences in most substance abuse treatment programs. Given that the bulk of attrition occurs very early in treatment, and retention in treatment has been linked to better outcome in several studies (Ball & Ross, 1991; McLellan et al., 1994; Simpson, Joe, & Brown, 1997), identifying effective, practical means of enhancing initial treatment engagement and outcome was seen as an important target for the CTN.
Motivational Interviewing (MI) (Miller & Rollnick, 1991) and Motivational Enhancement Therapy (MET) (Miller, Zweben, DiClemente, & Rychtarik, 1992) have a high level of empirical support as effective treatments with durable effects for several substance use disorders (Babor, 1994; Bien, Miller, & Tonigan, 1993; Project MATCH Research Group, 1997; Wilk, Jensen, & Havighurst, 1997). Although most trials evaluating these approaches have focused on alcohol- and cigarette-dependent populations, a smaller number of recent studies suggest they may be effective among drug abusing populations as well (MTP Research Group, 2001; Carroll, Libby, Sheehan, & Hyland, 2001; Martino, Carroll, O’Malley, & Rounsaville, 2000; Saunders, Wilkinson, & Philips, 1995; Swanson, Pantalon, & Cohen, 1999).
Despite the strong empirical support for MI and MET, a number of questions regarding their effectiveness in “real world” settings remain. First, although MET and MI have strong empirical support in efficacy trials involving alcohol and smoking populations, their effectiveness in community-based settings and with general populations of drug users has received less attention. Second, it is not clear whether MET and MI can be learned and implemented effectively by clinicians working in CTPs, many of whom utilize a primarily traditional, prescriptive (and sometimes confrontive) disease model approach that may not be compatible with the empathic, nonjudgmental approach associated with MI. Finally, MET and MI have been directly compared with a number of other well-defined treatments in earlier trials establishing their efficacy, but their effectiveness when integrated into standard treatment in CTPs is not known.
Given the limited study of MI and MET in community programs, a protocol evaluating these approaches was appropriate for the CTN for a number of reasons: (1) MI techniques were likely to be applicable to a broad range of clinical populations as well as feasible across a broad range of CTPs; (2) provision of training in MI was thought to be attractive to many clinicians at the CTPs; (3) CTPs could benefit from a training and supervision model designed to be sustainable over time; (4) focus on brief treatments and initial treatment engagement would facilitate comparatively rapid completion of the protocols, offering the advantage of rapid dissemination of findings to the academic and clinical communities; and (5) lack of motivation to change was frequently identified as a key factor associated with poor treatment response and, thus, an approach targeting motivation was identified as highly relevant to the work of community treatment providers. Moreover, as one of the first CTN protocols, a trial evaluating MET or MI was particularly attractive as it would allow evaluation of clinician training strategies and could also generate important data on the nature of “standard treatment” as delivered in the participating programs, thus setting the stage for future CTN protocols that will use “standard treatment” as a comparison condition.
A design team composed of both researchers and community providers from the participating CTN sites developed the protocol collaboratively through regular conference calls. This both enhanced the acceptance of the protocol and insured that it would be feasible in many diverse sites. The design team identified a number of issues involved in evaluating MI and MET in the CTN that highlight dynamic tensions inherent in developing Stage III protocols, that is, preserving scientific integrity of the trial while fostering greater generalizability of findings.
Rather than seeing internal and external validity as mutually exclusive, the design team adopted a hybrid model that sought to maximize the scientific yield of the study by retaining key design features associated with efficacy research such as random assignment of patients to treatments, independence of treatment delivery and data collection, use of objective outcomes (e.g., urine toxicology screens), definition, and monitoring of treatments delivered (through manuals for behavioral treatments, specialized training of providers in delivering study treatments, and evaluation of the integrity of study treatments) (Carroll & Rounsaville, in press). However, as shown in Table 1, in order to also address issues of interest to clinicians, policy makers, and payors, additional components associated with effectiveness research were added. These included a multisite format to enhance diversity in patients and settings where treatments are delivered, delivery of study treatments by “real world” clinicians, evaluation of patient and provider satisfaction, and comparison of novel treatments to standard approaches (Carroll & Rounsaville, in press). In the following sections, we will summarize how these issues influenced our decisions regarding protocol design and therapist training and supervision.
3. Development of the MET/MI protocol: design challenges and strategies
Design challenges included whether MET or MI should be evaluated as a stand-alone or initial components of treatment, how they could be integrated into a treatment system organized around the provision of group therapy, variations across sites in the nature of standard treatment to which MET and MI would be compared, and issues associated with broadening inclusion and exclusion criteria and managing a diverse subject sample.
3.1. Stand alone vs. initial component of treatment
Among alcohol-using populations, MET and MI have been evaluated primarily as brief interventions consisting of between one and four sessions in their entirety. However, given the comparatively high severity, morbidity, and co-occurring problems seen among treatment-seeking drug-dependent individuals, it was unclear whether only a few sessions of treatment would be sufficient. Thus, a design was developed in which MET or MI was integrated as early as possible into the orientation/entry/evaluation phase of treatment as a strategy to enhance initial retention and outcome. This had the advantage of greater compatibility with clinical practice and also allowed comparison with a standard treatment control group (i.e., treatment as usual).
3.2. Individual vs. group delivery of treatment
While group treatment is pervasive in the substance abuse treatment system, MET and MI were developed and have been evaluated as solely individual treatments. With emphasis on providing personalized, objective feedback on the consequences of substance use and the development of highly individualized change plans, many aspects of MET would be difficult to implement in a group setting. Moreover, no data on the effectiveness of MET or MI in a group format or treatment manuals were available.
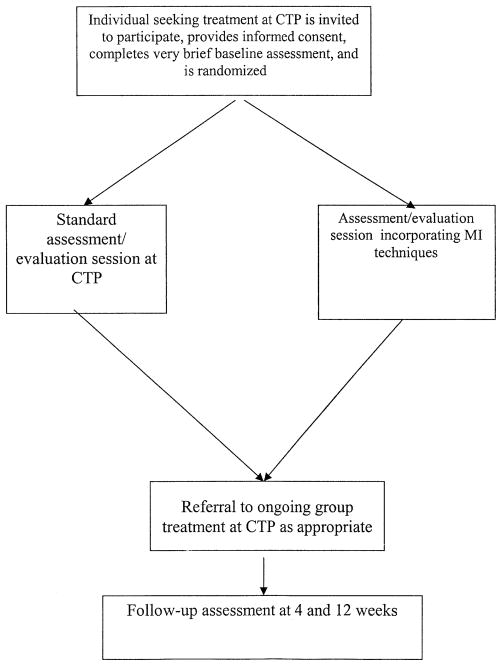
Thus, while it was fairly straightforward to develop a protocol evaluating MET or MI in those community treatment settings where individual treatment was customary, a new strategy was needed for those settings where solely group treatments were offered, given that another goal of the protocol team was to place minimal constraints and avoid changing standard treatments at the sites to accommodate the protocol. This led to the development of two independent protocols to accommodate these features of the treatment delivery system and participating sites. Therefore, for community programs that offered individual treatment, a protocol was developed that randomized patients to either three individual sessions of MET or three individual sessions of standard treatment, provided during the first month of treatment. The study design is summarized in Fig. 1.
Fig. 1.
MET protocol design.
For those settings that offered group treatments only, a second protocol was developed and is summarized in Fig. 2. Capitalizing on the programs’ convention of offering a single individual evaluation/assessment session prior to the patient’s being assigned to group treatment, this protocol will compare retention and outcome for individuals assigned to a standard evaluation/assessment session vs. one where techniques of MI are integrated. This resulted in two independent protocols addressing different, but related questions.
Fig. 2.
MI protocol design.
3.3. Setting diversity issues
Unlike efficacy studies where control or comparison conditions are selected to address very focused research questions (e.g., does Treatment X improve outcome compared with a minimal discussion control?), the MET/MI protocols and other CTN studies will be evaluating whether outcomes are improved when experimental treatments are added to or compared to standard treatments in community programs. Thus, the MET/MI protocols employed an “active treatment” comparison condition, which is usually associated with a smaller effect size than studies using no-treatment or less active discussion control conditions (Basham, 1986), and hence these protocols will provide a challenging test of MET and MI. Moreover, what constitutes “standard treatment” at the participating sites is not yet well-understood and is likely to vary widely across the participating programs. The programs themselves may espouse a particular orientation (disease model, CBT), but background and training differences across clinicians may also vary widely within a given program.
This had several implications for the design of the MET and MI protocols. First, given that the protocols are being conducted in 11 different CTPs across the country (six will implement the 3-session MET protocol, and five will implement the 1-session MI protocol), 11 different types of “standard treatment” may be offered as comparison conditions (although treatment modality and number of sessions would be constrained). One strategy used to anticipate this was to provide adequate statistical power through a comparatively large sample size. Thus, if meaningful site-by-treatment interactions occur, within-site analyses will be possible that might help pinpoint why MET or MI was more effective than standard treatment in some sites and not in others. Second, all study sessions (MET/MI and standard treatment) will be audio taped; process ratings will be done to determine whether there was any overlap of MET/MI techniques in standard treatment. Tape ratings will also characterize in detail the specific techniques used in standard treatment (disease model, cognitive behavioral, psychodynamic, other) at each of the participating sites.
3.4. Patient diversity issues: broadening inclusion/exclusion criteria
An important goal of the CTN is to evaluate the effectiveness of empirically validated treatments among more diverse samples of substance users than may be typical of efficacy trials (which have been criticized as being unrepresentative of patients seen in standard treatment) (Carroll, Nich, McLellan, McKay, & Rounsaville, 1999). Thus, the protocol sought to attract a highly heterogeneous sample by minimizing possible barriers to treatment entry and broadening study inclusion/exclusion criteria as much as possible. Therefore, inclusion criteria require only that prospective study participants be 18 years or older and current substance users seeking outpatient treatment. Excluded individuals are those who are seeking detoxification and methadone maintenance only or who are currently so psychiatrically or medically unstable that outpatient treatment is not feasible. Thus, these protocols are open to a wide variety of substance users (e.g. marijuana, cocaine, opioids, alcohol, and polysubstance users) with a wide variety of co-occurring psychiatric, legal, medical, employment, and social problems.
While the potential generalizability of such a study is exciting, higher levels of heterogeneity in the sample raised a variety of practical problems in developing a clinical research protocol that could meet the needs of “all comers.” For example, available treatment manuals for MET and MI were generally written targeting specific types of substance users (alcohol users, smokers, etc.). Thus, it was necessary to adapt existing MET and MI manuals (e.g., Ball, 1996; Miller et al., 1992; Miller & Rollnick, 1991; Obert, Rawson & Miotto, 1997) to be appropriate for a more diverse sample. Other adaptations involved adding a wider variety of exercises and strategies to address different levels of readiness to change, broadening the manual to anticipate working with participants with a variety of different mandates to treatment, and using flexible language to allow clinicians to adapt the interventions to a wide variety of individuals.
In addition, assessment instruments had to be selected or modified to anticipate a wide variety of types of substance use and related problems in the study sample while remaining quite brief (45 minutes total for the MI protocol, 90 minutes for the MET protocol). For example, the Short Inventory of Problems (SIP-R) was modified from the Drinker Inventory of Consequences (DrINC) (Miller, Tonigan, & Longabaugh, 1995) for use with drug users. The SIP-R was used in the assessment battery to allow for feedback on consequences of substance use to the participant and the development of discrepancies.
4. Training and supervisory challenges and strategies
Although methods and standards for training therapists to deliver manual-guided treatments in efficacy trials have been established for many years, the MET and MI protocol design team faced the additional challenge of developing a clinician training plan that would be feasible and effective for “real world” clinicians. This involved anticipating a high level of therapist diversity and adapting training and supervision procedures to meet the needs of this therapist group.
4.1. Therapist diversity issues
In many efficacy trials of behavioral treatments, therapists delivering the treatments are highly selected and experienced experts who have substantial commitment to the approach. Use of highly experienced and committed therapists is thought to simplify training, reduce variability in treatment delivery, and foster a high level of treatment fidelity (Carroll, Kadden, Donovan, Zweben, & Rounsaville, 1994; Crits-Christoph et al., 1998; Rounsaville, Chevron, Weissman, Prusoff, & Frank, 1986; Rounsaville, O’Malley, Foley, & Weissman, 1988).
However, a major question facing this protocol was whether MET/MI was effective when delivered by “real world” clinicians drawn from the staff of the participating CTPs. Thus, it would be necessary to recruit clinicians from the community programs who were willing to participate in the research project, undergo training in MET/MI, and agree to be supervised and have their clinical work taped for the duration of the study for process assessment of treatment fidelity.
An important threat to study validity might arise if the experimental treatment (MET/MI) was delivered by “eager volunteers” willing to participate in clinical research, while the standard treatment was delivered by clinicians who did not volunteer nor were interested in learning new approaches (as the two clinician groups might also differ with respect to other variables, such as general therapeutic skill, experience, ability to engage with clients, and so on). The solution adopted in this trial was to recruit a large number of volunteer clinicians from the staff of each participating site (at least six per site) and then randomize the clinicians themselves to deliver either MET/MI or standard treatment in the protocol. Clinicians assigned to the MET/MI condition would go through didactic training and supervised practice prior to being certified to deliver MET or MI in the protocol. Clinicians assigned to deliver standard treatment will be offered the opportunity to be trained in MET/MI after the protocol was completed.
Thus, unlike many efficacy trials of behavioral treatments, minimal training and educational requirements were made of the clinician/volunteers. The protocol required only that they be willing to learn MET/MI, participate in training and supervision sessions, and agree to have their sessions taped and monitored. This was intended to lead to a highly diverse group of clinicians, with wide variations in experience, education, and training backgrounds, knowledge of MET/MI or manual-guided treatments, and commitment to a wide variety of clinical approaches, but would also lead to particular challenges in training and supervising such a group of therapists.
Other important considerations in developing the therapist training/monitoring plans for this trial were its credibility and durability. That is, if MET/MI training and monitoring was highly centralized (e.g., provided through a single training center, as is common in many multisite efficacy studies to achieve a high degree of standardization across sites), it might be more difficult to recognize and respond to the unique issues involved in delivering MET/MI in each of the sites. Trainers in geographically distant locations might also be less well-equipped to work with the diversity of clinicians participating in the protocol. Moreover, a highly centralized approach would not broaden the availability in training resources across the sites.
Thus, the training protocol involved a decentralized system where an “MET/MI Expert Trainer” was identified at each site who was already skilled in and certified to provide MET/MI training. This group of expert trainers then participated in a specialized “training of trainers” program with Drs. William Miller and Theresa Moyers from the University of New Mexico. The training of the MET/MI expert trainers was intended to foster a consistent approach to training across the sites and to anticipate the challenges in training a highly diverse group of clinicians in MET/MI. The expert trainers then returned to their sites where they provided didactic training in MET/MI to the participating clinicians and one clinical supervisor in each site.
Training involved a 2-day didactic training seminar (including review of the MET or MI manuals, and training tapes plus several role plays) plus an ongoing certification/monitoring process that involved ongoing review of session tapes and evaluation of clinicians’ adherence and competence in delivering MET/MI throughout the trial. In addition, the expert trainers also trained one clinical supervisor at each site in MET/MI and in supervising clinicians to perform MET/MI. This was intended to provide additional supervisory support to clinicians, foster closer integration of the protocol in the clinics, as well as to provide durable, continuing MET/MI training resources at each of the participating programs.
4.2. MET/MI vs. standard approaches to treatment
A key challenge facing the trainers was the wide disparity between MET and MI and standard approaches to treatment at the programs. MET and MI were developed from observations that individuals seeking to change their behavior were often found to cycle through stages of readiness: precontemplation, contemplation, determination (or preparation), action, and maintenance. MET/MI applies a counseling style and specific techniques to mobilize inherent resources within the client for positive change. MET and MI are based on the premise that sustained positive change is most effectively achieved if the client is following a course that he/she has personally identified as being the “best,” rather than a course of treatment that has been imposed from an outside source.
The style in which these sessions are delivered is as important, if not more important than the content of the material. The client-centered, empathetic but directive interaction of MET/MI is designed to explore and reduce the inherent ambivalence in clients presenting for substance abuse treatment. This approach requires that the clinician relates to the client in a nonjudgmental, collaborative manner, which is a philosophical stance requiring both skill and patience. Working in the MET style, the clinician acts as a coach or consultant rather than an authority figure. While certain techniques may be useful in understanding how to deliver the interventions, the hallmark of MET therapy is the collaborative, empathic and respectful interactions. This nonjudgmental style may contrast with approaches used by many drug counselors. This led to a number of special considerations in training the clinicians for the protocol.
4.3. Experiences in didactic training
The experience of delivering a standardized training designed to teach the style and strategies of MET and MI proved to be both interesting and rewarding. The diversity of backgrounds and levels of previous knowledge of MI amongst recipients was quite apparent. The “real world” clinicians came from very different educational and practical backgrounds. Some entered the field from their own experience of recovery while others came from a range of education that varied from a 2-year community college experience to a doctoral degree. Many brought with them a long history of a confrontational-style practice or of being the authority who dictates to the client what to do.
In general, as in other recent trials of this type (Morgenstern, Morgan, McCrady, Keller, & Carroll, 2001), the clinicians were eager to learn a novel approach and found the MET/MI techniques persuasive and intuitive. Many clinicians expressed to the trainers their sense that they “already do this,’ that the MET/MI style and strategies were quite familiar, although these observations contrasted sharply with those of the trainers. During the seminars, the clinicians were able to recognize and adopt the empathic style of MET/MI with greater ease than some of the more subtle strategies associated with encouraging participants to change their behavior.
4.4. Experiences in supervision
After the didactic training, each clinician was assigned a number of “training cases,” in which they had an opportunity to practice MET or MI, depending on which of the two protocols their site implemented. All sessions were audio-taped and reviewed by the expert trainers who provided detailed feedback and supervision regarding the degree to which the clinician adhered to the manual and the skill in which they delivered the interventions. Thus, the trainers were faced with the challenge of reviewing session tapes from clinicians who were not accustomed to having their work scrutinized or assessed for fidelity to a treatment manual.
Moreover, despite many therapists’ sense that they were “already doing” MET or MI, the trainees lack of familiarity with the style and the complexity of delivering the treatment was heightened during the training cases. Many of the clinicians had been trained to offer advice, to tell clients what they think, and to confront denial by teaching the “facts” about drug dependence and recovery. Thus, the supervision process required that the trainers consistently challenge the clinicians to work very differently with their clients and think differently about their work.
Another issue encountered during the supervisory sessions was facilitating the clinicians’ adherence to the manual. Following a treatment manual was a novel concept for many of the clinicians (see Ball et al., 2001) who typically have a great deal of latitude in the way they deliver counseling. Thus, an important part of the supervision process became frequent review and reference to the MET or MI manuals. One of the most difficult concepts for some clinicians was the integration and utilization of available pretreatment assessment data as a basis for providing feedback to clients and developing discrepancy between stated goals and actual behavior, because it is not common practice in the real world to integrate structured feedback from objective assessments into the first few sessions with clients.
Trainers were careful to maintain a highly individualized, supportive stance with the clinicians, praising successful efforts to implement MET/MI, and pointing out specific instances where they had fallen back on a more traditional approach. Trainers found the most effective ways of spending supervision time was in the reviewing of actual session tapes, stopping the tape several times, and carefully analyzing specific interventions or missed opportunities for MET/MI techniques. Other useful methods of supervision were frequent role-plays and providing detailed feedback on adherence/competence rating forms. Supervisors found that merely asking the clinicians where they feel they need help without appropriately structuring the supervision time did not yield positive results.
Despite these challenges, the observation of the trainers was that the clinicians learned and implemented MET and MI quite well. Across the sites, the supervisors found that most of counselors were able to meet criteria for certification after the prescribed minimum number of training cases (one case for the MET protocol and three cases for the MI protocol) but approximately one-third of the clinicians required additional training cases to achieve minimal levels of proficiency.
5. Summary
The MET and MI protocols are large, multisite, randomized trials of brief behavioral interventions evaluating the effectiveness of manualized treatments in “real world” clinical settings. As one of the first CTN protocols, these trials will provide important data on the effectiveness and durability of these approaches across a wide range of patients and settings, on the capacity of clinicians to learn and implement these approaches effectively, and on the nature of standard treatments in these settings.
Table 1.
Design elements supporting internal and external validity used in MET and MI protocols
| Elements supporting internal validity | Elements supporting external validity |
|---|---|
| Random assignment to treatments | Comparison condition = treatment as usual |
| Manual guided treatments | Few restrictions on patient participation |
| Objective outcome measures, including urinalyses | Clinicians are volunteers from community programs |
| Training and ongoing supervision of therapists | Study conducted at 11 community treatment programs |
| Monitoring of treatment delivery, fidelity via independent evaluation of session tapes | Brief assessment battery (approximately 45 minutes for MI, 90 minutes for MET) |
Acknowledgments
Support was provided by NIDA grants U10 DA13038, DA DA13045, and K05-DA00457.
References
- Babor TF. Avoiding the horrid and beastly sin of drunkenness: does dissuasion make a difference? Journal of Consulting and Clinical Psychology. 1994;62:1127–1140. doi: 10.1037//0022-006x.62.6.1127. [DOI] [PubMed] [Google Scholar]
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment. New York: Springer-Verlag; 1991. [Google Scholar]
- Ball SA. Brief motivational intervention for heavy drinking. 1996. Unpublished treatment manual. [Google Scholar]
- Ball SA, Bachrach K, DeCarlo J, Farentinos C, Keen M, McSherry T, Polcin D, Snead N, Sockriter R, Wrigley P, Zammarelli L, Carroll KM. Characteristics of community clinicians trained to provide manual-guided therapy for substance abusers. 2001. Under review. [DOI] [PubMed] [Google Scholar]
- Basham RB. Scientific and practical advantages of comparative design in psychotherapy outcome research. Journal of Consulting and Clinical Psychology. 1986;34:88–94. doi: 10.1037//0022-006x.54.1.88. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kadden R, Donovan D, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. Journal of Studies on Alcohol. 1994;(Suppl 12):149–155. doi: 10.15288/jsas.1994.s12.149. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Libby B, Sheehan J, Hyland N. Motivational interviewing to enhance treatment initiation in substance abusers: an effectiveness study. American Journal on Addictions. 2001;10:335–339. doi: 10.1080/aja.10.4.335.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, McLellan AT, McKay JR, Rounsaville BJ. “Research” versus “real world” patients: representativeness of subjects participating in clinical trials of treatments for cocaine dependence. Drug and Alcohol Dependence. 1999;54:171–177. doi: 10.1016/s0376-8716(98)00161-6. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. Bridging the gap between research and practice in substance abuse treatment: a hybrid model linking efficacy and effectiveness research. Psychiatric Services. doi: 10.1176/appi.ps.54.3.333. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Chittams J, Barber JP, Beck AT, Frank A, Liese B, Luborsky L, Mark D, Mercer D, Onken LS, Najavits LM, Thase ME, Woody G. Training in cognitive, supportive-expressive, and drug counseling therapies for cocaine dependence. Journal of Consulting and Clinical Psychology. 1998;66:484–492. doi: 10.1037//0022-006x.66.3.484. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Bridging the gap between practice and research: forging partnerships with community-based drug and alcohol treatment. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]
- Martino S, Carroll KM, O’Malley SS, Rounsaville BJ. Motivational interviewing with psychiatrically ill substance abusing patients. American Journal on Addictions. 2000;9:88–91. doi: 10.1080/10550490050172263. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, O’Brien CP. Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: role of treatment services. Journal of Consulting and Clinical Psychology. 1994;62:1141–1158. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR. The treatment of addiction: what can research offer practice? In: Lamb S, Greenlick MR, McCarty D, editors. Bridging the gap between practice and research: forging partnerships with community based drug and alcohol treatment. Washington, DC: National Academy Press; 1998. pp. 147–185. [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford; 1991. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. NIAAA Project MATCH Monograph Series. Vol. 4. Rockville, MD: 1995. The Drinker Inventory of Consequences (DrInc): an instrument for assessing adverse consequences of alcohol abuse. Test manual. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Unpublished manuscript. Rockville, MD: 1992. Motivational enhancement therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. [Google Scholar]
- Morgenstern J, Morgan TJ, McCrady BS, Keller DS, Carroll KM. Manual-guided cognitive behavioral therapy training: a promising method for disseminating empirically supported substance abuse treatments to the practice community. Psychology of Addictive Behaviors. 2001;15:83–88. [PubMed] [Google Scholar]
- MTP Research Group. Treating cannabis dependence: findings from a multisite study. 2001. Under review. [Google Scholar]
- Obert JL, Rawson RA, Miotto K. Substance abuse treatment for “hazardous users”: an early intervention. Journal of Psychoactive Drugs. 1997;29:291–298. doi: 10.1080/02791072.1997.10400204. [DOI] [PubMed] [Google Scholar]
- Onken LS, Blaine JD, Battjes R. Behavioral therapy research: a conceptualization of a process. In: Hennegler SW, Amentos R, editors. Innovative approaches for difficult to treat populations. Washington, DC: American Psychiatric Press; 1997. pp. 477–485. [Google Scholar]
- Project MATCH Research Group. Matching Alcohol Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. NIDA’s stage model of behavioral therapies research: getting started and moving on from Stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. [Google Scholar]
- Rounsaville BJ, Chevron E, Weissman MM, Prusoff BA, Frank E. Training therapists to perform interpersonal psychotherapy in clinical trials. Comprehensive Psychiatry. 1986;27:364–371. doi: 10.1016/0010-440x(86)90012-x. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, O’Malley SS, Foley S, Weissman MM. Role of manual-guided training in the conduct and efficacy of interpersonal psychotherapy for depression. Journal of Consulting and Clinical Psychology. 1988;56:681–688. doi: 10.1037//0022-006x.56.5.681. [DOI] [PubMed] [Google Scholar]
- Saunders B, Wilkinson C, Philips M. The impact of a brief motivational intervention with opiate users attending a methadone programme. Addiction. 1995;90:415–424. doi: 10.1046/j.1360-0443.1995.90341510.x. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive Behaviors. 1997;11:294–307. [Google Scholar]
- Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. Journal of Nervous and Mental Disease. 1999;187:630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized controlled trials addressing brief interventions in heavy alcohol drinkers. Journal of General Internal Medicine. 1997;12:274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]