Abstract
Purpose
The long-term risk of prostate cancer–specific mortality (PCSM) after radical prostatectomy is poorly defined for patients treated in the era of widespread prostate-specific antigen (PSA) screening. Models that predict the risk of PCSM are needed for patient counseling and clinical trial design.
Methods
A multi-institutional cohort of 12,677 patients treated with radical prostatectomy between 1987 and 2005 was analyzed for the risk of PCSM. Patient clinical information and treatment outcome was modeled using Fine and Gray competing risk regression analysis to predict PCSM.
Results
Fifteen-year PCSM and all-cause mortality were 12% and 38%, respectively. The estimated PCSM ranged from 5% to 38% for patients in the lowest and highest quartiles of predicted risk of PSA-defined recurrence, based on a popular nomogram. Biopsy Gleason grade, PSA, and year of surgery were associated with PCSM. A nomogram predicting the 15-year risk of PCSM was developed, and the externally validated concordance index was 0.82. Neither preoperative PSA velocity nor body mass index improved the model's accuracy. Only 4% of contemporary patients had a predicted 15-year PCSM of greater than 5%.
Conclusion
Few patients will die from prostate cancer within 15 years of radical prostatectomy, despite the presence of adverse clinical features. This favorable prognosis may be related to the effectiveness of radical prostatectomy (with or without secondary therapy) or the low lethality of screen-detected cancers. Given the limited ability to identify contemporary patients at substantially elevated risk of PCSM on the basis of clinical features alone, the need for novel markers specifically associated with the biology of lethal prostate cancer is evident.
INTRODUCTION
Relative to other solid tumors, localized prostate cancer is characterized by an exceptionally protracted natural history. In population-based series of patients treated without curative intent in the era before prostate-specific antigen (PSA) screening, the 10-year prostate cancer–specific mortality (PCSM) ranged from 15% to 25%.1–3 After radical prostatectomy, the 10-year PCSM was 15% in an unscreened cohort.4 The natural history of prostate cancer in screened populations is poorly defined but may be substantially more favorable, given that the diagnostic lead time associated with screening is estimated to be 11 years.5
Given this natural history, PSA-defined prostate cancer recurrence is widely used as an end point to assess treatment success. Models that predict PSA recurrence are the primary tools for counseling patients, clinical decision making, and stratifying patients in clinical trials.6,7 A prostate cancer nomogram is currently the most widely used, disease-specific prediction tool in oncology.8 However, PSA recurrence is not a surrogate for PCSM.9 Within 15 years of PSA recurrence, men are as likely to die from competing causes as they are from prostate cancer.10
Treatment decision making for localized prostate cancer and the powering of clinical trials for clinically significant end points require accurate estimations of PCSM that account for the stage migration induced by PSA screening. We endeavored to evaluate the risk of PCSM after radical prostatectomy and to construct a predictive nomogram for patients treated in the era of widespread PSA screening.
METHODS
Study Population
Between 1987 and 2005, 6,398 patients underwent radical prostatectomy for localized prostate cancer at Memorial Sloan-Kettering Cancer Center (New York, NY) and Baylor College of Medicine (Houston, TX); these patients formed the modeling cohort for nomogram development. Of these patients, 809 (13%) received neoadjuvant androgen deprivation therapy (ADT) for a median of 3.2 months (interquartile range [IQR], 2.1 to 4.2 months), 94% of whom were treated before 2002 when neoadjuvant ADT was under investigation. External validation of the nomogram was performed on 4,103 patients treated at Cleveland Clinic (Cleveland, OH) and 2,176 patients treated at the University of Michigan (Ann Arbor, MI) during the same time period. Clinical information was obtained from prospectively maintained, institutional review board–approved databases (Table 1).
Table 1.
Clinical Characteristics of Modeling and Validation Cohorts
| Characteristic | Modeling Cohort |
Validation Cohort |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Patients | 6,398 | 6,279 | ||
| Age, years | ||||
| Median | 61 | 60 | ||
| IQR | 56-66 | 55-65 | ||
| PSA, ng/mL | ||||
| Median | 6.3 | 6.0 | ||
| IQR | 4.4-9.5 | 4.5-8.8 | ||
| Biopsy Gleason score | ||||
| 2-6 | 4,126 | 64 | 3,825 | 61 |
| 7 | 1,787 | 28 | 1,832 | 29 |
| 8-10 | 403 | 6 | 356 | 6 |
| Missing value | 82 | 1 | 266 | 4 |
| Clinical stage | ||||
| T1ab | 147 | 2 | 57 | 1 |
| T1c | 2,700 | 42 | 4,035 | 64 |
| T2a | 1,242 | 19 | 1,358 | 22 |
| T2b | 1,119 | 18 | 426 | 7 |
| T2c | 568 | 9 | 178 | 3 |
| T3 | 244 | 4 | 47 | 1 |
| Missing value | 378 | 6 | 178 | 3 |
| Neoadjuvant ADT | 809 | 13 | 397 | 6 |
| Year of surgery | ||||
| 1987-1990 | 488 | 8 | 348 | 6 |
| 1991-1998 | 2,442 | 38 | 1,782 | 28 |
| 1999-2005 | 3,468 | 54 | 4,149 | 66 |
| Postoperative pelvic radiation therapy | 115 | 2 | 538 | 8 |
| Postoperative androgen deprivation therapy | 426 | 7 | 343 | 6 |
| Death from prostate cancer | 117 | 2 | 98 | 2 |
| Death from competing causes | 343 | 5 | 343 | 6 |
| Follow-up, months | ||||
| Median | 48 | 54 | ||
| IQR | 18-90 | 24-99 | ||
Abbreviations: IQR, interquartile range; PSA, prostate-specific antigen; ADT, androgen deprivation therapy.
Prostate biopsy specimens were reviewed by pathologists at each institution before surgery. In general, patients were observed for disease recurrence postoperatively with regular serum PSA determinations and clinical assessment at 3- to 6-month intervals for the first 5 years and annually thereafter. For deceased patients, death was attributed to prostate cancer using death certificates and was confirmed by evidence of progressive metastatic, androgen-independent disease on review of the patients' medical records.
Statistical Analysis
Survival analysis was performed using Fine and Gray competing risks regression to estimate PCSM and to account for competing causes of mortality.11 PSA was modeled as a restricted cubic spline for suspected nonlinear effect. Primary and secondary biopsy Gleason grades were modeled as categoric variables (≤ 3 and ≥ 4). All decisions with respect to the coding of the variables were made before modeling. Patients with missing values were excluded rather than having missing values imputed. PSA velocity was calculated by linear regression analysis using all available values within 18 months of radical prostatectomy and a minimum of two measurements at least 6 weeks apart. Information for PSA velocity was available for 2,279 patients (36%) in the modeling cohort, and calculations were based on a median of three values (range, 2 to 17 months) over a median of 7 months (range, 2 to 18 months) before treatment. Body mass index (BMI) was available for 3,033 patients (47%) and was calculated using height and weight information obtained from objective measurements before treatment. BMI was calculated by dividing the weight (in kilograms) by the square of the height (in meters). For these patients, the median PSA velocity was 1.1 ng/mL/yr (IQR, 0.1 to 2.6 ng/mL/yr) and the median BMI was 27 kg/m2 (IQR, 25 to 30 kg/m2).
For external validation of the model, we assessed both discrimination and calibration. Discrimination refers to the ability of the nomogram to rank patients by their risk, such that patients with a higher predicted risk of PCSM should be more likely to die from prostate cancer. Discrimination is easily quantifiable using the concordance index, which is similar to an area under the receiver operating characteristic curve and is applicable to time-to-event data.12 Calibration refers to the accuracy of the nomogram as assessed by a visual inspection of the plots of predicted PCSM versus actual outcome. All statistical analysis was performed using S-Plus 2000 (Insightful, Redmond, WA) with additional functions (called “Design”) added. All P values resulted from the use of two-sided statistical tests.
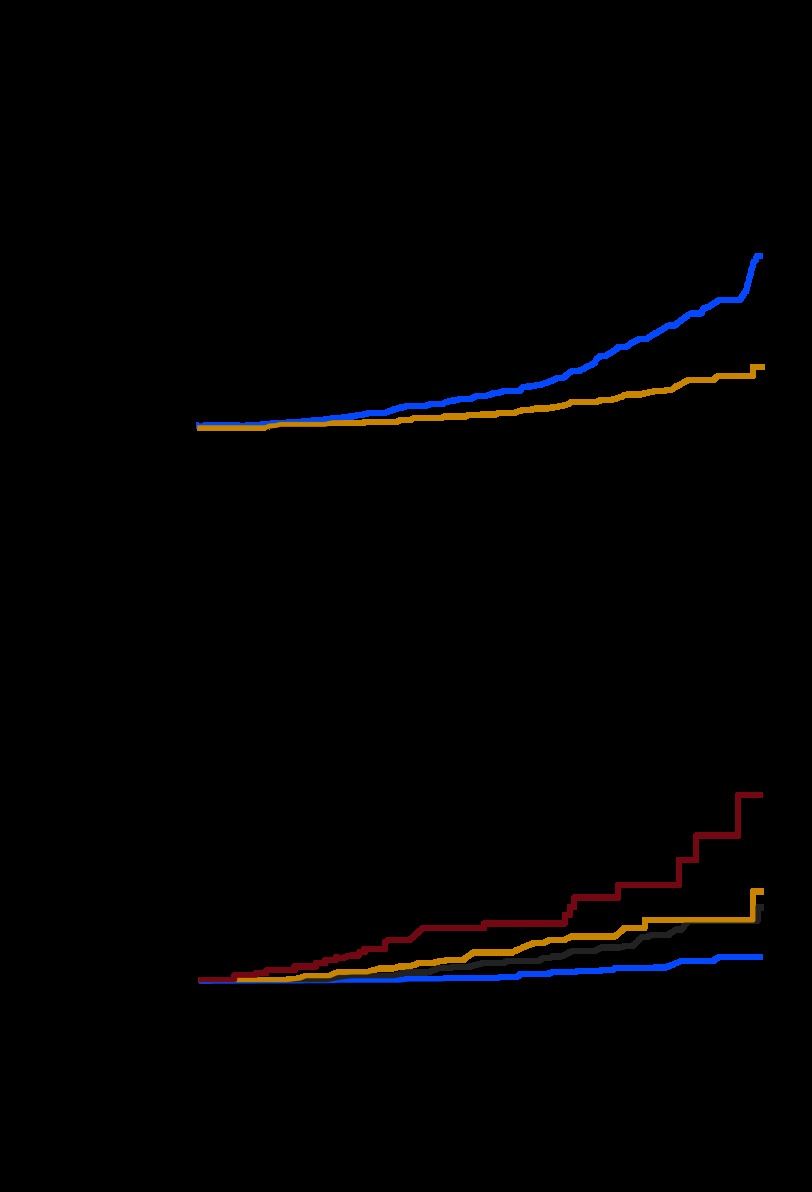
RESULTS
In the modeling cohort, 117 patients died as a result of prostate cancer and 343 died as a result of competing causes over a median follow-up of 48 months (IQR, 18 to 90 months; Table 1). The 15-year PCSM and all-cause mortality were 12% (95% CI, 9% to 15%) and 38% (95% CI, 33% to 42%), respectively (Fig 1A). These results were similar in the validation cohort. In both cohorts, the percentage of patients lost to follow-up at 5, 10, and 15 years was 17%, 24%, and 16%, respectively.
Fig 1.
(A) Prostate cancer–specific mortality (gold) and death from competing causes (blue) after radical prostatectomy. (B) Prostate cancer–specific mortality after radical prostatectomy stratified by validated preoperative nomogram predictions of 5-year prostate-specific antigen (PSA) progression-free probability (PFP) of 76% to 99% (blue), 51% to 75% (gray), 26% to 50% (gold), and 1% to 25% (red).
The risk of PCSM was assessed for commonly used prognostic tools for PSA recurrence based on clinical stage, Gleason grade, and PSA (Table 2). The 5-year PSA progression-free probability (PFP) derived from a nomogram was significantly associated with PCSM when analyzed either as a continuous or categoric variable based on quartiles of nomogram probabilities (P < .001 for both).6 For patients in the most favorable quartile (5-year PSA PFP, 76% to 99%), the 15-year PCSM was 5% compared with 38% in the lowest quartile (5-year PSA PFP, 1% to 25%; Fig 1B). When analyzed by previously validated risk groups for PSA recurrence, the 15-year PCSM was 2%, 10%, and 19% for patients classified as good risk, intermediate risk, and high risk (P < .001).7 The low PCSM rate among good-risk patients is noteworthy considering they constitute 46% of patients in this study. Most cancer deaths were observed in high-risk patients. However, the 15-year PCSM in this group was significantly less than the 31% (95% CI, 26% to 57%) mortality from competing causes. PCSM was similar to death as a result of competing causes (26%; 95% CI, 15% to 46%) only among patients with a nomogram-predicted 5-year PSA PFP of 1% to 25%.
Table 2.
Risk of Prostate Cancer–Specific Mortality at 10 and 15 Years After Radical Prostatectomy
| Variable | Patients* |
Events* |
10-Year PCSM |
15-Year PCSM |
||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | % | 95% CI | % | 95% CI | |
| Nomogram-predicted 5-year PFP, % | ||||||||
| 76-99 | 8,555 | 73 | 51 | 26 | 1.8 | 1.2 to 2.4 | 5 | 3 to 7 |
| 51-75 | 2,228 | 19 | 75 | 38 | 6 | 4 to 7 | 15 | 10 to 21 |
| 26-50 | 656 | 6 | 40 | 21 | 9 | 6 to 12 | 16 | 9 to 22 |
| 1-25 | 209 | 2 | 29 | 15 | 15 | 9 to 22 | 38 | 19 to 56 |
| Risk group | ||||||||
| PSA < 10, Gleason score 6, T1c or T2a | 5,200 | 46 | 14 | 7 | 0.9 | 0.3 to 1.5 | 2 | 0.3 to 4 |
| PSA 10-20, Gleason score 7, T2B | 4,184 | 37 | 64 | 32 | 4 | 2 to 5 | 10 | 6 to 14 |
| PSA > 20, Gleason score 8-10, T2c-T3 | 1,962 | 17 | 121 | 61 | 8 | 7 to 10 | 19 | 14 to 24 |
| Pretreatment PSA, ng/mL | ||||||||
| < 4 | 2,285 | 18 | 18 | 9 | 2 | 1 to 4 | 4 | 1 to 7 |
| 4-10 | 7,574 | 61 | 75 | 37 | 3 | 2 to 4 | 9 | 5 to 12 |
| 10.1-20 | 1,874 | 15 | 50 | 24 | 4 | 3 to 6 | 11 | 6 to 15 |
| 20.1-50 | 726 | 6 | 62 | 30 | 10 | 7 to 12 | 22 | 15 to 30 |
| 1992 TNM clinical stage | ||||||||
| T1ab | 174 | 2 | 4 | 2 | 2 | 0 to 4 | 6 | 0 to 12 |
| T1c | 6,413 | 56 | 28 | 14 | 2 | 1 to 3 | 6 | 5 to 7 |
| T2a | 2,520 | 22 | 42 | 21 | 3 | 2 to 4 | 7 | 4 to 10 |
| T2b | 1,461 | 13 | 57 | 29 | 5 | 3 to 7 | 14 | 9 to 19 |
| T2c | 714 | 6 | 38 | 19 | 7 | 4 to 9 | 12 | 8 to 17 |
| T3 | 254 | 2 | 28 | 14 | 15 | 9 to 21 | 38 | 22 to 54 |
| Biopsy Gleason score | ||||||||
| 2-6 | 7,454 | 65 | 78 | 40 | 2 | 1 to 3 | 6 | 4 to 8 |
| 7 | 3,292 | 29 | 55 | 28 | 5 | 3 to 7 | 17 | 8 to 26 |
| 8-10 | 702 | 6 | 61 | 32 | 16 | 11 to 20 | 34 | 23 to 46 |
NOTE. Values were based on a previously validated nomogram, risks groups, clinical stage, pretreatment PSA, and biopsy Gleason score.
Abbreviations: PCSM, prostate cancer–specific mortality; PFP, progression-free probability; PSA, prostate-specific antigen.
Percentages refer to proportion of total.
A univariable analysis of the long-term risk of PCSM by clinical stage, Gleason score, and PSA was performed (Table 2). Fifty-six percent of patients had stage T1c prostate cancer, and the 15-year PCSM was 6%. All 28 decedents with stage T1c had other adverse features such as a PSA > 10 ng/mL, specimen Gleason score 7 to 10 cancer, or advanced pathologic features (lymph node metastasis or seminal vesicle invasion). Of the 7,454 patients with biopsy Gleason score 2 to 6 cancer, only 78 cancer deaths were observed, 62 (79%) of whom were treated between 1987 and 1993, when biopsy technique and histological grading differed from current practice.13 Indeed, a significant reduction in the rate of upgrading at radical prostatectomy was observed for patients with biopsy Gleason score 2 to 6 cancers diagnosed before 1993 compared with diagnosis after 1998 (46% v 37%; P = .011). Both of these factors may have contributed to undergrading, because 86% of the decedents were upgraded to specimen Gleason score 7 to 10 cancer at radical prostatectomy.
By multivariable analysis, primary and secondary biopsy Gleason grade 4 and 5 (P < .001 for both) and increasing PSA (P = .021) were associated with PCSM. The year of surgery was inversely related to PCSM (P < .001), with contemporary patients having an improved prognosis. No significant association with PCSM was observed for PSA velocity (P = .072) or BMI (P = .4).
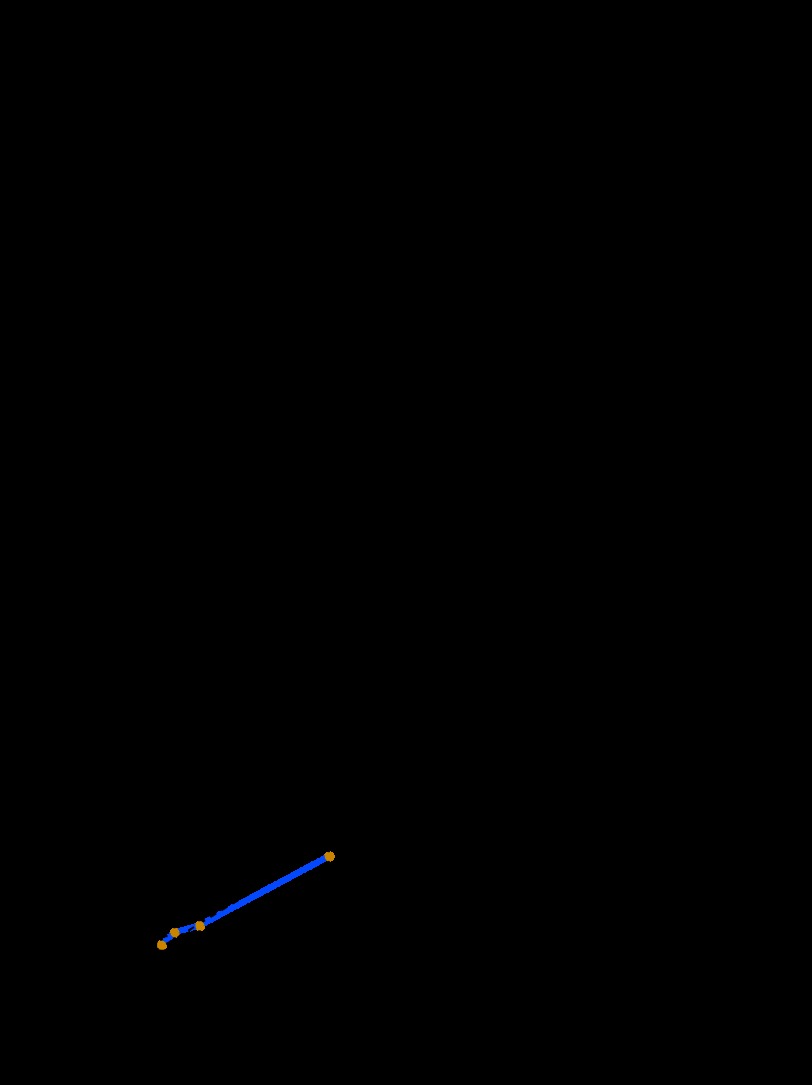
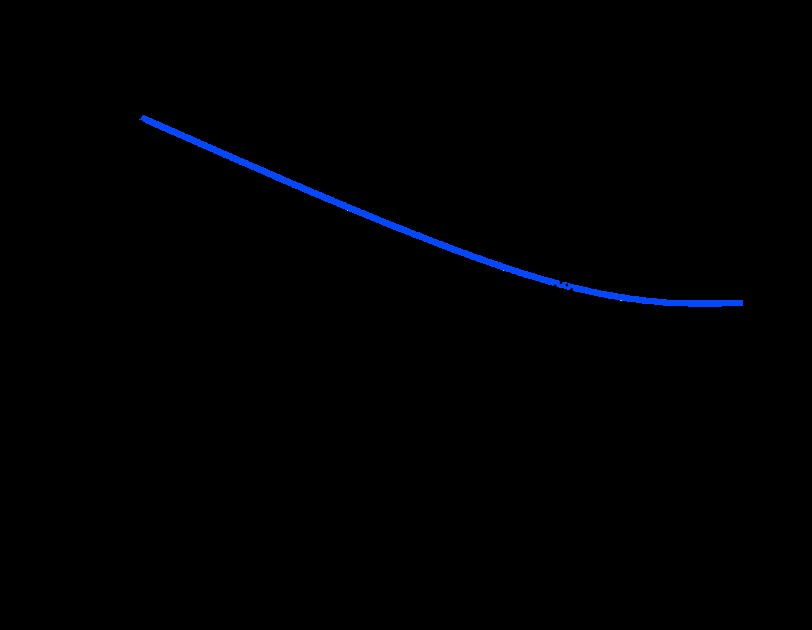
A nomogram predicting the risk of PCSM at 10 and 15 years was constructed on the basis of four standard parameters, and the predictions were adjusted for the year of surgery (the model assumes patients were treated in 2005; Fig 2A). The externally validated concordance index was 0.82, and predictions closely approximated the actual outcome (Fig 2B). Adjusting predictions for treatment in year 2005 is likely to be valid for future patients because the adjusted hazard ratio associated with year of surgery exhibited a sharp decline from 1987 to 1998 but was relatively stable thereafter (Fig 3). Neither the addition of PSA velocity (concordance index, 0.763 v 0.759) nor BMI (concordance index, 0.761 v 0.756) substantially improved the predictive accuracy of models based on standard parameters in the 2,279 and 3,033 patients with complete data for these parameters, respectively.
Fig 2.
(A) Preoperative nomogram predicting 10- and 15-year prostate cancer–specific mortality after radical prostatectomy. (B) Calibration of the nomogram. Dashed line indicates reference line where an ideal nomogram would lie. Instructions: Locate the patient's primary Gleason grade on the respective axis. Draw a straight line up to the Points axis to determine how many points toward prostate cancer–specific mortality he receives for his primary Gleason grade. Repeat this process for the other three parameters. Sum the points and locate this number on the Total Points axis. Draw a straight line down to find the patient's probability of dying as a result of prostate cancer within 10 or 15 years of treatment.
Fig 3.
Log relative hazard of prostate cancer–specific mortality (PCSM) associated with year of surgery after controlling for biopsy Gleason grade, pretreatment prostate-specific antigen (PSA), and clinical stage (dotted line) Performance of optimal model; (blue line) performance of nomogram.
Considering all 11,649 patients in both cohorts with complete data, only 1,980 (17%) had a predicted 15-year PCSM greater than 5%, and 467 (4%) had a probability greater than 30%. Considering the 7,403 patients treated since 1998, 296 (4%) had a probability of PCSM greater than 5%, and only 37 (0.5%) had a predicted risk greater than 30%.
DISCUSSION
The slow clinical progression of prostate cancer after radical prostatectomy has necessitated the use of PSA recurrence as the primary end point for evaluating treatment outcome. However, PSA recurrence has a highly variable natural history and poses limited threat to the longevity of many patients. Hence, models that predict the risk of PCSM are needed. Ours is the first multi-institutional study of PCSM after radical prostatectomy for patients diagnosed in the era of widespread PSA screening. Hitherto poorly defined, the risk of death as a result of prostate cancer in a screened population is low, even for patients with adverse clinical features. Our nomogram accurately predicts the probability of PCSM using standard clinical parameters. Few contemporary patients had a predicted 15-year PCSM greater than 5%, highlighting the difficulty in identifying patients at substantially increased risk on the basis of clinical parameters alone. The need for novel markers specifically associated with the biology of lethal prostate cancer is evident.
Large, single-institution radical prostatectomy series have reported rates of PSA recurrence in approximately 25% of patients.10,14,15 Studies analyzing PCSM after radical prostatectomy were previously limited to cohorts diagnosed before the introduction of PSA.4,16–18 In our study, the overall 15-year PCSM was 12% for patients treated in the PSA era. Even for patients at the highest risk of PSA recurrence, the 10-year PCSM was only 15%, which compares favorably with the 50% to 70% PCSM reported for similar patients from unscreened populations who received no curative treatment.2
Currently, the vast majority of patients diagnosed in the United States (including 71% of our patients since 1998) are classified as good risk (clinical stage T1c or T2a, PSA < 10, and biopsy Gleason grade ≤ 6). Our results demonstrate the low lethality of these cancers after radical prostatectomy. Most of the decedents who were classified as good risk at diagnosis were clinically understaged or undergraded because they had pathologically advanced and/or high-grade cancers on examination of the radical prostatectomy specimen. Potentially, many of these patients may have had a similarly low risk of PCSM had they received no treatment. Comparative studies of patients treated without curative intent are limited to cohorts diagnosed before the PSA era.1–4 In the United States, only 2% of patients younger than 65 years choose active surveillance,19 and an estimated 73% of those who do ultimately opt for radical therapy within 4 years.20 The feasibility and safety of active surveillance in appropriately selected patients has been demonstrated, but it is not widely embraced because of concerns that clinical staging and grading underestimate the threat posed by the cancer.21 Currently, an international randomized trial is comparing active surveillance against radical treatment for good-risk cancer, but results are not expected for many years.
The discrepancy between the risk of PSA recurrence and PCSM may be explained by the variable natural history of PSA recurrence; only patients with a short PSA doubling time have a higher risk of PCSM relative to mortality from competing causes.22 Alternatively, this discrepancy may be related to the efficacy of secondary therapy: adjuvant radiation therapy and ADT have been shown to improve metastasis-free and overall survival.23,24 Lastly, the favorable impact of local disease control on the survival of women with breast cancer has been observed,25 and a similar effect in prostate cancer is suggested by the improved survival of patients with metastatic disease who received prior radical prostatectomy.26
Given the inadequacies of PSA recurrence as a valid surrogate end point, clinical trials in localized prostate cancer have focused on distant metastasis and PCSM as end points. The few contemporary patients with a predicted PCSM of greater than 5% has significant implications for clinical trial design. Any clinical trial in localized prostate cancer would require a sample size of thousands and a follow-up of 20 years to have sufficient power to detect a significant survival difference. There are few examples of successful clinical trials of this size in genitourinary oncology. Until molecular markers are discovered that identify a cohort of patients with lethal prostate cancer, future clinical trials may need to rely on PSA recurrence as the primary end point, despite its limitations.
PSA velocity has previously been reported to be associated with PCSM, although its predictive utility in models that include PSA, grade, and clinical stage has not been evaluated.27,28 In a recent study using data from the US prostate cancer screening trial, PSA velocity (when combined with standard clinical parameters) did not improve the accuracy of predicting poorly differentiated or pathologically advanced cancer.29 When combined with PSA, PSA velocity did not enhance the ability to predict the long-term risk of metastatic or locally advanced prostate cancer in a large, unscreened population.30 PSA velocity also did not significantly add to the accuracy of our nomogram. Though the timing of PSA measurements and the assays used were not standardized in our study, PSA velocity is not a clinically useful marker for the general population if these conditions must be satisfied. Although PSA velocity data were available for only 36% of our patients, this information was missing for 23% to 39% of patients in other studies, which argues against selection bias as an explanation for its lack of prognostic significance in our study.27,28 The failure of PSA velocity to improve the accuracy of our nomogram may be explained by its close correlation with PSA.31 We were also unable to identify an association between BMI and PCSM, despite its reported association with PSA recurrence in surgical series,32 and PCSM in population-based studies.33
More recent year of surgery has been reported to be associated with an improved risk of PSA recurrence.34 Year of surgery was also significantly associated with PCSM. Although the improved prognosis of contemporary patients may reflect improvements in surgical technique or changes in the tumor grading practices over time,13,35 it may be explained by the diagnostic lead time associated with PSA screening, which is estimated to be 11 years.5 The independent prognostic significance of year of surgery suggests that screen-detected cancers may have different biologic properties compared with similar cancers detected in the absence of screening. The favorable effect of year of surgery on PSA recurrence and PCSM appears to stabilize after 1998. Among the patients treated after 1998, only 4% had a 15-year PCSM probability of greater than 5% and less than 1% had a risk of greater than 30%.
Our study has several limitations worth noting. The nomogram predicts the probability of PCSM within 15 years, but patients seem to be at risk of PCSM for up to 20 years after treatment.17 A recent study of patients treated without curative intent in the pre-PSA era has suggested an acceleration in PCSM after 15 years,3 although a contradictory finding was reported in a separate study.1 The long-term risk of PCSM was low among patients in our study, but we do not know how these patients would have fared without radical therapy. Likewise, we are unable to compare the effectiveness of radical prostatectomy with other forms of treatment such as external-beam radiation therapy or brachytherapy. Our model considers only PCSM and does not consider health-related quality-of-life issues. All treatments for localized prostate cancer affect urinary, sexual, and bowel function to varying degrees, which the patient must also consider when formulating a treatment decision.36 An optimal nomogram would predict quality-adjusted survival. However, prospective, longitudinal quality-of-life data using validated instruments from patients with long-term follow-up are not available at this time. Lastly, our study consists of patients treated at high-volume, tertiary referral centers and thus the model presented here may not be as accurate for those treated in the community setting.
In summary, the long-term risk of PCSM among patients treated with radical prostatectomy in the era of widespread PSA screening is low, even for patients with adverse clinical features. This favorable prognosis may be related to the effectiveness of radical prostatectomy (with or without secondary therapy) or the low lethality of screen-detected cancers within 15 years of treatment. We have constructed and validated a nomogram that accurately predicts the 15-year PCSM, but few patients are predicted to have a substantially elevated risk on the basis of standard clinical parameters. Neither PSA velocity nor BMI were useful markers in our model. Our study is anticipated to provide important and useful information for patients and physicians regarding treatment decision making for localized prostate cancer.
Footnotes
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Andrew J. Stephenson, Michael W. Kattan, James A. Eastham, Fernando J. Bianco Jr, Ofer Yossepowitch, Andrew J. Vickers, Eric A. Klein, David P. Wood, Peter T. Scardino
Financial support: James A. Eastham, Eric A. Klein, David P. Wood, Peter T. Scardino
Administrative support: Andrew J. Stephenson, James A. Eastham, Eric A. Klein, David P. Wood, Peter T. Scardino
Provision of study materials or patients: James A. Eastham, Eric A. Klein, David P. Wood, Peter T. Scardino
Collection and assembly of data: Andrew J. Stephenson, Michael W. Kattan, James A. Eastham, Eric A. Klein, David P. Wood, Peter T. Scardino
Data analysis and interpretation: Andrew J. Stephenson, Michael W. Kattan, James A. Eastham, Fernando J. Bianco Jr, Ofer Yossepowitch, Andrew J. Vickers, Eric A. Klein, David P. Wood, Peter T. Scardino
Manuscript writing: Andrew J. Stephenson, Peter T. Scardino
Final approval of manuscript: Andrew J. Stephenson, Michael W. Kattan, James A. Eastham, Fernando J. Bianco Jr, Ofer Yossepowitch, Andrew J. Vickers, Eric A. Klein, David P. Wood, Peter T. Scardino
REFERENCES
- 1.Albertsen PC, Hanley JA, Fine J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA. 2005;293:2095–2101. doi: 10.1001/jama.293.17.2095. [DOI] [PubMed] [Google Scholar]
- 2.Cuzick J, Fisher G, Kattan MW, et al. Long-term outcome among men with conservatively treated localised prostate cancer. Br J Cancer. 2006;95:1186–1194. doi: 10.1038/sj.bjc.6603411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johansson JE, Andren O, Andersson SO, et al. Natural history of early, localized prostate cancer. JAMA. 2004;291:2713–2719. doi: 10.1001/jama.291.22.2713. [DOI] [PubMed] [Google Scholar]
- 4.Bill-Axelson A, Holmberg L, Ruutu M, et al. Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med. 2005;352:1977–1984. doi: 10.1056/NEJMoa043739. [DOI] [PubMed] [Google Scholar]
- 5.Draisma G, Boer R, Otto SJ, et al. Lead times and overdetection due to prostate-specific antigen screening: Estimates from the European Randomized Study of Screening for Prostate Cancer. J Natl Cancer Inst. 2003;95:868–878. doi: 10.1093/jnci/95.12.868. [DOI] [PubMed] [Google Scholar]
- 6.Kattan MW, Eastham JA, Stapleton AM, et al. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst. 1998;90:766–771. doi: 10.1093/jnci/90.10.766. [DOI] [PubMed] [Google Scholar]
- 7.D'Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–974. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 8.Blumberg JW. PDA applications for physicians. ASCO News. 2004;16:S4–S6. [Google Scholar]
- 9.Prentice RL. Surrogate endpoints in clinical trials: Definition and operational criteria. Stat Med. 1989;8:431–440. doi: 10.1002/sim.4780080407. [DOI] [PubMed] [Google Scholar]
- 10.Bianco FJ, Jr, Scardino PT, Eastham JA. Radical prostatectomy: Long-term cancer control and recovery of sexual and urinary function (“trifecta”) Urology. 2005;66:83–94. doi: 10.1016/j.urology.2005.06.116. [DOI] [PubMed] [Google Scholar]
- 11.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. JASA. 1999;94:496–509. [Google Scholar]
- 12.Harrell FE, Jr, Califf RM, Pryor DB, et al. Evaluating the yield of medical tests. JAMA. 1982;247:2543–2546. [PubMed] [Google Scholar]
- 13.Albertsen PC, Hanley JA, Barrows GH, et al. Prostate cancer and the Will Rogers phenomenon. J Natl Cancer Inst. 2005;97:1248–1253. doi: 10.1093/jnci/dji248. [DOI] [PubMed] [Google Scholar]
- 14.Kupelian PA, Elshaikh M, Reddy CA, et al. Comparison of the efficacy of local therapies for localized prostate cancer in the prostate-specific antigen era: A large single-institution experience with radical prostatectomy and external-beam radiotherapy. J Clin Oncol. 2002;20:3376–3385. doi: 10.1200/JCO.2002.01.150. [DOI] [PubMed] [Google Scholar]
- 15.Han M, Partin AW, Zahurak M, et al. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003;169:517–523. doi: 10.1097/01.ju.0000045749.90353.c7. [DOI] [PubMed] [Google Scholar]
- 16.Zincke H, Oesterling JE, Blute ML, et al. Long-term (15 years) results after radical prostatectomy for clinically localized (stage T2c or lower) prostate cancer. J Urol. 1994;152:1850–1857. doi: 10.1016/s0022-5347(17)32399-6. [DOI] [PubMed] [Google Scholar]
- 17.Porter CR, Kodama K, Gibbons RP, et al. 25-year prostate cancer control and survival outcomes: A 40-year radical prostatectomy single institution series. J Urol. 2006;176:569–574. doi: 10.1016/j.juro.2006.03.094. [DOI] [PubMed] [Google Scholar]
- 18.Han M, Partin AW, Pound CR, et al. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy: The 15-year Johns Hopkins experience. Urol Clin North Am. 2001;28:555–565. doi: 10.1016/s0094-0143(05)70163-4. [DOI] [PubMed] [Google Scholar]
- 19.Harlan SR, Cooperberg MR, Elkin EP, et al. Time trends and characteristics of men choosing watchful waiting for initial treatment of localized prostate cancer: Results from CaPSURE. J Urol. 2003;170:1804–1807. doi: 10.1097/01.ju.0000091641.34674.11. [DOI] [PubMed] [Google Scholar]
- 20.Carter CA, Donahue T, Sun L, et al. Temporarily deferred therapy (watchful waiting) for men younger than 70 years and with low-risk localized prostate cancer in the prostate-specific antigen era. J Clin Oncol. 2003;21:4001–4008. doi: 10.1200/JCO.2003.04.092. [DOI] [PubMed] [Google Scholar]
- 21.Klotz L. Active surveillance for prostate cancer: For whom? J Clin Oncol. 2005;23:8165–8169. doi: 10.1200/JCO.2005.03.3134. [DOI] [PubMed] [Google Scholar]
- 22.Freedland SJ, Humphreys EB, Mangold LA, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005;294:433–439. doi: 10.1001/jama.294.4.433. [DOI] [PubMed] [Google Scholar]
- 23.Thompson IM, Jr, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: A randomized clinical trial. JAMA. 2006;296:2329–2335. doi: 10.1001/jama.296.19.2329. [DOI] [PubMed] [Google Scholar]
- 24.Messing EM, Manola J, Sarosdy M, et al. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med. 1999;341:1781–1788. doi: 10.1056/NEJM199912093412401. [DOI] [PubMed] [Google Scholar]
- 25.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 26.Thompson IM, Tangen C, Basler J, et al. Impact of previous local treatment for prostate cancer on subsequent metastatic disease. J Urol. 2002;168:1008–1012. doi: 10.1016/S0022-5347(05)64562-4. [DOI] [PubMed] [Google Scholar]
- 27.D'Amico AV, Chen MH, Roehl KA, et al. Preoperative PSA velocity and the risk of death from prostate cancer after radical prostatectomy. N Engl J Med. 2004;351:125–135. doi: 10.1056/NEJMoa032975. [DOI] [PubMed] [Google Scholar]
- 28.Carter HB, Ferrucci L, Kettermann A, et al. Detection of life-threatening prostate cancer with prostate-specific antigen velocity during a window of curability. J Natl Cancer Inst. 2006;98:1521–1527. doi: 10.1093/jnci/djj410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pinsky PF, Andriole G, Crawford ED, et al. Prostate-specific antigen velocity and prostate cancer Gleason grade and stage. Cancer. 2007;109:1689–1695. doi: 10.1002/cncr.22558. [DOI] [PubMed] [Google Scholar]
- 30.Ulmert D, Serio AM, O'Brien MF, et al. Long-term prediction of prostate cancer: Prostate-specific antigen (PSA) velocity is predictive but does not improve the predictive accuracy of a single PSA measurement 15 years or more before cancer diagnosis in a large, representative, unscreened population. J Clin Oncol. 2008;26:835–841. doi: 10.1200/JCO.2007.13.1490. [DOI] [PubMed] [Google Scholar]
- 31.Etzioni RD, Ankerst DP, Weiss NS, et al. Is prostate-specific antigen velocity useful in early detection of prostate cancer? A critical appraisal of the evidence. J Natl Cancer Inst. 2007;99:1510–1515. doi: 10.1093/jnci/djm171. [DOI] [PubMed] [Google Scholar]
- 32.Amling CL, Riffenburgh RH, Sun L, et al. Pathologic variables and recurrence rates as related to obesity and race in men with prostate cancer undergoing radical prostatectomy. J Clin Oncol. 2004;22:439–445. doi: 10.1200/JCO.2004.03.132. [DOI] [PubMed] [Google Scholar]
- 33.Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 34.Stephenson AJ, Scardino PT, Eastham JA, et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst. 2006;98:715–717. doi: 10.1093/jnci/djj190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vickers AJ, Bianco FJ, Serio AM, et al. The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst. 2007;99:1171–1177. doi: 10.1093/jnci/djm060. [DOI] [PubMed] [Google Scholar]
- 36.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate cancer survivors. N Engl J Med. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]