Abstract
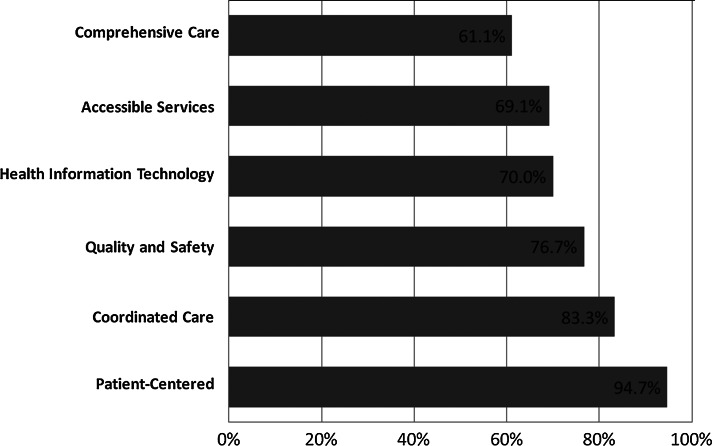
The patient-centered medical home (PCMH) has been introduced as a model for providing high-quality, comprehensive, patient-centered care that is both accessible and coordinated, and may provide a framework for optimizing the care of youth living with HIV (YLH). We surveyed six pediatric/adolescent HIV clinics caring for 578 patients (median age 19 years, 51% male, and 82% black) in July 2011 to assess conformity to the PCMH. Clinics completed a 50-item survey covering the six domains of the PCMH: (1) comprehensive care, (2) patient-centered care, (3) coordinated care, (4) accessible services, (5) quality and safety, and (6) health information technology. To determine conformity to the PCMH, a novel point-based scoring system was devised. Points were tabulated across clinics by domain to obtain an aggregate assessment of PCMH conformity. All six clinics responded. Overall, clinics attained a mean 75.8% [95% CI, 63.3–88.3%] on PCMH measures—scoring highest on patient-centered care (94.7%), coordinated care (83.3%), and quality and safety measures (76.7%), and lowest on health information technology (70.0%), accessible services (69.1%), and comprehensive care (61.1%). Clinics moderately conformed to the PCMH model. Areas for improvement include access to care, comprehensive care, and health information technology. Future studies are warranted to determine whether greater clinic PCMH conformity improves clinical outcomes and cost savings for YLH.
Introduction
The United States health care system faces significant challenges in providing consistent high quality care.1–3 To align local, state, and national efforts to improve health care quality, the U.S. Department of Health and Human Services released the first-ever National Quality Strategy (NQS). The NQS has identified three aims for improving health care quality: (1) better care—by making health care patient-centered, reliable, accessible, and safe; (2) healthy people and communities—by supporting proven interventions to address behavioral, social, and environmental determinants of health; and (3) affordable care—by reducing the cost of quality health care for individuals, families, employers, and government.4 The patient-centered medical home (PCMH) is one care delivery model capable of advancing the NQS goals.
The PCMH model seeks to provide high-quality, comprehensive, patient-centered care that is both accessible and coordinated.5–7 Studies demonstrate that clinics designated as PCMHs improve clinical quality and patient experiences, while simultaneously reducing emergency and inpatient service utilization and health care costs.8–12 This care model is particularly suited for the management of people with HIV infection, with recent studies describing the benefits of the PCMH model in managing warfarin therapy and treating depression.13,14
Young people (ages 13–24 years) in the U.S. are disproportionately affected by HIV, accounting for approximately 20% of all new HIV infections in 2009.15 Between 2006 and 2009, adolescent/young adult black men who have sex with men (MSM) were the only risk group in the U.S. to experience an increase in new HIV infections.16 Additionally, there is a cohort of perinatally HIV-infected children that have exceeded their initial survival expectations and are now emerging into adolescence and young adulthood.17 Both populations are seen at pediatric/adolescent HIV clinics, which often see patients through the age of 24 years. As the number of youth living with HIV (YLH) continues to grow, engagement in primary HIV care becomes paramount to improving patient outcomes and decreasing HIV transmission in the community.18–25 However, little is known about the delivery of outpatient care to HIV-infected youth, namely (1) the structures of pediatric/adolescent HIV clinics and (2) conformity to the PCMH model. Our study aimed to document key organizational features of medical care delivery in high-volume pediatric/adolescent HIV clinics in the U.S., with a focus on identifying essential components of the PCMH. New knowledge generated from this evaluation is intended to improve the organizational structure and delivery of quality care in outpatient pediatric/adolescent HIV clinics.
Methods
Study design and participants
We conducted a cross-sectional survey of medical directors of pediatric/adolescent HIV clinics affiliated with the HIV Research Network (HIVRN). The HIVRN is a consortium of 18 clinics that provide primary and subspecialty care to HIV-infected patients.26 It is sponsored by the Agency for Healthcare Research and Quality (AHRQ). Six clinics exclusively treat pediatric and adolescent patients, located in urban cities in the Northeastern (2), Southern (1), Midwestern (1), and Western (2) United States. These clinics cared for 578 patients in 2011, with a median number of 69 patients per clinic (range, 31–267). Most patients were of minority race/ethnicity (86%), had vertical/perinatal transmission as an HIV risk factor (64%), and had either Medicaid or no health insurance (76%). Median age was 19 years, with roughly equal proportions of males and females. Over 80% of patients were receiving antiretroviral therapy (ART), with a median CD4 cell count of 640 cells/mm3 (Table 1). The study was approved by the Institutional Review Board at the Johns Hopkins School of Medicine and at each participating site.
Table 1.
Demographic and Clinical Characteristics of Pediatric/Adolescent Patients in Surveyed Clinics
| Variable | 2011 N=578 (%) |
|---|---|
| Age, median (years) | 19 |
| Gender | |
| Female | 286 (49) |
| Male | 292 (51) |
| Race/ethnicity | |
| White | 66 (11) |
| Black | 475 (82) |
| Hispanic | 24 (4) |
| Other | 13 (2) |
| HIV transmission risk factor | |
| Vertical/perinatal | 371 (64) |
| Transfusion/blood product | 5 (1) |
| MSM | 107 (19) |
| HET | 87 (14) |
| CD4 count (cells/mm3) | |
| Median | 640 |
| ≤50 | 13 (2) |
| 51–200 | 26 (5) |
| 201–500 | 153 (26) |
| >501 | 386 (67) |
| HIV-1 RNA (copies/mL) | |
| Median | 50 |
| ≤400 | 360 (62) |
| 401–1000 | 29 (5) |
| 1001–10,000 | 86 (15) |
| 10,001–100,000 | 55 (10) |
| >100,000 | 13 (2) |
| Missing | 35 (6) |
| HAART receipt | |
| No | 91 (16) |
| Yes | 487 (84) |
| Insurance | |
| Private | 113 (20) |
| Medicaid | 334 (58) |
| Medicare | 14 (2) |
| None/Ryan White | 105 (18) |
| Other/unknown | 12 (2) |
Data collection
A structured questionnaire was sent to all pediatric/adolescent HIVRN medical directors in July 2011 and data were collected from July to October 2011. Medical directors were encouraged to consult with key clinic informants (e.g., clinicians, case managers, nursing staff, and front desk personnel) when completing the questionnaire and were instructed to answer each question using objective clinical data or to use best estimates if clinical information was not available. Missing or problematic responses were identified, reviewed with the site, and corrected. This process assured that complete questionnaire data was obtained from each site.
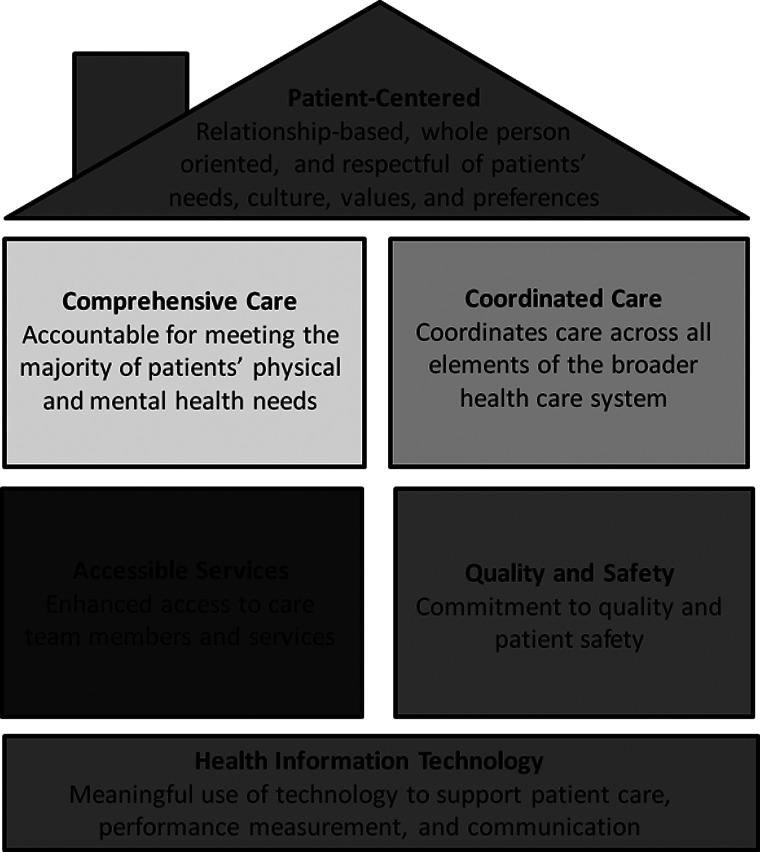
The survey contained 50 items covering provider characteristics, patient adherence to care, and the six PCMH domains: (1) comprehensive care, (2) patient-centered care, (3) coordinated care, (4) accessible services, (5) quality and safety, and (6) health information technology (HIT). Domains were based on the functions and attributes of the medical home as identified by AHRQ6 (Fig. 1). Fifteen items required a numerical answer, 10 were dichotomous yes/no questions, and 25 asked for descriptive statements.
FIG. 1.
Components of the Patient-Centered Medical Home.
Measures
Provider characteristics were ascertained by asking: (1) how many primary care providers work in your clinic; (2) how many half-day sessions per week does your clinic run; (3) how many providers work per half day session; (4) what is the distribution of providers (attending levels physicians, physician trainees, nurse practitioners [NPs], physician assistants [PAs], others); (5) how many patients is each provider scheduled per half day session; (6) how long are new and established patient appointments for each provider type; and (7) what is the average panel size per provider. Five questions were devoted to patient adherence to care covering loss to follow-up (how do you define loss to follow-up, what is your loss to follow-up rate each year) and retention in care (what is the appointment no-show rate for all, new patients, and established patients per month).
Comprehensive care was evaluated by asking sites to identify the availability of onsite medical consult services (i.e., located on the same medical campus), including psychiatry, gynecology, dermatology, colposcopy, hepatology, neurology, ophthalmology, gastroenterology, dental, and oncology. Additionally, clinics were asked about availability of case management, substance abuse counseling, clinical pharmacy, family planning, nutrition, language translation, and housing/transportation services. Delivery of patient-centered care was determined by inquiring about the presence of HIV educational programs and how patients and their families are involved in establishing care plans.
Seven questions related to coordinated care, focusing on inpatient–outpatient, primary–subspecialty, and pediatric–adult care coordination. Inpatient–outpatient coordination was determined by asking: (1) what procedures are in place to notify clinical staff if a patient has been hospitalized; and (2) are records routinely obtained after hospitalization at outside hospitals. Primary care/subspecialty care coordination questions were: (1) what procedures are used to coordinate care between HIV clinic staff and providers in other subspecialty areas; (2) do providers in different clinics have access to the same medical record; and (3) are patients with non-HIV-related co-morbidities frequently referred to providers in other subspecialty areas within the same clinic, same hospital, different clinic, or to an outside facility. Finally, to assess pediatric–adult care coordination, we asked respondents if they had a formally established program for transitioning patients from pediatric to adult clinics and if they had an adult HIV clinic located at the same institution.
Structures designed to improve the accessibility of services were assessed by asking each medical director how urgent clinical problems are handled during the day, at night, and on weekends. In addition, clinics were asked if they have a walk-in policy, offer same day urgent appointments, utilize group visits (e.g., siblings seen together), provide online patient services (e.g., access to medical records, appointment scheduling, and provider electronic messaging), and if laboratory results/clinical data are highly accessible to patients. Wait times were evaluated by asking clinics how long is the average wait for a new appointment, routine follow-up appointment, and the average time spent in the waiting room prior to scheduled visits.
Patient safety and quality of care practices were determined by inquiring about the presence of a clinic policy/procedure to: (1) promptly identify and respond to critical laboratory results; (2) screen for adverse drug interactions; (3) engage patients who missed appointments; (4) monitor quality of care; (5) and to collect patient satisfaction data. Health information technology was assessed by asking about the availability and use of electronic medical records (EMR), electronic prescribing, and point of care medical decision tools (e.g., assistance with drug dosing, and screening and preventative care reminders). Medical directors were queried about the use of mobile phone short message service (SMS) to communicate with patients and if their practice maintained a clinic website.
Data analyses
To assess conformity to the PCMH model, we developed a novel point-based scoring system. Each item (excluding provider characteristics and patient adherence to care) was assigned one point, for a possible 28 total points. Comprehensive care points were allocated as follows: one point for the availability of key medical services (psychiatry and gynecology), one point for ≥3 additional medical services (dermatology, colposcopy, hepatology, neurology, ophthalmology, gastroenterology, dental, or oncology), and one point for providing the following ancillary services: case management, substance abuse counseling, clinical pharmacy, family planning, nutrition, language translation, and housing/transportation services. For survey items requiring a numerical answer, wait time to schedule new and established patient appointments and time spent in the waiting room, we assigned one point for values ≤14 days, ≤7 days, and ≤20 min, respectively. For survey items requiring descriptive responses, two reviewers independently evaluated each response to determine if a point should be assigned. Any discrepancies between the reviewers were resolved by consensus. Points were tabulated across clinics by domain to obtain an aggregate assessment of PCMH conformity.
Results
All six pediatric/adolescent HIV clinics completed the questionnaire. The median number of providers working in each clinic was 5 (range, 1–10). Nearly all physicians were pediatricians (96.6%), with approximately half (49.0%) specializing in infectious diseases. Five of six clinics utilized NPs. Clinics ran a median of six half-day sessions per week (range, 1–10). Attending physicians had higher patient volumes per half-day session and shorter new patient appointment length compared to NPs. Specifically, median patient volume per half-day session was 6 (range, 2–8) for attending physicians and 4 (range, 1–10) for NPs. Attending physicians had a median appointment length of 53 min (range, 30–60) for new patients and 30 min (range, 20–60) for established patients. NPs had a median appointment length of 60 min (range, 45–90) for new patients and 30 min (range, 30–60) for established patients. The median no-show rate for clinic appointments was 22.0% (range, 5.5–42.0%), with median no-show rates for new patients at 10.0% (range, 0–30.0%) and median no-show rate for established patients at 23.0% (range, 5.5–58.0%).
Overall, clinics attained a mean 75.8% [95% CI, 63.3–88.3%] on PCMH measures—scoring highest on patient-centered care (94.4%), coordinated care (83.3%), and quality and safety measures (76.7%), and lowest on comprehensive care (61.1%), accessible services (69.1%), and health information technology (70.0%) (Fig. 2). Clinics performed best in the patient-centered care domain. Five out of six clinics offered educational programs to patients and their families, including HIV-specific support groups, psycho-educational programs, life skills classes, and HIV prevention/treatment adherence training; half of clinics partnered with local organization (e.g., AIDS Education and Training Centers) to facilitate the delivery of these education and training programs. All sites had a procedure for ensuring that patients and their families are actively involved in establishing care plans. This involved providers openly discussing options and alternatives, soliciting patient/caregiver comments, addressing any concerns, and ultimately making mutually agreed upon medical decisions.
FIG. 2.
Pediatric/adolescent HIV clinics conformity to the Patient-Centered Medical Home model.
Care was effectively coordinated across different health settings and between providers in our sample of clinics. All clinics have protocols in place that require notification of outpatient team members when patients are admitted to their home hospital, but have to rely on patients, family members, and other health providers if a patient is hospitalized at an outside facility. Most clinics (66.7%) routinely obtain records for hospitalizations occurring at outside institutions. To coordinate care with subspecialty providers, 83.3% of sites utilize an EMR which can be accessed by all providers within their health care system. In addition, clinics communicate with specialists via email, telephone, and by carbon copying providers on clinical documents. Almost all clinics (83.3%) have a designated program to help patients transition from pediatric/adolescent to adult care and five sites have an adult HIV clinic on the same medical campus.
Surveyed clinics had a number of established patient safety and quality assurance procedures. Nearly all clinics have policies to identify and respond to critical laboratory results (83.3%), monitor for adverse drug interactions (66.7%), and collect patient satisfaction data (66.7%). In addition, 83.3% of clinics have quality improvement programs, with the majority meeting monthly to quarterly to formally review data and make recommendations. Five of six clinics actively monitor patients who miss appointments and have specific programs to improve patient engagement in care. The reported patient loss to follow-up rate per year is <5% for most clinics with a designated engagement in care initiative (four of five clinics).
Only 61.1% of comprehensive care measures were met. All clinics provided patients with access to key medical services (psychiatry and gynecology) and half had three or more additional medical services (dermatology, colposcopy, hepatology, neurology, ophthalmology, gastroenterology, dental, or oncology) on location. Only two clinics (33.3%) offered all seven ancillary services (case management, substance abuse counseling, clinical pharmacy, family planning, nutrition, language translation, and housing/transportation services).
Clinics provided enhanced access to care, team members, and services in a variety of manners, including same-day appointments, walk-in appointments, referral to emergency departments, and by on-call providers. During the day, all clinics provide same-day appointments and 66.7% have a walk-in policy. For urgent problems at night and on weekends, 66.7% of the clinics refer patients to on-call providers, while the remaining clinics direct patients to emergency departments. The median wait time to schedule a clinic appointment was 4 days (range, 1–14) for new patients, and 7 days (range, 0–14) for return/established patients. Median waiting room time is 22.5 min (range, 5–45). In addition, few clinics (33.3%) use group visits, and when they do it is in the context of family visits. Only 33.3% of clinics offer online patient services, such as appointment scheduling, access to medical records, and provider electronic messaging.
Health information technology was moderately used by clinics, with 70.0% of HIT measures successfully attained. All sites utilize EMR systems, with half additionally using HIV specific point of care medical decision tools. Most sites (83.3%) have both electronic prescribing and use mobile phone short message service (SMS) messaging to communicate with patients. Two sites specifically used SMS messaging to improve ART adherence. Only a third of clinics have a practice website, which allow patients and their families' electronic access to medical records, appointment scheduling, and electronic communication with the care team.
Discussion
This study is among the first to document the organizational characteristics of pediatric/adolescent HIV clinics and notes that surveyed clinics moderately conformed to the PCMH model. Clinics excelled in providing coordinated, high quality, patient-centered care, but demonstrated weaknesses in offering comprehensive, accessible care, and in meaningfully using health information technology. Examining these lower scoring domains may offer insights into how clinics can improve the care and outcomes of HIV-infected youth.
Receipt of ancillary services, including case management, outreach services, and supportive counseling, is associated with retention of YLH in care.27,28 In adults, utilization of ancillary services has been linked to higher rates of ART receipt and retention in care, cessation of substance use, entry into stable housing, and improvements in quality of life.29–31 Despite these known benefits, only 83.3% of surveyed clinics offered case management and nutrition services, 66.7% had substance abuse counseling and clinical pharmacy, and less than half provided all measured ancillary services. YLH are in particular need of these services. Factors contributing to young people contracting HIV, such as being homeless/runaway, mental health illness, substance abuse, or being involved in sex for money, additionally serve as barriers to receiving adequate health care and achieving good health outcomes.28,32–34 Case management and other ancillary services play a critical role in helping youth and young adults overcome these barriers and receive needed care.
High no-show rates at surveyed sites may compromise the quality of care delivered and provider productivity. Dietz and colleagues prospectively examined appointment adherence in 178 HIV-infected female youth in five U.S. cities, noting that participants only attended 67.3% of scheduled visits;35 this is similar to adult rates which range from 71% to 75%.36 The behavioral model of health service utilization provides a framework for understanding how patient factors (coping skills, motivation to attend visits, social support, provider attitudes/trust, co-morbid conditions) and health system factors (convenience of clinic hours, appointment waiting time, ease/comfort of the outpatient process) jointly affect health seeking behavior (linkage to and retention in care).19,37–39 The PCMH model makes efforts to reduce health system barriers to care by providing enhanced access to providers and services. However, in our clinics, only 66.7% managed urgent patient issues by using a walk-in policy during the day and referring patients to an on-call provider at night and on weekends; implementation of these and other procedures to handle acute patient issues has been shown to decreased emergency department utilization.40,41 In addition, the PCMH model may serve as the ideal platform for implementing interventions to increase linkage and adherence to HIV care, including patient navigation, peer mentorship, and IMB (informational, motivational, behavioral skills) programs.42–44
Numerous studies record the positive benefits of advanced access scheduling on patient outcomes.45–48 Advanced access scheduling allows patients to schedule appointments with their provider at times of their choosing, typically on the same day or within 24 h of calling. In a systemic review of 24 studies evaluating advanced access scheduling outcomes, Rose et al. documented a reduction in no-show rates and neutral to positive improvement in patient satisfaction.45 While all clinics were able to schedule new patients within 14 days, only half provided established patients with an appointment within 1 week. Reducing the lead time to scheduling appointments may be particularly important to some YLH, whose lack of familiarity with the health system, denial of need for care, distrust of adults and professional agencies, and transportation difficulties may result in reduce clinic attendance.33,49
It is hoped that integrating HIT into the PCMH will go beyond the electronic medical record, holding promise for enhancing quality and safety of care, care coordination, and scheduling. Electronic prescribing and point of care medical decision tools can reduce medication errors, facilitate recommended diagnostic and treatment ordering, and increase preventive care services.50,51 Electronic prescribing is utilized at almost all sites (83.3%), but HIV-specific clinical decision tools were only present in half of clinics. Providers caring for YLH may value electronic prescriptions, which may assist in calculating weight or age-base dosing.52 The effect of clinical decision support systems on HIV outcomes has not been evaluated in either pediatric or adult populations, but is shown to improve health care process measures in other chronic diseases including cardiovascular disease, diabetes, and asthma.51 Future studies are needed to determine how implementation of such systems can be used to improve care and outcomes for YLH.
Emerging data suggest that text messaging improves adherence to ART and reduces virologic failure in people with HIV infection.53,54 Among a cohort of HIV-infected youth and young adults (ages 14–29 years), receipt of personalized daily SMS reminders statistically improved self-reported adherence over a 24-week period.54 Clinics should consider harnessing the benefits of SMS reminders to improve treatment and outpatient appointment adherence for youth. To determine the prevalence of social networking among people living with HIV, Horvath and colleagues surveyed 312 U.S. HIV-infected adults and noted that 76% used social networking websites/features at least once a week.55 This percentage is likely to underestimate the true penetration in YLH, who like other adolescents and young adults, are more likely to integrate technology into their daily lives than older adults. The potential of social networking to address medical and psychosocial needs of YLH is great. However, less than half of all clinics maintain a practice website. As technology advances, providers, public health practitioners, and health systems should actively explore how new technologies can be used to improve HIV prevention, treatment, and care.
This study has several limitations. First, although respondents used objective data when available, some responses were best estimates and could be affected by recall or good performance biases. Our study sites, though located in areas where the epidemic among youth is largely situated, are not nationally representative and may not generalize to all pediatric/adolescent clinics. In addition, there are no standard criteria for assessing compliance with the PCMH, as such we developed questions and a points system based on a review of the literature and previous HIVRN data. We did not assess patient outcomes (e.g., decreases in HIV-1 RNA, increases in CD4 cell count); future studies are needed to assess how conformity with PCMH principles influences patient immunologic and virologic outcomes. Implementation research exploring how to effectively build a PCMH and studies examining local and regional barriers to implementation are also needed to assist clinics seeking to become a PCMH.
In conclusion, pediatric/adolescent HIVRN clinics moderately conformed to the PCMH model using a novel measure of PCMH adoption; scoring highest on patient-centered care, coordinated care, and quality and safety measures, and lowest on comprehensive care, accessible services, and health information technology. This new PCMH assessment, specifically tailored to pediatric/adolescent HIV clinics, may help clinics identify areas of weakness and assist in targeting resources to improve the organizational structure and delivery of quality care. Adapting structures and processes of care consistent with the PCMH model may serve as one mechanism for improving the quality of care delivery to HIV-infected youth and young adults.
Acknowledgments
Funding/Support: This study was supported by the Agency for Healthcare Research and Quality (AHRQ) (290-01-0012). BRY was supported by the National Institutes of Health/Institute of Mental Health (K23-MH-097647-01A1).
Sponsoring Agencies: Agency for Healthcare Research and Quality, Rockville, Maryland (Fred Hellinger, PhD; John Fleishman, PhD; Irene Fraser, PhD); Health Resources and Services Administration, Rockville, Maryland (Robert Mills, PhD, Faye Malitz, MS). The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Data Coordinating Center: Johns Hopkins University (Richard Moore, MD, Jeanne Keruly, CRNP, Kelly Gebo, MD, Cindy Voss, MA, Nikki Balding, MS).
HIV Research Network Participating Sites: Alameda County Medical Center, Oakland, California (Howard Edelstein, MD); Children's Hospital of Philadelphia, Philadelphia, Pennsylvania (Richard Rutstein, MD); Community Health Network, Rochester, New York (Roberto Corales, DO); Drexel University, Philadelphia, Pennsylvania (Sara Allen, CRNP, Jeffrey Jacobson, MD); Fenway Health, Boston, Massachusetts (Stephen Boswell, MD); Johns Hopkins University, Baltimore, Maryland (Allison Agwu MD, Kelly Gebo, MD, Richard Moore, MD); Montefiore Medical Group, Bronx, New York (Robert Beil, MD, Carolyn Chu, MD); Montefiore Medical Center, Bronx, New York (Lawrence Hanau, MD); Oregon Health and Science University, Portland, Oregon (P. Todd Korthuis, MD); Parkland Health and Hospital System, Dallas, Texas (Muhammad Akbar, MD, Laura Armas-Kolostroubis, MD); St. Jude's Children's Hospital and University of Tennessee, Memphis, Tennessee (Aditya Gaur, MD); St. Luke's Roosevelt Hospital Center, New York, New York (Stephen Arpadi, MD, Victoria Sharp, MD); Tampa General Health Care, Tampa, Florida (Charurut Somboonwit, MD); University of California, San Diego, California (W. Christopher Mathews, MD); Wayne State University, Detroit, Michigan (Jonathan Cohn, MD).
Author Disclosure Statement
All authors have no potential conflicts of interests.
References
- 1.Kohn LT CJ, editor; Donaldson MS, editor. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.McGlynn EA. Asch SM. Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 3.Ostbye T. Yarnall KS. Krause KM. Pollak KI. Gradison M. Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3:209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services. National Quality Strategy 2011. http://www.healthcare.gov/law/resources/reports/quality03212011a.html#es. [Nov 19;2012 ]. http://www.healthcare.gov/law/resources/reports/quality03212011a.html#es
- 5.American Academy of Family Physicians (AAFP) American Academy of Pediatrics (AAP), American American College of Physicians (ACP), American Osteopathic Association (AOA). Joint Principles of the Patient-Centered Medical Home. http://www.acponline.org/running_practice/pcmh/demonstrations/jointprinc_05_17.pdf. [Nov 5;2012 ]. http://www.acponline.org/running_practice/pcmh/demonstrations/jointprinc_05_17.pdf
- 6.Agency for Health Care Research and Quality. Patient Centered Medical Home. http://www.pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483. [Nov 19;2012 ]. http://www.pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483
- 7.Berenson RA. Hammons T. Gans DN, et al. A house is not a home: Keeping patients at the center of practice redesign. Health Aff. 2008;27:1219–1230. doi: 10.1377/hlthaff.27.5.1219. [DOI] [PubMed] [Google Scholar]
- 8.Reid RJ. Coleman K. Johnson EA, et al. The group health medical home at year two: Cost savings, higher patient satisfaction, and less burnout for providers. Health Aff. 2010;29:835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 9.Coleman K. Reid RJ. Johnson E, et al. Implications of reassigning patients for the medical home: A case study. Ann Fam Med. 2010;8:493–498. doi: 10.1370/afm.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Counsell SR. Callahan CM. Clark DO, et al. Geriatric care management for low-income seniors: A randomized controlled trial. JAMA. 2007;298:2623–2633. doi: 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- 11.Dorr DA. Wilcox AB. Brunker CP. Burdon RE. Donnelly SM. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. J Am Geriatr Soc. 2008;56:2195–2202. doi: 10.1111/j.1532-5415.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- 12.Grumbach K. Grundy P. The Outcomes of Implementing Patient-Centered Medical Home Interventions: A Review of the Evidence on Quality, Access and Costs from Recent Prospective Evaluation Studies. Washington, D.C.: Patient-Centered Primary Care Collaborative; Aug, 2009. 2009. [Google Scholar]
- 13.Anderson AM. Chane T. Patel M, et al. Warfarin therapy in the HIV medical home model: Low rates of therapeutic anticoagulation despite adherence and differences in dosing based on specific antiretrovirals. AIDS Patient Care STDS. 2012;26:454–462. doi: 10.1089/apc.2012.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams JL. Gaynes BN. McGuinness T, et al. Treating depression within the HIV "medical home": A guided algorithm for antidepressant management by HIV clinicians. AIDS Patient Care STDS. 2012;26:647–654. doi: 10.1089/apc.2012.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. HIV Among Youth. 2011. http://www.cdc.gov/hiv/youth/pdf/youth.pdf. [Nov 19;2012 ]. http://www.cdc.gov/hiv/youth/pdf/youth.pdf
- 16.Prejean J. Song R. Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hazra R. Siberry GK. Mofenson LM. Growing up with HIV: Children, adolescents, and young adults with perinatally acquired HIV infection. Annu Rev Med. 2010;61:169–185. doi: 10.1146/annurev.med.050108.151127. [DOI] [PubMed] [Google Scholar]
- 18.Mugavero MJ. Improving engagement in HIV care: What can we do? Top HIV Med. 2008;16:156–161. [PubMed] [Google Scholar]
- 19.Ulett KB. Willig JH. Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23:41–49. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berg MB. Safren SA. Mimiaga MJ. Grasso C. Boswell S. Mayer KH. Nonadherence to medical appointments is associated with increased plasma HIV RNA and decreased CD4 cell counts in a community-based HIV primary care clinic. AIDS Care. 2005;17:902–907. doi: 10.1080/09540120500101658. [DOI] [PubMed] [Google Scholar]
- 21.Lucas GM. Chaisson RE. Moore RD. Highly active antiretroviral therapy in a large urban clinic: Risk factors for virologic failure and adverse drug reactions. Ann Intern Med. 1999;131:81–87. doi: 10.7326/0003-4819-131-2-199907200-00002. [DOI] [PubMed] [Google Scholar]
- 22.Sethi AK. Celentano DD. Gange SJ. Moore RD. Gallant JE. Association between adherence to antiretroviral therapy and human immunodeficiency virus drug resistance. Clin Infect Dis. 2003;37:1112–1118. doi: 10.1086/378301. [DOI] [PubMed] [Google Scholar]
- 23.Giordano TP. Gifford AL. White AC, Jr., et al. Retention in care: A challenge to survival with HIV infection. Clin Infect Dis. 2007;44:1493–1499. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 24.Mugavero MJ. Lin HY. Willig JH, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009;48:248–256. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Metsch LR. Pereyra M. Messinger S, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis. 2008;47:577–584. doi: 10.1086/590153. [DOI] [PubMed] [Google Scholar]
- 26.Yehia BR. Gebo KA. Hicks PB, et al. Structures of care in the clinics of the HIV Research Network. AIDS Patient Care STDS. 2008;22:1007–1013. doi: 10.1089/apc.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naar-King S. Green M. Wright K. Outlaw A. Wang B. Liu H. Ancillary services and retention of youth in HIV care. AIDS Care. 2007;19:248–251. doi: 10.1080/09540120600726958. [DOI] [PubMed] [Google Scholar]
- 28.Harris SK. Samples CL. Keenan PM. Fox DJ. Melchiono MW. Woods ER. Outreach, mental health, and case management services: Can they help to retain HIV-positive and at-risk youth and young adults in care? Matern Child Health J. 2003;7:205–218. doi: 10.1023/a:1027386800567. [DOI] [PubMed] [Google Scholar]
- 29.Chin JJ. Botsko M. Behar E. Finkelstein R. More than ancillary: HIV social services, intermediate outcomes and quality of life. AIDS Care. 2009;21:1289–1297. doi: 10.1080/09540120902732019. [DOI] [PubMed] [Google Scholar]
- 30.Lo W. MacGovern T. Bradford J. Association of ancillary services with primary care utilization and retention for patients with HIV/AIDS. AIDS Care. 2002;14(Suppl 1):S45–S57. doi: 10.1080/0954012022014992049984. [DOI] [PubMed] [Google Scholar]
- 31.Messeri PA. Abramson DM. Aidala AA. Lee F. Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002;14(Suppl 1):S15–S29. doi: 10.1080/09540120220149948. [DOI] [PubMed] [Google Scholar]
- 32.Brady RE. Singer B. Marconi KM. Special Projects of National Significance Program: Ten models of adolescent HIV care. J Adolescent Health. 1998;23:1–4. [PubMed] [Google Scholar]
- 33.Geber GM. Barriers to health care for street youth. J Adolescent Health. 1997;21:287–290. doi: 10.1016/S1054-139X(97)00111-0. [DOI] [PubMed] [Google Scholar]
- 34.Klein JD. Adolescents, health services, and access to care. J Adolescent Health. 2000;27:293–294. doi: 10.1016/s1054-139x(00)00187-7. [DOI] [PubMed] [Google Scholar]
- 35.Dietz E. Clum GA. Chung SE, et al. Adherence to scheduled appointments among HIV-infected female youth in five U.S. cities. J Adolescent Health. 2010;46:278–283. doi: 10.1016/j.jadohealth.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yehia BR. Fleishman JA. Metlay JP, et al. Comparing different measures of retention in outpatient HIV care. AIDS. 2012;26:1131–1139. doi: 10.1097/QAD.0b013e3283528afa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Outlaw A. Naar-King S. Green-Jones M, et al. Brief report: Predictors of optimal HIV appointment adherence in minority youth: A prospective study. J Pediatr Psychol. 2010;35:1011–1015. doi: 10.1093/jpepsy/jsq002. [DOI] [PubMed] [Google Scholar]
- 38.Christopoulos KA. Das M. Colfax GN. Linkage and retention in HIV care among men who have sex with men in the United States. Clin Infect Dis. 2011;52:S214–S222. doi: 10.1093/cid/ciq045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yehia BR. Kangovi S. Frank I. Patients in transition: Avoiding detours on the road to HIV treatment success. AIDS. 2013 Feb 21; doi: 10.1097/QAD.0b013e328360104e. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 40.Markson LE. Houchens R. Fanning TR. Turner BJ. Repeated emergency department use by HIV-infected persons: Effect of clinic accessibility and expertise in HIV care. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:35–41. doi: 10.1097/00042560-199801010-00005. [DOI] [PubMed] [Google Scholar]
- 41.Mauskopf J. Turner BJ. Markson LE. Houchens RL. Fanning TR. McKee L. Patterns of ambulatory care for AIDS patients, and association with emergency room use. Health Serv Res. 1994;29:489–510. [PMC free article] [PubMed] [Google Scholar]
- 42.Bradford JB. Coleman S. Cunningham W. HIV System Navigation: An emerging model to improve HIV care access. AIDS Patient Care STDS. 2007;21:S49–S58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 43.Cully JA. Mignogna J. Stanley MA, et al. Development and pilot testing of a standardized training program for a patient-mentoring intervention to increase adherence to outpatient HIV care. AIDS Patient Care STDS. 2012;26:165–172. doi: 10.1089/apc.2011.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith LR. Fisher JD. Cunningham CO. Amico KR. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDS. 2012;26:344–355. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rose KD. Ross JS. Horwitz LI. Advanced access scheduling outcomes: A systematic review. Arch Intern Med. 2011;171:1150–1159. doi: 10.1001/archinternmed.2011.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murray M. Berwick DM. Advanced access: Reducing waiting and delays in primary care. JAMA. 2003;289:1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 47.Bundy DG. Randolph GD. Murray M. Anderson J. Margolis PA. Open access in primary care: Results of a North Carolina pilot project. Pediatrics. 2005;116:82–87. doi: 10.1542/peds.2004-2573. [DOI] [PubMed] [Google Scholar]
- 48.Solberg LI. Crain AL. Sperl-Hillen JM. Hroscikoski MC. Engebretson KI. O'Connor PJ. Effect of improved primary care access on quality of depression care. Ann Fam Med. 2006;4:69–74. doi: 10.1370/afm.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blum RW. McNeely C. Nonnemaker J. Vulnerability, risk, and protection. J Adolescent Health. 2002;31:28–39. doi: 10.1016/s1054-139x(02)00411-1. [DOI] [PubMed] [Google Scholar]
- 50.Ammenwerth E. Schnell-Inderst P. Machan C. Siebert U. The effect of electronic prescribing on medication errors and adverse drug events: A systematic review. JAMIA. 2008;15:585–600. doi: 10.1197/jamia.M2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bright TJ. Wong A. Dhurjati R, et al. Effect of cinical decision-support systems: A systematic review. Ann Intern Med. 2012;157:29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 52.Caldwell NA. Prescribing for children. Int Emerg Nurs. 2011;19:168–172. doi: 10.1016/j.ienj.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 53.Ammassari A. Trotta MP. Shalev N, et al. Timed short messaging service improves adherence and virological outcomes in HIV-1-infected patients with suboptimal adherence to antiretroviral therapy. JAIDS. 2011;58:e113–115. doi: 10.1097/QAI.0b013e3182359d2a. [DOI] [PubMed] [Google Scholar]
- 54.Dowshen N. Kuhns LM. Johnson A. Holoyda BJ. Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: A pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14:e51. doi: 10.2196/jmir.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Horvath KJ. Danilenko GP. Williams ML, et al. Technology use and reasons to participate in social networking health websites among people living with HIV in the US. AIDS Behav. 2012;16:900–910. doi: 10.1007/s10461-012-0164-7. [DOI] [PMC free article] [PubMed] [Google Scholar]