Abstract
Purpose
Mounting evidence shows that low birth weight and prematurity are related to serious health problems in adulthood, including increased body fat, decreased fitness, poor bone mineralization, pulmonary problems, and cardiovascular disease. There is data to suggest that increasing physical activity in preterm infants will have effects on short term muscle mass and fat mass, but we also hypothesized that increasing physical activity early in life can lead to improved health outcomes in adulthood. Because few studies have addressed the augmentation of physical activity in premature babies, the objective of this study was to evaluate the feasibility of whether caregivers (mostly mothers) can learn from nurses and other health care providers to implement a program of assisted infant exercise following discharge.
Study Design and Methods
Ten caregivers of preterm infants were taught by nurses, along with occupational therapists and other health care providers, to perform assisted infant exercise and instructed to conduct the exercises daily for approximately three weeks. The researchers made home visits and conducted qualitative interviews to understand the caregivers’ (mostly mothers’) experiences with this exercise protocol. Quantitative data included a caregiver’s daily log of the exercises completed to measure adherence as well as videotaped caregiver sessions, which were used to record errors as a measure of proficiency in the exercise technique.
Results
On average, the caregivers completed a daily log on 92% of the days enrolled in the study and reported performing the exercises on 93% of the days recorded. Caregivers made an average of 1.8 errors on two tests (with a maximum of 23 or 35 items on each, respectively) when demonstrating proficiency in the exercise technique. All caregivers described the exercises as beneficial for their infants, and many reported that these interventions fostered increased bonding with their babies. Nearly all reported feeling “scared” of hurting their babies during the first few days of home exercise, but stated that fears were alleviated by practice in the home and further teaching and learning.
Clinical Implications
Caregivers were willing and able to do the exercises correctly, and they expressed a belief that the intervention had positive effects on their babies and on caregiver-infant interactions. These findings have important implications for nursing practice because nurses are in key positions to teach and encourage caregivers to practice these exercises with their newborn babies.
Nurses are in pivotal roles to provide teaching to parents in the NICU. As parents anticipate and prepare for the discharge of their neonate to home, they often have much trepidation and fear, despite their excitement about bringing their infant home. Melynk, Bullock, McGrath, Jacobson, Kelly, and Baba (2010) suggested using evidence-based practice nurse mentors whose primary role is to assist nurses in teaching parents how to gain confidence in caring for their infants while in the NICU, using the Creating Opportunities for Personal Empowerment (COPE) program. The nurse’s role in teaching parents about caring for their infant provides important background for our study. Schlittenhart, Smart, Miller, and Severtson (2011) noted that parents often view their babies as fragile, being afraid to even touch them until their confidence in themselves as caregivers grows. Our previous study (Gravem, Lakes, Teran, Rich, Cooper, Olshansky, 2009) corroborated this perception that parents had of their infants, although with encouragement from nurses and other health professionals (occupational therapists, physical therapists), parents were able to more confidently touch and interact with their babies.
Nurses have been described as the “primary source of information” for parents in the NICU (Kowalski, Leef, Mackley, Spear, Paul, 2006, p. 48). A major reason that nurses are central to effective teaching of new parents is that the parents find the nurses to be nurturing, embracing the psychosocial aspects of communication with parents (Jones, Woodhouse, Rowe, 2007). McKechnie and Pridham (2012) emphasized that effective communication between parents and health care providers (nurses) must include a high level of understanding of the emotional responses of parents. In the present study, we examine the feasibility of teaching caregivers (mothers) how to perform assisted exercise with their newborns, both in the NICU and upon discharge from the NICU, with an emphasis on understanding the emotional issues and concerns of the parents. Moreover, despite the strong preparation nurses have to address the human aspects of parents’ concerns, the reality of the NICU may make it difficult to set aside time for optimal teaching. Therefore, it is important to study the feasibility of implementing effective teaching in such a challenging environment.
The Active Baby for Child Development (ABCD) Intervention
Prematurity, birth at less than 37 completed weeks gestation, is an increasingly prevalent condition, a major determinant of neonatal morbidity and mortality and one of the most significant problems in perinatology (Beck et al, 2010). As a group, preterm infants are at an increased risk for decreased bone mineral density, delays in neuromotor development, chronic lung disease, altered growth patterns, and obesity (Casey, 2008; Eliakim and Nemet, 2005; Stephens and Vohr, 2009). The mechanisms that affect growth and body composition in the preterm infant are complex. Small-for-gestational-age infants enter a period of catch-up growth after birth that can persist into early childhood. This period of catch-up growth may predispose infants to an altered body composition later in life as it has been shown that low birth weight is related to higher body fat percentage, lower lean mass and increased blood pressure in adulthood (Casey; Chomtho et al., 2008; Euser, de Wit, Finken, Rijken, & Wit, 2008; Evensen et al., 2009 Yliharsila et al., 2007). A recent study with term and late preterm infants also showed that low birth weight is associated with decreased muscle strength, muscle endurance, and fitness in adulthood (Ridgway et al., 2009). An intervention aimed at changing body composition and increasing physical activity in infants during this critical period of growth and development may prove to alter the natural course of this disorder. This hypothesis is supported by recent literature reporting that children who had participated since birth in the Infant Health and Development Program (a multi-factorial education program for caregivers of premature, low-birth-weight babies) were, at 8-years of age, heavier and taller and had larger head circumference than controls (Casey et al, 2009). Therefore, research on the physical activity during a “critical period” of growth and development is important to our understanding of childhood predictors of adult body composition (Druet et al, 2008).
We developed an assisted exercise intervention (ABCD) for preterm infants for this very purpose. This exercise program is based on previous research that demonstrated that just five minutes of passive-stretching exercises per day increases bone mineralization and weight gain in preterm infants in the Neonatal Intensive Care Unit (NICU) after just four weeks of exercise (Aly et al., 2004; Litmanovitz et al., 2004; Moyer-Mileur, Brunstetter, McNaught, Gill and Chan, 2000; Nemet et al., 2002). In addition, a recent study by Vignochi, Miura, and Canan (2008) demonstrated that a similar intervention of flexion and extension exercises in preterm infants in the NICU could increase weight gain, bone mineral content and lean mass. In our research group, we are studying the impact of assisted exercise on premature infants in the NICU and at home following discharge. We have documented that mothers of preterm infants are interested in being taught to implement exercise interventions and perceive them as potentially beneficial (Gravem et al., 2009).
The first step toward conducting a randomized, controlled trial to evaluate the effects of an exercise intervention is to determine if the intervention is feasible and acceptable to infants’ caregivers. Thus, in the present feasibility study, nurses taught caregivers (mostly mothers) to implement assisted exercise so that the intervention could be performed in the home. Our primary aim was to examine the feasibility of caregivers learning to perform the assisted exercise regimen and then being able to implement the intervention at home. We aimed to identify caregivers’ perceptions about the intervention that might have implications for both the process and content of teaching. Our secondary aims were to assess the caregivers’ adherence to the exercise program as well as their ability to implement the exercises correctly, which we expected would be a reflection of the teaching process.
Study Design and Methods
Study Sample
After receiving approval from the Institutional Review Board at UC Irvine, we screened the NICU medical records for current patients to identify potential participants. We recruited caregivers (18 years and older) of preterm infants with a gestational age at birth of between 23 and 36 weeks who had reached 32 weeks post-menstrual age at the time of the exercise training, were on full feeds, and nearing discharge. We excluded infants with supplemental oxygen at discharge, tracheostomy, symptomatic congestive heart disease, or bone or skin disorders. Thirteen caregivers provided written informed consent to participate in the study (12 mothers and 1 aunt). Three babies were discharged prior to their caregivers completing the exercise training, resulting in a final sample of ten caregivers (Table 1).
Table 1.
Patient Demographics
| Patient Demographics (N=10) | Average/Percent (Range) |
|---|---|
|
| |
| Age of Caregiver | 24.3.years (19–35 years) |
|
| |
| Infant Gestational Age at Birth | 31.5 weeks (26–36 weeks) |
|
| |
| Number of Children | 1.9 children (1–4 children) |
|
| |
| Marital Status | |
| • Single | 20% |
| •Significant Other | 40% |
| •Married | 40% |
|
| |
| Education Level | |
| •Some High School | 30% |
| •High school Graduate | 50% 0% |
| •Some College | 0% |
| •College Graduate | 20% |
| •Graduate Degree | |
Procedure
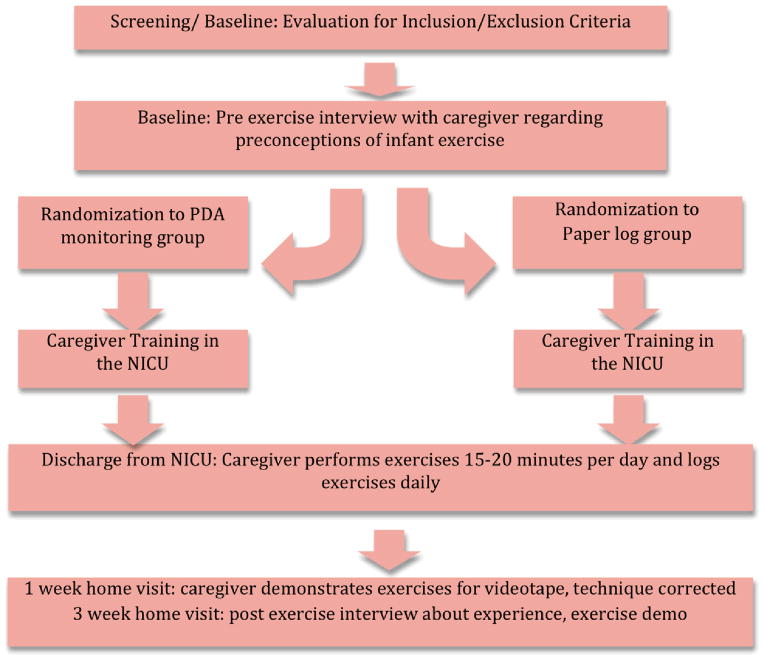
Figure 1 summarizes our study procedures. This section describes the procedures of the study, beginning with the time prior to the infant’s discharge from the hospital and continuing after the infant is at home.
Figure 1.
Prior to Discharge from the Hospital
Prior to providing training for the intervention, we conducted face-to-face interviews with each caregiver while the premature infant was hospitalized in the NICU. Grounded theory guided our approach, including the use of semi-structured, open-ended interview questions, and line-by-line analysis (Strauss and Corbin, 1998). The analytic outcome was a qualitative description (Sandelowski, 2000), providing a conceptual understanding of caregivers’ perspectives and experiences, which aided us in the development of the assisted exercise regimen. Sandelowski (2000) describes qualitative description as a useful method of presenting qualitative findings that are not at a high level of abstraction. In our research, although we used methods of grounded theory, as noted, we did not construct an abstract theory, but rather, we were able to present a description of mothers’ experiences of engaging in an assisted exercise regimen with their infants. We conducted the interviews in the caregiver’s primary language (9 in English and 1 in Spanish). Two interviewers (one medical student and one doctorally prepared researcher) were trained by an experienced qualitative researcher. Consistent with qualitative research guidelines, the interviews were conducted using a semi-structured interview guide. The open-ended interview questions focused on the caregiver’s perceptions of infant exercises. We audio-taped, transcribed, and analyzed the interviews for emergent themes related to infant exercise and caregiver concerns.
Next, we trained the caregivers in the exercise techniques in the NICU. The training personnel determined the appropriate number of teaching sessions (a range from two to seven) based on each caregiver’s performance. We provided the caregivers with a binder containing pictures of the exercises, a blanket, a colorful toy and a timer for the exercise sessions. The exercises used in this study were both passive stretching exercises and active exercises. The passive exercises included range of motion movements in which the caregiver would stretch the infant’s joints in order to provide proprioceptive input. These passive exercises have previously been used in preterm infants by Eliakim and Nemet (2005) who reported increased weight gain and improved bone strength and mineralization from assisted exercise in preterm infants. The active exercises used in the study were developed based on exercises currently taught to mothers in the University of California, Irvine NICU. The exercises were based in part on the principles of Neuro-Developmental Treatment (NDT) (Howle 2002). NDT based interventions have been successful in improving gross motor performance in a group of high-risk preterm infants in the NICU (Girolami et al 1994) and in group of four to twelve month old infants receiving therapy for posture and movement dysfunction (Arndt 2008). We modified the activities from NDT to ensure that the exercises increased physical activity in a manner that is commensurate with the motor capabilities of each enrolled premature baby. This regimen included exercises in which the infants were laid prone and encouraged to use their upper extremity, core and neck muscles to lift their heads. In addition, mothers were taught to do gentle compressions while rolling the infant to sitting or side-to-side.
After Discharge to Home
The exercise intervention began on the day of the infant’s discharge to home. We asked the caregiver to perform 15–20 minutes of assisted infant exercise 7 days a week for approximately 3 weeks. The caregivers were asked to do the exercises when the infant was awake and to wait at least one hour after feeding before starting the exercises. All infants in the study performed active exercises. Flexion-extension exercises were only used in the first six participants because it was determined that as the infants matured, these exercises were no longer appropriate. The caregivers were told that they could break the exercises up throughout the day if their infant seemed agitated when completing the entire set at one time. Caregivers also received training addressing safety precautions and were encouraged to contact the study team if questions arose during the intervention.
We measured caregiver adherence and proficiency using quantitative tools developed for this study. To measure caregiver adherence, we used either paper logs or mobile phone logs. Both methods were designed to obtain identical information, but we randomized caregivers (five per group) to use either a mobile phone or paper log because our research team will eventually look more in depth at how to use technology to improve data collection. The reason for randomizing the caregivers into these two groups is that another member of our research team is investigating the efficacy and feasibility of two different methods for reporting adherence. Although the comparison of these methods is outside of the scope of the current paper, the data obtained through these logs was used in the current study to record the daily completed exercises and the caregiver’s assessment of the state of her infant, so that we could evaluate how this might impact completion of exercises. To assess infant state, caregivers were asked to select one of the following options: sleeping, quiet awake, active awake, or fussy. We provided definitions of each infant state during training. In the mobile phone group, the log entries were delivered over the mobile phone network to the research team. If an entry was not received for two days in a row, a research team member called the caregiver to prompt her to make her entries. We entered the data from the paper and electronic logs into our study database.
To measure proficiency in the exercises, after one week of daily exercise, members of the research team made a home visit. At this home visit, the investigator videotaped the caregiver demonstrating the exercises, corrected errors, reminded the caregivers to complete the exercises daily and answered questions. After two to three weeks of daily exercises, the participants had a final home visit. During this visit, the caregivers again demonstrated the exercises and were recorded, and a researcher conducted an exit interview. A trained observer evaluated the caregivers on their proficiency in the exercise technique by scoring the video of the exercise demonstration in the final home visit using a standard evaluation form that was developed for this study. The evaluation form contained key components of each exercise as identified by a research occupational therapist. As there is no established mechanism to assign a numerical value to the components of the exercises, no numerical proficiency score was generated from evaluation form responses. However, errors in technique were counted and recorded by the observer. Furthermore, we randomly selected 20% of the video assessments and had a second trained observer rate them independently using the same evaluation instrument. We measured rater agreement by comparing the two rater's scores for each of items on the evaluation form. Rater agreement ranged from 96% to 100% across evaluation forms. This high level of agreement meets commonly accepted standards for inter-rater reliability on objective measurements.
Analyses
Qualitative Analyses
Interviews were audio taped and transcribed. Codes and themes that reflected the meaning in the data were generated. Credibility and trustworthiness were ensured by having several members of the research team review the transcripts together, discussing areas of differences in interpretation of data and arriving at consensus based on analytic team discussion. In addition, this study followed a previous study (Gravem et al, 2009) in which we used qualitative, semi-structured, open-ended interviews to explore caregivers’ perceptions and thoughts about engaging their infants in an assisted exercise regimen. By following up on that study, we were able to use “peer debriefing,” a process in which other respondents verify or modify our initial analysis. Thus, the questions we asked in our current study were based on our previous research and were somewhat focused, which allowed us to elicit more supporting data as well as to modify previous understandings of the data. Using constant comparative analysis, a key analytic process in grounded theory methodology, we compared the codes and themes across all interviews. However, as stated earlier, while we used processes of grounded theory (open-ended, semi-structured interviews, line-by-line analysis of the transcripts with coding of data grouped into categories), the analytic outcome of this study was not a grounded theory (i.e. an abstract theoretical explanation), but a qualitative description (Sandelowski, 2000) that provided a less abstract analytical description of caregivers’ experiences of conducting the assisted exercise regimen with the infants.
Quantitative Analyses
To evaluate adherence, we calculated the number of days caregivers reported completing all of the exercises as well as the number of days caregivers completed the logs. To evaluate infant state, we tallied the number of sessions for each of the four categories of infant state. To evaluate proficiency, we tallied the number of errors observed in the videotapes of caregivers performing the exercises on the infant.
Results
Intervention Adherence
Participants completed a daily log on 92% of the days in the study. Of those, caregivers reported performing the exercises an average of 93% of the days. Reasons given for not performing the exercises included: “No time”, “Grandmother in Town”, “Moving”, “Baby Sick,” and “Infant Sleeping.” Caregivers also completed a daily report of the state of their infants. Infant state was assessed in order to confirm that the exercises did not universally cause agitation as well as to understand potential reasons for not completing the exercises. Data indicated that the infants were “fussy” 21% of the time, “active awake” 36% of the time, “quiet awake” 26% of the time, and sleeping 11% of the “time.” The data did not specify whether this represented the infant state at the end of the exercise period or throughout the exercises; however, caregivers were instructed to stop the exercises if the infant was not awake or was agitated (i.e., fussy). Although being agitated and fussy may be subjective assessments, the healthcare providers explained to the mothers the descriptions of these states. The home visits then provided a “check” wherein the healthcare provider was able to follow up with the mothers to assess their proficiency in doing the exercises at the appropriate times. Results indicated that in all but one of the intervention sessions, infants were in an awake state and did not exhibit agitation. Further discussion of this one exception is included in the next section.
Caregiver Intervention Proficiency
The proficiency scale had 35 items for the first set of exercises and 23 items for the second set of exercises. On average, the caregivers made errors on 1.8 items with a range of one to three item errors. We found that four caregivers missed one step in a multi-step exercise, three caregivers had incorrect positioning of the infant’s arms in prone, and one participant demonstrated incorrect compressions. One caregiver demonstrated insufficient proficiency at the 1-week home visit and it was determined that this caregiver’s enrollment should be ended early at 12 days to protect the infant’s safety. Consequently, based on the clinical judgment of the home visitor, we discontinued her participation in the study in order to avert a potential adverse event.
Interview Themes
Pre-Intervention
1) Perceptions of what they could do for their infants’ health
Caregivers described several concrete actions that they could do to improve the health of their infants such as taking extra precautions, breastfeeding, and protecting their infants from infection. One caregiver stated that it was important to “Give them the right kinds of foods… make sure he doesn’t get into anything toxic. No chemicals or just keep him away from everything that’s bad.” Another caregiver said that she will “Try to take a number of, a lot of precautions with them…such as not taking them out on the street too much, because they might catch some virus, because they don’t have many defenses.” Caregivers also described abstract concepts, such as a loving family, as a mechanism to improve their infant’s health. One caregiver stated, “I can talk to them…once I’m allowed to touch them, I can touch them, hug them…so they’ll feel that someone is here with them; that is, that they’re not alone and that…that they have parents.”
2) Perceptions of exercise
Caregivers often used their own experiences with exercise as a framework for describing infant exercise. While some caregivers equated exercise with the gym or actively trying to work out, others considered their routine daily activities as exercise. One mother stated, “‘cause I live in the second floor, so that’s all my exercise I do…. and walk to the store, to the house, to the library… to the mail, to school with my girls… That’s all the exercise.” The same was true of caregivers’ descriptions of infant exercise. While some commented that they could encourage their infant to increase physical activity with specific exercises, other caregivers described infant exercises as something that would normally be incorporated into the daily routine of any infant, such as eating as a time to incorporate exercise. One caregiver said, “They say during bath time and changing time and feeding time, those are some times you know when you can exercise and make it playful.” In addition, some caregivers had previous experiences with infant exercise that influenced their perceptions of it. One mother said, “I did it before with my other girls… so it works… They have healthy bones… they jump all over, [if] they fall they don’t hurt.”
3) Anticipated Benefits
While some caregivers described negative feelings about exercise for themselves, they all reported that infant exercise would be beneficial for their infant. One caregiver said, “I don’t like to exercise, because I’m really lazy, so I don’t know. It just means, like for me, like sweating… it reminds me of sweating… Yeah, I don’t like it.” Perceived benefits of infant exercise included increased muscle and bone strength and accelerated growth. One mother stated, “Because he is little. He is a smaller baby so maybe strengthening up and encouraging some natural growth I’m hoping.”
Post-Intervention
1) Perceived Benefits
After participating in the study, all caregivers described the exercises as being beneficial for their infants. Furthermore, most believed that their infants had increased strength secondary to the exercise intervention. When describing the exercise intervention one caregiver said, “Perfect… I think she developed a little of her muscles, her movements, and I think …just perfect for her. Another mother said, “I think that he is a lot stronger because of those exercises…He is picking up his head and he’s rearing up against my chest. He’s pushing back from my chest!” The caregivers described their experience in the exercise study very positively. In addition to the perceived physiological benefits of the exercises, many mothers reported that these interventions fostered increased bonding with their babies. Caregivers mentioned that the exercise intervention was additional time that they may not otherwise have spent with their infants. A mother stated, “It was a time to bond and play with my baby and things like that. Even if I was too tired I’d still do the exercises.” Another mother said, “[The Intervention] was a reprieve to take your mind off everything that was stressful. Because they are fun. To hold and play with your baby is a fun, enjoyable thing…. Enlightening I guess as far as knowing my baby’s body and um I guess seeing him grow and develop.”
2) Fears of Performing Infant Exercise
While the caregivers anticipated benefit from the exercises, nearly all caregivers in the study reported feeling scared of hurting their baby during the first few days after discharge from the NICU. One caregiver said, “At first, I was a little bit of scared… To hurt her….just, she was too little.” Reasons given for fear included the small size of their infant, fussiness of the baby during exercises, the position of the prone exercise, and the new transition from hospital to the home.
3) Caregiver Responsiveness to the Infant’s Cues
Another key theme identified in the interviews was the necessity for the caregiver to demonstrate responsiveness to the infant’s needs during the exercises. Many caregivers stated that at certain times their infant resisted the exercises or appeared uncomfortable. One mother said, “Sometimes I feel a little bit uncomfortable because she didn’t seem to like it much … she would get really tense…sometimes I felt that I might hurt her.” However, most caregivers reported an appropriate responsiveness to this resistance. These caregivers stated that they did not want to force the exercises and that instead they waited for cues from their infants and responded accordingly. Caregivers said, “Well, sometimes she was fussy…then I stopped for a little bit and then started again” and “I would spread ‘em out if I saw that he was too sleepy or you know he just wasn’t as active.”
4) Professional Involvement Can Both Reduce and Increase Maternal Stress
Caregivers paradoxically expressed both a feeling of decreased stress as a result of the training program and nurse instruction and at the same time a feeling of increased stress secondary to nursing instructions that seemed contrary to their maternal instinct. These subthemes are discussed below.
Perceived Benefits of Professional Involvement in Success of Exercise Intervention
Caregivers reported that the training sessions left them feeling prepared and more confident to perform the exercises in the home, alleviating many of their fears. A caregiver said, “I’m glad that (the training) was in the hospital and stuff because you feel a little more comfortable touching and doing those different touches with your baby”. Another caregiver expressed comfort regarding the training in the home saying, “At first, before you came out to see me, I was a little nervous to do some of the exercises. But then we got the (home visit) and so that gave me a little more confidence.”
The participants reported that they enjoyed the home visits for several reasons. The caregivers saw the visits as a chance to receive additional training on the exercise technique or ask questions. One mother said regarding the home visits, “Yes, yes, yes...Please do come… We feel comfortable too. Once we see you, so we feel, Okay, thank God …someone is here.” In addition, caregivers stated that the home visits were important for accountability and adherence. One mother said, “‘Cause for all [the researchers] know, a mom could be lying and saying they’re doing it every day and then you guys come and check on them.”
Perceived Conflicts between Recommendations from Medical Authorities and Maternal/Caregiver Instinct
Participant responses also revealed a perceived conflict between maternal instinct and medical authorities. While caregivers expressed wanting to hold their infants, they reported that they were told that the infant needed to be left alone to grow. A caregiver said, “I want to hold them all the time …but I know that they need their sleep to grow… The nurses told me that… after they eat, you should put them back to sleep…so they can grow, or something like that…. I want to hold them all of the time, you know…. But, they’re like, oh, they need to sleep. I’m like, he’s not sleeping, he’s crying.”
Discussion
While interventions in the NICU have shown promising effects for infant exercise, the benefits may be lost if the program is not continued in the home after discharge. This study was the first attempt to understand the feasibility of teaching parents to implement a program of increased physical activity in the home.
Caregivers were diligent in completing daily exercise logs and the exercise intervention. Of the days of missed exercise, 38% occurred during the first 4 days after discharge. This identifies the first week in the home as a crucial time to address adherence to the intervention. Reasons for missing days of exercise included thinking that the infant was not awake enough to complete the exercise, interruptions in daily routine such as visiting relatives and moving, and sickness. Results from data assessing infant state indicated that during the majority of intervention sessions, infants were in a quiet or active awake state. It was important to assess the state of the infant during the exercise sessions because if the exercises seemed to cause agitation, this may suggest that changes to the exercise regimen are needed; in addition, if mothers routinely documented that infants were sleeping or fussy during the period chosen to implement the program, this would suggest the need for additional training to help mothers select the most appropriate times (“active awake” or “quiet awake”) to implement the intervention. In future studies, we can anticipate these potential barriers to performing the exercises daily, and trainers can use this information in an attempt to maximize daily adherence.
The errors identified in exercise demonstrations included: missing one step in a multi-step exercise, incorrect positioning of the infant’s arms in prone, and incorrect compressions. This highlights key areas that must be emphasized during training. In addition, each step of a multistep exercise should be clearly explained in the exercise binder so that key components are not overlooked. Furthermore, we are exploring new means of providing long-term training to caregivers, such as online communities, video training, and interactive educational materials that might be more engaging than the paper binders and encourage caregivers to make more use of the materials.
Overall, the caregivers described the exercise intervention as a positive experience and beneficial for their infants. While the perceived benefit of the intervention was not quantitatively measured, it is important that caregivers believe that the exercises are beneficial in order to implement a long-term intervention. Without parental engagement, it would be impossible to implement a home intervention, as this requires significant time and effort from the caregivers each day. In addition, studies have shown that parental perceptions regarding physical activity significantly impact the quantity of physical activity performed by the child (Trost, 2003). Therefore, a positive perception of the intervention and physical activity in general, on the part of the parent may be necessary to increase physical activity in the long term.
Clinical Nursing Implications
The fears expressed by caregivers during the first few days of home exercise have important clinical implications for nurses. Although we recognize that some fear and apprehension are normal parts of learning to care for a fragile infant, it is important to anticipate these feelings and structure teaching and intervention around them. Caregivers report that while they were nervous to do the exercises in the beginning, the fears were alleviated by practice in the home and further teaching at the first home visit. This highlights the idea that teaching cannot end in the hospital. It must continue in the home to provide additional reassurance and support to caregivers. This has important implications for nursing practice. Nurses are central to providing teaching and encouragement to parents, as well as answering questions and alleviating concerns.
The importance of caregiver responsiveness to infant cues also has clinical implications. Nurses can model this type of responsiveness when demonstrating recommended interventions with infants, such as our exercise program. In addition, it may be important to notice the caregivers’ responsiveness to the infant’s cues during hospital or home visits. Inappropriate responsiveness may alert nurses that more teaching is needed. We hypothesize, and caregivers in this study reported, that the infant exercises would improve maternal-infant interactions. However, it is conceivable that if the caregiver ignores infant cues to adhere tightly to the exercise routine, this could potentially worsen maternal infant interactions. These findings may be generalized to caregiver-implemented nursing interventions as a whole. Following discharge after potentially months of NICU care, parents may feel overwhelmed with the perceived fragility of their premature infant. Parents may be asked to perform regular eye drops or tube feedings. Difficulties implementing daily exercise interventions, such as poor adherence during the first few days at home and fears of hurting their infants, may overlap with barriers to other tasks that new caregivers are asked to perform. In addition, this study demonstrated that home visits were a critical part of training, serving to both correct mistakes and alleviate fears. Home visits from NICU nurses may be similarly valuable when parents are asked to perform medical interventions in the home.
Limitations and Recommendations for Future Research
This study is limited by the small sample size of 10 participants; however, theoretical saturation was reached in the participant interviews. An important limitation of this study was the wide range in number of sessions required for parents to learn the intervention; this highlights the diversity in caregivers’ needs when it comes to learning how to care for a high-risk infant. The fact that caregivers’ educational needs differed so widely is consistent with current emphases in medicine to examine individualized treatment approaches that are tailored to individual patient needs. In future research, it will be important to standardize training and study how to best address caregivers’ needs for instruction. Future studies of caregiver-implemented infant exercise must be done to assess fully the effects of home exercise interventions on physical activity and body composition in infants. Future research also should address factors that may moderate intervention outcomes, including caregiver proficiency and adherence.
Conclusion
In summary, we have demonstrated that it is feasible to implement a home-based exercise intervention program for premature babies. Caregivers were willing and able to do the exercises correctly, and they expressed a belief that the intervention had positive effects on both their babies and their relationships with their babies.
Table 2.
Clinical Nursing Implications
| Clinical Nursing Implications |
| Positive caregiver perception of a medical intervention to be carried out in the home may be a critical determinate of caregiver adherence. |
| Caregivers may express fear regarding infant fragility after discharge from the NICU. |
| This fear may be alleviated by: |
|
| Caregivers may experience increased difficulty adhering to interventions during the first few days after discharge from the NICU. |
| Caregivers may have difficulty performing multi-step interventions with their preterm infants. This difficulty may be alleviated by increased training. |
Acknowledgments
Funding: NIH National Institute of Nursing Research #RO1 NR09070
Contributor Information
Dana Gravem, University of Chicago, Department of Obstetrics and Gynecology.
Kimberley Lakes, Pediatrics, University of California, Irvine.
Julia Rich, Institute for Clinical and Translational Science, University of California, Irvine Jessica Vaughan BA, University of California, Irvine.
Gillian Hayes, Informatics, University of California, Irvine.
Dan Cooper, Pediatrics, University of California, Irvine.
Ellen Olshansky, Program in Nursing Science, University of California, Irvine.
References
- Aly H, Moustafa M, Hassanein S, Massaro A, Amer H, Patel K. Physical activity combined with massage improves bone mineralization in premature infants: a randomized trial. J Perinatol. 2004;24(5):305–309. doi: 10.1038/sj.jp.7211083. [DOI] [PubMed] [Google Scholar]
- Arndt S, Chandler L, Sweeney J, Sharkey M, McElroy J. Effects of a neurodevelopmental treatment-based trunk protocol for infants with posture and movement dysfunction. Pediatr Phys Ther. 2008;20:11–22. doi: 10.1097/PEP.0b013e31815e8595. [DOI] [PubMed] [Google Scholar]
- Beck S, Wojdyla D, Say L, Betran A, Merialdi M, Requejo H, Rubens C, Menon R, Van Look P. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bulletin of the World Health Organization. 2010;88(1):1–80. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey P. Growth of low birth weight preterm children. Semin Perinatol. 2008;32(1):20–27. doi: 10.1053/j.semperi.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Casey P, Bradley R, Whiteside-Mansell L, Barrett K, Gossett J, Simpson P. Effect of early intervention on 8-year growth status of low-birth-weight preterm infants. Arch Pediatr Adolesc Med. 2009;163:1046–1053. doi: 10.1001/archpediatrics.2009.192. [DOI] [PubMed] [Google Scholar]
- Chomtho S, Wells J, Williams J, Davies P, Lucas A, Fewtrell M. Infant growth and later body composition: evidence from the 4-component model. Am J Clin Nutr. 2008;87(6):1776–1784. doi: 10.1093/ajcn/87.6.1776. [DOI] [PubMed] [Google Scholar]
- Druet C, Ong K. Early childhood predictors of adult body composition. Best Pract Res Clin Endocrinol Metab. 2008;22:489–502. doi: 10.1016/j.beem.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Eliakim A, Nemet D. Osteopenia of prematurity – the role of exercise in prevention and treatment. Pediatr Endocrinol Rev. 2005;2(4):675–682. [PubMed] [Google Scholar]
- Euser A, de Wit C, Finken MJ, Rijken M, Wit JM. Growth of preterm born children. Horm Res. 2008;70(6):319–328. doi: 10.1159/000161862. [DOI] [PubMed] [Google Scholar]
- Evensen K, Steinshamn S, Tjonna A, Stolen T, Hoydal M, Wisloff U, Brubakk A, Vik T. Effects of preterm birth and fetal growth retardation on cardiovascular risk factors in young adulthood. Early Hum Dev. 2009;85(4):239–245. doi: 10.1016/j.earlhumdev.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Girolami G, Campbell S. Efficacy of a Neuro-Developmental Treatment program to improve motor control of preterm infants. Pediatric Physical Therapy. 1994;6:175–184. [Google Scholar]
- Gravem D, Lakes K, Teran L, Rich J, Cooper D, Olshansky E. Maternal perceptions of infant exercise in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2009;38(5):527–33. doi: 10.1111/j.1552-6909.2009.01055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A. Long-term pulmonary outcome in the preterm infant. Neonatology. 2008;93(4):324–327. doi: 10.1159/000121459. [DOI] [PubMed] [Google Scholar]
- Howle J. Neurodevelopmental Treatment Approach: Theoretical Foundations and Principles of Clinical Practice. Laguna Beach, CA: North American Neuro-Developmental Treatment Association; 2002. [Google Scholar]
- Jones L, Woodhouse D, Rowe J. Effective nurse parent communication: A study of parents’ perceptions in the NICU environment. Patient Education and Counseling. 2007;69:206–212. doi: 10.1016/j.pec.2007.08.014. [DOI] [PubMed] [Google Scholar]
- Kowalski WJ, Leef KH, Mackley A, Spear ML, Paul DA. Communicating with parents of premature infants: Who is the informant? J of Perinatology. 2006;26:44–48. doi: 10.1038/sj.jp.7211409. [DOI] [PubMed] [Google Scholar]
- Litmanovitz I, Dolfin T, Regev R, Arnon S, Friedland O, Shainkin-Kestenbaum R, Lis M, Eliakim A. Bone turnover markers and bone strength during the first weeks of life in very low birth weight premature infants. J Perinat Med. 2004;32(1):58–61. doi: 10.1515/JPM.2004.010. [DOI] [PubMed] [Google Scholar]
- McKechnie AC, Pridham K. Qual Health Research. 2012. Published Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk BM, Bullock T, McGrath J, Jacobson D, Kelly St, Baba L. Translating the evidence-based NICU COPE Program for parents of premature infants into clinical practice. J Perinat Neonat Nurs. 2010;24(1):74–80. doi: 10.1097/JPN.0b013e3181ce314b. [DOI] [PubMed] [Google Scholar]
- Moyer-Mileur L, Brunstetter V, McNaught T, Gill G, Chan G. Daily physical activity program increases bone mineralization and growth in preterm very low birth weight infants. Pediatrics. 2000;106(5):1088–1092. doi: 10.1542/peds.106.5.1088. [DOI] [PubMed] [Google Scholar]
- Nemet D, Dolfin T, Litmanowitz I, Shainkin-Kestenbaum R, Lis M, Eliakim A. Evidence for exercise-induced bone formation in premature infants. Int J Sports Med. 2002;23(2):82–85. doi: 10.1055/s-2002-20134. [DOI] [PubMed] [Google Scholar]
- Ridgway C, Ong K, Tammelin T, Sharp S, Ekelund U, Jarvelin MR. Birth size, infant weight gain, and motor development influence adult physical performance. Med Sci Sports Exerc. 2009;41(6):1212–1221. doi: 10.1249/MSS.0b013e31819794ab. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Schlittenhart JM, Smart D, Miller K, Severtson B. Preparing parents for NICU discharge: An evidence-based teaching tool. Nursing for Women’s Health. 2011;15(6):485–494. doi: 10.1111/j.1751-486X.2011.01676.x. [DOI] [PubMed] [Google Scholar]
- Stephens B, Vohr B. Neurodevelopmental outcome of the premature infant. Pediatr Clin North Am. 2009;56(3):631–46. doi: 10.1016/j.pcl.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research techniques and procedures for developing grounded theory. Newbury Park, CA: Sage; 1998. [Google Scholar]
- Trost S, Sallis J, Pate R, Freedson P, Taylor W, Dowda M. Evaluating a model of parental influence on youth physical activity. Am J Prev Med. 2003;25(4):277–282. doi: 10.1016/s0749-3797(03)00217-4. [DOI] [PubMed] [Google Scholar]
- Vignochi C, Miura E, Canani L. Effects of motor physical therapy on bone mineralization in premature infants: a randomized controlled study. J Perinatol. 2008;28(9):624–631. doi: 10.1038/jp.2008.60. [DOI] [PubMed] [Google Scholar]
- Yliharsila H, Kajantie E, Osmond C, Forsen T, Barker D, Eriksson J. Birth size, adult body composition and muscle strength in later life. Int J Obes (Lond) 2007;31(9):1392–1399. doi: 10.1038/sj.ijo.0803612. [DOI] [PubMed] [Google Scholar]