Abstract
Background
This study examined self-reported frequency and intensity of physical activity in gastric bypass patients, and the relationship between physical activity and weight loss and psychosocial outcomes during 12-month postoperative follow-up.
Methods
Participants were 131 obese patients who underwent gastric bypass surgery and completed psychometrically established measures assessing physical activity, depression, and physical and mental health preoperatively and at a 12-month follow-up assessment.
Results
Preoperatively, 62.6% of patients reported at least one episode of a minimum of 15 minutes of physical activity per week. This figure increased to 92.4% at 12-month postoperative follow-up. Both the frequency and intensity levels of physical activity episodes increased significantly from preoperative to 12-month postoperative assessments. Hierarchical regression analyses, controlling for demographic variables and preoperative body mass index (BMI), revealed that the intensity of physical activity was significantly associated with postoperative weight loss at 12-month follow-up. Both the frequency and intensity of physical activity were significantly associated with depression, and physical and mental well-being at the 12-month postoperative follow-up.
Conclusion
Gastric bypass patients increase both the frequency and intensity of their physical activity during the first 12 months postoperatively. Higher postoperative intensity levels of physical activity are associated with better weight loss outcomes while both increased frequency and intensity levels of physical activity are associated with better psychosocial outcomes.
Keywords: Gastric bypass, Physical activity, Exercise, Obesity, Weight loss, Psychosocial functioning
Introduction
Regular physical activity has been empirically established as a critical component of successful weight control and weight loss maintenance programs [1, 2]. It can also have important psychosocial benefits [1]. Recent research has produced further evidence suggesting that regular physical activity is associated with improved physical health and psychosocial functioning across diverse obese patient populations [3, 4]. However, remarkably little is known about physical activity in severely obese patients who undergo bariatric surgery. A recent systematic review of the literature by Livhits and colleagues [5] identified only 13 published studies that reported on the relationship between physical activity and degree of postoperative weight loss following bariatric surgery. Overall, the available literature suggests that physical activity following bariatric surgery is associated with greater weight loss [5]. However, the literature is mixed, with studies reporting a considerable range in terms of both the amounts of physical activity reported by bariatric surgery patients and the strength of associations with weight losses [6, 7]. Differences in study designs, assessment methods, bariatric surgery methods, and small sample sizes may account in part for some of the variability in findings across studies. Nonetheless, to date, little attention has been paid to considering both the frequency and intensity of physical activity postoperatively and considering associations with broader outcomes (i.e., psychosocial outcomes) in addition to weight losses. The few available data do suggest that increased physical activity is associated with improved mental health outcomes following bariatric surgery [6, 8] although the relative importance of dimensions of physical activity such as frequency and intensity remains unknown.
This study examined the frequency and intensity of physical activity reported by extremely obese patients prior to undergoing gastric bypass surgery and again at a postoperative 12-month follow-up. This study also examined the associations between both frequency and intensity of physical activity with weight loss and psychosocial functioning at 12-month postoperative follow-up.
Method
Participants
Participants for this study were 131 (15 males and 116 females) extremely obese patients who underwent gastric bypass surgery at a general medical center in an urban center. These 131 subjects were selected from a larger consecutive series of 221 patients who underwent gastric bypass surgery based on completing all of the assessments described below (including measured heights and weights) at both assessment points (i.e., prior to surgery and again at 12-month postoperative follow-ups). Analyses revealed no significant differences between the study sample and the bariatric surgery patients who did not complete both assessments in age, gender, ethnicity (white versus non-white), or preoperative body mass index (BMI). Participants had a mean age of 42.9 years (SD=10.3); 72.5% were Caucasian, 14.5% African-American, and 11.5% Hispanic. Sixty-five percent had completed at least some college.
Assessments and Measures
A human subjects committee (IRB) approved the study protocol, and written informed consent was obtained from each participant. Participants were recruited by clinical staff members at the time of a routine evaluation for surgical candidacy. Patients were informed that they could participate in a research study to learn about the effects of bariatric surgery over time on weight, behaviors, psychological functioning, and quality of life. Participants were informed that taking part in the research would not influence the type of care provided by the surgical team and that there would be no direct medical benefit to them, although it was hoped that the knowledge gained might ultimately benefit future bariatric surgery patients. No compensation was provided.
Participants completed a battery of psychometrically established self-report measures and had height and weight measured prior to surgery and again at 12-month postoperative follow-ups. The following measures were administered during the two time points.
The Godin Leisure Time Questionnaire (GLTQ) [9] is a brief four-item measure of physical activity. Participants rate their frequency of participation in mild (e.g., easy walking, bowling), moderate (e.g., fast walking, tennis), and strenuous (e.g., jogging, basketball) episodes of physical activity for more than 15 min on a weekly basis. The GLTQ assesses these two physical activity dimensions (frequency and intensity) specifically for the past week. The GLTQ has been used extensively in physical activity research (e.g., [10]); reliability and validity studies are summarized in the 1997 Supplement to Medicine and Science in Sports and Exercise [11].
The Beck Depression Inventory (BDI) [12] is a 21-item measure of the features and symptoms of depression. The BDI taps a broad range of negative affect, not just depressive affect, and is a useful marker for broad psychosocial distress and psychopathology [13, 14]. Higher scores reflect higher depression and negative affect levels. It has been used extensively and is a well-established measure with demonstrated reliability and validity [15, 16]. In the present study, internal consistency of the BDI was 0.85.
The Medical Outcomes Study Short Form-36 Health Survey (SF-36) [17] was used to assess health-related quality of life. This widely used and well-established 36-item instrument consists of eight subscales assessing different aspects of physical and mental well-being, producing physical component (SF-36-PC) and mental component (SF-36-MC) summary scores. These summary scores have a mean of 50 and standard deviation of 10 [17–19].
Results
Changes in Weight and Psychosocial Functioning
Prior to proceeding with analyses, all distributions were examined for normality. Postsurgical BDI showed moderate positive skew, while mild negative skew was observed in the postsurgical distribution of the SF-36-MC. The degree of skew was deemed acceptable for proceeding with analyses.
The mean preoperative BMI was 51.6 (SD=8.0). At the 12-month postoperative follow-up, the mean reduction in BMI was 18.1 BMI units (SD=4.5), resulting in a mean 12-month postoperative BMI of 33.4 (SD=6.4). Thus, the mean percentage of excess BMI loss (%EBL) was 71.3 (SD= 18.1). Mean BDI scores showed improvement from preoperative to postoperative time points (M=13.8 (SD=8.4) versus M=4.9 (SD=5.5), respectively; t(130)=13.9, p< 0.001). Mean SF-36-PC scores also showed significant improvement from preoperative to postoperative time points (M=32.2 (SD=10.5) versus M=51.0 (SD=9.1), respectively; t(130)=19.1<0.001). Mean SF-36-PC scores showed a similar pattern (M=47.5 (SD=11.7) versus 53.0 (SD= 11.0); t(130)=5.0, p<0.001). These represent both statistically significant and clinically robust improvements.
Levels of Physical Activity at Preoperative and Postoperative Assessments
Participants were categorized as reporting no physical activity (no episodes of exercise), mild physical activity (at least one mild episode but no moderate or strenuous episodes), moderate physical activity (at least one moderate episode but no strenuous episodes), or strenuous physical activity (at least one strenuous episode) based on their responses on the GLTQ. Figure 1 shows the proportion of participants categorized in each category of physical activity at the two time points (preoperative and 12-month postoperative assessments). Overall, 37.4% (n=49) of participants reported no episodes of physical activity preoperatively whereas only 7.6% (n=10) of participants reported not engaging in any physical activity at the 12-month postoperative follow-up. The frequency of episodes of physical activity increased significantly from preoperative to postoperative time points (M=2.9 (SD=3.2) versus M=6.6 (SD=4.3), respectively; t(130)=8.7, p< 0.001). The intensity of physical activity also increased from 32.9% of participants reporting at least one weekly episode of moderate or strenuous physical activity preoperatively to 74.8% at the 12-month postoperative follow-up.
Fig. 1.
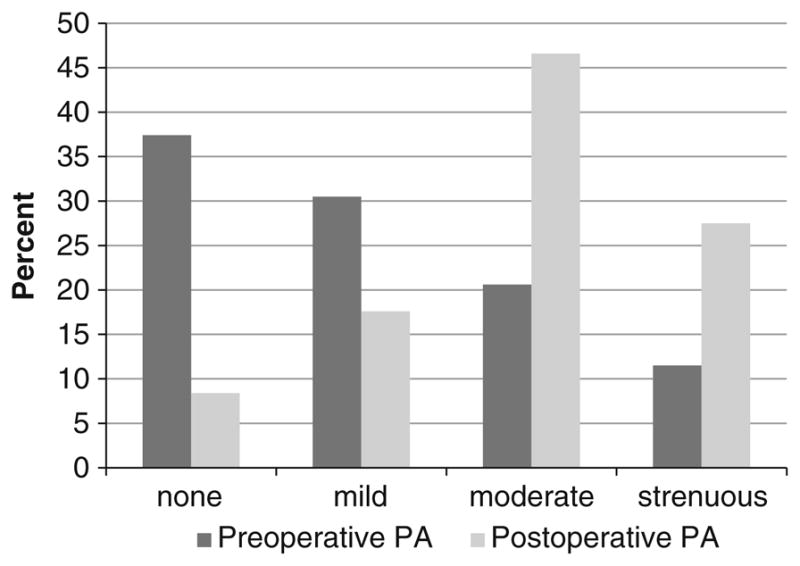
Percent of patients engaging in physical activity preoperatively and at 12-month postoperative follow-up
Physical Activity and Postoperative Weight Loss
In order to examine the relationship between physical activity and weight loss, physical activity was correlated with %EBL 12 months postsurgery. Frequency of total physical activity was calculated by adding the number of episodes of mild, moderate, and strenuous physical activity reported on the GLTQ. Frequency of moderate/strenuous activity was calculated by adding the moderate and strenuous items (i.e., number of episodes of each) of the GLTQ. The frequency of total physical activity was not associated with %EBL (r=0.14, p=0.11); however, the frequency of moderate/strenuous physical activity was significantly correlated with %EBL (r=0.24, p=0.007). Two hierarchical regression analyses were conducted to examine the relationships between (1) frequency and (2) intensity of postoperative physical activity and weight loss at the 1-year postoperative time point. Intensity of postoperative physical activity was measured by creating a dichotomous variable including (1) patients reporting either no physical activity or only episodes of mild physical activity and (2) patients reporting episodes of moderate or strenuous physical activity. Because of their relationship to BMI and/or postoperative weight loss, we followed the standard practice of controlling for sex, ethnicity, age, and preoperative BMI by entering them into the first block of each regression, followed by one of the two physical activity variables. Table 1 summarizes the results for each regression model.
Table 1.
Hierarchical regression analyses: 12-month postoperative weight loss
| Variable | ΔR2 | Adjusted R2 | F | β (standardized) PA frequency as predictor | β (standardized) PA intensity as predictor |
|---|---|---|---|---|---|
| Demographic | 0.347 | 0.326 | 16.73*** | ||
| Sex | 0.089 | 0.114 | |||
| Age | −0.097 | −0.073 | |||
| Ethnicity | −0.140 | −0.131 | |||
| Preoperative BMI | −0.531*** | −0.504*** | |||
| PA Frequency | 0.000 | 0.321 | 0.94 | 0.023 | |
| PA Intensity | 0.030 | 0.352 | 6.08* | 0.180* |
Sex was coded as 0 (female) or 1 (male). Ethnicity was dichotomized and coded as 1 (white) or 2 (non-white)
BMI body mass index, PA physical activity
p<0.05;
p<0.01;
p<0.001
Frequency of postoperative physical activity was not significantly associated with %EBL (ΔR2=0.000, p>0.05) at the 1-year postoperative time point. However, intensity of physical activity was significantly associated with %EBL (ΔR2=0.030, p<0.05); the entire model accounted for 35% of the variance in %EBL.
Physical Activity and Postoperative Psychosocial Outcomes
Six hierarchical regression analyses were performed to examine the relationships between frequency and intensity of postoperative physical activity and the psychosocial outcomes. Dependent variables included total BDI, SF-36-PC, and SF-36-MC scores. As with the preceding analyses, demographic factors (sex, age, and ethnicity) and preoperative BMI were entered in the first block of the regression, preoperative values of the appropriate psychosocial variable were entered in the second block, and either physical activity frequency or intensity was entered in the third block. Results from these analyses are summarized in Tables 2, 3, and 4.
Table 2.
Hierarchical regression: 12-month postoperative Beck Depression Inventory
| Variable | ΔR2 | Adjusted R2 | F | β (standardized) PA frequency as predictor | β (standardized) PA intensity as predictor |
|---|---|---|---|---|---|
| Demographic | 0.053 | −0.023 | 1.77 | ||
| Sex | −0.040 | −0.056 | |||
| Age | −0.064 | −0.058 | |||
| Ethnicity | 0.034 | 0.064 | |||
| Preoperative BMI | 0.134 | 0.132 | |||
| Preoperative BDI | 0.222 | 0.246 | 38.19*** | 0.459*** | 0.465*** |
| PA Frequency | 0.053 | 0.295 | 9.80** | −0.242** | |
| PA Intensity | 0.059 | 0.302 | 11.05*** | −0.252*** |
Sex was coded as 0 (female) or 1 (male). Ethnicity was dichotomized and coded as 1 (white) or 2 (non-white)
BMI body mass index, PA physical activity
p<0.05;
p<0.01;
p<0.001
Table 3.
Hierarchical regression analyses: 12-month postoperative SF-36 physical health
| Variable | ΔR2 | Adjusted R2 | F | β (standardized) PA frequency as predictor | β (standardized) PA intensity as predictor |
|---|---|---|---|---|---|
| Demographic | 0.128 | 0.100 | 4.61** | ||
| Sex | 0.035 | 0.058 | |||
| Age | −0.133 | −0.126 | |||
| Ethnicity | −0.053 | −0.074 | |||
| Preoperative BMI | −0.128 | −0.144 | |||
| Preoperative SF-36-PC | 0.051 | 0.146 | 7.82** | 0.260** | 0.272** |
| PA Frequency | 0.037 | 0.178 | 5.77** | 0.200* | 0.260** |
| PA Intensity | 0.063 | 0.205 | 10.30** |
Sex was coded as 0 (female) or 1 (male). Ethnicity was dichotomized and coded as 1 (white) or 2 (non-white)
BMI body mass index, PA physical activity
p<0.05;
p<0.01;
p<0.001
Table 4.
Hierarchical regression analyses: 12-month postoperative SF-36 mental health
| Variable | ΔR2 | Adjusted R2 | F | β (standardized) PA frequency as predictor | β (standardized) PA intensity as predictor |
|---|---|---|---|---|---|
| Demographic | 0.064 | 0.034 | 2.15 | ||
| Sex | −0.091 | −0.089 | |||
| Age | 0.214* | 0.191* | |||
| Ethnicity | 0.069 | 0.029 | |||
| Preoperative BMI | −0.154 | −0.175* | |||
| Preoperative SF-36-MC | 0.149 | 0.182 | 23.71*** | 0.393*** | 0.402*** |
| PA Frequency | 0.065 | 0.243 | 11.10*** | 0.266*** | |
| PA Intensity | 0.029 | 0.205 | 4.70* | 0.175* |
Sex was coded as 0 (female) or 1 (male). Ethnicity was dichotomized and coded as 1 (white) or 2 (non-white)
BMI body mass index, PA physical activity
p<0.05;
p<0.01;
p<0.001
Both frequency of physical activity (ΔR2=0.053, p< 0.01) and intensity of physical activity (ΔR2=0.059, p< 0.001) were significantly associated with BDI scores at the 1-year postoperative time point; jointly, the variables accounted for 29% and 30% of the total variance in % EBL, respectively. In addition, both frequency (ΔR2= 0.037, p<0.05) and intensity (ΔR2=0.063, p<0.01) of physical activity were significantly associated with SF-36-PC scores at the 1-year postoperative time point; jointly, the variables accounted for 18% and 21% of the variance in % EBL, respectively. Finally, both frequency (ΔR2=0.065, p<0.001) and intensity (ΔR2=0.029, p<0.05) of physical activity were also significantly associated with SF-36-MC scores at the 1-year postoperative time point; jointly, the variables accounted for 24% and 21% of the variance in % EBL, respectively.
Discussion
Extremely obese patients who undergo gastric bypass surgery report increases in both the frequency and intensity of physical activity during the year following surgery. Even these modest physical activity levels are significantly associated with important positive outcomes. Specifically, we found that patients’ reports of higher intensity levels of physical activity postoperatively are associated with greater weight loss outcomes while both higher frequency and intensity levels of physical activity are associated with better psychosocial outcomes at 12 months postoperatively.
Prior to undergoing gastric bypass surgery, one third of patients denied engaging in physical activity for even as little as a minimum of 15 min/week. By the 12-month postoperative follow-up, only 7.6% of patients continued to report no physical activity. Self-reported intensity of physical activity also increased, with roughly three-fourths of patients reporting at least one episode of moderate or intense physical activity during the past week at the 12-month postoperative follow-up assessment. While there are many factors that may contribute to this improvement (e.g., improved mobility resulting from weight loss following surgery, encouragement from family, friends, and health care providers), increased physical activity should be considered a positive surgical outcome.
Our findings extend previous research, suggesting that intensity of physical activity is associated with postoperative weight loss [6, 20]. Patients who reported engaging in moderate or strenuous physical activity had a significantly higher %EBL, although the frequency of physical activity was not associated with %EBL. These findings suggest that engaging in physical activity of higher intensity may facilitate weight loss during the first postoperative year. Alternatively, it is possible that greater weight loss facilitates increased engagement in physical activity as activity becomes easier at a lower patient weight or that the effects are bidirectional, with patients engaging in more physical activity due to weight loss, which then promotes further weight loss. Physical activity was associated with a significant but relatively small amount of variance in weight loss outcomes. This should not be surprising, given that weight loss during the first year following surgery is primarily the result of the surgical procedure.
Our findings that both frequency and intensity of postoperative physical activity were significantly associated with better psychosocial outcomes are consistent with previous reports demonstrating this relationship across a variety of populations [3, 21, 22]. The benefit was more pronounced in patients who engaged in moderate or strenuous physical activity. While this relationship is most typically conceptualized as physical activity improving psychosocial functioning, the possibility that patients who improve psychosocially increase their physical activity cannot be ruled out. Experimental research is needed to determine whether increasing physical activity in bariatric patients will produce these benefits.
We note several methodological strengths and limitations of the study as context for interpreting the findings. Strengths of the present study include its prospective design, use of a standardized measure of physical activity that allowed examination of both frequency and intensity dimensions, and assessment of multiple-outcome domains both preoperatively and postoperatively at a 12-month follow-up. One potential limitation is our reliance on self-report for assessing physical activity given research suggesting that it tends to be associated with overestimation of physical activity [23]. Among bariatric surgery patients, objective measures of physical activity (e.g., accelerometer data) reveal smaller increases in exercise than do subjective (e.g., self-report) measures [24]. Because this study was naturalistic and not experimental, caution is needed in interpreting the observed associations or their directionality. Additional research is needed to test physical activity in controlled treatment studies in order to more definitively determine its contributions to bariatric outcomes. For example, future research might control for frequency, intensity, and duration of physical activity in bariatric surgery patients to determine optimal prescription approaches.
Acknowledgments
This study was supported, in part, by funding from the Rudd Center for Food Policy and Obesity (Dr. Henderson) and grants from the National Institutes of Health (K23 DK071646 (Dr. White) and K24 DK070052 (Dr. Grilo)).
Footnotes
Conflict of interest statement The authors declare that they have no conflict of interest.
Contributor Information
Patricia H. Rosenberger, Email: patricia.rosenberger@va.gov, VA Connecticut Healthcare System, 950 Campbell Ave. Psychology 116B, West Haven, CT 06516, USA. Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
Kathryn Elizabeth Henderson, Rudd Center for Food Policy and Obesity, Yale University, New Haven, CT, USA.
Marney A. White, Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
Robin M. Masheb, Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
Carlos M. Grilo, Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA. Department of Psychology, Yale University, New Haven, CT, USA
References
- 1.Grilo CM, Brownell KD, Stunkard AJ. The metabolic and psychological importance of exercise in weight control. In: Stunkard A, Wadden TA, editors. Obesity: theory and therapy. New York: Raven; 1993. pp. 253–73. [Google Scholar]
- 2.Jeffery RW, Wing RR, Sherwood NE, et al. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–89. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 3.Elavsky S, McAuley E. Physical activity and mental health outcomes during menopause: a randomized controlled trial. Ann Behav Med. 2007;33:132–42. doi: 10.1007/BF02879894. [DOI] [PubMed] [Google Scholar]
- 4.Wolin KY, Glynn RJ, Colditz GA, et al. Long-term physical activity patterns and health-related quality of life in U.S. women. Am J Prev Med. 2007;32:490–99. doi: 10.1016/j.amepre.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Livhits M, Mercado C, Yermilov I, et al. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20:657–65. doi: 10.1007/s11695-010-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity. 2009;17:78–83. doi: 10.1038/oby.2008.501. [DOI] [PubMed] [Google Scholar]
- 7.Elkins G, Whitfield P, Marcus J, et al. Noncompliance with behavioral recommendations following bariatric surgery. Obes Surg. 2005;15:546–51. doi: 10.1381/0960892053723385. [DOI] [PubMed] [Google Scholar]
- 8.Larsen J, Geenen R, van Ramshorst B, et al. Binge eating and exercise behavior after surgery for severe obesity: a structural equation model. Int J Eat Disord. 2006;39:369–75. doi: 10.1002/eat.20249. [DOI] [PubMed] [Google Scholar]
- 9.Godin G, Sheppard RJ. Godin leisure-time exercise questionnaire. Can J Appl Sport Sci. 1985;10:141–46. [Google Scholar]
- 10.Godin G, Amireault S, Belanger-Gravel A, et al. Prediction of leisure-time physical activity among obese individuals. Obesity. 2009;17:706–12. doi: 10.1038/oby.2008.599. [DOI] [PubMed] [Google Scholar]
- 11.Godin G, Shephard RJ. Godin leisure-time exercise questionnaire. Cited by Kriska AM, Caspersen CJ. A collection of physical activity questionnaires for health-related research. Suppl. Med Sci Sports. 1997;29:s36–8. [PubMed] [Google Scholar]
- 12.Beck AT, Steer RA. BDI beck depression inventory manual. San Antonio: Harcourt Brace; 1993. [Google Scholar]
- 13.Fechner-Bates S, Coyne JC, Schwenk TL. The relationship of self-reported distress to depressive disorders and other psychopathology. J Consult Clin Psychol. 1992;64:550–59. doi: 10.1037//0022-006x.62.3.550. [DOI] [PubMed] [Google Scholar]
- 14.Grilo CM, Masheb RM, Wilson GT. Subtyping binge eating disorder. J Consult Clin Psychol. 2001;69:1066–72. doi: 10.1037//0022-006x.69.6.1066. [DOI] [PubMed] [Google Scholar]
- 15.Svanborg P, Asborg M. A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Asberg Depression Rating Scale (MADRS) J Affect Disord. 2001;64:203–16. doi: 10.1016/s0165-0327(00)00242-1. [DOI] [PubMed] [Google Scholar]
- 16.Clark MM, Balsiger BM, Sletten CD, et al. Psychosocial factors and 2-year outcome following bariatric surgery for weight loss. Obes Surg. 2003;13:739–45. doi: 10.1381/096089203322509318. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Snow KK, Kosinski M, et al. SF-36 health survey manual and interpretation guide. Boston: New England Medical Center, The Health Institute; 1993. [Google Scholar]
- 18.McHorney CA, Kosinski M, Ware JE. Comparisons of the costs and quality of norms for the Sf-36 Health Survey collected by mail versus telephone interview—results from a national survey. Med Care. 1994;32:551–67. doi: 10.1097/00005650-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 19.McHorney CA, Ware JE, Lu JFR, et al. The MOS 36-item short-form health survey (Sf-36).3. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Evans RK, Bond DS, Wolfe LG, et al. Participation in 150 min/wk of moderate or higher intensity physical activity yields greater weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2007;3:526–30. doi: 10.1016/j.soard.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Elavsky S, McAuley E, Motl R, et al. Physical activity enhances long-term quality of life in older adults: efficacy, esteem, and affective influences. Ann Behav Med. 2003;30:138–45. doi: 10.1207/s15324796abm3002_6. [DOI] [PubMed] [Google Scholar]
- 22.Fox KR. The influence of physical activity on mental wellbeing. Public Health Nutr. 1999;2:411–18. doi: 10.1017/s1368980099000567. [DOI] [PubMed] [Google Scholar]
- 23.Sallis JF, Saelens JE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- 24.Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self-report vs. objective measures. Obesity. 2010 doi: 10.1038/oby.2010.88. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]


