Abstract
An indispensable role for the brain renin-angiotensin system (RAS) has been documented in most experimental animal models of hypertension. To identify the specific efferent pathway activated by the brain RAS that mediates hypertension, we examined the hypothesis that elevated arginine vasopressin (AVP) release is necessary for hypertension in a double-transgenic model of brain-specific RAS hyperactivity (the “sRA” mouse model). sRA mice experience elevated brain RAS activity due to human angiotensinogen expression plus neuron-specific human renin expression. Total daily loss of the 4-kDa AVP prosegment (copeptin) into urine was grossly elevated (≥8-fold). Immunohistochemical staining for AVP was increased in the supraoptic nucleus of sRA mice (∼2-fold), but no quantitative difference in the paraventricular nucleus was observed. Chronic subcutaneous infusion of a nonselective AVP receptor antagonist conivaptan (YM-087, Vaprisol, 22 ng/h) or the V2-selective antagonist tolvaptan (OPC-41061, 22 ng/h) resulted in normalization of the baseline (∼15 mmHg) hypertension in sRA mice. Abdominal aortas and second-order mesenteric arteries displayed AVP-specific desensitization, with minor or no changes in responses to phenylephrine and endothelin-1. Mesenteric arteries exhibited substantial reductions in V1A receptor mRNA, but no significant changes in V2 receptor expression in kidney were observed. Chronic tolvaptan infusion also normalized the (5 mmol/l) hyponatremia of sRA mice. Together, these data support a major role for vasopressin in the hypertension of mice with brain-specific hyperactivity of the RAS and suggest a primary role of V2 receptors.
Keywords: antidiuretic hormone, Vaprisol
activity of the local tissue renin-angiotensin system (RAS) within the brain has been implicated in the development and maintenance of elevated blood pressure in many forms of hypertension. Evidence specifically demonstrating a causal role for brain RAS activity in hypertension comes from various rodent models. These many models include peripheral angiotensin infusion models (46, 58, 77), both elevated (14) and suppressed (29, 38, 50) plasma renin models, psychogenic (42), cold exposure (61), renal injury (73), sleep apnea (12) models, transgenic TGR (mRen2)27 rats (62), and both Dahl salt-sensitive (29) and spontaneously hypertensive rats (SHR) maintained on high-salt diets (37, 47, 72). Two major mechanisms have been documented that account for the blood pressure effects of brain angiotensin. First, actions of the RAS within the supraoptic (SON) and paraventricular hypothalamic nuclei (PVN) stimulate the production and release of arginine vasopressin (AVP, also known as antidiuretic hormone, ADH, or argipressin) (4, 10, 17, 31, 51, 53, 62). Second, hindbrain and brain stem actions of the RAS alter baroreflex function and sympathetic output (22, 26). Interestingly, a population of AVP-expressing neurons project from the PVN to the hindbrain and spinal cord and appear to be involved in the regulation of sympathetic nervous activity (reviewed in Refs. 1, 10, 52), suggesting a possible AVP-mediated cross-talk between these two mechanisms.
Although some studies have failed to document a substantial role for AVP in blood pressure control in heterogenous groups of human subjects (49), AVP has been implicated as a significant contributor to blood pressure control in selected populations of humans (19, 48). Specifically, African Americans (3), the elderly (15), and patients with congestive heart failure (19) or chronic renal failure (2) all exhibit AVP-dependent hemodynamic changes (7). Importantly, these populations of humans all exhibit low levels of circulating renin (75). As low-renin hypertension accounts for a larger (27%) fraction of human essential hypertensives than high-renin hypertension (16%) (39), it is unclear whether therapeutic targeting of AVP may have been prematurely overlooked as an antihypertensive therapy for selected populations of hypertensive patients.
Together, these findings have led us to question whether the elevations in AVP are necessary to cause or maintain hypertension due to chronically elevated brain RAS activity and to probe the mechanism(s) of action of AVP in this context. We hypothesized that transgenic activation of the brain RAS would elevate plasma AVP, and that actions of AVP are required to induce hypertension by the brain RAS through some combination of vasoconstriction and altered renal function. To examine these hypotheses, we utilized a unique transgenic animal model previously developed in our laboratory (21, 54). This double-transgenic model (the “sRA” model) takes advantage of the species specificity of the renin-mediated cleavage of angiotensinogen to cause brain-specific hyperactivity of the RAS. We have previously demonstrated that these animals exhibit a robust chronic hypertension, polydipsia, polyuria, and an elevated resting metabolic rate. Importantly, we have also previously determined that sRA mice exhibit elevated plasma AVP levels and a suppression of the circulating RAS despite elevated renal sympathetic nerve activity (21). Here we demonstrate elevated neuronal AVP immunostaining (specifically in the supraoptic nucleus), increased daily secretion of AVP, robust desensitization of the vasculature of sRA mice to AVP, and the necessity of V2 AVP receptor signaling in the maintenance of hypertension and hyponatremia in this model. These findings highlight a major role for AVP in the hypertension of sRA mice.
MATERIALS AND METHODS
Animals.
All animal work was approved by the University of Iowa Animal Care and Use Committee and was performed in accordance with the National Institutes of Health “Guide for the Care and Use of Laboratory Animals.”
Double-transgenic (sRA) mice were generated as previously described (21, 54). Briefly, “sR” mice expressing human renin under transcriptional control by the neuron-specific synapsin promoter were bred with “A” mice expressing human angiotensinogen under transcriptional control by its own promoter (line 11110/2 × 4284/1). Because of the species specificity of the reaction, human angiotensinogen is only cleaved to form angiotensin I by human renin. Hyperactivity of the RAS is thereby restricted to sites of overlapping transgene expression in sRA offspring (i.e., subsections of the central nervous system that normally produce angiotensinogen).
Immunohistochemistry.
Immunohistochemical detection of AVP in the brain was performed on 50-μm thick sections using a rabbit polyclonal antibody to a synthetic peptide corresponding to the first six amino acids of arginine8-vasopressin (Phoenix Pharmaceuticals, Burlingame, CA). Sections were cut from six (3 sRA, 3 wild type) brains perfusion fixed with 4% paraformaldehyde and 0.5% glutaraldehyde and incubated in a 1:1,000 dilution of antibody for 24 h at 4°C. The brains of sRA mice were “notched” for identification and incubated with sections from wild-type animals. After incubation in a biotinylated goat anti-rabbit secondary antibody and avidin-horseradish peroxidase, immunoreactivity was detected using 3,3′-diaminobenzidine as a chromagen. On four sections from each animal, matched for rostrocaudal level, AVP-immunostained fragments larger than 10 μm were counted in the PVN and SON using ImageJ software from the NIH.
Blood pressure (tail-cuff).
Here we first examined blood pressure in sRA mice using a Visitech Systems BP-2000 tail-cuff blood pressure monitoring system, as previously described (59). Briefly, animals were acclimated to warmed restraint boxes daily for 1 wk. Once acclimated, 30 measurements of systolic blood pressure were averaged from each animal daily for 2 wk to assess baseline blood pressure. Conivaptan (Vaprisol, YM 087, 22 ng/h sc, Baxter Healthcare) or tolvaptan (OPC-41061, 22 ng/h sc, Sigma Aldrich) was delivered to distinct subsets of mice by osmotic minipump (model 1004, Alzet). After osmotic minipump implantation, pressures were recorded daily for 10 days to assess drug effects.
Blood pressure (telemetry).
Radiotelemetric blood pressures were recorded from the carotid artery essentially as previously reported (21). Briefly, a telemeter probe (DSI, model TA11PA-C10) was inserted into the common carotid artery under ketamine-xylazine anesthesia. After >2 days of recovery, blood pressure, heart rate, and spontaneous physical activity were recorded for 30 s every 5 min using the Dataquest program (DSI). After baseline recordings, mice were chronically delivered conivaptan and tolvaptan via osmotic minipump that was implanted through an interscapular incision into the subcutaneous space of the back under isoflurane anesthesia.
Aortic vascular reactivity.
Abdominal aortic rings were assessed for vascular reactivity as previously described (24). Briefly, mice were euthanized by overdose of pentobarbital (50 mg ip), and the abdominal aorta was quickly removed and placed in Krebs buffer containing (in mmol/l) 118.3 NaCl, 4.7 KCl, 1.2 MgSO4, 1.2 KH2PO4, 25 NaHCO3, 2.5 CaCl2, and 11 glucose. Vascular rings (4–5 mm in length) were suspended in oxygenated Krebs buffer (95% O2-5% CO2) in organ baths at 37°C and connected to a force transducer via steel hooks. Resting tension was adjusted to 0.5 grams over 45 min. Contractile responses were tested in response to AVP (10−10-10−6 mol/l), phenylephrine (PE, 10−8-3 × 10−5), endothelin-1 (ET-1, 10−10-10−7), prostaglandin F2α (PGF2α, 10−7-10−4), and angiotensin II (ANG II, 10−10-10−7). After submaximal contraction with PGF2α (40–50% of max; 3 × 10−6-6 × 10−6), relaxation responses to acetylcholine (10−8-3 × 10−5) and sodium nitroprusside (10−9-10−5) were determined.
Mesenteric artery vascular reactivity.
Secondary branches of mesenteric artery were dissected and placed in chilled oxygenated (21% O2-5% CO2-74% N2) Krebs buffer. A segment (∼1 mm long) of artery was transferred to a vessel chamber (DMT), cannulated with glass micropipettes, and secured with silk ligatures. The artery was slowly pressurized to 40 mmHg without flow. After 30 min equilibration, vessel viability was tested by constriction response to 100 mM KCl. Vascular responses to PE (10−9-10−5 mol/l), AVP (10−12-10−7 mol/l), and ET-1 (10−11-10−8 mol/l) were then assessed. The artery was then superfused with calcium-free Krebs buffer containing 10−5 mol/l sodium nitroprusside and 2 mmol/l EGTA to maximally dilate the vessel. Internal and external diameters were measured at 75 mmHg. Wall thickness, media-to-lumen ratio, and cross-sectional area (CSA) were calculated as previously described by Neves et al. (45).
Gene expression.
Mesenteric arteries (superior mesenteric artery excluded) and kidneys were snap frozen in liquid nitrogen and RNA was extracted in TRIzol. Total RNA was isolated using an RNA Purelink Minikit (Invitrogen) following the manufacturer's protocol. Concentrations were determined using a NanoDrop ND-1000 spectrophotometer. cDNA was generated by RT-PCR using SuperScript III (Invitrogen). qRT-PCR was performed using TaqMan gene expression assays (Applied Biosystems): RGS2 (Mm00501385_m1), RGS5 (Mm00501393_m1), V1A (Mm00444092_m1), ETA (Mm01243722_m1), GAPDH (4352932E), or SYBR-green assays (primer sequences in Table 1: NKCC2, NCC, NHE3, ENaC-α, ENaC-β, ENaC-γ, NKA-α, V2R, AQP1, AQP2, AQP3, AQP4, PGES, and UT1-A) normalized against β-actin. SYBR-green reagents from Bio-Rad were utilized, and all real time reactions were performed on a Bio-Rad iQ5 iCycler.
Table 1.
SYBR green primer sequences for quantitative PCR
| Gene | Primer Sequences |
|---|---|
| NKCC2A | Forward: 5′-CCATGGTAACCTCTATCACTGGGT-3′ |
| Reverse: 5′-TCAAGCCTATTGACCCACCGAACT-3′ | |
| NCC | Forward: 5′-AAGTCGGGTGGCACCTATTTCCTT-3′ |
| Reverse: 5′-TTACGGTTTCTGCAAAGCCCACAG-3′ | |
| NHE3 | Forward: 5′-TCCTCTCAGCCATTGAGGACATCT-3′ |
| Reverse: 5′-ACTTTGCTGAGGAACTTCCGGTCA-3′ | |
| ENaCα | Forward: 5′-ACAATGGTTTGTCCCTGACACTGC-3′ |
| Reverse: 5′-TCACGTTGAAGCCACCATCATCCA-3′ | |
| ENaCβ | Forward: 5′-TCTGCCAACCCTGGGACTGAATTT-3′ |
| Reverse: 5′-TGGCATAGATGCCCTCCTCTCTAA-3′ | |
| ENaCγ | Forward: 5′-GCCAATCAGTGTGCAAGCAATCCT-3′ |
| Reverse: 5′-TTATTTGCTGGCTTTGGTCCCAGG-3′ | |
| Na-K-ATPase-α | Forward: 5′-TGAAGCTGACACCACGGAGAATCA-3′ |
| Reverse: 5′-TGCCGCTTAAGAATAGGCAGGTT-3′ | |
| V2R | Forward: 5′-TGTGATTGTCTACGTGCTGTGCTG-3′ |
| Reverse: 5′-GGGTTGGTACAGCTGTTAAGGCTA-3′ | |
| AQP1 | Forward: 5′-CTGGGCATTGAGATCATTGGCACT-3′ |
| Reverse: 5′-TGATACCGCAGCCAGTGTAGTCAA-3′ | |
| AQP2 | Forward: 5′-TAGCCCTGCTCTCTCCATTGGTTT-3′ |
| Reverse: 5′-AAACTTGCCAGTGACAACTGCTGG-3′ | |
| AQP3 | Forward: 5′-ATGGTGGCTTCCTCACCATCAACT-3′ |
| Reverse: 5′-AGGAAGCACATTGCGAAGGTCACA-3′ | |
| AQP4 | Forward: 5′-TGCCAGCTGTGATTCCAAACGAAC-3′ |
| Reverse: 5′-TCCCATGATAACTGCGGGTCCAAA-3′ | |
| PGES | Forward: 5′-TTTGCAACAAGTACTGGCCCATGC-3′ |
| Reverse: 5′-TGTTCGGTACACGTTGGGAGAGAT-3′ | |
| UT1-A | Forward: 5′-CACTGGCGACATGAAGGAATGCAA-3′ |
| Reverse: 5′-GGGTTGTTGACAAACATCACCTGAGC-3′ | |
| β-Actin | Forward 5′-CATCCTCTTCCTCCCTGGAGAAGA-3′ |
| Reverse 5′-ACAGGATTCCATACCCAAGAAGGAAGG-3′ |
See text for abbreviations and more information.
Blood and urine analyses.
Plasma was obtained by collecting whole blood by submandibular bleed into lithium-heparin-coated tubes, then centrifuged at 5,000 g for 5 min, and the supernatant transferred to a fresh tube and frozen at −80°C until analysis. Urine was collected using Nalgene single-mouse metabolism cages as previously described (21). Copeptin was measured using an ELISA kit (USCN Life Sciences) according to the manufacturer's instructions. Blood chemistries and urine creatinine were determined using a handheld iSTAT clinical chemistry analyzer (Abbott), with CHEM8+ cartridges. Urine protein was determined using a bicinchoninic acid assay kit (Thermo Fisher/Pierce), according to the manufacturer's instructions.
Statistics.
Data were analyzed by ANOVA with repeated measures as appropriate. Post hoc analyses were performed using Bonferroni multiple-comparisons procedures. EC50 and maximum response calculations were performed by fitting individual dose-response data sets to a four-parameter logistic function (Hill slope method); y = min + (max − min)/[1 + (x/EC50)^Hill slope]. All mRNA-fold changes were calculated using the Livak method (40). All analytical comparisons were performed using SigmaStat/SigmaPlot (Systat). All data are presented as means ± SE.
RESULTS
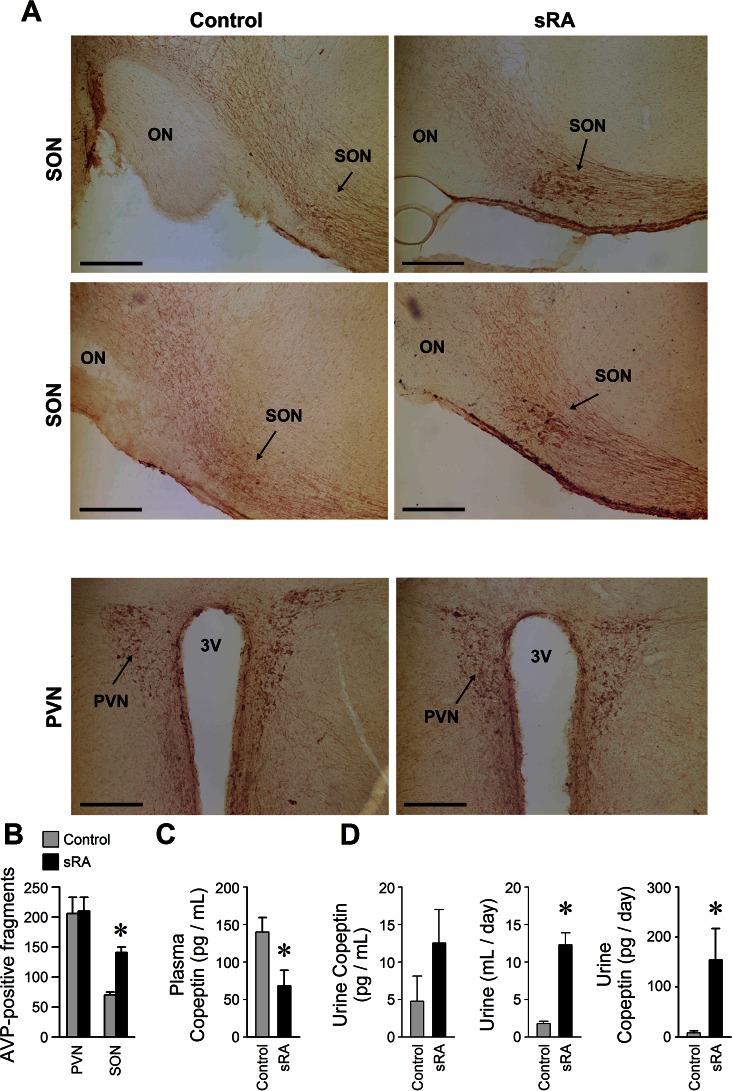
In both sRA and wild-type animals, AVP immunoreactivity was observed in the cells in the suprachiasmatic (SCN), SON, PVN, and circular nuclei of the hypothalamus as expected (32, 70). AVP-immunoreactive fibers were traceable from the SON and PVN to the median eminence (Fig. 1A). Though there was no obvious difference in the numbers of AVP immunoreactive neurons in the SCN and PVN between sRA and wild-type animals, neuronal and fiber immunoreactivity was consistently denser in the sRA animals. The most striking difference between sRA and control animals was the doubling of the number of AVP immunoreactive neurons detected in the retrochiasmatic part of the SON in sRA animals (Fig. 1, A and B) compared with the retrochiasmatic SON in wild-type animals.
Fig. 1.
Elevated vasopressin in sRA mice. A: arginine vasopressin (AVP) immunoreactivity in the supraoptic (SON, top and middle rows, from four separate animals) and paraventricular (PVN, bottom row, from two separate animals) nuclei in female sRA and control animals. Note the increased numbers of strongly immunoreactive AVP neurons in the retrochiasmatic part of the SON in sRA animals. ON, optic tract; 3V, third ventricle. Bars = 200 μm. B: total immunoreactive cell fragments per side, greater than 10 μm in diameter, in four serial sections (spaced 200 μm apart) through the PVN and SON of littermate control and sRA mice (n = 3 females each group). C: plasma copeptin levels (n = 4 male + 4 female control, 4 male + 4 female sRA). D: urine copeptin concentration, total daily urine volume, and total daily copeptin loss into urine (n = 12 male + 5 female control, 10 male + 7 female sRA). All data are means ± SE. *P < 0.05 vs. control.
Copeptin is the COOH-terminal fragment of the fully translated AVP proprotein and is therefore translated in a 1:1 molar ratio with AVP. Because it exhibits a far greater biological half-life than AVP, it has been proposed as a more reliable measure of chronic AVP release than AVP itself (63). Copeptin levels were significantly reduced in plasma from sRA mice (Fig. 1C). Because of its small size (38 amino acids, 4.22 kDa), however, this protein is rapidly cleared from the plasma by the kidneys. Copeptin concentrations appeared elevated in the urine from sRA mice, though the difference was not significantly different. After we accounted for the grossly elevated (∼7-fold) urine production rate of sRA mice, however, it is clear that the total daily copeptin clearance into urine is grossly elevated in sRA mice (∼20-fold, Fig. 1D). These data together indicate that there is an approximate 20-fold increase in AVP secretion in sRA mice. This large difference in total daily copeptin loss to urine was still present (8-fold) after normalization for total daily urine creatinine (creatinine: control, 0.20 ± 0.03 vs. sRA, 0.40 ± 0.05 mg/day, P < 0.01, and copeptin/creatinine: control, 49 ± 36 vs. sRA, 406 ± 176 pg/mg, P = 0.05) or (10-fold) after normalization total daily urine protein (protein: control, 41 ± 4 vs. sRA, 86 ± 9 mg/day, P < 0.01, and copeptin/protein: control, 180 ± 100 vs. sRA, 1,845 ± 665 mg/mg, P = 0.02).
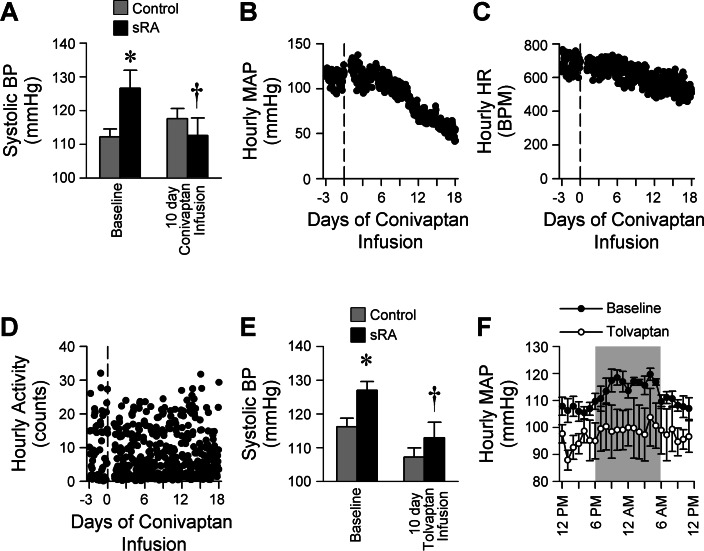
Under baseline conditions, sRA mice exhibited a hypertension that was easily detectable by tail-cuff (Fig. 2A). These data replicate our previously published measures of hypertension in this model, as determined by direct cannulas and by radiotelemetry (21, 54). Chronic subcutaneous infusion of the nonselective, nonpeptide AVP V1A/V2 receptor antagonist conivaptan resulted in a complete normalization of the hypertension in sRA mice. Continuous recording of blood pressures in an exemplar sRA mouse at baseline and during 18 days of continuous subcutaneous conivaptan infusion documented a gradual but substantial reduction in blood pressure (Fig. 2B) that was paralleled by a slight reduction in heart rate (Fig. 2C). Importantly, spontaneous physical activity remained normal throughout the recording period, suggesting that the animal was not lethargic or otherwise ill due to the surgery and conivaptan infusion (Fig. 2D).
Fig. 2.
Blood pressure responses to vasopressin receptor antagonists. A: systolic blood pressure (BP), monitored by tail-cuff, at baseline and with 10 days of chronic subcutaneous infusion (22 ng/h) of the V1A/V2 nonpeptide antagonist conivaptan (n = 2 male + 4 female control, 2 male + 4 female sRA). Hourly telemetric blood pressure (B, MAP) and heart rate (C, HR) recordings for 3 days preceding and 18 days during subcutaneous infusion of the nonselective V1A/V2 receptor antagonist conivaptan (22 ng/h) in a female sRA mouse are shown. D: spontaneous ambulatory physical activity counts during conivaptan infusion experiment (in B and C). E: systolic BP, monitored by tail-cuff, at baseline and with 10 days of chronic subcutaneous infusion (22 ng/h) of the V2-selective antagonist tolvaptan (n = 4 male + 5 female control, 4 male + 6 female sRA). F: hourly average radiotelemetric MAP recordings from (n = 4 female) sRA mice at baseline and after 10 days of subcutaneous tolvaptan infusion (Drug × Time, P = 0.029). All data are means ± SE. *P < 0.05 vs. control, †P < 0.05 vs. baseline sRA.
To dissect the relative contributions of various vasopressin receptor subtypes in the hypertension of sRA mice, we next examined the blood pressure consequences of chronic subcutaneous infusion of the V2-selective antagonist tolvaptan. Chronic infusion of tolvaptan caused a nearly identical normalization of blood pressure (Fig. 2E) to that observed with conivaptan (Fig. 2A). Importantly, this blood pressure reduction was confirmed in a cohort of sRA mice tested using radiotelemetry (Fig. 2F).
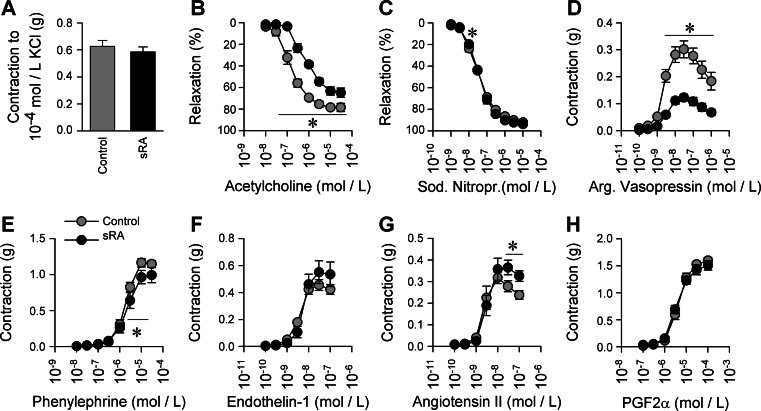
Additional evidence for chronic hypertension and vasopressin-specific changes in sRA mice comes from vascular reactivity assays. First, abdominal aortic rings were examined ex vivo for reactivity to selected vasoconstrictor and vasodilator compounds. Aortic rings from sRA mice exhibited normal constrictor responses to potassium chloride (Fig. 3A). Abdominal aortic rings exhibited a robust rightward shift in responses to the vasodilator acetylcholine (Table 2), but normal responses to sodium nitroprusside, indicating endothelial dysfunction typical in chronic hypertension models (Fig. 3, B and C). Supporting a chronic elevation in AVP levels, abdominal aortas from sRA mice exhibited a robust suppression of constrictor responses to AVP (Fig. 3D), reflected both in a trend toward a rightward (reduced) potency shift and a significant suppression of maximal response (Table 2). No potency or efficacy changes were observed in contractile responses to PE, ET-1, ANG II, or PGF2α (Fig. 3, E–H), suggesting AVP-specific changes in the sRA vasculature.
Fig. 3.
Vascular reactivity of abdominal aorta. A: maximum contractile response to 100 mmol/l KCl. B and C: relaxation responses to graded doses of acetylcholine and sodium nitroprusside after half-maximal contraction to PGF2α. D–H: contractile responses to graded doses of arginine vasopressin, phenylephrine, endothelin-1, angiotensin II, and prostaglandin-F2α (PGF2α) (n = 6 male control, 5 male sRA). All data are means ± SE. *P < 0.05 vs. control.
Table 2.
Potency and efficacy analyses of various vasoactive compounds in abdominal aortas and 2°-branch mesenteric artery of male sRA and control littermate mice
| EC50 |
Maximum Response |
|||
|---|---|---|---|---|
| Compound | Control | sRA | Control | sRA |
| Abdominal aorta | nmol/l | nmol/l | g | g |
| Phenylephrine | 1,900 ± 250 | 2,430 ± 620 | 1.18 ± 0.05 | 1.02 ± 0.10 |
| Angiotensin II | 2.26 ± 0.45 | 4.24 ± 1.14 | 0.32 ± 0.03 | 0.38 ± 0.03 |
| Arginine vasopressin | 2.19 ± 0.19 | 3.72 ± 0.73* | 0.29 ± 0.03 | 0.12 ± 0.01† |
| Prostaglandin F2α | 4,600 ± 750 | 3,600 ± 290 | 1.59 ± 0.06 | 1.50 ± 0.10 |
| Endothelin-1 | 3.40 ± 0.33 | 5.19 ± 0.93 | 0.45 ± 0.04 | 0.55 ± 0.09 |
| nmol/l | nmol/l | % | % | |
| Acetylcholine | 130 ± 35 | 879 ± 298* | 78.9 ± 3.3 | 70.4 ± 8.9 |
| Sodium nitroprusside | 29.4 ± 3.7 | 34.2 ± 1.7 | 91.5 ± 0.5 | 93.5 ± 0.8 |
| Mesenteric artery | nmol/l | nmol/l | % | % |
| Phenylephrine | 1,460 ± 660 | 560 ± 80 | 67.3 ± 3.0 | 64.5 ± 4.1 |
| Arginine vasopressin | 0.57 ± 0.15 | 15.89 ± 13.46 | 52.5 ± 3.2 | 17.3 ± 6.5† |
| Endothelin-1 | 1.68 ± 0.43 | 0.45 ± 0.17* | 67.8 ± 4.3 | 58.0 ± 4.6 |
Data are presented as means ± SE. Aortas: Control, n = 6; sRA, n = 5. Mesenteric artery: Control, n = 6; sRA, n = 6.
P ≤ 0.05, and
P ≤ 0.001 vs. Control.
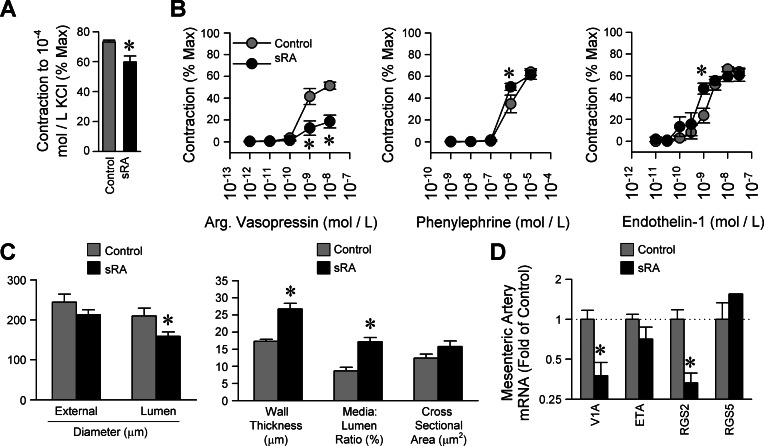
Acknowledging that smaller arteries are important in controlling peripheral resistance, vascular reactivity of second-order branches of mesenteric arteries were next examined using pressurized myography. Mesenteric artery branches exhibited a significant reduction in contractile response to potassium chloride (Fig. 4A); however, normalization of other constrictor responses to this lower KCl response in sRA mice had no qualitative effect on data interpretation (not shown). Similar to abdominal aortic rings, mesenteric arteries from sRA mice exhibited a trend toward a rightward shift and a substantial suppression of maximal response (Table 2) to AVP (Fig. 4B). Mesenteric arteries exhibited normal contractile responses to PE, with no change in efficacy or potency. In response to ET-1, mesenteric arteries from sRA mice exhibited a normal maximal response and a small but statistically significant leftward potency shift. These data confirm an AVP-specific desensitization in smaller arteries of sRA mice, further supporting the conclusion that AVP is chronically elevated in sRA mice.
Fig. 4.
Mesenteric artery vascular reactivity. A: maximum contractile response to 100 mmol/l KCl. B: contractile responses to graded doses of arginine vasopressin, phenylephrine, and endothelin-1 (n = 6 male control, 6 male sRA). C: external and lumen diameters, wall thickness, media-to-lumen ratio, and cross-sectional area of mesenteric arteries maintained at 75 mmHg lumen pressure, in calcium-free conditions. D: mesenteric artery mRNA expression of the AVP V1A receptor, the endothelin-1 ETA receptor, RGS2, and RGS5 (V1A, RGS2, and RGS5; n = 4 male + 5 female control, 4 male + 3 female sRA. ETA, n = 4 male control, 4 male sRA). All data are means ± SE. *P < 0.05 vs. control.
Mesenteric arteries from sRA mice exhibited substantial eutrophic inward remodeling, providing further evidence of chronic hypertension in this model. While no difference in external diameter was detected between control and sRA mice (Fig. 4C), lumen diameter was significantly smaller in sRA mice because of increased wall thickness. This resulted in an increased media-to-lumen ratio but no significant change in cross-sectional area.
To explain the reduced vascular reactivity to AVP, we next measured expression of the V1A receptor. Mesenteric arteries from sRA mice exhibited significantly suppressed V1A receptor mRNA but no change in ETA receptor expression (Fig. 4D). Furthermore, there was a selective downregulation of regulator of G protein signaling-2 (RGS2) expression but no change in RGS5 expression.
In contrast to vascular V1A downregulation, renal V2 receptors and aquaporin-2 mRNA levels were unchanged in sRA mice (Table 3). The only renal transporter that showed significant changes in expression in sRA mice was the sodium-chloride cotransporter (NCC, 5-fold of control, P < 0.05), though the sodium/hydrogen exchanger (NHE) showed a trend toward reduction (NHE3, 0.6-fold of control, P = 0.08) and the ENaC-α subunit showed a trend toward elevation (ENaC-α, 10-fold of control, P = 0.08). It should be noted that these renal gene expression assays were performed on only male sRA and littermate control mice, and the statistical power is low due to a small number of replicates per group (n = 4 each). Thus it is possible that the changes in NHE3 and ENaC-α may both be physiologically significant.
Table 3.
Renal expression of selected receptors and transporters in sRA and littermate control mice
| Gene | Control (n = 4) | sRA (n = 4) | t-Test P Value |
|---|---|---|---|
| AVPR2 | 1.000 (0.840–1.191) | 0.778 (0.583–1.038) | 0.425 |
| NCC | 1.000 (0.736–1.359) | 5.232 (3.850–7.112) | 0.009 |
| NHE3 | 1.000 (0.825–1.212) | 0.605 (0.522–0.701) | 0.075 |
| NKCC2 | 1.000 (0.632–1.581) | 0.621 (0.415–0.929) | 0.464 |
| ENaCα | 1.000 (0.468–2.135) | 10.021 (4.556–22.041) | 0.080 |
| ENaCβ | 1.000 (0.657–1.522) | 0.596 (0.282–1.263) | 0.611 |
| ENaCγ | 1.000 (0.669–1.495) | 1.682 (1.120–2.525) | 0.398 |
| Na-K-ATPase-α | 1.000 (0.620–1.613) | 0.819 (0.553–1.215) | 0.744 |
| AQP1 | 1.000 (0.610–1.640) | 0.643 (0.511–0.808) | 0.441 |
| AQP2 | 1.000 (0.747–1.338) | 0.541 (0.440–0.665) | 0.133 |
| AQP3 | 1.000 (0.636–1.571) | 0.317 (0.192–0.524) | 0.640 |
| AQP4 | 1.000 (0.397–2.521) | 0.483 (0.237–0.983) | 0.506 |
| PGES | 1.000 (0.779–1.283) | 0.616 (0.237–1.597) | 0.164 |
| UT1-A | 1.000 (0.486–2.057) | 0.569 (0.406–0.799) | 0.643 |
Data are presented as fold-of-control; means ± SE. See text for abbreviations and more information.
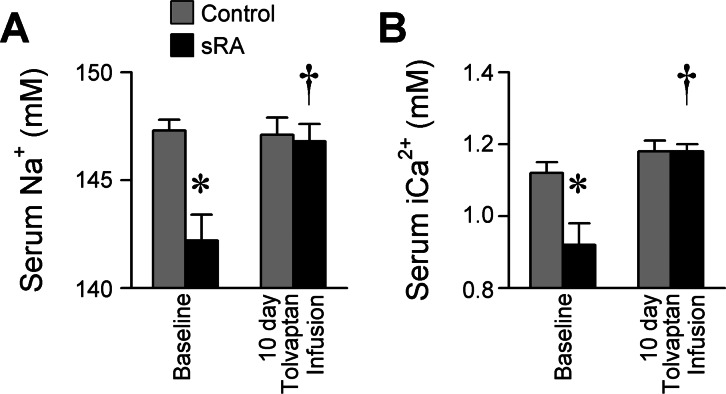
Finally, to more directly probe a V2-mediated mechanism in the cardiovascular phenotypes of sRA mice, we examined blood chemistry responses to tolvaptan (Table 4). We previously documented an approximate 4 mM hyponatremia in sRA mice under baseline conditions (21). Here we determined that sRA mice were hyponatremic (Fig. 5A) and hypocalcemic (Fig. 5B), and chronic tolvaptan delivery corrected both of these imbalances (genotype × drug interaction P < 0.05 for both). sRA mice also exhibited alterations in chloride, total CO2, glucose, blood urea nitrogen, creatinine, hematocrit, and anion gap, and whereas tolvaptan treatment did affect some of these endpoints (potassium, chloride, and blood urea nitrogen), it did so in a manner independent of genotype as no genotype × drug interactions were uncovered (Table 4).
Table 4.
Blood chemistry at baseline or following tolvaptan infusion in sRA and control littermate mice
| Females |
Males |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline |
Tolvaptan |
Baseline |
Tolvaptan |
|||||
| Parameter | Control (n = 12) | sRA (n = 8) | Control (n = 5) | sRA (n = 6) | Control (n = 8) | sRA (n = 5) | Control (n = 4) | sRA (n = 4) |
| Females | ||||||||
| Age, wk | 23.5 ± 0.1 | 23.6 ± 0.2 | 22.7 ± 0.2 | 22.6 ± 0.2 | 19.4 ± 1.1 | 18.5 ± 1.3 | 22.5 ± 0.3 | 22.5 ± 0.3 |
| Sodium, mMG, T, G×T | 147.3 ± 0.7 | 142.6 ± 1.2 | 146.2 ± 0.7 | 146.3 ± 0.7 | 147.4 ± 0.9 | 141.4 ± 2.8 | 148.3 ± 1.3 | 147.5 ± 1.9 |
| Potassium, mMT | 6.6 ± 0.3 | 6.5 ± 0.5 | 6.4 ± 0.1 | 5.3 ± 0.3 | 6.5 ± 0.5 | 6.8 ± 0.7 | 6.6 ± 0.5 | 5.4 ± 0.1 |
| Chloride, mMG, S, T | 115.7 ± 1.0 | 110.3 ± 1.7 | 112.4 ± 0.5 | 105.2 ± 1.6 | 119.4 ± 2.0 | 115.8 ± 2.2 | 115.5 ± 0.3 | 107.0 ± 2.7 |
| Ionized calcium, mMG, T, G×T | 1.15 ± 0.04 | 1.01 ± 0.04 | 1.19 ± 0.05 | 1.18 ± 0.03 | 1.07 ± 0.06 | 0.78 ± 0.12 | 1.18 ± 0.04 | 1.18 ± 0.03 |
| Total CO2, mMG, T | 18.4 ± 1.1 | 21.6 ± 2.1 | 24.0 ± 1.1 | 28.8 ± 1.7 | 17.0 ± 1.2 | 18.8 ± 1.7 | 24.0 ± 0.8 | 26.0 ± 3.4 |
| Glucose, mg/dlG, S×T | 215 ± 8 | 193 ± 16 | 190 ± 13 | 136 ± 15 | 196 ± 11 | 155 ± 16 | 182 ± 7 | 181 ± 28 |
| BUN, mg/dlG, T | 22.4 ± 1.5 | 42.4 ± 4.9 | 18.4 ± 0.9 | 24.5 ± 1.7 | 28.5 ± 4.0 | 40.8 ± 9.0 | 21.5 ± 0.9 | 27.3 ± 2.1 |
| Creatinine, mg/dlG* | 0.21 ± 0.01 | 0.33 ± 0.06 | 0.24 ± 0.02 | 0.33 ± 0.04 | 0.21 ± 0.01 | 0.24 ± 0.02 | 0.25 ± 0.03 | 0.30 ± 0.04 |
| Hematocrit, %RBCG, G×S | 45.8 ± 0.5 | 52.6 ± 0.6 | 45.4 ± 0.7 | 49.8 ± 1.1 | 43.8 ± 0.7 | 52.6 ± 0.9 | 43.8 ± 1.1 | 52.0 ± 1.1 |
| Anion gap, mMG, G×S | 21.2 ± 0.6 | 18.4 ± 1.0 | 17.0 ± 1.5 | 18.5 ± 0.7 | 18.3 ± 1.4 | 14.8 ± 4.4 | 16.3 ± 0.5 | 21.0 ± 2.4 |
Values are means ± SE. Three-way ANOVA results: GP < 0.05 main effect of genotype, SP < 0.05 main effect of sex, TP < 0.05 main effect of tolvaptan (22 ng/h, 10 days sc), G×SP < 0.05 genotype × sex interaction, G×TP < 0.05 genotype × tolvaptan interaction, S×TP < 0.05 sex × tolvaptan interaction.
Lower detection limit for creatinine assay was 0.20 mg/dl; values below detection were assigned value of 0.20. All end points were evaluated from cheek capillary blood collected in lithium-heparin coated tubes and tested using CHEM8+ cartridges in an iSTAT handheld chemistry analyzer (Abbott Labs).
Fig. 5.
Serum electrolytes. A: serum sodium concentration. B: serum-ionized calcium concentration (baseline: n = 8 male and 12 female control, 5 male and 8 female sRA; tolvaptan: n = 4 male and 5 female control, 4 male and 6 female sRA). All data are means ± SE. *P < 0.05 vs. control, †P < 0.05 vs. baseline sRA.
DISCUSSION
Here we examined a unique double-transgenic mouse model to test the hypothesis that AVP is required for the hypertension induced by the brain RAS. Immunohistochemical examination of the brain revealed elevated AVP levels in the retrochiasmatic part of the supraoptic hypothalamic nucleus but no consistent change in PVN immunostaining in sRA mice. Confirming a required role for AVP signaling in the hypertension, chronic blockade of vasopressin V1A/V2 receptors resulted in normalization of blood pressure in sRA mice. While vascular reactivity in multiple arteries to PE, ET-1, ANG II, and PGF2α were largely unchanged in sRA mice, responses to AVP were greatly desensitized. Selective inhibition of V2 receptors had a potent antihypertensive action in sRA mice and normalized the hyponatremia typical of this model. Together, these data strongly support a required role for AVP, acting at V2 receptors, in the maintenance of brain RAS-derived hypertension.
Increased AVP signaling has been suggested as a mechanism for the hypertension in many models. Mice with either tightly regulated or strongly overexpressed transgenic hyperactivity of the RAS throughout the body require elevated AVP signaling to maintain hypertension (13, 44). Deoxycorticosterone acetate (DOCA)-salt hypertension, which is dependent on elevated brain RAS activity (31, 38, 50), also depends on AVP signaling. DOCA-salt treatment results in elevated plasma AVP levels (11, 41, 43, 69). Intracerebroventricular infusion of the angiotensin-converting enzyme inhibitor captopril into rats both prevented and reversed DOCA-salt hypertension and was associated with a reduction in plasma vasopressin levels despite a reduced blood pressure (31). The dependence of DOCA-salt hypertension on AVP has also been demonstrated using AVP-deficient Brattleboro rats, as the hypertensive effects of DOCA-salt are greatly diminished in these animals (11, 76). Complimenting these findings from various hypertensive models, TGR(ASrAOGEN) rats, which exhibit reduced glial production of angiotensinogen, are hypotensive and have reduced plasma AVP levels (56). These animals also exhibit altered patterns of AVP V1A receptor expression within the brain (9), further supporting a brain RAS-AVP interaction. Mice deficient for the V1A AVP receptor are hypotensive, though the relative importance of brain, vascular, cardiac, thrombocyte, and hepatic receptors is unclear (1, 36).
Effects of the RAS on the production and release of AVP were reported as early as 1970, when Bonjour and Melvin (4) demonstrated that peripherally administered renin or angiotensin II resulted in dose-dependent increases in plasma AVP in dogs. Evidence for direct actions of angiotensin on AVP release within the brain was provided by ex vivo experiments using isolated rat neurohypophysis (17). Electrolytic lesion of the subfornical organ (30) or transection of efferent projections from the subfornical organ (35) both attenuate the release of AVP into the plasma in response to intravenous ANG II. Thus the demonstrations here of elevated brain AVP staining and increased daily copeptin (and thereby AVP) release in sRA transgenic mice were expected. Further work is required to causally link specific RAS receptor subtypes to the AVP elevation, as morphological and functional evidence support roles for both AT1 and AT2 receptors in AVP release (reviewed in Ref. 10).
The strongly increased AVP immunoreactivity in the SON implicates ANG II-mediated hyperactivity in the supraoptic-neurohypophysial pathway as leading to elevated AVP in sRA mice. ANG II injections into the SON depolarize neurosecretory cells (70), ANG II-immunoreactive neurons and axon terminals are found in the rodent SON intermingled with AVP immunoreactive neurons, and ANG II and AVP are colocalized in some neurons (32). It is thus likely that local production and/or actions of ANG II within the SON regulate AVP production and secretion.
AVP is an endogenous agonist for at least four subtypes of receptors. The V1A receptor subtype is primarily found in the vasculature, signals primarily through Gαq, and mediates vasoconstriction. V1A receptors are also present in neurons and appear to signal through cAMP to regulate neuronal function (1, 68). The V1B receptor subtype is primarily found in the brain, signals through Gαq, and stimulates adrenocorticotropic hormone. The V2 receptor subtype is primarily found in the collecting duct of kidney nephrons, signals through Gαs, and stimulates water reabsorption through aquaporin mobilization. There is some evidence for expression of V2 receptors in extrarenal tissues such as lung (16) and cerebellum (33), though their physiological significance in these tissues is unclear. Finally, AVP is also an agonist at the VACM-1 receptor, also known as Cullin-5, where it elicits calcium mobilization in endothelial cells and renal collecting ducts (5, 6). Our determination that mesenteric artery V1A receptors were downregulated in sRA mice but renal V2 receptor expression was unchanged may suggest a greater role for AVP-mediated renal water retention in the hypertension of sRA mice. Though not directly tested herein, this conclusion is supported by the slow time course for the effects of conivaptan (several days of infusion to see an effect, Fig. 2B), the antihypertensive effects of tolvaptan (Fig. 2, E and F), and the normalization of baseline hyponatremia and hypocalcemia in this model (Table 4 and Fig. 5) that are typical of the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) (18).
RGS2 is expressed throughout the cardiovascular system and acts to negatively regulate Gαq-mediated GPCR signaling, and therefore oppose vasoconstrictor responses (57). Studies in human patients have revealed a negative correlation between RGS2 expression and blood pressure, with hypertensive patients showing reduced RGS2 expression and hypotensive patients exhibiting elevated RGS2 expression (28, 57, 71). A similar correlation is observed in hypertensive animal models (9) and was again observed in the present study (Fig. 4D). RGS2 is known to be regulated in a tissue-specific manner, and within cardiovascular tissues RGS2 is controlled through multiple biphasic mechanisms (74). Acute activation of Gαq by various hormone/receptor combinations upregulates RGS2 rapidly, possibly to serve as a negative feedback mechanism. In contrast, chronic stimulation of Gαq systems appears to cause a tonic suppression of RGS2 expression (9, 67, 74). Mice deficient for RGS2 exhibit robust hypertension due to chronic increases in peripheral vasoconstriction (25, 27). Vasopressin-induced calcium transients in vascular smooth muscle cells from RGS2 knockout mice are augmented, highlighting the relationship between RGS2 and AVP signaling, presumably through V1A receptors (65) as these receptors utilize Gαq signaling (1, 68). RGS2 knockout mice also exhibit substantially greater end-organ damage from chronic hypertension than do wild-type animals (60). RGS2 also attenuates cAMP signaling in the kidney through modulation of adenylyl cyclases (23, 64), which may result in modulation of AVP signaling through V2 receptors, Gαs, and cAMP. Indeed, modulation of RGS2 greatly affects renal V2 receptor signaling and the renal effects of AVP in vivo (55). Thus it is tempting to speculate that modulation of RGS2 in various tissues, along with elevated AVP signaling, may contribute to the maintenance of hypertension in the context of chronically elevated brain RAS activity.
Differential regulation patterns for V1A receptors and V2 receptors in pathological states have previously been described. Góźdź et al. (20) previously demonstrated that in the TGR(mRen2)27 rat model of high-renin hypertension, cardiac V1A receptors are upregulated compared with control Sprague-Dawley rats, while renal V2 receptors are unchanged between strains. Trinder et al. (66) previously demonstrated that in the streptozotocin-injection model of Type 1 diabetes mellitus, rats exhibited reduced hepatic and renal expression of V1 receptors and AVP-induced inositol phosphate production, while renal V2 receptors and AVP-induced cAMP production are again unchanged. Thus our observation that vascular V1A receptors were downregulated and vascular reactivity to AVP was desensitized while renal V2 receptors and their function were largely unchanged is not unprecedented.
Previously we demonstrated a robust (twofold) elevation in plasma AVP levels in female sRA mice under baseline conditions (collected 4 h into the light phase of a 12:12 light-dark cycle), and this difference was not detected in males (21). The doubling of plasma AVP concentration was achieved in sRA males as well, following a very brief (4 h) water restriction that had no effect on plasma AVP in control males. In the present study we determined that copeptin loss to urine (the major mechanism for clearance of this 4-kDa peptide) was the same in both male and female mice (Fig. 1D). While urine copeptin measures relate to the rate of AVP secretion, direct plasma AVP measures relate to both AVP secretion and degradation/clearance. Thus we now hypothesize that AVP secretion rates are similarly elevated in both male and female sRA mice, but that there exist sex-specific differences in the rates of AVP degradation/clearance. The determination that AVP receptor blockade effectively eliminated hypertension in both sexes in the present study (Fig. 2) further supports this hypothesis. Studies into the sex-specific differences in AVP clearance mechanisms are ongoing.
Perspectives and Significance
Collectively, our data support a model of elevated brain RAS activity driving an increase in AVP secretion. AVP action upon V2 receptors subsequently contributes to elevated blood pressure and hyponatremia. We hypothesize that these effects are mediated through excessive water retention, which when combined with the extreme polydipsia of this model, results in a polyuria phenotype possibly through a pressure-diuresis mechanism. Based on the well-known function of V2 receptors in renal collecting duct aquaporin-2 mobilization, we suspect a renal-mediated mechanism is hyperactive in sRA mice, though we have not here directly examined the localization of the V2 receptors responsible for the observed antihypertensive actions of tolvaptan. These data may support the use of the sRA mouse as an experimental model of the SIADH (18) or other diseases characterized by elevated AVP production or reduced clearance. The brain-specific generation and action of angiotensin peptides is gaining substantial interest for the regulation of cardiovascular function, fluid balance, metabolic control, and even learning and memory. Vasopressin is also well-recognized for its role in fluid balance, blood pressure regulation, and various behaviors (pair bonding, altruism, learning, memory, fluid, and food intake), and its production and release are well known to be stimulated by angiotensins within the brain. Therefore, the implication of vasopressin as a primary mediator of angiotensinergic hypertension simultaneously 1) identifies vasopressin as a possible mediator of other newly recognized functions of the brain RAS (e.g., metabolic control, learning and memory, etc.); and 2) identifies angiotensin-sensitive, vasopressin-producing brain structures (e.g., the supraoptic nucleus) as major cardiovascular regulatory centers that may deserve substantially more investigation for therapeutically targeting hypertension and other disorders, especially in selected human populations with low-renin hypertension (2, 3, 7, 15, 19, 39, 48, 49, 75).
GRANTS
R. B. Siel was supported by a fellowship from the University of Iowa College of Medicine Medical Student Research Program (MSRP). P. Ketsawatsomkron, A. M. Hilzendeger, and H. Li were supported by Postdoctoral Fellowships from the American Heart Association, Midwest Affiliate. C. J. Pelham was supported by a Predoctoral Fellowship, and B. A. Buehrer and B. J. Weidemann were supported through Summer Undergraduate Research Fellowships from the American Heart Association, Midwest Affiliate. B. A. Buehrer was also supported through a fellowship from the University of Iowa Summer Research Opportunities Program (SROP). B. J. Weidemann was also supported through an academic year fellowship from the University of Iowa Center for Research by Undergraduates (ICRU). J. L. Grobe was supported by a K99/R00 “Pathway to Independence” award from the National Insititutes of Health (HL-098276) and a University of Iowa Carver Trust Collaborative Pilot Grant. This work was supported through NIH research Grants HL-084207, HL-048058, HL-061446, and HL-062984 to C. D. Sigmund. The authors also gratefully acknowledge the generous research support of the Roy J. Carver Trust.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: N.K.L., R.B.S., P.k., C.J.P., N.A.P., A.M.H., B.A.B., B.J.W., H.L., D.R.D., A.P.T., X.L., M.D.C., and J.L.G. performed experiments; N.K.L., R.B.S., P.k., C.J.P., N.A.P., A.M.H., B.A.B., B.J.W., H.L., D.R.D., A.P.T., X.L., M.D.C., C.D.S., and J.L.G. analyzed data; N.K.L., R.B.S., P.k., C.J.P., N.A.P., A.M.H., B.A.B., B.J.W., H.L., D.R.D., A.P.T., X.L., M.D.C., C.D.S., and J.L.G. interpreted results of experiments; N.K.L., R.B.S., P.k., C.J.P., N.A.P., A.M.H., B.A.B., B.J.W., H.L., D.R.D., A.P.T., X.L., M.D.C., C.D.S., and J.L.G. edited and revised manuscript; N.K.L., R.B.S., P.k., C.J.P., N.A.P., A.M.H., B.A.B., B.J.W., H.L., D.R.D., A.P.T., X.L., M.D.C., C.D.S., and J.L.G. approved final version of manuscript; M.D.C., C.D.S., and J.L.G. conception and design of research; M.D.C. and J.L.G. prepared figures; J.L.G. drafted manuscript.
ACKNOWLEDGMENTS
The authors thank the University of Iowa Office of Animal Resources and the University of Iowa Transgenic and Genome Manipulation Facility staff for their assistance in this project.
REFERENCES
- 1. Aoyagi T, Koshimizu TA, Tanoue A. Vasopressin regulation of blood pressure and volume: findings from V1a receptor-deficient mice. Kidney Int 76: 1035–1039, 2009 [DOI] [PubMed] [Google Scholar]
- 2. Argent NB, Burrell LM, Goodship TH, Wilkinson R, Baylis PH. Osmoregulation of thirst and vasopressin release in severe chronic renal failure. Kidney Int 39: 295–300, 1991 [DOI] [PubMed] [Google Scholar]
- 3. Bakris G, Bursztyn M, Gavras I, Bresnahan M, Gavras H. Role of vasopressin in essential hypertension: racial differences. J Hypertens 15: 545–550, 1997 [DOI] [PubMed] [Google Scholar]
- 4. Bonjour JP, Malvin RL. Stimulation of ADH release by the renin-angiotensin system. Am J Physiol 218: 1555–1559, 1970 [DOI] [PubMed] [Google Scholar]
- 5. Burnatowska-Hledin M, Zeneberg A, Roulo A, Grobe J, Zhao P, Lelkes PI, Clare P, Barney C. Expression of VACM-1 protein in cultured rat adrenal endothelial cells is linked to the cell cycle. Endothelium 8: 49–63, 2001 [DOI] [PubMed] [Google Scholar]
- 6. Burnatowska-Hledin M, Zhao P, Capps B, Poel A, Parmelee K, Mungall C, Sharangpani A, Listenberger L. VACM-1, a cullin gene family member, regulates cellular signaling. Am J Physiol Cell Physiol 279: C266–C273, 2000 [DOI] [PubMed] [Google Scholar]
- 7. Burrell LM, Risvanis J, Johnston CI, Naitoh M, Balding LC. Vasopressin receptor antagonism–a therapeutic option in heart failure and hypertension. Exp Physiol 85 Spec No: 259S–265S, 2000 [DOI] [PubMed] [Google Scholar]
- 8. Calò LA, Pagnin E, Davis PA, Sartori M, Ceolotto G, Pessina AC, Semplicini A. Increased expression of regulator of G protein signaling-2 (RGS-2) in Bartter's/Gitelman's syndrome. A role in the control of vascular tone and implication for hypertension. J Clin Endocrinol Metab 89: 4153–4157, 2004 [DOI] [PubMed] [Google Scholar]
- 9. Campos LA, Couto AS, Iliescu R, Santos JA, Santos RA, Ganten D, Campagnole-Santos MJ, Bader M, Baltatu O. Differential regulation of central vasopressin receptors in transgenic rats with low brain angiotensinogen. Regul Pept 119: 177–182, 2004 [DOI] [PubMed] [Google Scholar]
- 10. Coleman CG, Anrather J, Iadecola C, Pickel VM. Angiotensin II type 2 receptors have a major somatodendritic distribution in vasopressin-containing neurons in the mouse hypothalamic paraventricular nucleus. Neuroscience 163: 129–142, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Crofton JT, Share L, Shade RE, Lee-Kwon WJ, Manning M, Sawyer WH. The importance of vasopressin in the development and maintenance of DOC-salt hypertension in the rat. Hypertension 1: 31–38, 1979 [DOI] [PubMed] [Google Scholar]
- 12. da Silva AQ, Fontes MA, Kanagy NL. Chronic infusion of angiotensin receptor antagonists in the hypothalamic paraventricular nucleus prevents hypertension in a rat model of sleep apnea. Brain Res 1368: 231–238, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davisson RL, Yang G, Beltz TG, Cassell MD, Johnson AK, Sigmund CD. The brain renin-angiotensin system contributes to the hypertension in mice containing both the human renin and human angiotensinogen transgenes. Circ Res 83: 1047–1058, 1998 [DOI] [PubMed] [Google Scholar]
- 14. de Oliveira-Sales EB, Nishi EE, Boim MA, Dolnikoff MS, Bergamaschi CT, Campos RR. Upregulation of AT1R and iNOS in the rostral ventrolateral medulla (RVLM) is essential for the sympathetic hyperactivity and hypertension in the 2K-1C Wistar rat model. Am J Hypertens 23: 708–715, 2010 [DOI] [PubMed] [Google Scholar]
- 15. de Paula RB, Plavnik FL, Rodrigues CI, Neves Fde A, Kohlmann O, Ribeiro AB, Gavras I, Gavras H. Contribution of vasopressin to orthostatic blood pressure maintenance in essential hypertension. Am J Hypertens 6: 794–798, 1993 [DOI] [PubMed] [Google Scholar]
- 16. Fay MJ, Du J, Yu X, North WG. Evidence for expression of vasopressin V2 receptor mRNA in human lung. Peptides 17: 477–481, 1996 [DOI] [PubMed] [Google Scholar]
- 17. Gagnon DJ, Cousineau D, Boucher PJ. Release of vasopressin by angiotensin II and prostaglandin E2 from the rat neuro-hypophysis in vitro. Life Sci 12: 487–497, 1973 [Google Scholar]
- 18. Gassanov N, Semmo N, Semmo M, Nia AM, Fuhr U, Er F. Arginine vasopressin (AVP) and treatment with arginine vasopressin receptor antagonists (vaptans) in congestive heart failure, liver cirrhosis and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Eur J Clin Pharmacol 67: 333–346, 2011 [DOI] [PubMed] [Google Scholar]
- 19. Gavras H. Pressor systems in hypertension and congestive heart failure. Role of vasopressin. Hypertension 16: 587–593, 1990 [DOI] [PubMed] [Google Scholar]
- 20. Góźdź A, Szczepańska-Sadowska E, Szczepańska K, Maśliński W, Luszczyk B. Vasopressin V1a, V1b and V2 receptors mRNA in the kidney and heart of the renin transgenic TGR(mRen2)27 and Sprague Dawley rats. J Endocrinol 176: 111–119, 2003 [PubMed] [Google Scholar]
- 21. Grobe JL, Grobe CL, Beltz TG, Westphal SG, Morgan DA, Xu D, de Lange WJ, Li H, Sakai K, Thedens DR, Cassis LA, Rahmouni K, Mark AL, Johnson AK, Sigmund CD. The brain renin-angiotensin system controls divergent efferent mechanisms to regulate fluid and energy balance. Cell Metab 12: 431–442, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grobe JL, Xu D, Sigmund CD. An intracellular renin-angiotensin system in neurons: fact, hypothesis, or fantasy. Physiology (Bethesda) 23: 187–193, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gu S, Anton A, Salim S, Blumer KJ, Dessauer CW, Heximer SP. Alternative translation initiation of human regulators of G-protein signaling-2 yields a set of functionally distinct proteins. Mol Pharmacol 73: 1–11, 2008 [DOI] [PubMed] [Google Scholar]
- 24. Halabi CM, Beyer AM, de Lange WJ, Keen HL, Baumbach GL, Faraci FM, Sigmund CD. Interference with PPAR gamma function in smooth muscle causes vascular dysfunction and hypertension. Cell Metab 7: 215–226, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hao J, Michalek C, Zhang W, Zhu M, Xu X, Mende U. Regulation of cardiomyocyte signaling by RGS proteins: differential selectivity towards G proteins and susceptibility to regulation. J Mol Cell Cardiol 41: 51–61, 2006 [DOI] [PubMed] [Google Scholar]
- 26. Head GA, Mayorov DN. Central angiotensin and baroreceptor control of circulation. Ann NY Acad Sci 940: 361–379, 2001 [DOI] [PubMed] [Google Scholar]
- 27. Heximer SP, Knutsen RH, Sun X, Kaltenbronn KM, Rhee MH, Peng N, Oliveira-dos-Santos A, Penninger JM, Muslin AJ, Steinberg TH, Wyss JM, Mecham RP, Blumer KJ. Hypertension and prolonged vasoconstrictor signaling in RGS2-deficient mice. J Clin Invest 111: 445–452, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Heximer SP, Watson N, Linder ME, Blumer KJ, Hepler JR. RGS2/G0S8 is a selective inhibitor of Gqalpha function. Proc Natl Acad Sci USA 94: 14389–14393, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Huang BS, Leenen FH. Both brain angiotensin II and “ouabain” contribute to sympathoexcitation and hypertension in Dahl S rats on high salt intake. Hypertension 32: 1028–1033, 1998 [DOI] [PubMed] [Google Scholar]
- 30. Iovino M, Steardo L. Vasopressin release to central and peripheral angiotensin II in rats with lesions of the subfornical organ. Brain Res 322: 365–368, 1984 [DOI] [PubMed] [Google Scholar]
- 31. Itaya Y, Suzuki H, Matsukawa S, Kondo K, Saruta T. Central renin-angiotensin system and the pathogenesis of DOCA-salt hypertension in rats. Am J Physiol Heart Circ Physiol 251: H261–H268, 1986 [DOI] [PubMed] [Google Scholar]
- 32. Johren O, Imboden H, Hauser W, Mave I, Sanvitto GL, Saavedra JM. Localization of angiotensin-converting enzyme,angiotensin II, angiotensin II receptor subtypes, and vasopressin in the mouse hypothalamus. Brain Res 757: 218–227, 1997 [DOI] [PubMed] [Google Scholar]
- 33. Kato Y, Igarashi N, Hirasawa A, Tsujimoto G, Kobayashi M. Distribution and developmental changes in vasopressin V2 receptor mRNA in rat brain. Differentiation 59: 163–169, 1995 [DOI] [PubMed] [Google Scholar]
- 34. Knepel W, Anhut H, Nutto D, Holland A, Meyer DK. Vasopressin release from rat medial basal hypothalamus induced in vitro by angiotensin. Eur J Pharmacol 80: 247–249, 1982 [DOI] [PubMed] [Google Scholar]
- 35. Knepel W, Nutto D, Meyer DK. Effect of transection of subfornical organ efferent projections on vasopressin release induced by angiotensin or isoprenaline in the rat. Brain Res 248: 180–184, 1982 [DOI] [PubMed] [Google Scholar]
- 36. Koshimizu TA, Nasa Y, Tanoue A, Oikawa R, Kawahara Y, Kiyono Y, Adachi T, Tanaka T, Kuwaki T, Mori T, Takeo S, Okamura H, Tsujimoto G. V1a vasopressin receptors maintain normal blood pressure by regulating circulating blood volume and baroreflex sensitivity. Proc Natl Acad Sci USA 103: 7807–7812, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kubo T, Yamaguchi H, Tsujimura M, Hagiwara Y, Fukumori R. An angiotensin system in the anterior hypothalamic area anterior is involved in the maintenance of hypertension in spontaneously hypertensive rats. Brain Res Bull 52: 291–296, 2000 [DOI] [PubMed] [Google Scholar]
- 38. Kubo T, Yamaguchi H, Tsujimura M, Hagiwara Y, Fukumori R. Blockade of angiotensin receptors in the anterior hypothalamic preoptic area lowers blood pressure in DOCA-salt hypertensive rats. Hypertens Res 23: 109–118, 2000 [DOI] [PubMed] [Google Scholar]
- 39. Laragh JH. Biochemical profiling and the natural history of hypertensive diseases: low-renin essential hypertension, a benign condition. Circulation 44: 971–974, 1971 [DOI] [PubMed] [Google Scholar]
- 40. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25: 402–408, 2001 [DOI] [PubMed] [Google Scholar]
- 41. Matsuguchi H, Schmid PG. Acute interaction of vasopressin and neurogenic mechanisms in DOC-salt hypertension. Am J Physiol Heart Circ Physiol 242: H37–H43, 1982 [DOI] [PubMed] [Google Scholar]
- 42. Mayorov DN, Head GA. AT1 receptors in the RVLM mediate pressor responses to emotional stress in rabbits. Hypertension 41: 1168–1173, 2003 [DOI] [PubMed] [Google Scholar]
- 43. Möhring J, Möhring B. Reevaluation of DOCA escape phenomenon. Am J Physiol 223: 1237–1245, 1972 [DOI] [PubMed] [Google Scholar]
- 44. Morimoto S, Cassell MD, Sigmund CD. The brain renin-angiotensin system in transgenic mice carrying a highly regulated human renin transgene. Circ Res 90: 80–86, 2002 [DOI] [PubMed] [Google Scholar]
- 45. Neves MF, Virdis A, Schiffrin EL. Resistance artery mechanics and composition in angiotensin II-infused rats: effects of aldosterone antagonism. J Hypertens 21: 189–198, 2003 [DOI] [PubMed] [Google Scholar]
- 46. Northcott CA, Watts S, Chen Y, Morris M, Chen A, Haywood JR. Adenoviral inhibition of AT1a receptors in the paraventricular nucleus inhibits acute increases in mean arterial blood pressure in the rat. Am J Physiol Regul Integr Comp Physiol 299: R1202–R1211, 2010 [DOI] [PubMed] [Google Scholar]
- 47. Oparil S, Yang RH, Jin HG, Chen SJ, Meng QC, Berecek KH, Wyss JM. Role of anterior hypothalamic angiotensin II in the pathogenesis of salt sensitive hypertension in the spontaneously hypertensive rat. Am J Med Sci 307: S26–S37, 1994 [PubMed] [Google Scholar]
- 48. Os I, Kjeldsen SE, Skjøtø J, Westheim A, Lande K, Aakesson I, Frederichsen P, Leren P, Hjermann I, Eide IK. Increased plasma vasopressin in low renin essential hypertension. Hypertension 8: 506–513, 1986 [DOI] [PubMed] [Google Scholar]
- 49. Padfield PL, Brown JJ, Lever AF, Morton JJ, Robertson JI. Blood pressure in acute and chronic vasopressin excess: studies of malignant hypertension and the syndrome of inappropriate antidiuretic hormone secretion. N Engl J Med 304: 1067–1070, 1981 [DOI] [PubMed] [Google Scholar]
- 50. Park CG, Leenen FH. Effects of centrally administered losartan on deoxycorticosterone-salt hypertension rats. J Korean Med Sci 16: 553–557, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Phillips MI. Angiotensin in the brain. Neuroendocrinology 25: 354–377, 1978 [DOI] [PubMed] [Google Scholar]
- 52. Raggenbass M. Overview of cellular electrophysiological actions of vasopressin. Eur J Pharmacol 583: 243–254, 2008 [DOI] [PubMed] [Google Scholar]
- 53. Ramsay DJ. Effects of circulating angiotensin II on the brain. In: Frontiers in Neuroendocrinology, edited by Ganong WF, Martini L. New York: Raven, 1982, vol. 7, p. 263–285 [Google Scholar]
- 54. Sakai K, Agassandian K, Morimoto S, Sinnayah P, Cassell MD, Davisson RL, Sigmund CD. Local production of angiotensin II in the subfornical organ causes elevated drinking. J Clin Invest 117: 1088–1095, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Salim S, Sinnarajah S, Kehrl JH, Dessauer CW. Identification of RGS2 and type V adenylyl cyclase interaction sites. J Biol Chem 278: 15842–15849, 2003 [DOI] [PubMed] [Google Scholar]
- 56. Schinke M, Baltatu O, Böhm M, Peters J, Rascher W, Bricca G, Lippoldt A, Ganten D, Bader M. Blood pressure reduction and diabetes insipidus in transgenic rats deficient in brain angiotensinogen. Proc Natl Acad Sci USA 96: 3975–3980, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Semplicini A, Lenzini L, Sartori M, Papparella I, Calò LA, Pagnin E, Strapazzon G, Benna C, Costa R, Avogaro A, Ceolotto G, Pessina AC. Reduced expression of regulator of G-protein signaling 2 (RGS2) in hypertensive patients increases calcium mobilization and ERK1/2 phosphorylation induced by angiotensin II. J Hypertens 24: 1115–1124, 2006 [DOI] [PubMed] [Google Scholar]
- 58. Shi P, Diez-Freire C, Jun JY, Qi Y, Katovich MJ, Li Q, Sriramula S, Francis J, Sumners C, Raizada MK. Brain microglial cytokines in neurogenic hypertension. Hypertension 56: 297–303, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sinn PL, Zhang X, Sigmund CD. JG cell expression and partial regulation of a human renin genomic transgene driven by a minimal renin promoter. Am J Physiol Renal Physiol 277: F634–F642, 1999 [DOI] [PubMed] [Google Scholar]
- 60. Sun X, Kaltenbronn KM, Steinberg TH, Blumer KJ. RGS2 is a mediator of nitric oxide action on blood pressure and vasoconstrictor signaling. Mol Pharmacol 67: 631–639, 2005 [DOI] [PubMed] [Google Scholar]
- 61. Sun Z, Cade R, Morales C. Role of central angiotensin II receptors in cold-induced hypertension. Am J Hypertens 15: 85–92, 2002 [DOI] [PubMed] [Google Scholar]
- 62. Szczepańska-Sadowska E, Paczwa P, Loń S, Ganten D. Increased pressor function of central vasopressinergic system in hypertensive renin transgenic rats. J Hypertens 16: 1505–1514, 1998 [DOI] [PubMed] [Google Scholar]
- 63. Szinnai G, Morgenthaler NG, Berneis K, Struck J, Müller B, Keller U, Christ-Crain M. Changes in plasma copeptin, the c-terminal portion of arginine vasopressin during water deprivation and excess in healthy subjects. J Clin Endocrinol Metab 92: 3973–3978, 2007 [DOI] [PubMed] [Google Scholar]
- 64. Takimoto E, Koitabashi N, Hsu S, Ketner EA, Zhang M, Nagayama T, Bedja D, Gabrielson KL, Blanton R, Siderovski DP, Mendelsohn ME, Kass DA. Regulator of G protein signaling 2 mediates cardiac compensation to pressure overload and antihypertrophic effects of PDE5 inhibition in mice. J Clin Invest 119: 408–420, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Tang KM, Wang GR, Lu P, Karas RH, Aronovitz M, Heximer SP, Kaltenbronn KM, Blumer KJ, Siderovski DP, Zhu Y, Mendelsohn ME. Regulator of G-protein signaling-2 mediates vascular smooth muscle relaxation and blood pressure. Nat Med 9: 1506–1512, 2003 [DOI] [PubMed] [Google Scholar]
- 66. Trinder D, Phillips PA, Stephenson JM, Risvanis J, Aminian A, Adam W, Cooper M, Johnston CI. Vasopressin V1 and V2 receptors in diabetes mellitus. Am J Physiol Endocrinol Metab 266: E217–E223, 1994 [DOI] [PubMed] [Google Scholar]
- 67. Tsang S, Woo AY, Zhu W, Xiao RP. Deregulation of RGS2 in cardiovascular diseases. Front Biosci (Schol Ed) 2: 547–557, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wrobel LJ, Dupré A, Raggenbass M. Excitatory action of vasopressin in the brain of the rat: role of cAMP signaling. Neuroscience 172: 177–186, 2011 [DOI] [PubMed] [Google Scholar]
- 69. Yamamoto J, Yamane Y, Umeda Y, Yoshioka T, Nakai M, Ikeda M. Cardiovascular hemodynamics and vasopressin blockade in DOCA-salt hypertensive rats. Hypertension 6: 397–407, 1984 [DOI] [PubMed] [Google Scholar]
- 70. Yang CR, Phillips MI, Renaud LP. Angiotensin II receptor activation depolarizes rat supraoptic neurons in vitro. Am J Physiol Regul Integr Comp Physiol 263: R1333–R1338, 1992 [DOI] [PubMed] [Google Scholar]
- 71. Yang J, Kamide K, Kokubo Y, Takiuchi S, Tanaka C, Banno M, Miwa Y, Yoshii M, Horio T, Okayama A, Tomoike H, Kawano Y, Miyata T. Genetic variations of regulator of G-protein signaling 2 in hypertensive patients and in the general population. J Hypertens 23: 1497–1505, 2005 [DOI] [PubMed] [Google Scholar]
- 72. Yang RH, Jin H, Wyss JM, Oparil S. Depressor effect of blocking angiotensin subtype 1 receptors in anterior hypothalamus. Hypertension 19: 475–481, 1992 [DOI] [PubMed] [Google Scholar]
- 73. Ye S, Zhong H, Duong VN, Campese VM. Losartan reduces central and peripheral sympathetic nerve activity in a rat model of neurogenic hypertension. Hypertension 39: 1101–1106, 2002 [DOI] [PubMed] [Google Scholar]
- 74. Zhang W, Anger T, Su J, Hao J, Xu X, Zhu M, Gach A, Cui L, Liao R, Mende U. Selective loss of fine tuning of Gq/11 signaling by RGS2 protein exacerbates cardiomyocyte hypertrophy. J Biol Chem 281: 5811–5820, 2006 [DOI] [PubMed] [Google Scholar]
- 75. Zhang X, Hense HW, Riegger GA, Schunkert H. Association of arginine vasopressin and arterial blood pressure in a population-based sample. J Hypertens 17: 319–324, 1999 [DOI] [PubMed] [Google Scholar]
- 76. Zicha J, Kunes J, Lébl M, Pohlová I, Slaninová J, Jelínek J. Antidiuretic and pressor actions of vasopressin in age-dependent DOCA-salt hypertension. Am J Physiol Regul Integr Comp Physiol 256: R138–R145, 1989 [DOI] [PubMed] [Google Scholar]
- 77. Zimmerman MC, Lazartigues E, Sharma RV, Davisson RL. Hypertension caused by angiotensin II infusion involves increased superoxide production in the central nervous system. Circ Res 95: 210–216, 2004 [DOI] [PubMed] [Google Scholar]