Abstract
Objectives. Growth hormone deficiency patients exhibited reduced bone mineral density compared with healthy controls, but previous researches demonstrated uncertainty about the effect of growth hormone replacement therapy on bone in growth hormone deficient adults. The aim of this study was to determine whether the growth hormone replacement therapy could elevate bone mineral density in growth hormone deficient adults. Methods. In this meta-analysis, searches of Medline, Embase, and The Cochrane Library were undertaken to identify studies in humans of the association between growth hormone treatment and bone mineral density in growth hormone deficient adults. Random effects model was used for this meta-analysis. Results. A total of 20 studies (including one outlier study) with 936 subjects were included in our research. We detected significant overall association of growth hormone treatment with increased bone mineral density of spine, femoral neck, and total body, but some results of subgroup analyses were not consistent with the overall analyses. Conclusions. Our meta-analysis suggested that growth hormone replacement therapy could have beneficial influence on bone mineral density in growth hormone deficient adults, but, in some subject populations, the influence was not evident.
1. Introduction
The major role of growth hormone (GH) during childhood is to promote bone growth and linear growth, but GH continues to have important metabolic actions throughout life. Besides growth, GH is known to affect body composition, bone mineralization, and lipid and glucose metabolism [1]. For instance, GH can accelerate bone turnover, which is supported by several lines of evidence. In vitro studies show that GH and its major effector, insulin-like growth factor-1 (IGF-1), are both mitogens for osteoblasts [2, 3].
The condition of GH deficiency (GHD) has been accepted as a definite syndrome, and the clinical and biochemical abnormalities in GHD patients are also well known. They involve mainly the cardiovascular system, lipid metabolism, body composition, mineral metabolism, and quality of life [4, 5]. For example, adult patients with childhood-onset or adult-onset GHD exhibit reduced bone mineral density (BMD) compared with healthy controls [6, 7]. Moreover, clinical studies have shown that the prevalence of fractures is 2.7–3 times higher in GHD patients than in age-matched controls. Data from these studies suggest that the increased risk may be due to GHD rather than other pituitary hormone deficiencies [8, 9].
Many studies have demonstrated that the abnormalities of GHD patients may be reversed by GH replacement therapy, but the evidence is not all conclusive. In particular, the effect of GH treatment on BMD is less clear, though it is well established that GH promotes longitudinal bone growth. Some studies suggest an improvement in BMD [10], some show no effect [11], and others suggest a decrease in BMD related to GH treatment [12]. Moreover, the association between GH treatment and BMD may be influenced by other factors such as gender, treatment time, GH dosage, or geographic location.
We, therefore, undertook a meta-analysis on the effects of GH replacement therapy on BMD based on available studies.
2. Methods
2.1. Search Strategy and Inclusion Criteria
We systematically searched Medline, Embase, and Cochrane Library for studies written in English (from their commencements to December 2012). The search used the following terms: “growth hormone,” “GH,” “somatotropin,” “bone,” “bone mineral density” and “BMD.” The following three sites of BMD were included in this meta-analysis: spine, femoral neck (FN), and total body (TB).
Studies in humans of the effects of GH treatment on BMD, regardless of sample size, were included if they met the following criteria: (1) data were reported on at least one of the three sites (spine, FN, and TB) of BMD; (2) BMD was measured by dual-energy X-ray absorptiometry (DXA); (3) we only included studies in which mean BMD and standard deviations (SDs), or standard errors (SEs) were available; (4) adult subjects (>16 years old); (5) subjects were patients with GHD who received GH treatment. The excluded studies included reviews, editorials, comments, letters, and abstracts.
2.2. Data Extraction
Two investigators independently reviewed the articles and selected eligible studies according to the inclusion criteria for eligible studies. Irrelevant studies were excluded. For studies with the same population resources or overlapping datasets, the most complete one was included. Study details and data were extracted independently and to a standardized electronic form by two investigators, and discrepancies were adjudicated by a third reviewer until consensus was achieved on every item. The following information was extracted from each study: last name of first author, year of publication, country, subject population, mean, BMD and SDs (or SEs) of subjects at baseline and after GH treatment.
2.3. Statistical Analysis
For this meta-analysis, all data should be given as mean and SDs. In those studies, where values of SEs were originally reported, the values of SDs were calculated. When information was reported for more than one subpopulation in one study, each subpopulation was treated as a separate comparison in our meta-analysis. BMDs in the three sites (spine, FN, and TB) were continuous outcomes presented on different scales (g/cm2, z-scores or t-scores), so we used a pooled standardized mean difference (SMD) with 95% confidence intervals (CI) calculated using the final follow-up P values to analyze the effects of GH treatment on BMD. All data were initially analyzed with a fixed effects model. If heterogeneity was found, the analysis should be redone using a random effects model. A P value of 0.05 was considered statistically significant.
Heterogeneity of the effect across studies was assessed by Q statistics, which is distributed as χ 2 statistics. I 2 statistics were provided to quantify the percentage of total variation across studies that was attributable to heterogeneity rather than to chance. An I 2 value >50% represented substantial variability, and heterogeneity was considered to be significant at P < 0.10, a conservative standard for meta-analyses. In the presence of heterogeneity, sensitivity analyses were performed to identify the outlier studies. The influence of outliers was also assessed to evaluate the impact of their removal. Moreover, there might be effective modificationcaused by study-level characteristics including treatment time, GH dosage, manufacturer of DXA scanner, and geographic location. Thus, subgroup analyses were further conducted to detect the source of heterogeneity. Treatment time subgroups were defined as ≤2 years or >2 years. GH dosage subgroups were defined as fixed dosage and dosage depending on serum IGF-1 values. Manufacturer of DXA scanner subgroups was defined as GE-Lunar or Hologic Inc, since the studies using other manufacturers of DXA scanner (Norland) are too few. Geographic location subgroups were defined as Europe, America, or Oceania.
We performed a visual inspection of the funnel plot for publication bias. The funnel plot should be asymmetric when there is publication bias and symmetric in the case of no publication bias. We performed Egger and Begg tests to measure the funnel plot asymmetry using a significance level of P < 0.05.
All statistical analyses were performed by using STATA 11.0 (Stata Corporation, College Station, TX, USA). The results of our research were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
3. Results
3.1. Studies Included in the Meta-Analysis
Our literature search produced 657 citations written in English, of which we selected 69 for further review of the full text. A total of 49 studies were excluded for unavailable or incomplete data. Finally, 20 unique studies were available for this meta-analysis [10, 11, 13–30]. Of these, 18 studies (included 20 comparisons), 16 studies (included 18 comparisons), and 11 studies (included 12 comparisons) presented data on BMD of spine, FN, and TB, respectively. Tables 1 and 2 summarized the characteristics and the data of the included studies.
Table 1.
Patient characteristics in included studies.
| References | Countries | Study subjects | Criteria of GHD | Treatment time | GH usage |
|---|---|---|---|---|---|
| Hansen et al., 1996 [13] | Denmark | 9 males and 5 females aged 31–57 | <10 mU/L in ITTa | 1 yr | 2.0 IU/m2·day |
|
| |||||
| Johannsson et al., 1996 [14] | Sweden | 24 males and 20 females aged 23–66 | <5 mU/L in ITT | 2 yr | First 4 weeks: 0.1 IU/kg·week Thereafter: 0.25 IU/kg·week |
|
| |||||
| Rodríguez-Arnao et al., 1998 [15] | UK | 18 males and 17 females aged 21.1–59.9 | <10 mU/L in ITT | 1 yr | First 4 weeks: 0.125 IU/kg·week Thereafter: 0.25 IU/kg·week |
|
| |||||
| Cuneo et al., 1998 [16] | Australia | 50 males and 33 females aged 41.2 ± 1.5 | <5 mU/L in ITT | 1 yr | First month: 0.125 IU/kg·week Thereafter: 0.25 IU/kg·week |
|
| |||||
| Biller et al., 2000 [17] | USA | 38 males aged 48.9 ± 2.0 | NAb | 1.5 yr | Initial dose: 10 μg/kg·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Koranyi et al., 2001 [18] | Sweden | 28 males and 14 females aged 17–61 | NA | 5 yr | Initial dose: 0.25 IU/kg·week Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Lanzi et al., 2003 [19] | Italy | 10 males and 8 females aged 17–50 | <9 μg/L in ARGc | 0.5 yr | Initial dose: 4 μg/kg·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Underwood et al., 2003 [20] | USA | 39 males and 25 females aged 23.8 ± 4.2 | <5 μg/L in clonidine and L-dopa stimulation tests | 2 yr | 25 μg/kg·day or 12.5 μg/kg·day |
|
| |||||
| Hubina et al., 2004 [21] | Hungary | 11 males and 9 females aged 22–67 | <3 μg/L in ITT or ARG | 3 yr | 1.2 IU/day (average dose) |
|
| |||||
| Bravenboer et al., 2005 [22] | The Netherlands | 38 males aged 20–35 | <7 μg/L in ITT or GHRHd | 5 yr | 0.67 mg/m2·day |
|
| |||||
| Arwert et al., 2005 [23] | The Netherlands | 23 males aged 20–40 | <7 μg/L in ITT or GHRH | 10 yr | First 0.5 yr: 1.2 or 3 IU/m2·day 0.5–2 yr: 2 IU/m2·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Boguszewski et al., 2005 [24] | Brazil | 7 males and 11 females aged 21–58 | <3 μg/L in ITT | 1 yr | 0.6 IU/day |
|
| |||||
| Benedini et al., 2006 [25] | Italy | 6 males and 6 females aged 29–54 | <9 μg/L in ARG and GHRH | 1 yr | Initial dose: 0.25 mg/day (for men) or 0.4 mg/day (for women) Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Snyder et al., 2007 [26] | USA | 20 males and 13 females aged 29–54 | <2.4 μg/L in ITT or ARG | 2 yr | Initial dose: 2 μg/kg·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Gotherstrom et al., 2007 [27] | Sweden | 52 males and 35 females aged 22–74 | <3 μg/L in ITT | 10 yr | 64 patients: the initial dose was 0.25 IU/kg·week and then individualized 23 patients: the dose was individualized from the start of the treatment |
|
| |||||
| Rota et al., 2008 [28] | Italy | 35 males and 29 females aged 30–50 | <9 μg/L in ARG and GHRH | 2 yr | Initial dose: 4 μg/kg·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Fideleff et al., 2008 [10] | Argentina | 22 males and 26 females aged 18–66 | <0.14 pmol/L in ITT | 4 yr | Initial dose: 0.1 mg/day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Conway et al., 2009 [29] | Australia | 65 males and 44 females aged 21.1 ± 2.3 | <3 μg/L in ITT | 2 yr | Initial dose: 0.2 mg/day (for men) or 0.4 mg/day (for women) Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| van den Heijkant et al., 2011 [11] | The Netherlands | 12 males and 8 females aged 23.9 ± 3.0 | <3 μg/L in ITT | 2 yr | Initial dose: 0.1 mg/m2·day Then adjusted accordingly to the serum IGF-I values |
|
| |||||
| Elbornsson et al., 2012 [30] | Sweden | 72 males and 54 females aged 22–74 | <3 μg/L in ITT or GHRH | 15 yr | 64 patients: the initial dose was 0.25 IU/kg·week and then individualized 62 patients: the dose was individualized from the start of the treatment |
aInsulin tolerance test; bnot available; carginine test; dGH-releasing hormone.
Table 2.
BMD measurements and outcomes.
| References | DXA scanner manufacturer | BMD sites | CVa of BMD measurements | Baseline BMD (mean ± SD) |
Posttreatment BMD (mean ± SD) | BMD scales | Serum IGF1 changes |
|---|---|---|---|---|---|---|---|
| Hansen et al., 1996 [13] | Hologic Inc. | Spine FN TB |
0.6% 1.4% 1.6% |
0.960 ± 0.170 0.920 ± 0.150 1.100 ± 0.070 |
0.950 ± 0.150 0.920 ± 0.150 1.080 ± 0.110 |
g/cm2 | Increased 263 ± 98% |
|
| |||||||
| Johannsson et al., 1996 [14] | GE-Lunar | Spine FN TB |
0.5% 1.6% 0.4% |
1.170 ± 0.186 0.944 ± 0.133 1.164 ± 0.133 |
1.218 ± 0.179 0.986 ± 0.146 1.167 ± 0.119 |
g/cm2 | Increased from 77 ± 7 to 302 ± 15 μg/L |
|
| |||||||
| Rodríguez-Arnao et al., 1998 [15] | Hologic Inc. | Spine FN TB |
1.0% 1.8% NAb |
1.000 ± 0.030 0.790 ± 0.030 1.150 ± 0.020 |
1.040 ± 0.030 0.840 ± 0.030 1.180 ± 0.020 |
g/cm2 | Increased significantly with 31% of the total patients showing IGF1 levels above the age-corrected limit of normal |
|
| |||||||
| Cuneo et al., 1998 [16] | GE-Lunar | TB | <3.8% | 1.149 ± 0.155 | 1.120 ± 0.092 | g/cm2 | Increased from 100 to 280 ± 20 μg/L |
|
| |||||||
| Biller et al., 2000 [17] | Hologic Inc. | Spine FN TB |
NA NA NA |
0.700 ± 0.134 0.920 ± 0.165 1.189 ± 0.134 |
0.751 ± 0.161 0.948 ± 0.206 1.219 ± 0.215 |
g/cm2 | NA |
|
| |||||||
| Koranyi et al., 2001 (1) [18] | GE-Lunar | FN TB |
NA NA |
0.919 ± 0.206 1.111 ± 0.110 |
0.975 ± 0.211 1.161 ± 0.110 |
g/cm2 | Increased from 85.8 ± 15.9 to 295.1 ± 36.3 μg/L |
|
| |||||||
| Koranyi et al., 2001 (2) [18] |
GE-Lunar | FN TB |
NA NA |
1.012 ± 0.142 1.214 ± 0.101 |
1.048 ± 0.147 1.210 ± 0.092 |
g/cm2 | Increased from 135.4 ± 15.5 to 283.3 ± 28.9 μg/L |
|
| |||||||
| Lanzi et al., 2003 [19] | Hologic Inc. | Spine FN |
0.5% NA |
−1.080 ± 0.180 −0.900 ± 0.370 |
−1.050 ± 0.180 −0.810 ± 0.340 |
t-score | Increased from 102.94 ± 16.93 to 226.17 ± 17.10 μg/L |
|
| |||||||
| Underwood et al., 2003 (1) [20] | GE-Lunar | Spine | NA | −1.340 ± 1.360 | −1.050 ± 0.180 | z-score | IGF1 SDS increased from −5.2 ± 2.6 to −0.6 ± 1.5 |
|
| |||||||
| Underwood et al., 2003 (2) [20] | GE-Lunar | Spine | NA | −1.010 ± 1.410 | −0.610 ± 1.300 | z-score | IGF1 SDS increased from −3.8 ± 1.5 to 1.2 ± 1.5 |
|
| |||||||
| Hubina et al., 2004 (1) [21] | Hologic Inc. | Spine FN |
0.35% NA |
−1.690 ± 1.480 −0.750 ± 2.147 |
−1.210 ± 1.252 −0.380 ± 1.789 |
t-score | IGF1 SDS increased from −2.53 ± 0.85 to 0.12 ± 0.41 |
|
| |||||||
| Hubina et al., 2004 (2) [21] | Hologic Inc. | Spine FN |
0.35% NA |
−1.200 ± 2.147 −0.450 ± 0.894 |
−0.210 ± 1.565 0.210 ± 1.118 |
t-score | IGF1 SDS increased from −3.61 ± 0.96 to 0.74 ± 0.28 |
|
| |||||||
| Bravenboer et al., 2005 [22] | Norland | Spine FN |
2.4% 2.3% |
0.920 ± 0.140 0.820 ± 0.150 |
1.050 ± 0.180 0.940 ± 0.170 |
g/cm2 | Increased from 9.9 ± 5.7 to 27.2 ± 11.8 nM |
|
| |||||||
| Arwert et al., 2005 [23] | Hologic Inc. | Spine FN |
NA 2.1% |
0.900 ± 0.150 0.780 ± 0.120 |
0.960 ± 0.120 0.800 ± 0.100 |
g/cm2 | Increased from 9.7 ± 2.1 to 26.6 ± 6.1 nM |
|
| |||||||
| Boguszewski et al., 2005 [24] | GE-Lunar | Spine FN |
1.2% 1.5% |
1.121 ± 0.210 0.903 ± 0.170 |
1.131 ± 0.210 0.948 ± 0.180 |
g/cm2 | Increased from 76.9 ± 70.4 to 133.7 ± 134.1 μg/L |
|
| |||||||
| Benedini et al., 2006 [25] | Hologic Inc. | Spine | NA | 0.950 ± 0.130 | 1.000 ± 0.100 | g/cm2 | Increased from 60 ± 29 to 151 ± 49 μg/L |
|
| |||||||
| Snyder et al., 2007 [26] | Hologic Inc. | Spine FN |
0.37–0.51% | 1.050 ± 0.130 0.820 ± 0.130 |
1.080 ± 0.140 0.830 ± 0.130 |
g/cm2 | IGF1 SDS increased from −1.65 ± 0.92 to 0.20 ± 1.40 |
|
| |||||||
| Gotherstrom et al., 2007 [27] | GE-Lunar | Spine FN TB |
0.5% 0.6% 0.4% |
1.161 ± 0.205 0.939 ± 0.159 1.163 ± 0.140 |
1.243 ± 0.270 0.976 ± 0.159 1.194 ± 0.149 |
g/cm2 | Increased from 99.5 ± 6.6 to 223.3 ± 9.8 μg/L |
|
| |||||||
| Rota et al., 2008 [28] | Hologic Inc. | Spine FN |
1.0% 1.5% |
−1.700 ± 0.200 −0.700 ± 0.200 |
−1.300 ± 0.100 −0.400 ± 0.100 |
z-score | Increased 174.1 ± 31.2% in men and 301.7 ± 97.1% in women |
|
| |||||||
| Fideleff et al., 2008 [10] | GE-Lunar | Spine FN TB |
NA NA NA |
−1.300 ± 1.386 −1.200 ± 1.386 −1.000 ± 1.386 |
0.300 ± 0.693 0.400 ± 0.693 0.100 ± 0.693 |
z-score | IGF1 SDS increased from −4.54 ± 0.42 to 0.36 ± 0.25 |
|
| |||||||
| Conway et al., 2009 [29] | Hologic Inc. | Spine TB |
NA NA |
0.910 ± 0.130 0.980 ± 0.110 |
0.960 ± 0.140 1.000 ± 0.120 |
g/cm2 | Increased from 132.9 ± 128.1 to 361.6 ± 259.5 μg/L |
|
| |||||||
| Van den Heijkant et al., 2011 [11] | Hologic Inc. | Spine FN TB |
NA NA NA |
0.960 ± 0.110 0.840 ± 0.130 1.010 ± 0.100 |
0.980 ± 0.100 0.840 ± 0.130 1.030 ± 0.110 |
g/cm2 | NA |
|
| |||||||
| Elbornsson et al., 2012 [30] | GE-Lunar | Spine FN TB |
<1.5% | 1.170 ± 0.224 0.940 ± 0.112 1.170 ± 0.112 |
1.230 ± 0.190 0.940 ± 0.190 1.190 ± 0.190 |
g/cm2 | Increased from 103 ± 6 to 183 ± 7 μg/L |
aCoefficient of variation; bnot available.
In all eligible studies, there were 3 studies separately providing the information on more than one subpopulation. Each subpopulation was treated as a separate comparison. A total of 936 subjects were included in this meta-analysis.
3.2. Association between GH Treatment and BMD of Spine
We initially performedthe meta-analysis on all 18 studies (including 20 comparisons) with a fixed effects model. For the presence of significant heterogeneity (I 2 = 82.9%), the analysis wasredone using a random effects model. The results suggested significant association between GH treatment and increased BMD of spine (SMD = 0.540, 95% CI [0.272, 0.808], P < 0.001; I 2 = 82.9%, P < 0.001 for Q test).
Sensitivity analyses showed that there was an outlier study (study ID: Rota et al.). When the outlier study was omitted, 17 studies (including 19 comparisons) were included in the meta-analysis. The heterogeneity was decreased and the results also suggested significant association between GH treatment and increased BMD of spine (SMD = 0.429, 95% CI [0.263, 0.594], P < 0.001; I 2 = 50.0%, P = 0.007 for Q test) (Figure 1(a)).
Figure 1.
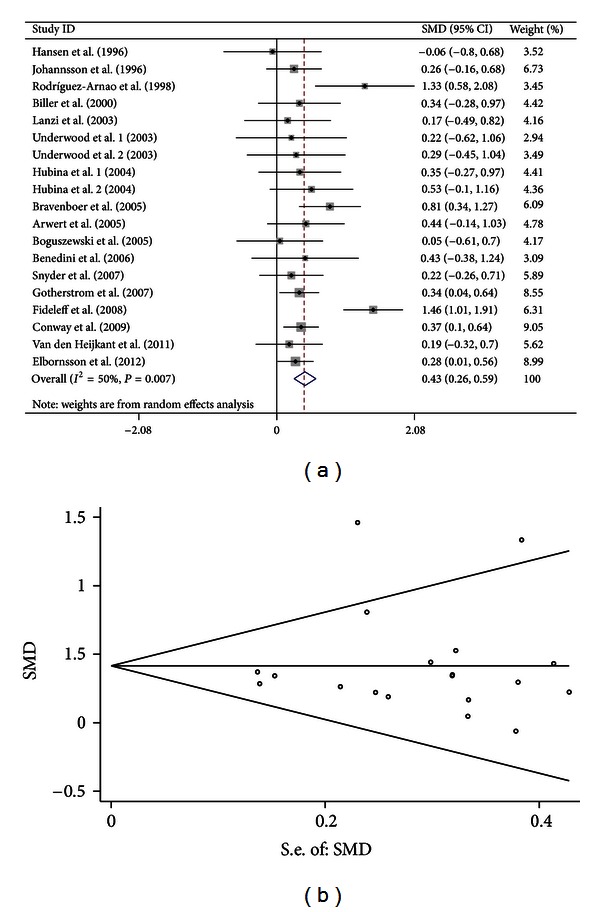
Forest plot and funnel plot for the association between GH treatment and BMD of spine. (a) Forest plot using a random effects model. (b) Funnel plot using Begg methods.
To further detect the source of heterogeneity, we performed subgroup analyses stratified by the characteristics (treatment time, GH dosage, manufacturer of DXA scanner, and geographic location) of the subjects. The results did not suggest significant association between GH treatment and BMD of spine in American subjects (SMD = 0.461, 95% CI [−0.049, 0.971], P = 0.076; I 2 = 76.3%, P = 0.001 for Q test). But a significant association between GH treatment and increased BMD of spine in the other subgroups was found. Significant heterogeneity was removed or decreased in some subgroups. Table 3 summarizes the subgroup analyses results.
Table 3.
Subgroup analyses results of the association between GH treatment and BMD of spine
| Subgroups | Effects of GH treatment on BMD | Heterogeneity | ||||
|---|---|---|---|---|---|---|
| SMD | 95% CI | P | I 2 (%) | χ2 | P | |
| Treatment time | ||||||
| ≤2 yr | 0.311 | 0.159–0.463 | 0.000 | 0.0 | 9.62 | 0.565 |
| >2 yr | 0.597 | 0.275–0.919 | 0.000 | 73.6 | 22.69 | 0.001 |
| GH dosage | ||||||
| Fixed dosage | 0.429 | 0.172–0.686 | 0.001 | 34.2 | 12.16 | 0.144 |
| Dosage depending on serum IGF-1 values | 0.429 | 0.203–0.655 | 0.000 | 62.2 | 23.79 | 0.005 |
| Manufacturer of DXA scanner | ||||||
| Hologic Inc | 0.362 | 0.204–0.520 | 0.000 | 0.0 | 9.15 | 0.518 |
| GE-lunar | 0.440 | 0.097–0.783 | 0.012 | 74.7 | 23.72 | 0.001 |
| Geographic locationa | ||||||
| Europe | 0.385 | 0.232–0.537 | 0.000 | 13.9 | 12.78 | 0.308 |
| America | 0.461 | −0.049–0.971 | 0.076 | 76.3 | 21.07 | 0.001 |
aThere was only one study including Oceanian subjects.
3.3. Association between GH Treatment and BMD of FN
Similarly, we performed the meta-analysis on all 16 studies (including 18 comparisons) with arandom effects model. The results suggested significant association between GH treatment and increased BMD of FN (SMD = 0.476, 95% CI [0.190, 0.761], P = 0.001; I 2 = 83.0%, P < 0.001 for Q test).
Sensitivity analyses showed that there was also an outlier study (study ID: Rota et al.). When the outlier study was omitted, 15 studies (including 17 comparisons) were included in the meta-analysis. The heterogeneity was decreased and the results also suggested significant association between GH treatment and increased BMD of FN (SMD = 0.377, 95% CI [0.158, 0.595], P = 0.001; I 2 = 67.8%, P < 0.001 for Q test) (Figure 2(a)).
Figure 2.
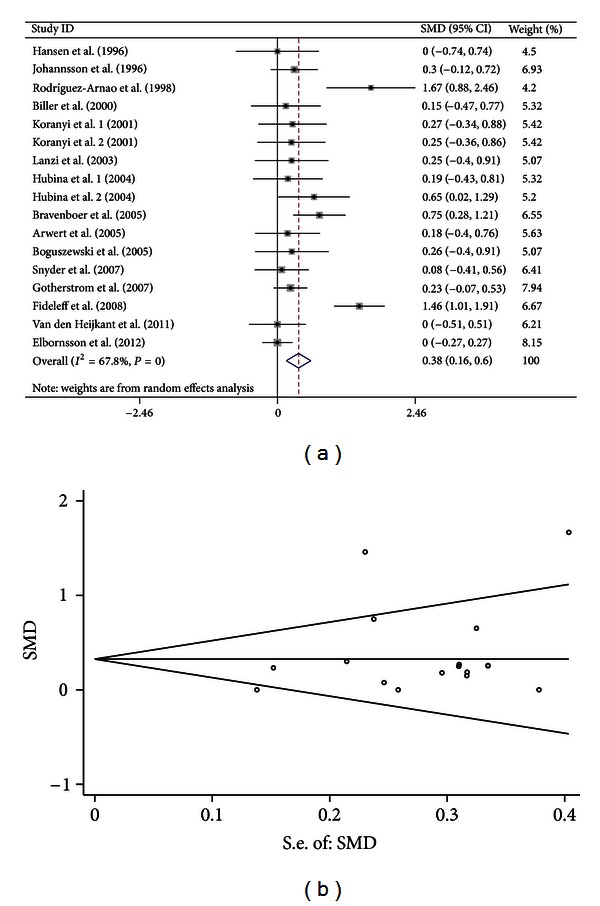
Forest plot and funnel plot for the association between GH treatment and BMD of FN. (a) Forest plot using a random effects model. (b) Funnel plot using Begg methods.
We also performed subgroup analyses to further detect the source of heterogeneity. The results did not suggest significant association between GH treatment and BMD of FN in subjects treated by GH for ≤2 years (SMD = 0.289, 95% CI [−0.009, 0.587], P = 0.057; I 2 = 51.2%, P = 0.045 for Q test) and American subjects (SMD = 0.501, 95% CI [−0.227, 1.229], P = 0.177; I 2 = 86.1%, P < 0.001 for Q test). But significant association between GH treatment and increased BMD of FN in the other subgroups were found. Moreover, the significant heterogeneity was removed or decreased in some subgroups. Table 4 summarizes the subgroup analyses results.
Table 4.
Subgroup analyses results of the association between GH treatment and BMD of FN.
| Subgroups | Effects of GH treatment on BMD | Heterogeneity | ||||
|---|---|---|---|---|---|---|
| SMD | 95% CI | P | I 2 (%) | χ2 | P | |
| Treatment time | ||||||
| ≤2 yr | 0.289 | −0.009–0.587 | 0.057 | 51.2 | 14.36 | 0.045 |
| >2 yr | 0.440 | 0.119–0.761 | 0.007 | 76.9 | 34.70 | 0.000 |
| GH usage | ||||||
| Fixed dosage | 0.520 | 0.178–0.861 | 0.003 | 56.5 | 13.79 | 0.032 |
| Dosage depending on serum IGF-1 values | 0.289 | 0.007–0.571 | 0.045 | 72.3 | 32.51 | 0.000 |
| Manufacturer of DXA scanner | ||||||
| Hologic Inc | 0.306 | 0.018–0.595 | 0.037 | 49.7 | 15.89 | 0.044 |
| GE-lunar | 0.392 | 0.026–0.758 | 0.036 | 80.2 | 30.34 | 0.000 |
| Geographic locationa | ||||||
| Europe | 0.313 | 0.117–0.508 | 0.002 | 48.0 | 23.08 | 0.027 |
| America | 0.501 | −0.227–1.229 | 0.177 | 86.1 | 21.54 | 0.000 |
aThere was no study including Oceanian subjects.
3.4. Association between GH Treatment and BMD of TB
Analogously, we performed the meta-analysis on all 11 studies (including 12 comparisons) with a random effects model. The results suggested significant association between GH treatment and increased BMD of TB (SMD = 0.242, 95% CI [0.019, 0.466], P = 0.034; I 2 = 69.6%, P < 0.001 for Q test) (Figure 3(a)).
Figure 3.

Forest plot and funnel plot for the association between GH treatment and BMD of TB. (a) Forest plot using a random effects model. (b) Funnel plot using Begg methods.
Sensitivity analyses showed that there was no outlier study.
We also performed subgroup analyses to further detect the source of heterogeneity. The results did not suggest significant association between GH treatment and BMD of TB in subjects with treatment time ≤2 years (SMD = 0.159, 95% CI [−0.148, 0.466], P = 0.311; I 2 = 68.1%, P = 0.004 for Q test), subjects who received fixed GH dosage (SMD = 0.205, 95% CI [−0.406, 0.816], P = 0.512; I 2 = 82.7%, P = 0.001 for Q test), subjects whose BMD was measured by DXA scanner manufactured by Hologic Inc (SMD = 0.317, 95% CI [−0.101, 0.736], P = 0.137; I 2 = 66.8%, P = 0.017 for Q test), subjects whose BMD was measured by DXA scanner manufactured by GE-Lunar Inc (SMD = 0.207, 95% CI [−0.083, 0.497], P = 0.162; I 2 = 74.8%, P = 0.001 for Q test), European subjects (SMD = 0.224, 95% CI [−0.015, 0.463], P = 0.066; I 2 = 51.2%, P = 0.045 for Q test), American subjects (SMD = 0.618, 95% CI [−0.200, 1.435], P = 0.139; I 2 = 78.9%, P < 0.029 for Q test,) and Oceanian subjects (SMD = −0.028, 95% CI [−0.438, 0.381], P = 0.892; I 2 = 75.6%, P = 0.043 for Q test), but as significant association between GH treatment and increased BMD of TB in the other subgroups was found. Moreover, the significant heterogeneity was removed or decreased in some subgroups. Table 5 summarizes the subgroup analyses results.
Table 5.
Subgroup analyses results of the association between GH treatment and BMD of TB.
| Subgroups | Effects of GH treatment on BMD | Heterogeneity | ||||
|---|---|---|---|---|---|---|
| SMD | 95% CI | P | I 2 (%) | χ2 | P | |
| Treatment time | ||||||
| ≤2 yr | 0.159 | −0.148–0.466 | 0.311 | 68.1 | 18.81 | 0.004 |
| >2 yr | 0.352 | 0.015–0.688 | 0.041 | 70.9 | 13.76 | 0.008 |
| GH usage | ||||||
| Fixed dosage | 0.205 | −0.406–0.816 | 0.512 | 82.7 | 17.35 | 0.001 |
| Dosage depending on serum IGF-1 values | 0.283 | 0.076–0.491 | 0.007 | 52.0 | 14.59 | 0.042 |
| Manufacturer of DXA scanner | ||||||
| Hologic Inc | 0.317 | −0.101–0.736 | 0.137 | 66.8 | 12.06 | 0.017 |
| GE-lunar | 0.207 | −0.083–0.497 | 0.162 | 74.8 | 23.77 | 0.001 |
| Geographic location | ||||||
| Europe | 0.224 | −0.015–0.463 | 0.066 | 51.2 | 14.34 | 0.045 |
| America | 0.618 | −0.200–1.435 | 0.139 | 78.9 | 4.75 | 0.029 |
| Oceania | −0.028 | −0.438–0.381 | 0.892 | 75.6 | 4.10 | 0.043 |
3.5. Heterogeneity and Publication Bias
Significant heterogeneity was separately observed among the available studies on BMD of spine, FN, and TB. To detect the source of heterogeneity, we performed subgroup analyses stratified by the characteristics of the subjects. Significant heterogeneity was removed or decreased in some subgroups but still existed in other subgroups.
For the 17 studies (with an outlier study excluded) focusing on BMD of spine, both Egger's regression (P = 0.789) and Begg methods (P = 0.889) did not show publication bias (Figure 1(b)). For the 15 studies (with an outlier study excluded) focusing on BMD of FN, both Egger's regression (P = 0.285) and Begg methods (P = 0.303) did not show publication bias (Figure 2(b)). For the 11 studies focusing on BMD of TB, both Egger's regression (P = 0.309) and Begg methods (P = 0.631) did not show publication bias (Figure 3(b)).
4. Discussion
In our meta-analysis, we detected an outlier study (study ID: Rota 2008) through sensitivity analyses when we performed the meta-analysis on the association of GH treatment and BMD of spine and FN. In the study mentioned above, patients aged below 30 years and above 50 years were excluded, which might make it an outlier study.
We detected significant overall association between GH treatment and increased BMD of spine, FN, and TB. GH could exert both direct and indirect effects on bone. (1) For direct effects on bone, there was increasing evidence that the GH-IGF axis played a vital role in determining BMD and maintaining bone health and that perturbations in this axis might predispose to the development of osteoporosis. Although GH could act on cells directly through specific receptors [31, 32], most of its anabolic actions were mediated through IGF-1 [33–35]. GH stimulated the secretion of IGF-1, largely from the liver, which then acted in an endocrine fashion. GH also stimulated IGF-1 locally in target tissues such as bone, where it might act in a paracrine or autocrine fashion [36, 37]. Thus, the effect of GH on bone was mediated, at least in part by IGF-1, and bone mass was known to be linked to circulating levels of IGF-1 [38]. In vitro studies had shown that GH-IGF-1 bound to preosteoblasts or mature osteoblasts to induce differentiation and proliferation while also regulating osteoclastic differentiation and activity providing a mechanism to couple bone resorption and formation [39, 40]. In addition, GH also increased biomarkers of bone turnover in normal subjects as well as adults and children with GHD [13, 41]. In almost all of the included studies in our meta-analysis, the serum IGF1 levels of adult GHD patients were significantly increased by the GH treatment, which were listed in Table 2. (2) For indirect effects on bone, It was known that GH had an anabolic effect on skeletal muscle, and it particularly seemed to increase muscle mass and isometric muscle strength when given in physiologically therapeutic doses to GHD patients. Klefter and Feldt-Rasmussen analyzed many trials measuring effects of GH on both muscle and bones [42], and then suggested that there could be a connection between increases in muscle mass and strength and changes in BMD in GHD patients treated with GH. This supported the present physiological concept that the mass and strength of bones were primarily determined by dynamic loads from the skeletal muscles [43, 44].
Significant heterogeneity was found in our meta-analysis. Several study-level variables leading to heterogeneity were defined by subgroup analyses including treatment time, GH dosage, manufacturer of DXA scanner and geographic location. Some results of subgroup analyses were not consistent with the overall analyses.
Firstly, we did not detect significant association between GH treatment and BMD of FN and TB in subjects with treatment time ≤2 yr. GH-IGF1 stimulated bone remodeling which occurred as a biphasic process, dominated initially by bone resorption and only later by bone formation. This biphasic sequence might also explain the initial decrease in BMD reported in several clinical trials [45, 46]. Thus, significant increases in BMD did not usually occur until 12–24 months of treatment, and clinical trials with duration of 24 months or less might not be expected to find significant increases in bone parameters.
Secondly, we did not detect significant association between GH treatment and BMD of TB in subjects received fixed GH dosage (weight- or surface-area-based dosing regimens). Early studies used weight- or surface-area-based dosing regimens that resulted in a higher GH dose than titrating GH dose to normalize the serum IGF-1 level in subsequent years [47]. And the use of dose titration means that it takes longer to establish the patient on a maintenance GH dose. Thus, known differences in the time until response of BMD to GH are recognized. In our meta-analysis, GH treatment time in the studies which determined the GH dosage depending on serum IGF-1 level is mostly longer than that isthe studies which used fixed GH dosage. So, the effect of the former dosing regimens on BMD might be more evident.
Thirdly, we did not detect significant association between GH treatment and BMD of TB in the subjects whose BMD was measured by DXA scanner manufactured by Hologic Inc or GE-lunar but got a significant overall association between GH treatment and increased BMD of TB. Absolute values of BMD, using DXA, might differ between instruments from different manufacturers. previous study performed a comparison of longitudinal measurements in the spine and proximal femur using lunar and Hologic instruments [48]. Despite the significant correlations, the agreement between the two densitometers was not high and there might be significant errors in individual subjects if one uses measurements from one densitometer to predict the change in BMD using the scanner of the other manufacturer. Furthermore, there were three studies (study ID: Arwert 2005, Gotherstrom 2007, Elbornsson 2012) which lasted for more than 10 years included in our meta-analysis. In the three studies, the operating criterion of BMD measurements changed partly during the GH treatment. In the study reported by Arwert et al., BMD measurements were performed with Norland XR-26 at the beginning of the study, and with Hologic QDR-4500 at the end of the study, but they tried to resolve this problem. They measured the European Spine Phantom (ESP) on both devices, and the results of ESP measurements showed very similar BMD values. In the study reported by Gotherstrom et al., the software versions of Lunar DPX-L were changed several times (from 1.1 to finally 1.35) during the study, but the version 1.33 was generally used during the large period of the study. In the study reported by Elbornsson et al., BMD measurements were performed with LUNAR DPX-L scanner at the beginning of the study and with LUNAR Prodigy scanner at the end of the study. They measured 31 subjects' BMD with both scanners on the same day, and the BMD values of the subjects were not significantly different between scanners.
Fourthly, we did not detect significant association between GH treatment and BMD of spine, F, and TB in American subjects. In addition, we did not detect significant association between GH treatment and BMD of TB in European and Oceanian subjects but got a significant overall association between GH treatment and increased BMD of TB. Although GH was a major regulator of IGF-1 concentrations, other factors such as nutrition and insulin concentration were also important in its regulation. In different countries or geographic location, the nutrition or insulin concentration of GHD patients might also be different.
Heterogeneity was removed or decreased in some subgroups but still existed in other subgroups. Thus, in addition to treatment time, GH dosage, manufacturer of DXA scanner and geographic location, there might be other factors leading to heterogeneity. For instance, previous study indicated that gender might influence the association between GH treatment and BMD, and several studies suggested that men had a greater treatment response to GH replacement than women. The mechanisms underlying these gender differences were not fully understood, but sex hormones might play a role [49, 50]. However, there were too few studies analyzing the results of GH treatment separately for males and females in the studies included in our meta-analysis, which made it impossible to undertake subgroup analyses stratified by gender. For the studies focus on BMD of spine, FN and TB, both Egger's regression and Begg methods did not show publication bias.
In our study, we mainly investigated the effects of GH treatment on BMD in adult GHD patients. Besides its beneficial effects on bone, GH treatment is also suggested to alleviate at least some of the aspects of the reduced physical and psycHological health associated with GHD in adult life [51, 52]. Severe quality of life (QoL) impairment is evident in a significant proportion of adults with GHD, and the beneficial effects of physiological GH replacement on QoL in affected individuals are well documented [53–55]. However, the risk of adverse effects may increase in the GHD adults treated with GH, such as oedema, joint stiffness, and carpal tunnel syndrome [54]. Moreover, serum IGF1 levels increase in the GHD patients with GH treatment. In the general population, higher circulating IGF1 levels are associated with increased incidence of prostate, colorectal, and premenopausal breast cancer [56]. To date, however, there have been no published long-term studies in adults with GHD treated with GH with respect to the development of nonpituitary malignancies.
The present study has some limitations that should be considered. Firstly, because only studies that were indexed by the selected databases were included for data analysis, some relevant published studies or unpublished studies might be missed, which might have biased our results. Secondly, our meta-analysis only included adult subjects since it was inappropriate to pool data from studies in children, where growth had a major effect of GH therapy; with studies in adults, this was not the case.
5. Conclusions
Considered together, these studies seem to indicate that GH treatment had beneficial influence on BMD in GHD adults, but in some subject populations, the influence was not evident.
Conflict of Interests
None of the authors has any conflict of interests to declare.
Authors' Contributions
P. Xue and Y. Wang contributed equally to this work.
Acknowledgments
This work was supported by the National Natural Science Foundation of Hebei Province (no. C2009001179) and Grant from Hebei Provincial Health Bureau (no. 20090316).
References
- 1.Shimon I. Growth hormone replacement for adult growth hormone deficiency. Expert Opinion on Pharmacotherapy. 2003;4(11):1977–1983. doi: 10.1517/14656566.4.11.1977. [DOI] [PubMed] [Google Scholar]
- 2.Ernst M, Froesch ER. Growth hormone dependent stimulation of osteoblast-like cells in serum-free cultures via local synthesis of insulin-like growth factor I. Biochemical and Biophysical Research Communications. 1988;151(1):142–147. doi: 10.1016/0006-291x(88)90570-0. [DOI] [PubMed] [Google Scholar]
- 3.Joung YH, Lim EJ, Darvin P, et al. MSM enhances GH signaling via the Jak2/STAT5b pathway in osteoblast-like cells and osteoblast differentiation through the activation of STAT5b in MSCs. PLoS One. 2012;7(10) doi: 10.1371/journal.pone.0047477.e47477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll PV, Christ ER, Bengtsson BÅ, et al. Growth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. Journal of Clinical Endocrinology and Metabolism. 1998;83(2):382–395. doi: 10.1210/jcem.83.2.4594. [DOI] [PubMed] [Google Scholar]
- 5.Geisler A, Lass N, Reinsch N, et al. Quality of life in children and adolescents with growth hormone deficiency: association with growth hormone treatment. Hormone Research in Paediatrics. 2012;78(2):94–99. doi: 10.1159/000341151. [DOI] [PubMed] [Google Scholar]
- 6.Kann P, Piepkorn B, Schehler B, et al. Effect of long-term treatment with GH on bone metabolism, bone mineral density and bone elasticity in GH-deficient adults. Clinical Endocrinology. 1998;48(5):561–568. doi: 10.1046/j.1365-2265.1998.00439.x. [DOI] [PubMed] [Google Scholar]
- 7.Tritos NA, Hamrahian AH, King D, et al. A longer interval without GH replacement and female gender are associated with lower bone mineral density in adults with childhood-onset GH deficiency: a KIMS database analysis. European Journal of Endocrinology. 2012;167(3):343–351. doi: 10.1530/EJE-12-0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wüster C, Abs R, Bengtsson BA, et al. The influence of growth hormone deficiency, growth hormone replacement therapy, and other aspects of hypopituitarism on fracture rate and bone mineral density. Journal of Bone and Mineral Research. 2001;16(2):398–405. doi: 10.1359/jbmr.2001.16.2.398. [DOI] [PubMed] [Google Scholar]
- 9.Rosén T, Wilhelmsen L, Landin-Wilhelmsen K, Lappas G, Bengtsson BÅ. Increased fracture frequency in adult patients with hypopituitarism and GH deficiency. European Journal of Endocrinology. 1997;137(3):240–245. doi: 10.1530/eje.0.1370240. [DOI] [PubMed] [Google Scholar]
- 10.Fideleff HL, Boquete HR, Stalldecker G, Giaccio AV, Sobrado PGV. Comparative results of a 4-year study on cardiovascular parameters, lipid metabolism, body composition and bone mass between untreated and treated adult growth hormone deficient patients. Growth Hormone and IGF Research. 2008;18(4):318–324. doi: 10.1016/j.ghir.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 11.van den Heijkant S, Hoorweg-Nijman G, Huisman J, et al. Effects of growth hormone therapy on bone mass, metabolic balance, and well-being in young adult survivors of childhood acute lymphoblastic leukemia. Journal of Pediatric Hematology/Oncology. 2011;33(6):e231–e238. doi: 10.1097/MPH.0b013e31821bbe7a. [DOI] [PubMed] [Google Scholar]
- 12.Suganuma N, Furuhashi M, Hirooka T, et al. Bone mineral density in adult patients with Turner’s syndrome: analyses of the effectiveness of GH and ovarian steroid hormone replacement therapies. Endocrine Journal. 2003;50(3):263–269. doi: 10.1507/endocrj.50.263. [DOI] [PubMed] [Google Scholar]
- 13.Hansen TB, Brixen K, Vahl N, et al. Effects of 12 months of growth hormone (GH) treatment on calciotropic hormones, calcium homeostasis, and bone metabolism in adults with acquired GH deficiency: a double blind, randomized, placebo-controlled study. Journal of Clinical Endocrinology and Metabolism. 1996;81(9):3352–3359. doi: 10.1210/jcem.81.9.8784096. [DOI] [PubMed] [Google Scholar]
- 14.Johannsson G, Rosén T, Bosaeus I, Sjöström L, Bengtsson BÅ. Two years of growth hormone (GH) treatment increases bone mineral content and density in hypopituitary patients with adult-onset GH deficiency. Journal of Clinical Endocrinology and Metabolism. 1996;81(8):2865–2873. doi: 10.1210/jcem.81.8.8768843. [DOI] [PubMed] [Google Scholar]
- 15.Rodríguez-Arnao J, James I, Jabbar A, et al. Serum collagen crosslinks as markers of bone turn-over during GH replacement therapy in growth hormone deficient adults. Clinical Endocrinology. 1998;48(4):455–462. doi: 10.1046/j.1365-2265.1998.00405.x. [DOI] [PubMed] [Google Scholar]
- 16.Cuneo RC, Judd S, Wallace JD, et al. The Australian multicenter trial of growth hormone (GH) treatment in GH- deficient adults. Journal of Clinical Endocrinology and Metabolism. 1998;83(1):107–116. doi: 10.1210/jcem.83.1.4482. [DOI] [PubMed] [Google Scholar]
- 17.Biller BMK, Sesmilo G, Baum HBA, Hayden D, Schoenfeld D, Klibanski A. Withdrawal of long-term physiological growth hormone (GH) administration: differential effects on bone density and body composition in men with adult-onset GH deficiency. Journal of Clinical Endocrinology and Metabolism. 2000;85(3):970–976. doi: 10.1210/jcem.85.3.6474. [DOI] [PubMed] [Google Scholar]
- 18.Koranyi J, Svensson J, Götherström G, Sunnerhagen KS, Bengtsson BÅ, Johannsson G. Baseline characteristics and the effects of five years of GH replacement therapy in adults with GH deficiency of childhood or adulthood onset: a comparative, prospective study. Journal of Clinical Endocrinology and Metabolism. 2001;86(10):4693–4699. doi: 10.1210/jcem.86.10.7896. [DOI] [PubMed] [Google Scholar]
- 19.Lanzi R, Losa M, Villa I, et al. GH replacement therapy increases plasma osteoprotegerin levels in GH-deficient adults. European Journal of Endocrinology. 2003;148(2):185–191. doi: 10.1530/eje.0.1480185. [DOI] [PubMed] [Google Scholar]
- 20.Underwood LE, Attie KM, Baptista J. Growth hormone (GH) dose-response in young adults with childhood-onset GH deficiency: a two-year, multicenter, multiple-dose, Placebo-controlled study. Journal of Clinical Endocrinology and Metabolism. 2003;88(11):5273–5280. doi: 10.1210/jc.2003-030204. [DOI] [PubMed] [Google Scholar]
- 21.Hubina E, Kovacs L, Szabolcs I, et al. The effect of gender and age on growth hormone replacement in growth hormone-deficient patients. Hormone and Metabolic Research. 2004;36(4):247–253. doi: 10.1055/s-2004-814458. [DOI] [PubMed] [Google Scholar]
- 22.Bravenboer N, Holzmann PJ, Ter Maaten JC, Stuurman LM, Roos JC, Lips P. Effect of long-term growth hormone treatment on bone mass and bone metabolism in growth hormone-deficient men. Journal of Bone and Mineral Research. 2005;20(10):1778–1784. doi: 10.1359/JBMR.050613. [DOI] [PubMed] [Google Scholar]
- 23.Arwert LI, Roos JC, Lips P, Twisk JWR, Manoliu RA, Drent ML. Effects of 10 years of growth hormone (GH) replacement therapy in adult GH-deficient men. Clinical Endocrinology. 2005;63(3):310–316. doi: 10.1111/j.1365-2265.2005.02343.x. [DOI] [PubMed] [Google Scholar]
- 24.Boguszewski CL, Meister LHF, Zaninelli DCT, Radominski RB. One year of GH replacement therapy with a fixed low-dose regimen improves body composition, bone mineral density and lipid profile of GH-deficient adults. European Journal of Endocrinology. 2005;152(1):67–75. doi: 10.1530/eje.1.01817. [DOI] [PubMed] [Google Scholar]
- 25.Benedini S, Dalle Carbonare L, Albiger N, et al. Effect of short-term therapy with recombinant human growth hormone (GH) on metabolic parameters and preclinical atherosclerotic markers in hypopituitary patients with growth hormone deficiency. Hormone and Metabolic Research. 2006;38(1):16–21. doi: 10.1055/s-2006-924970. [DOI] [PubMed] [Google Scholar]
- 26.Snyder PJ, Biller BMK, Zagar A, et al. Effect of growth hormone replacement on BMD in adult-onset growth hormone deficiency. Journal of Bone and Mineral Research. 2007;22(5):762–770. doi: 10.1359/jbmr.070205. [DOI] [PubMed] [Google Scholar]
- 27.Gotherstrom G, Bengtsson BA, Bossæus I, Johansson G, Svensson J. Ten-year GH replacement increase bone mineral density in hypopituitary patients with adult onset GH deficiency. European Journal of Endocrinology. 2007;156(1):55–64. doi: 10.1530/eje.1.02317. [DOI] [PubMed] [Google Scholar]
- 28.Rota F, Savanelli MC, Tauchmanova L, et al. Bone density and turnover in young adult patients with growth hormone deficiency after 2-year growth hormone replacement according with gender. Journal of Endocrinological Investigation. 2008;31(2):94–103. doi: 10.1007/BF03345574. [DOI] [PubMed] [Google Scholar]
- 29.Conway GS, Szarras-Czapnik M, Racz K, et al. Treatment for 24 months with recombinant human GH has a beneficial effect on bone mineral density in young adults with childhood-onset GH deficiency. European Journal of Endocrinology. 2009;160(6):899–907. doi: 10.1530/EJE-08-0436. [DOI] [PubMed] [Google Scholar]
- 30.Elbornsson M, Gotherstrom G, Bosaeus I, Bengtsson BA, Johannsson G, Svensson J. Fifteen years of GH replacement increases bone mineral density in hypopituitary patients with adult-onset GH deficiency. European Journal of Endocrinology. 2012;166(5):787–795. doi: 10.1530/EJE-11-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leung DW, Spencer SA, Cachianes G, et al. Growth hormone receptor and serum binding protein: purification, cloning and expression. Nature. 1987;330(6148):537–543. doi: 10.1038/330537a0. [DOI] [PubMed] [Google Scholar]
- 32.Andreassen M, Frystyk J, Faber J, Kristensen LO. GH activity and markers of inflammation: a crossover study in healthy volunteers treated with GH and a GH receptor antagonist. European Journal of Endocrinology. 2012;166(5):811–819. doi: 10.1530/EJE-11-1009. [DOI] [PubMed] [Google Scholar]
- 33.Mathews LS, Hammer RE, Brinster RL, Palmiter RD. Expression of insulin-like growth factor I in transgenic mice with elevated levels of growth hormone is correlated with growth. Endocrinology. 1988;123(1):433–437. doi: 10.1210/endo-123-1-433. [DOI] [PubMed] [Google Scholar]
- 34.Becker NS, Verdu P, Georges M, et al. The role of GHR and IGF1 genes in the genetic determination of African pygmies’ short stature. European Journal of Human Genetics. 2012 doi: 10.1038/ejhg.2012.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barner C, Petersson M, Eden Engstrom B, Hoybye, : C. Effects on insulin sensitivity and body composition of combination therapy with GH and IGF1 in GH deficient adults with type 2 diabetes. European Journal of Endocrinology. 2012;167(5):697–703. doi: 10.1530/EJE-12-0484. [DOI] [PubMed] [Google Scholar]
- 36.Holly JMP, Wass JAH. Insulin-like growth factors; autocrine, paracrine or endocrine? New perspectives of the somatomedin hypothesis in the light of recent developments. Journal of Endocrinology. 1989;122(3):611–618. doi: 10.1677/joe.0.1220611. [DOI] [PubMed] [Google Scholar]
- 37.Arnaldez FI, Helman LJ. Targeting the insulin growth factor receptor 1. Hematology/Oncology Clinics of North America. 2012;26(3):527–542. doi: 10.1016/j.hoc.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yakar S, Rosen CJ, Beamer WG, et al. Circulating levels of IGF-1 directly regulate bone growth and density. Journal of Clinical Investigation. 2002;110(6):771–781. doi: 10.1172/JCI15463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kassem M, Mosekilde L, Eriksen EF. Growth hormone stimulates proliferation of normal human bone marrow stromal osteoblast precursor cells in vitro. Growth Regulation. 1994;4(3):131–135. [PubMed] [Google Scholar]
- 40.Wit JM, Camacho-Hubner C. Endocrine regulation of longitudinal bone growth. Endocrine Development. 2011;21:30–41. doi: 10.1159/000328119. [DOI] [PubMed] [Google Scholar]
- 41.Baroncelli GI, Bertelloni S, Ceccarelli C, Cupelli D, Saggese G. Dynamics of bone turnover in children with GH deficiency treated with GH until final height. European Journal of Endocrinology. 2000;142(6):549–556. doi: 10.1530/eje.0.1420549. [DOI] [PubMed] [Google Scholar]
- 42.Klefter O, Feldt-Rasmussen U. Is increase in bone mineral content caused by increase in skeletal muscle mass/strength in adult patients with GH-treated GH deficiency? A systematic literature analysis. European Journal of Endocrinology. 2009;161(2):213–221. doi: 10.1530/EJE-09-0160. [DOI] [PubMed] [Google Scholar]
- 43.Proctor DN, Melton LJ, Khosla S, Crowson CS, O’Connor MK, Riggs BL. Relative influence of physical activity, muscle mass and strength on bone density. Osteoporosis International. 2000;11(11):944–952. doi: 10.1007/s001980070033. [DOI] [PubMed] [Google Scholar]
- 44.Frost HM. The Utah paradigm of skeletal physiology: an overview of its insights for bone, cartilage and collagenous tissue organs. Journal of Bone and Mineral Metabolism. 2000;18(6):305–316. doi: 10.1007/s007740070001. [DOI] [PubMed] [Google Scholar]
- 45.Giustina A, Mazziotti G, Canalis E. Growth hormone, insulin-like growth factors, and the skeleton. Endocrine Reviews. 2008;29(5):535–559. doi: 10.1210/er.2007-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaur A, Phadke SR. Analysis of short stature cases referred for genetic evaluation. The Indian Journal of Pediatrics. 2012;79(12):1597–1600. doi: 10.1007/s12098-012-0732-x. [DOI] [PubMed] [Google Scholar]
- 47.Murray RD, Skillicorn CJ, Howell SJ, Lissett CA, Rahim A, Shalet SM. Dose titration and patient selection increases the efficacy of GH replacement in severely GH deficient adults. Clinical Endocrinology. 1999;50(6):749–757. doi: 10.1046/j.1365-2265.1999.00722.x. [DOI] [PubMed] [Google Scholar]
- 48.Pocock NA, Noakes KA, Griffiths M, et al. A comparison of longitudinal measurements in the spine and proximal femur using lunar and hologic instruments. Journal of Bone and Mineral Research. 1997;12(12):2113–2118. doi: 10.1359/jbmr.1997.12.12.2113. [DOI] [PubMed] [Google Scholar]
- 49.Drake WM, Rodríguez-Arnao J, Weaver JU, et al. The influence of gender on the short and long-term effects of growth hormone replacement on bone metabolism and bone mineral density in hypopituitary adults: a 5-year study. Clinical Endocrinology. 2001;54(4):525–532. doi: 10.1046/j.1365-2265.2001.01246.x. [DOI] [PubMed] [Google Scholar]
- 50.Olson LE, Ohlsson C, Mohan S. The role of GH/IGF-I-mediated mechanisms in sex differences in cortical bone size in mice. Calcified Tissue International. 2011;88(1):1–8. doi: 10.1007/s00223-010-9436-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carroll PV, Drake WM, Maher KT, et al. Comparison of continuation or cessation of growth hormone (GH) therapy on body composition and metabolic status in adolescents with severe GH deficiency at completion of linear growth. Journal of Clinical Endocrinology and Metabolism. 2004;89(8):3890–3895. doi: 10.1210/jc.2003-031588. [DOI] [PubMed] [Google Scholar]
- 52.Prabhakar VKB, Shalet SM. Aetiology, diagnosis, and management of hypopituitarism in adult life. Postgraduate Medical Journal. 2006;82(966):259–266. doi: 10.1136/pgmj.2005.039768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Woodhouse LJ, Mukherjee A, Shalet SM, Ezzat S. The influence of growth hormone status on physical impairments, functional limitations, and health-related quality of life in adults. Endocrine Reviews. 2006;27(3):287–317. doi: 10.1210/er.2004-0022. [DOI] [PubMed] [Google Scholar]
- 54.Hazem A, Elamin MB, Bancos I, et al. Body composition and quality of life in adults treated with GH therapy: a systematic review and meta-analysis. European Journal of Endocrinology. 2012;166(1):13–20. doi: 10.1530/EJE-11-0558. [DOI] [PubMed] [Google Scholar]
- 55.Deijen JB, Arwert LI, Witlox J, Drent ML. Differential effect sizes of growth hormone replacement on quality of life, well-being and health status in growth hormone deficient patients: a meta-analysis. Health and Quality of Life Outcomes. 2005;3:p. 63. doi: 10.1186/1477-7525-3-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Renehan AG, Zwahlen M, Minder C, O’Dwyer ST, Shalet SM, Egger M. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. The Lancet. 2004;363(9418):1346–1353. doi: 10.1016/S0140-6736(04)16044-3. [DOI] [PubMed] [Google Scholar]


