Abstract
Objective
Benchmark data are provided for a national sample of patients who received inpatient rehabilitation for debility.
Design
Patients with debility from 830 inpatient rehabilitation facilities in the United States contributing to the Uniform Data System for Medical Rehabilitation from 2000 – 2010 were examined. Demographic information (age, marital status, gender, race/ethnicity, pre-hospital living setting, and discharge setting), hospital information (length of stay [LOS], program interruptions, payer, codes for admitting diagnosis), and functional status (Functional Independence Measure [FIM®] instrument ratings at admission and discharge, FIM change and FIM efficiency) were analyzed.
Results
Data from 2000 to 2010 (N= 260,373) revealed a decrease in mean (SD) FIM total admission ratings from 73.9 (16.2) to 62.5 (15.8). FIM total discharge ratings decreased from 95.0 (19.7) to 88.2 (19.8). Mean (SD) LOS decreased from 14.3 (9.1) to 12.1 (6.2) days. FIM efficiency (change/day) increased from 1.9 (1.7) to 2.4 (1.9). Discharge to community decreased from 80% to 75%. Acute care discharges accounted for 12% of cases. Policy changes affecting classification, reimbursement, and/or documentation processes may have influenced results.
Conclusions
National data indicate the number of debility cases is increasing with diverse composition of etiologic diagnoses. A high proportion of these patients discharge to acute care compared to other impairment groups.
Keywords: Rehabilitation Outcome, Activities of Daily Living, Benchmarking, Muscle Weakness
This report summarizes information for patients with debility who received comprehensive inpatient rehabilitation services in facilities that subscribed to the UDSMR from 2000 through 2010. The objective of this report is to provide benchmark information for important rehabilitation outcomes such as length of stay (LOS), functional status, and discharge setting for inpatient rehabilitation impairment groups. This article represents the sixth in the series of impairment-specific longitudinal reports from the Uniform Data System for Medical Rehabilitation (UDSMR®) database using information from 2000 and forward. Previous reports presented data on patients receiving inpatient rehabilitation for stroke,1 traumatic brain injury,2 lower limb joint replacement,3 hip fracture,4 and spinal cord injury.5 This series represents an extension of previous reports published in this journal, which provided single-year summaries. The last annual benchmark report contained data for the most common rehabilitation impairment categories during 1999: stroke, orthopedic diagnoses, brain dysfunction, spinal cord dysfunction, and other neurologic conditions.6 This report is the first UDSMR longitudinal benchmark study focusing on the debility impairment group. This impairment group has become more prevalent in inpatient rehabilitation facilities (IRF). Debility accounted for 6.1% of Medicare inpatient rehabilitation cases in 2004 and has increased to 10.4% of cases during the first half of 2011.7 Patients with debility have “generalized deconditioning not attributable to any of the other Impairment Groups,”8;9 such as a neurological, orthopedic, or cardiopulmonary diagnoses. This report displays trends in rehabilitation information and outcomes over time as a resource for researchers, administrators, policy makers, clinicians, individuals and their families, and other stakeholders in quality improvement efforts.
Data Source
The UDSMR is a not-for-profit organization affiliated with the UB Foundation Activities, Inc, at the University of Buffalo, The State University of New York.10 The UDSMR maintains the largest nongovernmental database for medical rehabilitation outcomes in the United States. Since 1987, the UDSMR has collected data from rehabilitation hospitals and units, long-term care hospitals, skilled nursing facilities, and pediatric and outpatient rehabilitation programs. Approximately 70% of inpatient rehabilitation facilities in the United States use UDSMR services. Subscribing facilities receive detailed summaries comparing their patient data to both regional and national benchmarks. This information is used to evaluate quality management efforts and to comply with criteria required by The Joint Commission and CARF International as well as other accrediting organizations. Additional information on the UDSMR is available from their website at http://www.udsmr.org/.10
This report contains information for persons discharged from inpatient medical rehabilitation services from January 1, 2000 through September 30, 2010. The data are aggregated and presented using an October to September fiscal year schedule (see “Variable Definitions” section). Thus, in all tables and figures, 2000 includes only three-quarters (January 1, 2000 – September 30, 2000) of the calendar year.
Data Set
The UDSMR database contains demographic, hospitalization, diagnostic, and functional status data. Demographic data include age, sex, marital status, race or ethnicity, pre-hospital living setting, and discharge setting. Hospitalization and diagnostic information include length of stay (LOS), program interruptions, payer, rehabilitation impairment group, and International Classification of Diseases, Ninth Revision,11 codes for the admitting diagnosis and complications or comorbidities. Functional status information includes ratings from the FIM instrument for admission and discharge, FIM efficiency, and FIM change (see descriptions below).
The FIM instrument includes 18 items covering six domains (self-care, sphincter control, transfer, locomotion, communication, and social cognition). The self-care subscale is the sum of ratings for eating, grooming, bathing, dressing - upper, dressing – lower, and toileting. Sphincter subscale is the sum of bladder and bowel control ratings. The transfer subscale is the sum of three types of transfers: bed/chair/wheelchair, toilet, and tub/shower. Locomotion subscale is the sum of walk or wheelchair and stairs. Communication subscale is the sum of comprehension and expression. Social cognition subscale is the sum of social interaction, problem solving, and memory. Each item is rated on a scale from 1 (complete dependence) to 7 (complete independence), with higher ratings representing greater functional independence. FIM total score for the 18 items ranges from 18 to 126. The FIM instrument was designed as an indicator of disability, which is measured in terms of assistance required to complete a task. FIM ratings are also presented as Motor and Cognitive subscales. The Motor subscale includes 13 items assessing self-care, sphincter control, transfer, and locomotion. The Cognition subscale includes 5 items assessing communication and social cognition. The reliability, validity, and responsiveness of the FIM instrument have been established.12-14 The total FIM score is also a valid measure for burden of care, the amount of daily time that a person requires for assistance with activities of daily living.15-19 An estimated four hours of care per day is needed for FIM total of 60.20 A higher FIM total of 90 corresponds to approximately one hour of daily care.20
The data collected in 2000 and 2001 included the original UDSMR protocol for administering the FIM instrument (version 5.1). In 2002, the FIM instrument was integrated into the Inpatient Rehabilitation Facilities – Patient Assessment Instrument (IRF-PAI), developed by the Centers for Medicare and Medicaid Services (CMS) as part of the prospective payment system (PPS) for inpatient rehabilitation facilities.9 Some changes were made to the FIM protocol and rating procedures. These changes have been described in documents produced by the CMS21 and in recent publications and will not be presented in detail here.22;23 Major changes potentially impacting comparisons between pre-PPS and PPS FIM data include the following: (1) admission and discharge assessment time frame, (2) change in recording for bowel and bladder management, (3) change in definition for program interruption, and (4) use of 0 for some admission motor items. The FIM total includes recoding of 0 values to 1 for individual motor items. In fiscal year 2006, policy changes included recoding 0 values to 2 for transfer to toilet.24
Variable Definitions
Consistent with previous reports in this series, specific terms and variables used within rehabilitation, the UDSMR, and IRF-PAI data sets are described here.
Case-mix group (CMG) refers to the patient classification system that determines the reimbursement for Medicare Part A fee-for-service inpatient care. Each Medicare beneficiary is assigned to a CMG upon admission to an inpatient rehabilitation facility based on primary medical condition or impairment, FIM rating, and, age for select CMGs.8 The debility impairment group currently has four CMGs (2001, 2002, 2003, 2004). From 2002 to 2005, this group had five CMGs (2001 – 2005).
CMG comorbidity tiers represent another factor that affects facility reimbursement from CMS. Relative weightings (converted to payments) are stratified by tier across each CMG based on the presence of specific comorbidities associated with increased costs.25 These payment adjustments for comorbidities consist of a four-tier system: tier 1 (high cost), tier 2 (medium cost), tier 3 (low cost) and no tier.26
Community discharge identifies patients discharged to a community-based setting: home, assisted living, a board and care, or transitional living setting.
FIM efficiency refers to the average change in total FIM instrument ratings per day. FIM efficiency is calculated by subtracting FIM admission from FIM discharge ratings and then dividing by LOS (in days).
FIM change (or gain) is the difference between total FIM admission and total FIM discharge ratings. LOS is the total number of days spent in the rehabilitation facility. Interim days spent in an acute care setting resulting in a program interruption are not included in this value.
Program interruption identifies patients who were temporarily transferred to an acute care setting and subsequently returned for additional inpatient rehabilitation services. This interruption timeframe was defined as ≤ 30 days from 2000-2001 and ≤ 3 days beginning in 2002.
Year discharged refers to the date of discharge from inpatient rehabilitation in relation to the Federal fiscal year, which runs from October 1 through September 30. For example, fiscal year 2006 includes October 1, 2005 through September 30, 2006. CMS policy changes governing inpatient rehabilitation are traditionally implemented at the beginning of the fiscal year rather than the calendar year.
Inclusion Criteria
Inclusion criteria for this benchmark report are: (1) The patient received inpatient rehabilitation for impairment category 16, which is the debility impairment group, (2) the patient received initial rehabilitation services for debility (i.e., no admissions for evaluation only or readmission), (2) the record could not have missing data for key benchmarking variables such as discharge setting or FIM ratings, (3) the patient age was at least 18 years at admission, and (4) the total LOS could not exceed 548 days (1.5 years). The debility cohort is further described in the descriptive summary section below “Debility Impairment Group.”
The research was approved by the University's Institutional Review Board and conducted in accordance with Declaration of the World Medical Association (www.wma.net).
Descriptive Summary of Aggregate Data
The number of contributing facilities across the years ranged from 789 to 830. Table 1 shows the patient characteristics, percentage of patients receiving care by hospital type, primary insurance classification, and outcomes from 2000 to 2010. The percentage of debility cases in freestanding inpatient rehabilitation facilities was higher in 2007 – 2010 (46 - 48%) compared to previous years (31 – 39%). Total number of debility cases increased substantially from 15,275 in 2000 to 32,501 in 2010.
Table 1. Facility and patient characteristics stratified by discharge year.
| Patients, N | Total 260,373 | 2000 15,275 | 2001 23,231 | 2002 18,101 | 2003 20,375 | 2004 23,327 | 2005 21,319 | 2006 19,183 | 2007 25,764 | 2008 29,586 | 2009 31,711 | 2010 32,501 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Facility type | ||||||||||||
| Hospital Unit | 59.5% | 68.0% | 61.1% | 64.9% | 66.0% | 66.5% | 67.0% | 65.5% | 52.0% | 51.7% | 53.6% | 52.7% |
| Freestanding | 40.4% | 31.3% | 38.8% | 35.1% | 34.0% | 33.5% | 33.1% | 34.5% | 48.0% | 48.3% | 46.4% | 47.4% |
| Age, yrs | ||||||||||||
| Mean | 74.2 | 74.0 | 74.1 | 75.1 | 75.2 | 75.1 | 74.7 | 74.4 | 74.3 | 73.8 | 73.5 | 73.3 |
| (SD) | (13.4) | (13.3) | (13.4) | (12.9) | (12.9) | (13.0) | (13.4) | (13.4) | (13.4) | (13.4) | (13.5) | (13.7) |
| 18 – 44 | 3.5% | 3.9% | 4.1% | 3.3% | 3.3% | 3.2% | 3.5% | 3.5% | 3.4% | 3.4% | 3.4% | 3.7% |
| 45 – 64 | 16.7% | 15.6% | 15.3% | 14.1% | 14.3% | 14.9% | 15.8% | 16.7% | 17.0% | 18.4% | 19.1% | 19.3% |
| 65 – 74 | 21.4% | 22.5% | 22.0% | 20.7% | 19.9% | 20.3% | 20.2% | 20.7% | 21.0% | 21.6% | 22.5% | 22.7% |
| ≥ 75 | 58.4% | 58.0% | 58.7% | 61.9% | 62.6% | 61.7% | 60.5% | 59.2% | 58.6% | 56.6% | 55.0% | 54.4% |
| Gender | ||||||||||||
| Male | 42.3% | 41.5% | 40.8% | 40.3% | 39.4% | 40.0% | 41.4% | 42.5% | 42.9% | 44.0% | 44.3% | 44.9% |
| Female | 57.7% | 58.3% | 59.1% | 59.7% | 60.6% | 60.0% | 58.6% | 57.5% | 57.1% | 55.9% | 55.7% | 55.1% |
| Race/ethnicity | ||||||||||||
| White | 81.5% | 80.8% | 81.6% | 82.1% | 82.3% | 81.7% | 81.5% | 80.4% | 82.2% | 81.5% | 81.3% | 81.0% |
| Black | 11.3% | 13.2% | 12.9% | 11.9% | 11.9% | 11.9% | 11.6% | 10.9% | 9.2% | 11.0% | 10.7% | 10.5% |
| Hispanic | 3.4% | 2.3% | 2.5% | 3.2% | 3.3% | 3.6% | 3.5% | 3.7% | 2.9% | 3.3% | 4.1% | 4.1% |
| Other | 2.0% | 1.8% | 1.5% | 1.4% | 1.3% | 1.3% | 2.1% | 2.6% | 3.7% | 2.1% | 1.8% | 2.0% |
| Married | ||||||||||||
| Yes | 41.7% | 40.2% | 40.2% | 40.6% | 40.2% | 40.4% | 40.4% | 41.9% | 42.4% | 43.3% | 43.4% | 43.2% |
| No | 56.8% | 56.8% | 57.4% | 58.2% | 58.7% | 58.7% | 58.7% | 56.6% | 56.2% | 55.3% | 55.3% | 55.6% |
| Primary Insurance | ||||||||||||
| Medicare fee-for-service | 78.6% | 78.2% | 79.2% | 82.7% | 83.5% | 82.6% | 81.3% | 80.4% | 78.2% | 75.8% | 74.0% | 75.0% |
| Medicare – managed care | 4.4% | 2.5% | 2.0% | 2.2% | 2.1% | 2.4% | 2.9% | 3.2% | 3.4% | 6.7% | 8.3% | 7.7% |
| Commercial | 5.2% | 5.7% | 5.6% | 4.6% | 4.7% | 4.2% | 4.6% | 4.9% | 6.4% | 5.6% | 5.4% | 4.9% |
| Managed care | 2.6% | 3.7% | 3.9% | 2.5% | 2.1% | 2.3% | 2.4% | 2.6% | 2.9% | 2.5% | 2.5% | 2.0% |
| Medicaid | 2.5% | 3.4% | 3.0% | 2.2% | 2.1% | 2.5% | 2.6% | 2.4% | 2.2% | 2.2% | 2.3% | 2.4% |
| Medicaid – managed care | 0.7% | 0.4% | 0.5% | 0.6% | 0.6% | 0.7% | 0.8% | 0.8% | 0.6% | 0.8% | 0.8% | 1.0% |
| Other | 5.9% | 5.6% | 5.3% | 5.0% | 5.0% | 5.3% | 5.4% | 5.7% | 6.5% | 6.4% | 6.7% | 7.1% |
| Living Situation | ||||||||||||
| With Others | 61.4% | 58.4% | 58.6% | 58.7% | 59.0% | 59.3% | 59.6% | 61.2% | 62.1% | 63.4% | 64.6% | 64.8% |
| Alone | 32.7% | 34.2% | 34.6% | 34.4% | 34.7% | 34.5% | 34.5% | 33.0% | 32.3% | 31.1% | 30.3% | 30.2% |
| Admitted from | ||||||||||||
| Acute care | 92.8% | 91.2% | 92.2% | 91.0% | 90.7% | 91.9% | 92.0% | 92.1% | 93.3% | 94.2% | 94.3% | 94.5% |
| Community | 4.1% | 4.9% | 4.6% | 5.9% | 5.9% | 5.0% | 4.5% | 4.7% | 3.6% | 3.0% | 2.8% | 2.8% |
| Long-term care facility | 2.2% | 2.2% | 1.6% | 2.1% | 2.5% | 2.2% | 2.6% | 2.5% | 2.4% | 2.1% | 2.3% | 2.2% |
| Discharge setting | ||||||||||||
| Community | 75.8% | 79.8% | 79.9% | 77.5% | 76.6% | 75.9% | 76.0% | 75.0% | 74.7% | 74.0% | 73.5% | 74.8% |
| Acute care | 12.3% | 8.2% | 8.3% | 10.8% | 11.9% | 12.7% | 12.6% | 13.2% | 13.7% | 13.9% | 13.9% | 13.1% |
| Long-term care facility | 8.1% | 8.8% | 9.1% | 9.2% | 8.5% | 8.2% | 8.0% | 7.9% | 8.0% | 7.6% | 7.1% | 7.5% |
| Rehab/subacute | 3.4% | 2.0% | 2.0% | 1.8% | 2.5% | 2.8% | 3.1% | 3.6% | 3.3% | 4.2% | 5.2% | 4.2% |
| Length of stay days | 12.6 (7.4) | 14.3 (9.1) | 14.3 (10.4) | 12.9 (7.8) | 12.5 (7.1) | 12.4 (7.1) | 12.4 (7.8) | 12.1 (6.7) | 12.6 (7.0) | 12.4 (6.7) | 12.1(6.4) | 12.1(6.2) |
| FIM total admission | 66.8 (16.5) | 73.9 (16.2) | 73.4 (16.1) | 71.3 (16.4) | 69.5 (16.4) | 68.6 (16.0) | 68.2 (15.7) | 66.2 (16.0) | 63.4 (16.1) | 63.0 (15.9) | 62.7 (15.9) | 62.5 (15.8) |
| FIM total discharge | 89.5 (20.1) | 95.0 (19.7) | 95.0 (19.6) | 91.7 (20.3) | 89.6 (20.1) | 89.3 (19.9) | 89.6 (19.8) | 88.2 (19.9) | 87.5 (20.1) | 87.4 (20.1) | 87.4 (20.0) | 88.2 (19.8) |
| FIM total change | 22.8 (14.3) | 21.1 (12.6) | 21.6 (12.8) | 20.4 (13.2) | 20.1 (13.7) | 20.7 (13.8) | 21.4 (13.8) | 22.0 (14.0) | 24.1 (14.9) | 24.4 (14.9) | 24.7 (14.9) | 25.7 (15.1) |
| Efficiency, change per day | 2.1 (1.9) | 1.9 (1.7) | 1.9 (1.8) | 1.9 (1.8) | 1.9 (1.9) | 2.0 (1.8) | 2.0 (1.9) | 2.1 (1.9) | 2.2 (1.9) | 2.3 (2.0) | 2.3 (2.0) | 2.4 (1.9) |
Data are presented as percentage or mean (SD).
Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Fiscal year 2000 only includes data from January through September 2000.
FIM® indicates Functional Independence Measure. FIM® total ratings include all 18 items.
Of the original 280,240 patients admitted to inpatient rehabilitation for debility, 18,859 were not admitted for initial rehabilitation, 66 had missing data for discharge setting, 173 were less than 18 years of age, and 769 died. The descriptive statistics (means, standard deviations, counts, and percentages) represent unadjusted aggregate values from the remaining 260,373 patients meeting the inclusion criteria. Thus, 93% of the original sample is included in this report.
The following sections include summary descriptive statistics and trends for select variables. Caution must be applied to interpretations of trends in these data, which are arranged in longitudinal format. As noted previously, the Inpatient Rehabilitation Facilities – Patient Assessment Instrument developed for PPS contained assessment and coding changes beginning in 2002.21-23 Additional modifications related to PPS have been introduced over subsequent years. Thus, some of the year-to-year difference may reflect changes in classification and/or documentation processes rather than actual changes in rehabilitation services or patient outcomes.22;23 In addition, the number of inpatient rehabilitation facilities varied slightly across the years.
Patient Characteristics
Table 1 displays total and yearly summary statistics for descriptive characteristics of rehabilitation patients with debility. The mean (SD) age of the entire sample was 74.2 (13.4) years with more than half of patients in the age group of 75 years and older. Patient characteristics for gender, marital status, and race/ethnicity are generally consistent over time with approximately 58% female, 82% non-Hispanic white, and 57% not married. Medicare fee-for-service was the most common primary payer category, and represented 79% of total cases. Medicare fee-for-service cases steadily declined since 2003 while Medicare managed care cases increased and likely reflects higher enrollment in Medicare managed care across this time.
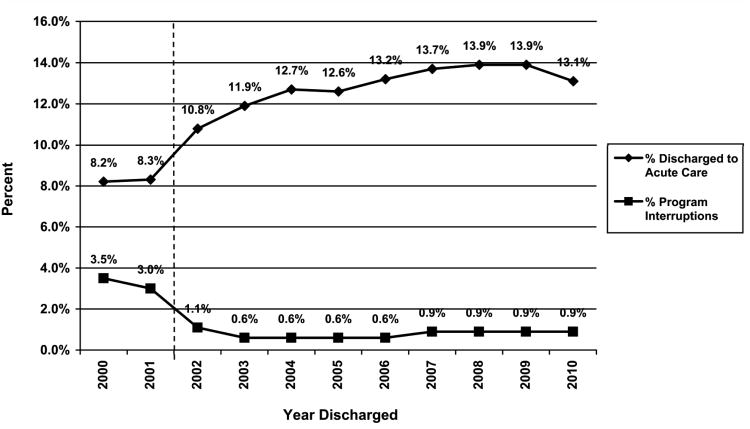
Overall, 93% of patients were admitted to inpatient rehabilitation directly from acute care. Approximately three-fourths of patients were discharged to the community after rehabilitation across the 11-year period. Community discharge declined from 80% in 2000-2001 to 74-75% in 2006-2010. The sudden drop in community discharges and sudden rise in discharges to acute care in 2002 reflects PPS changes in the definition and coding of program interruptions as well as actual change in the percentage of patients who returned to the community upon discharge.22Figure 1 depicts these changes in terms of discharges to acute care and program interruptions. From 2004 to 2010, acute care represented the discharge setting for 13-14% of cases for the debility impairment group.
Figure 1.
Percentage of program interruptions and cases discharged to acute care by discharge year. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. In 2002, the definition for program interruption changed from ≤ 30 days to ≤ 3 days.
LOS and Functional Status
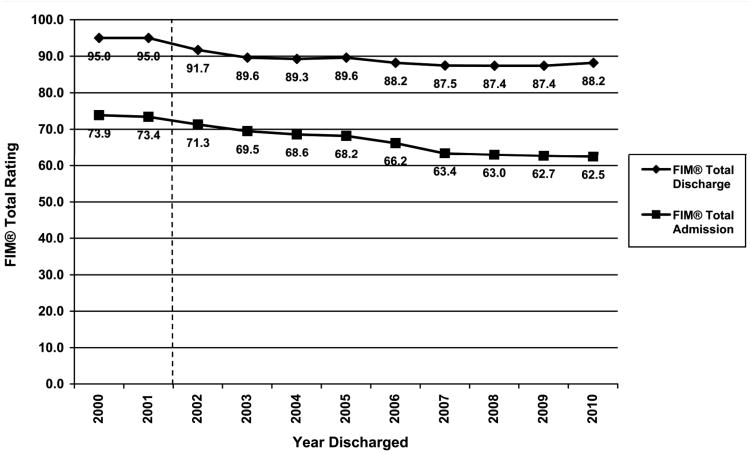
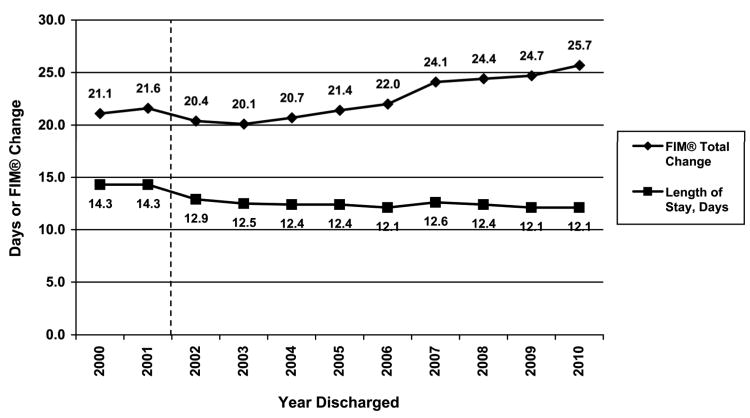
Table 1 also provides descriptive information for LOS, functional status (FIM total) at admission and discharge, change in functional status from admission to discharge (i.e. functional gain). Figures 2 and 3 display trends in these outcomes by discharge year. Mean LOS decreased by 1.4 days between 2001 and 2002, a decrease partially explained by the program interruption change, and overall by another 0.8 day from 2002 to 2010. Increase in discharges to acute and subacute settings may also influence LOS trends. FIM total admission ratings decreased each year with the yearly average 11 points lower in 2010 compared to 2000.
Figure 2.
Mean admission and discharge FIM® total ratings by discharge year. FIM® indicates Functional Independence Measure. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. In 2002, some rules for completing the FIM instrument items were changed.
Figure 3.
Mean FIM® total change and length of stay by discharge year. FIM® indicates Functional Independence Measure. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. In 2002, some rules for completing the FIM instrument items were changed, and the procedure for coding program interruptions changed.
Table 2 depicts mean admission, discharge, and change values for items within the six functional domains of the FIM instrument. FIM admission and discharge ratings gradually decreased across the 11-year period for all subscales. Locomotion (walk/wheelchair and stairs) was the lowest scoring subscale for patients with debility. Communication (comprehension and expression) had the highest mean FIM ratings.
Table 2. Mean Ratings for individual FIM® items within each FIM® subscale stratified by discharge year.
| FIM® Subscale | Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission | ||||||||||||
| Self-care | 3.6 (1.1) | 4.1 (1.1) | 4.0 (1.1) | 3.9 (1.1) | 3.8 (1.1) | 3.7 (1.0) | 3.7 (1.0) | 3.6 (1.0) | 3.4 (1.0) | 3.4 (1.0) | 3.4 (1.0) | 3.4 (1.0) |
| Sphincter | 3.7 (1.8) | 4.2 (1.8) | 4.1 (1.8) | 3.9 (1.9) | 3.8 (1.9) | 3.8 (1.8) | 3.7 (1.8) | 3.6 (1.8) | 3.5 (1.8) | 3.5 (1.8) | 3.5 (1.8) | 3.5 (1.8) |
| Transfer | 2.8 (1.1) | 3.1 (1.1) | 3.1 (1.1) | 3.0 (1.1) | 3.0 (1.1) | 2.9 (1.0) | 2.9 (1.0) | 2.8 (1.0) | 2.7 (1.0) | 2.7 (1.0) | 2.7 (1.0) | 2.6 (1.0) |
| Locomotion | 1.7 (0.9) | 1.8 (1.0) | 1.8 (1.0) | 1.8 (0.9) | 1.7 (0.9) | 1.7 (0.9) | 1.7 (0.9) | 1.6 (0.9) | 1.6 (0.8) | 1.6 (0.8) | 1.6 (0.8) | 1.6 (0.8) |
| Communication | 5.4 (1.4) | 5.9 (1.3) | 5.9 (1.3) | 5.7 (1.4) | 5.6 (1.3) | 5.6 (1.3) | 5.6 (1.3) | 5.4 (1.4) | 5.2 (1.4) | 5.1 (1.4) | 5.1 (1.4) | 5.1 (1.4) |
| Social cognition | 5.0 (1.5) | 5.4 (1.5) | 5.4 (1.5) | 5.3 (1.5) | 5.1 (1.5) | 5.1 (1.4) | 5.1 (1.4) | 5.0 (1.5) | 4.7 (1.5) | 4.7 (1.5) | 4.7 (1.4) | 4.7 (1.4) |
| Discharge | ||||||||||||
| Self-care | 5.1 (1.3) | 5.4 (1.2) | 5.4 (1.2) | 5.2 (1.3) | 5.1 (1.3) | 5.1 (1.3) | 5.1 (1.3) | 5.0 (1.3) | 5.0 (1.3) | 5.0 (1.3) | 5.0 (1.3) | 5.0 (1.3) |
| Sphincter | 5.0 (1.8) | 5.4 (1.6) | 5.4 (1.6) | 5.1 (1.8) | 4.9 (1.8) | 4.9 (1.8) | 4.9 (1.8) | 4.8 (1.8) | 4.8 (1.8) | 4.8 (1.8) | 4.8 (1.8) | 4.8 (1.8) |
| Transfer | 4.5 (1.4) | 4.9 (1.3) | 4.9 (1.3) | 4.7 (1.3) | 4.5 (1.4) | 4.5 (1.4) | 4.5 (1.4) | 4.4 (1.4) | 4.4 (1.4) | 4.4 (1.4) | 4.4 (1.4) | 4.4 (1.4) |
| Locomotion | 3.6 (1.6) | 3.8 (1.6) | 3.8 (1.6) | 3.6 (1.6) | 3.6 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) | 3.5 (1.6) |
| Communication | 5.9 (1.2) | 6.2 (1.2) | 6.1 (1.2) | 6.0 (1.2) | 5.9 (1.2) | 5.9 (1.2) | 5.9 (1.2) | 5.9 (1.2) | 5.8 (1.2) | 5.8 (1.2) | 5.8 (1.2) | 5.8 (1.2) |
| Social cognition | 5.5 (1.3) | 5.8 (1.4) | 5.8 (1.4) | 5.6 (1.4) | 5.5 (1.4) | 5.6 (1.3) | 5.6 (1.3) | 5.5 (1.3) | 5.4 (1.3) | 5.4 (1.3) | 5.4 (1.3) | 5.5 (1.3) |
| Change | ||||||||||||
| Self-care | 1.5 (1.0) | 1.3 (1.0) | 1.4 (1.0) | 1.3 (1.0) | 1.3 (1.0) | 1.3 (1.0) | 1.4 (1.0) | 1.4 (1.0) | 1.6 (1.1) | 1.6 (1.1) | 1.6 (1.1) | 1.6 (1.1) |
| Sphincter | 1.2 (1.7) | 1.2 (1.5) | 1.3 (1.5) | 1.2 (1.6) | 1.1 (1.6) | 1.1 (1.6) | 1.2 (1.6) | 1.2 (1.7) | 1.3 (1.7) | 1.3 (1.7) | 1.3 (1.7) | 1.3 (1.7) |
| Transfer | 1.7 (1.2) | 1.7 (1.1) | 1.8 (1.1) | 1.6 (1.1) | 1.6 (1.1) | 1.6 (1.2) | 1.6 (1.2) | 1.6 (1.2) | 1.7 (1.2) | 1.8 (1.2) | 1.8 (1.2) | 1.8 (1.2) |
| Locomotion | 1.9 (1.5) | 2.0 (1.5) | 2.0 (1.5) | 1.9 (1.5) | 1.8 (1.5) | 1.8 (1.4) | 1.9 (1.5) | 1.8 (1.5) | 1.9 (1.5) | 1.9 (1.5) | 1.9 (1.5) | 1.9 (1.5) |
| Communication | 0.5 (0.9) | 0.2 (0.7) | 0.2 (0.7) | 0.3 (0.8) | 0.3 (0.8) | 0.3 (0.8) | 0.4 (0.8) | 0.5 (0.9) | 0.6 (1.0) | 0.6 (1.0) | 0.7 (1.0) | 0.7 (1.0) |
| Social cognition | 0.5 (0.9) | 0.3 (0.7) | 0.3 (0.7) | 0.4 (0.8) | 0.4 (0.9) | 0.4 (0.9) | 0.5 (0.9) | 0.5 (0.9) | 0.7 (1.0) | 0.7 (1.0) | 0.7 (1.0) | 0.8 (1.0) |
Data are presented as mean (SD). Cell values represent mean ratings for individual FIM® items within a particular subscale. FIM® indicates Functional Independence Measure. Mean ratings for individual items range from 1 to 7.
Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Fiscal year 2000 only includes data from January through September 2000.
Self-care subscale includes eating, grooming, bathing, dressing – upper, dressing – lower, and toileting
Sphincter subscale includes bladder and bowel control
Transfer subscale includes bed/chair/wheelchair, toilet, and tub/shower
Locomotion subscale includes walk/wheelchair and stairs
Communication subscale includes comprehension and expression
Social cognition subscale includes social interaction, problem solving, and memory
Table 3 shows summary comparisons for age, LOS, and FIM ratings stratified by community discharge versus all other discharge settings combined. Patients who discharge to a community setting after rehabilitation were, on average, only 1.5 years younger than patients who discharged to other settings. LOS was 1.7 days shorter for the community discharge group in 2000. This difference decreased to 0.4 days shorter in 2003. The trend reversed with longer LOS for community discharges compared to other settings combined in 2007 – 2010. FIM total was about 10 points higher at admission and 24 points higher upon discharge for those who return to the community compared to an institution. This trend remained stable across the 11-year period. Efficiency gradually increased over time after 2003 and remained higher for persons discharged to the community (2.2 in 2000 to 2.8 in 2010) compared to an institution (0.9 in 2000 to 1.4 in 2010).
Table 3. Patient characteristics according to discharge setting stratified by discharge year.
| Community Discharge | Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, yrs | Yes | 73.9 (13.5) | 73.5 (13.5) | 73.7 (13.6) | 74.7 (13.1) | 74.8 (13.1) | 74.9 (13.0) | 74.4 (13.5) | 74.1 (13.5) | 74.0 (13.5) | 73.4 (13.6) | 73.1 (13.6) | 72.9 (13.8) |
| No | 75.4 (12.9) | 75.8 (12.4) | 75.9 (12.9) | 76.2 (12.4) | 76.5 (12.4) | 76.0 (13.0) | 75.7 (13.0) | 75.4 (13.0) | 75.4 (13.0) | 74.9 (12.9) | 74.6 (13.0) | 74.5 (13.2) | |
| Length of stay, days | Yes | 12.6 (7.1) | 13.9 (8.5) | 14.0 (10.3) | 12.8 (7.5) | 12.4 (6.5) | 12.4 (6.7) | 12.4 (7.6) | 12.1 (6.1) | 12.6 (6.3) | 12.5 (6.1) | 12.2 (5.9) | 12.2 (5.8) |
| No | 12.7 (8.5) | 15.6 (10.9) | 15.4 (10.5) | 13.3 (8.8) | 12.8 (8.7) | 12.3 (8.0) | 12.5 (8.3) | 12.1 (8.1) | 12.5 (8.7) | 12.3 (8.1) | 11.9 (7.5) | 11.7 (7.2) | |
| FIM® total admission | Yes | 69.3 (15.7) | 76.2 (15.1) | 75.7 (15.1) | 73.7 (15.5) | 71.9 (15.4) | 71.1 (15.0) | 70.6 (14.9) | 68.7 (15.1) | 65.9 (15.3) | 65.5 (15.3) | 65.2 (15.2) | 64.9 (15.2) |
| No | 58.9 (16.5) | 64.9 (17.1) | 64.6 (17.0) | 62.9 (16.9) | 61.6 (16.8) | 60.8 (16.6) | 60.6 (15.9) | 58.9 (16.1) | 56.1 (15.9) | 55.9 (15.6) | 55.8 (15.7) | 55.5 (15.6) | |
| FIM® motor admission | Yes | 42.8 (11.6) | 47.2 (11.6) | 46.8 (11.6) | 45.9 (11.6) | 44.7 (11.6) | 44.0 (11.3) | 43.5 (11.2) | 42.3 (11.2) | 40.7 (11.3) | 40.5 (11.3) | 40.3 (11.3) | 40.1 (11.3) |
| No | 35.2 (11.7) | 39.4 (12.2) | 39.0 (12.1) | 38.1 (12.0) | 37.0 (12.1) | 36.4 (11.7) | 36.1 (11.5) | 34.9 (11.5) | 33.3 (11.2) | 33.2 (11.0) | 33.1 (11.1) | 33.0 (11.0) | |
| FIM® cognition admission | Yes | 26.4 (6.6) | 28.9 (6.3) | 28.8 (6.3) | 27.9 (6.6) | 27.2 (6.5) | 27.1 (6.3) | 27.1 (6.3) | 26.4 (6.6) | 25.1 (6.6) | 25.1 (6.6) | 24.9 (6.6) | 24.8 (6.5) |
| No | 23.7 (7.5) | 25.4 (7.8) | 25.6 (7.7) | 24.9 (7.7) | 24.6 (7.6) | 24.4 (7.5) | 24.5 (7.3) | 24.0 (7.4) | 22.8 (7.5) | 22.7 (7.4) | 22.7 (7.3) | 22.4 (7.3) | |
| FIM® total discharge | Yes | 95.2 (16.2) | 99.6 (16.1) | 99.6 (16.0) | 97.0 (16.6) | 94.9 (16.4) | 94.9 (15.9) | 95.2 (15.8) | 94.0 (16.2) | 93.6 (16.0) | 93.6 (16.0) | 93.5 (16.1) | 94.1 (15.7) |
| No | 71.7 (20.8) | 77.0 (22.0) | 76.9 (21.9) | 73.7 (21.3) | 72.2 (21.3) | 71.8 (21.0) | 71.7 (20.8) | 70.9 (20.2) | 69.7 (20.3) | 69.9 (20.3) | 70.5 (20.2) | 70.5 (20.1) | |
| FIM® motor discharge | Yes | 65.9 (12.9) | 69.1 (12.7) | 69.2 (12.7) | 67.2 (13.1) | 65.5 (13.1) | 65.5 (12.8) | 65.6 (12.6) | 64.8 (12.9) | 64.9 (12.8) | 64.8 (12.8) | 64.7 (12.8) | 65.1 (12.6) |
| No | 46.4 (16.3) | 50.8 (16.9) | 50.5 (17.0) | 48.1 (16.6) | 46.6 (16.6) | 46.3 (16.4) | 46.1 (16.5) | 45.5 (15.9) | 44.9 (15.9) | 45.0 (15.9) | 45.4 (15.8) | 45.4 (15.9) | |
| FIM® cognition discharge | Yes | 29.3 (5.4) | 30.5 (5.4) | 30.4 (5.3) | 29.8 (5.6) | 29.4 (5.4) | 29.4 (5.3) | 29.6 (5.3) | 29.2 (5.4) | 28.7 (5.4) | 28.8 (5.4) | 28.8 (5.4) | 29.0 (5.2) |
| No | 25.4 (7.4) | 26.3 (7.9) | 26.4 (7.7) | 25.6 (7.7) | 25.6 (7.5) | 25.5 (7.5) | 25.6 (7.3) | 25.4 (7.3) | 24.8 (7.3) | 24.9 (7.2) | 25.1 (7.1) | 25.1 (7.1) | |
| FIM® total change | Yes | 25.9 (12.6) | 23.4 (11.0) | 24.0 (11.2) | 23.2 (11.5) | 23.0 (12.1) | 23.8 (12.0) | 24.6 (11.9) | 25.3 (12.2) | 27.7 (13.0) | 28.1 (13.0) | 28.3 (13.0) | 29.2 (13.3) |
| No | 12.8 (14.9) | 12.2 (14.5) | 12.2 (14.5) | 10.8 (14.4) | 10.6 (14.4) | 10.9 (14.6) | 11.1 (14.6) | 12.0 (14.1) | 13.6 (14.9) | 14.0 (15.2) | 14.6 (15.5) | 15.1 (15.1) | |
| FIM® motor change | Yes | 23.0 (10.7) | 21.9 (10.0) | 22.4 (10.1) | 21.3 (10.2) | 20.8 (10.6) | 21.5 (10.6) | 22.1 (10.4) | 22.5 (10.6) | 24.1 (10.9) | 24.4 (10.9) | 24.4 (10.9) | 25.0 (11.1) |
| No | 11.2 (12.2) | 11.3 (12.2) | 11.5 (12.3) | 10.1 (11.9) | 9.7 (12.0) | 9.9 (12.1) | 10.0 (12.2) | 10.6 (11.8) | 11.6 (12.1) | 11.9 (12.3) | 12.3 (12.4) | 12.4 (12.3) | |
| FIM® cognition change | Yes | 2.9 (4.1) | 1.5 (3.0) | 1.6 (3.0) | 1.9 (3.3) | 2.2 (3.6) | 2.3 (3.6) | 2.5 (3.7) | 2.8 (4.0) | 3.6 (4.4) | 3.7 (4.5) | 3.9 (4.5) | 4.2 (4.6) |
| No | 1.6 (4.9) | 0.8 (4.1) | 0.7 (4.1) | 0.7 (4.6) | 1.0 (4.5) | 1.0 (4.6) | 1.1 (4.4) | 1.4 (4.6) | 2.0 (5.0) | 2.1 (5.1) | 2.4 (5.3) | 2.7 (5.2) | |
| Efficiency (change/ day) | Yes | 2.5 (1.7) | 2.2 (1.7) | 2.2 (1.6) | 2.2 (1.5) | 2.2 (1.5) | 2.3 (1.6) | 2.4 (1.6) | 2.5 (1.6) | 2.6 (1.7) | 2.6 (1.8) | 2.7 (1.7) | 2.8 (1.8) |
| No | 1.1 (2.2) | 0.9 (1.6) | 0.9 (2.2) | 0.8 (2.3) | 0.8 (2.4) | 0.9 (2.0) | 0.9 (2.2) | 1.0 (2.0) | 1.1 (2.1) | 1.2 (2.2) | 1.3 (2.3) | 1.4 (2.1) |
Data are presented as mean (SD). FIM® indicates Functional Independence Measure. FIM® motor subscale includes 13 items assessing self care, sphincter control, transfers, and locomotion. FIM® cognition subscale includes 5 items assessing communication and social cognition. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Fiscal year 2000 only includes data from January through September 2000.
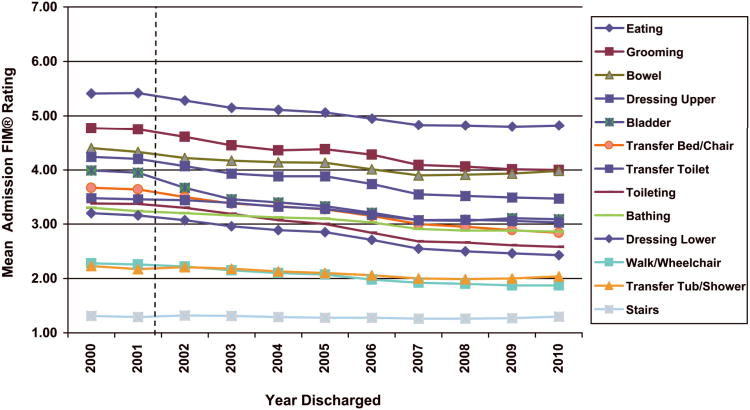
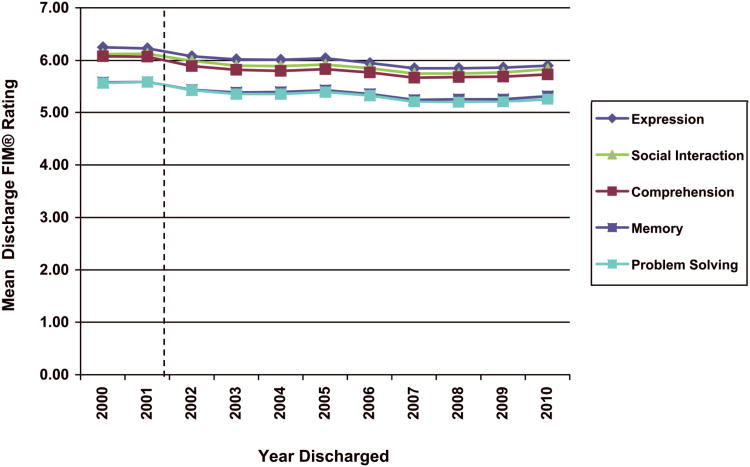
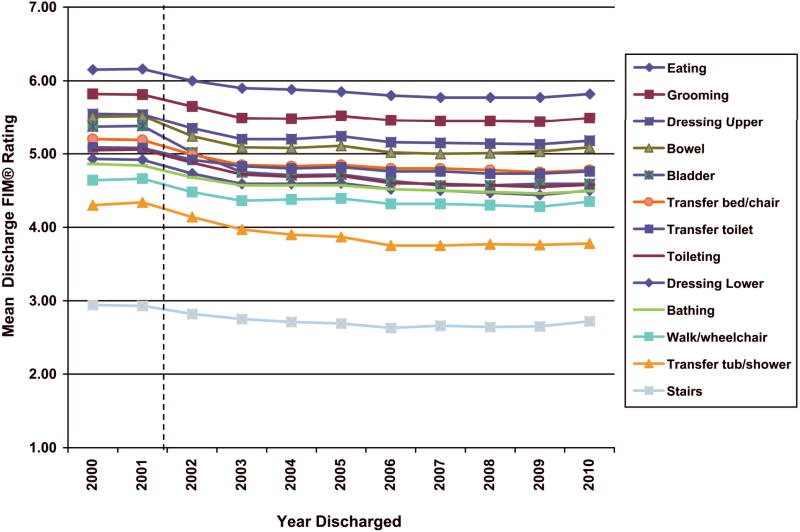
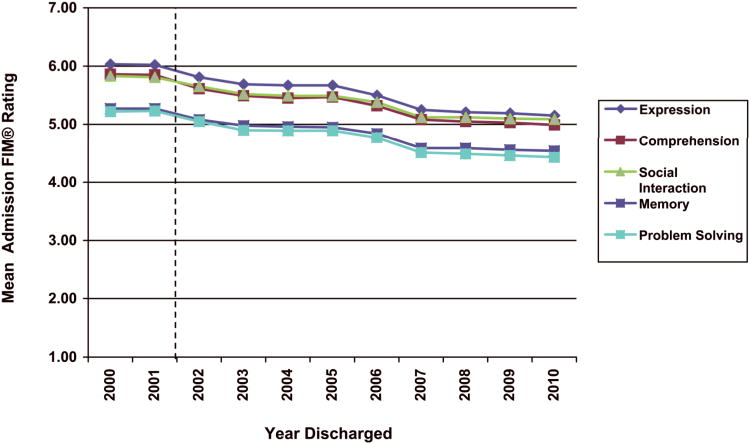
Figures 4-7 collectively display mean ratings for all 18 FIM items. These figures depict average admission and discharge ratings for motor and cognitive subscale items across the 11-year period. Among the 13 motor items, patients with debility displayed the least independence with stair mobility, followed by tub/shower transfers, and walking/wheelchair use (Figures 4 and 5). Figure 6 depicts a slight decrease in admission cognition scores from 2001 to 2007. This change is less pronounced for the discharge cognition scores with an overall plateau from 2002 to 2010 (Figure 7).
Figure 4.
Mean ratings for individual FIM® motor items at admission to inpatient rehabilitation. FIM® indicates Functional Independence Measure. Ratings for individual FIM® items range from 1 to 7. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Figure 7.
Mean ratings for individual FIM® cognitive items at discharge from inpatient rehabilitation. FIM® indicates Functional Independence Measure. Ratings for individual FIM® items range from 1 to 7. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Figure 5.
Mean ratings for individual FIM® motor items at discharge from inpatient rehabilitation. FIM® indicates Functional Independence Measure. Ratings for individual FIM® items range from 1 to 7. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Figure 6.
Mean ratings for individual FIM® cognitive items at admission to inpatient rehabilitation. FIM® indicates Functional Independence Measure. Ratings for individual FIM® items range from 1 to 7. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Case Severity
CMG assignment was introduced as part of the PPS in 2002. Table 4 includes CMG data from that year forward. CMGs for debility were derived from motor FIM ratings and age (for the lowest motor FIM range) in discharge years 2002 through 2005.8;9 From 2006 forward, CMGs were calculated from weighted motor FIM ratings.24 Higher CMG indicates lower motor FIM. The number of CMGs for debility decreased from five to four in Federal fiscal year 2006. CMG 2001 decreased from 14% in 2000 to 4.4% in 2010. CMG 2003 accounted for about one-third of debility cases across all years. Combined CMGs 2004 and 2005 increased from 22% in 2000 to 39% in 2010.
Table 4. Case-mix groups (CMG) stratified by discharge year.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|
| CMG 2001 | 13.9% | 11.4% | 10.1% | 7.9% | 6.1% | 4.8% | 4.9% | 4.6% | 4.4% |
| CMG 2002 | 29.7% | 29.7% | 27.5% | 29.0% | 27.0% | 23.5% | 22.1% | 21.3% | 21.2% |
| CMG 2003 | 34.4% | 34.6% | 36.7% | 36.6% | 35.9% | 35.9% | 36.0% | 36.0% | 35.5% |
| CMG 2004 | 8.4% | 12.2% | 9.0% | 22.3% | 31.1% | 35.8% | 37.0% | 38.1% | 39.0% |
| CMG 2005 | 13.7% | 12.1% | 16.7% | 4.3% |
Data are presented as percentage. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services.
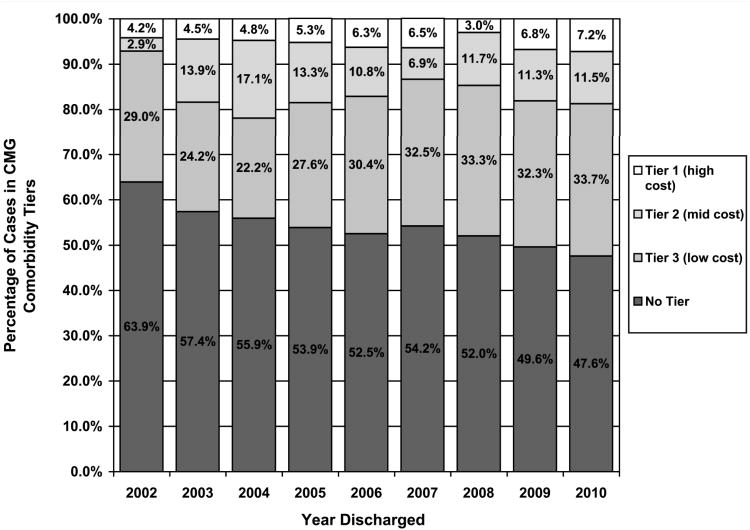
Figure 8 shows the percentages of patients assigned to each CMG comorbidity tier. The tier criteria have been revised over the years,24 and the figure represents the tier structure in place for that year. Overall, about half of debility cases were classified as no tier. Tier 1 (high cost) accounted for 4% to 7% of debility cases.
Figure 8.
Relative proportions of CMG comorbidity tier assignment under the prospective payment systems (PPS) by discharge year. CMG indicates case-mix group. Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services.
Deaths
Approximately 0.3% of patients died during inpatient rehabilitation over the 11-year study period. Comparison of yearly values for those who died (Table 5) with the values of those who survived (Table 1) shows that patients who died were approximately 2.8 years older with an admission functional status about 11 FIM points lower than those who survived. Of this FIM total difference, FIM motor admission subscale accounted for 8 points; FIM cognition admission difference was 3 points (data not shown).
Table 5. Characteristics of patients who died during inpatient rehabilitation by year of death.
| Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Died, N | 769 | 65 | 102 | 68 | 77 | 70 | 54 | 59 | 71 | 80 | 65 | 58 |
| Died, % | 0.3% | 0.4% | 0.4% | 0.4% | 0.4% | 0.3% | 0.3% | 0.3% | 0.3% | 0.3% | 0.2% | 0.2% |
| Age, yrs | 77.0 (12.7) | 76.3 (12.0) | 77.5 (12.1) | 78.2 (12.1) | 76.6 (12.4) | 78.8 (12.6) | 75.2 (13.5) | 77.9 (10.7) | 78.1 (11.9) | 76.6 (12.5) | 77.2 (13.5) | 73.8 (16.3) |
| FIM® total admission | 55.7 (18.4) | 61.3 (19.9) | 61.5 (17.8) | 56.7 (19.7) | 55.6 (17.7) | 60.0 (16.2) | 54.7 (20.4) | 55.1 (17.7) | 51.2 (17.7) | 53.0 (18.1) | 50.2 (16.8) | 49.6 (16.0) |
| FIM motor admission | 32.7 (12.3) | 36.8 (12.7) | 36.1 (12.1) | 33.3 (13.1) | 32.2 (12.8) | 35.1 (11.3) | 32.3 (14.2) | 32.4 (11.8) | 29.9 (10.9) | 30.9 (12.1) | 29.3 (10.7) | 29.4 (10.7) |
| FIM cognition admission | 23.0 (8.3) | 24.5 (9.4) | 25.3 (8.4) | 23.4 (8.8) | 23.4 (7.5) | 24.9 (7.7) | 22.4 (8.9) | 22.8 (8.1) | 21.4 (8.3) | 22.1 (8.4) | 20.9 (7.7) | 20.2 (7.1) |
| Length of stay, days | 9.6 (9.3) | 9.9 (7.1) | 10.8 (8.5) | 10.7 (8.9) | 9.8 (9.4) | 8.8 (6.0) | 11.5 (20.5) | 8.8 (6.6) | 7.7 (6.2) | 9.7 (7.2) | 9.5 (8.7) | 8.4 (7.9) |
Data are presented as mean (SD). FIM® indicates Functional Independence Measure.
Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Fiscal year 2000 only includes data from January through September 2000.
Note: % is calculated from sample with complete data.
Debility Impairment Group
The debility group includes “cases with generalized deconditioning not attributable to any of the other Impairment Groups.”8;9 The IRF-PAI training manual specifies that the debility for this impairment group code is not secondary to cardiac or pulmonary conditions;8;9 other codes exist for deconditioning associated with these conditions. The most prevalent etiologic diagnosis for the debility impairment group is 799.3 “Debility, unspecified.”11 However, the prevalence of this diagnostic code has decreased from 40% in 2000 to only 12% of debility cases in 2010 (Table 6). The “other” diagnoses represented 81% of debility cases in 2010 and include numerous medical conditions such as infections and multisystem pathologies.
Table 6. Debility diagnosis groups stratified by discharge year.
| Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Debility | 27.1% | 40.1% | 41.4% | 41.2% | 42.8% | 37.1% | 31.4% | 27.8% | 19.6% | 16.3% | 13.5% | 11.6% |
| Generalized Weakness | 8.7% | 6.6% | 5.6% | 11.7% | 13.7% | 12.4% | 10.0% | 10.4% | 8.1% | 7.2% | 6.3% | 6.8% |
| Other | 61.4% | 40.1% | 40.3% | 42.6% | 42.5% | 49.6% | 57.9% | 61.2% | 71.4% | 76.0% | 79.7% | 80.8% |
Data are presented as percentages. Etiologic diagnosis was missing for 2.8% of cases which were not included this table.
Yearly summaries represent fiscal year periods (October 1 to September 30) from the Centers for Medicare and Medicaid Services. Fiscal year 2000 only includes data from January through September 2000.
Debility indicates ICD-9-CM code for debility (799.3); Generalized weakness indicates ICD-9-CM code 728.2, 728.87, or 780.79); Other indicates any other ICD-9-CM code. Data represent the ICD-9-CM codes listed for etiologic diagnosis on the Inpatient Rehabilitation Facilities – Patient Assessment Instrument.
Discussion and Conclusions
This report provides aggregated national summary statistics of characteristics and outcomes for 260,373 patients with debility discharged from inpatient medical rehabilitation programs from 2000 through 2010. Caution must be applied when interpreting year-to-year changes or trends in the data presented in this report. Changes over time may be related to CMS-mandated modifications in documentation, admission eligibility, and/or reimbursement processes implemented during the years covered. In addition, the number of inpatient rehabilitation facilities varied slightly across the years.
Patient characteristics of gender, race/ethnicity, and marital status show consistent patterns across years with the dominant demographic categories being female, non-Hispanic white, and not married. Seventy-five years and older represents the largest age category with Medicare being the most common primary insurance. Most patients were admitted to inpatient rehabilitation directly from acute care and previously lived with others.
Admission FIM ratings declined gradually over the 11-year period (Figure 2). Discharge FIM ratings remained relatively stable after a decline from 2001 to 2003 (Figure 2). Therefore, the magnitude of FIM change increased from 2003 to 2010 (Figure 3). LOS was slightly higher in 2000-2001 compared to PPS years and is partially explained by the PPS changes. Comparison of FIM item ratings reveal the greatest difficulty with stair mobility, which is consistent with other rehabilitation impairment groups.1-4 Stair mobility, tub/shower transfers, and walking/wheelchair use had mean admission ratings below 3.0, which indicate the need for more than moderate (50 - 74%) assistance to perform the activity.
The decline in percentage of patients discharge to community settings may be related to multiple factors including, but not limited to, the PPS changes, the patient's functional abilities, social support and resources, and policies and procedures impacting admission and discharge patterns. PPS definition changes in program interruptions had a corresponding change in discharges to acute care (Figure 1). In PPS years, percentage of discharges to acute care was higher for patients with debility (11-14%) compared to patients with lower limb joint replacement (2-3%)3, hip fracture (7-8%),4 stroke (9-11%), and traumatic brain injury (8-11%).2 Acute care discharge outcome for patients with debility is closer to the 2002 – 2010 benchmark for patients with traumatic spinal cord injury (10-13%).5 The high rate of discharge to acute care for patients with debility warrants further investigation.
This study examined all cases in the debility impairment group from 2000 to 2010 that met inclusion criteria. This impairment group represents cases with heterogeneous medical conditions, as exemplified in Table 6. The extent to which coding practices and policy changes influenced the etiologic diagnoses associated with debility is unknown. The common factor among these patients is functional impairment with deconditioning. This study contributes important yearly benchmark information to existing literature examining patients with debility.27-29 The UDSMR recommends that when rehabilitation facilities compare their own data with published benchmark information, they should: (1) identify by discharge date the period of interest using at least a full year of data, (2) include information on all patients within the pertinent impairment group and period under review, and (3) include statistics that show patient variability such as standard deviations. Meaningful comparison of outcomes between facility and national data requires case-mix adjustment.
The information presented in this report using national data from the UDSMR provides descriptive statistics for the rehabilitation impairment category of debility. This article and previous articles in this series, examining UDSMR data are designed to provide the field with descriptive benchmark information. These articles are not designed to answer specific research questions or to statistically evaluate data based on a hypothesis. Rather, the goal is to report data and information regarding the status of relevant indicators for rehabilitation. This information can be used to generate scientific, clinical, and policy questions of interest to rehabilitation professionals, researchers, administrators, and individuals and their families.
Acknowledgments
This study was supported in part by grants from the National Institutes of Health (R24 HD065702) and the National Institute on Disability and Rehabilitation Research (H133G080163). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The agencies did not influence the design, analysis or interpretation of the study results. The FIM Instrument is a registered trademark of the Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
Footnotes
Disclosures: Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Granger CV, Markello SJ, Graham JE, Deutsch A, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: Report of patients with stroke discharged from Comprehensive Medical Programs in 2000-2007. Am J Phys Med Rehabil. 2009;88:961–972. doi: 10.1097/PHM.0b013e3181c1ec38. [DOI] [PubMed] [Google Scholar]
- 2.Granger CV, Markello SJ, Graham JE, Reistetter TA, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: Report of patients with traumatic brain injury discharged from rehabilitation programs in 2000-2007. Am J Phys Med Rehabil. 2010;89:265–278. doi: 10.1097/PHM.0b013e3181d3eb20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: Report of patients with lower limb joint replacement discharged from rehabilitation programs in 2000-2007. Am J Phys Med Rehabil. 2010;89:781–794. doi: 10.1097/PHM.0b013e3181f1c83a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: Report of patients with hip fracture discharged from comprehensive medical programs in 2000-2007. Am J Phys Med Rehabil. 2011;90:177–189. doi: 10.1097/PHM.0b013e31820b18d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Granger CV, Karmarkar AM, Graham JE, et al. The Uniform Data System for Medical Rehabilitation: Report of patients with traumatic spinal cord injury discharged from rehabilitation programs in 2002-2010. Am J Phys Med Rehabil. 2012;91:289–299. doi: 10.1097/PHM.0b013e31824ad2fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deutsch A, Fiedler RC, Granger CV, Russell CF. The Uniform Data System for Medical Rehabilitation report of patients discharged from comprehensive medical rehabilitation programs in 1999. Am J Phys Med Rehabil. 2002;81:133–142. doi: 10.1097/00002060-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. [Accessed 3-17-2012];2012 Available at: www.medpac.gov.
- 8.UB Foundation Activities. Inpatient Rehabilitation Facility - Patient Assessment Instrument (IRF-PAI) Training Manual. [Accessed 4-24-2012];2004 Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/downloads//irfpaimanual040104.pdf.
- 9.UB Foundation Activities. Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) Training Manual. [Accessed 4-24-2012];2002 Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/downloads//irfpai-manualint.pdf.
- 10.UDSMR. [Accessed 3-1-2011];2011 Available at: www.udsmr.org.
- 11.International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) 6th. Los Angeles: Practice Management Information Corporation; 2000. [Google Scholar]
- 12.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the Functional Independence Measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74:531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 13.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the Functional Independence Measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 14.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: Tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77:1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 15.Corrigan JD, Smith-Knapp K, Granger CV. Validity of the functional independence measure for persons with traumatic brain injury. Arch Phys Med Rehabil. 1997;78:828–834. doi: 10.1016/s0003-9993(97)90195-7. [DOI] [PubMed] [Google Scholar]
- 16.Granger C, Cotter A, Hamilton B, Fiedler R, Hens M. Functional assessment scales: a study of persons with multiple sclerosis. Arch Phys Med Rehabil. 1990;71:870–875. [PubMed] [Google Scholar]
- 17.Granger CV, Cotter A, Hamilton D, Fiedler R. Functional assessment scales: a study of persons after stroke. Arch Phys Med Rehabil. 1993;74:133–138. [PubMed] [Google Scholar]
- 18.Hamilton BB, Deutsch A, Russell C, Fiedler RC, Granger CV. Relation of disability costs to function: spinal cord injury. Arch Phys Med Rehabil. 1999;80:385–391. doi: 10.1016/s0003-9993(99)90274-5. [DOI] [PubMed] [Google Scholar]
- 19.Disler PB, Roy CW, Smith BP. Predicting hours of care needed. Arch Phys Med Rehabil. 1993;74:139–143. [PubMed] [Google Scholar]
- 20.Granger CV. The emerging science of functional assessment: our tool for outcomes analysis. Arch Phys Med Rehabil. 1998;79:235–240. doi: 10.1016/s0003-9993(98)90000-4. [DOI] [PubMed] [Google Scholar]
- 21.Carter GM, Relles DA, Ridgeway GK, Rimes CM. Measuring function for Medicare inpatient rehabilitation payment. Health Care Financ Rev. 2003;24:25–44. [PMC free article] [PubMed] [Google Scholar]
- 22.Deutsch A, Granger CV, Russell C, Heinemann AW, Ottenbacher KJ. Apparent changes in inpatient rehabilitation facility outcomes due to a change in the definition of program interruption. Arch Phys Med Rehabil. 2008;89:2274–2277. doi: 10.1016/j.apmr.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 23.Granger CV, Deutsch A, Russell C, Black T, Ottenbacher KJ. Modifications of the FIM instrument under the inpatient rehabilitation facility prospective payment system. Arch Phys Med Rehabil. 2007;86:883–892. doi: 10.1097/PHM.0b013e318152058a. [DOI] [PubMed] [Google Scholar]
- 24.Federal Register. Medicare Program; Inpatient rehabilitation facility prospective payment system for FY 2006; Final rule. 156. Vol. 70. Department of Health and Human Services: Centers for Medicare & Medicaid Services; Aug 15, 2005. pp. 47880–48006. [PubMed] [Google Scholar]
- 25.Carter GM, Buchanan JL, Buntin MB, et al. Executive Summary of Analyses for the Initial Implementation of the Inpatient Rehabilitation Facility Prospective Payment System. Santa Monica, CA: Rand Corporation; 2002. [Google Scholar]
- 26.Federal Register. Medicare Program; Changes to the Inpatient Rehabilitation Facility Prospective Payment System and Fiscal Year 2004 Rates. 148. Vol. 68. Department of Health and Human Services: Centers for Medicare & Medicaid Services; Jan 8, 2003. pp. 45674–45728. [PubMed] [Google Scholar]
- 27.Haley R, Sullivan DH, Granger CV, Kortebein P. Inpatient rehabilitation outcomes for older adults with nondebility generalized weakness. Am J Phys Med Rehabil. 2011;90:791–797. doi: 10.1097/PHM.0b013e31822deaf4. [DOI] [PubMed] [Google Scholar]
- 28.Kortebein P, Bopp MM, Granger CV, Sullivan DH. Outcomes of inpatient rehabilitation for older adults with debility. Am J Phys Med Rehabil. 2008;87:118–125. doi: 10.1097/PHM.0b013e3181588429. [DOI] [PubMed] [Google Scholar]
- 29.Kortebein P, Granger CV, Sullivan DH. A comparative evaluation of inpatient rehabilitation for older adults with debility, hip fracture, and myopathy. Arch Phys Med Rehabil. 2009;90:934–938. doi: 10.1016/j.apmr.2008.12.010. [DOI] [PubMed] [Google Scholar]