Abstract
The workplace may be an ideal venue for engaging African American women in behavioral interventions for weight reduction. This study examines the effectiveness of a culturally-enhanced EatRight dietary intervention among a group of predominately African American women in a workplace setting. Thirty-nine women volunteered for this cross-over design study, with 27 completing. The control period involved observation of participants for 22 weeks after receiving standard counseling on lifestyle methods to achieve a healthy weight; following the control period, participants crossed over to the 22-week intervention period. The intervention was culturally-enhanced using feedback derived from formative assessment and delivered as 15 group sessions. The primary outcome measure was the difference in weight change between the control and intervention periods; changes in waist circumference and quality of life were secondary outcomes. Most participants were obese with a mean baseline body mass index of 36 kg/m2, weight of 97.9 kg and waist circumference of 111 cm. Weight increased during the control period by 0.7 kg but decreased by 2.6 kg during the intervention (net difference = −3.4 kg, p<0.001), with 30% of participants losing ≥5% of body weight. Compared to the control period, there was a significant decrease in waist circumference (−3.6 cm, p = 0.006) and improvement in weight-related quality of life (5.7, p = 0.03). This pilot study demonstrated the feasibility of a culturally-enhanced behavioral weight loss intervention in a predominately African American workplace setting. The workplace may be conducive for targeting African American women who are disproportionately affected by obesity.
African American women have a prevalence of obesity of 53.9%, 20% higher than that of non-Hispanic Caucasian women. The prevalence of obesity in African American women has increased by 4.4% since 1999 based on data from the CDC and at a much higher rate than other major ethnic-gender subgroups. As a result of the increasing rates of obesity among African American women, many more African American women will be at risk for suffering from chronic diseases related to being obese. The severe health consequences associated with obesity for African American women typically involve increased risk of diabetes, hypertension, and impaired mobility due to arthritis and joint pain (1).
The adverse effects of obesity for African American women extend beyond personal health into other arenas. Nowhere is this truer than in the area of the impact of obesity on employers. Obesity has been shown to be associated with increased absenteeism, decreased productivity, and higher medical insurance cost (2, 3). Many of these factors are related to direct health effects from being obese and have a significant impact on the productivity of the company (4). Previous studies have shown that workplace wellness programs focused on weight control can lead to improvements in absenteeism and productivity, while decreasing expenditures for medical care (5, 6). Employers may have a vested interest in improving the health of their work force using these types of programs, and increasingly, the work force includes more African American women. African American women represented the largest share of minority women's employment from 1990 to 2001 with 7.6 percent of employment in 2001 (7). During this time frame, there was a 43% increase in the employment of African American women (7). As more African American women make up larger percentages of the work force, employers may increasingly find the need to focus specifically on the health of their female African American employees.
One type of intervention that may be particularly useful to address this issue of increasing obesity within the workforce is the use of low energy dense food items to promote decreases in caloric intake. Energy density is defined as the calories per gram weight of a food item (8–10). Foods that are low in energy density typically have high water content and/or a low fat content. Low energy density dietary patterns have been shown to result in significant weight loss and to be associated with maintenance of weight over 2 years (11–13). Weight reduction is typically achieved by calorie restriction created as a result of decreasing the overall energy density of a given meal. This can be accomplished by increasing the intake of fruit and vegetables, eating low energy dense soups or salads prior to the meal, or adding fruit and vegetables to recipes that may not typically call for these items (8–10). This strategy has been a central component of the University of Alabama at Birmingham (UAB) EatRight Lifestyle program since its inception (10,14,15). The EatRight Lifestyle program not only focuses on promoting a low energy dense dietary pattern for weight management, but the program also encourages increased physical activity, which can play a key role in creating the energy deficit needed to achieve weight loss by increasing energy expenditure.
We wanted to use the dietary intervention strategy of lowering energy density in a workplace setting that was predominately African American (95% African American, 4% Caucasian, 1% other). To effectively deliver the intervention, we chose to use a culturally specific framework to design and implement the behavior change intervention (16). The purpose of this pilot was to determine the effectiveness of a culturally enhanced EatRight dietary intervention delivered in a workplace setting that included predominately African American women. The primary outcome was change in weight after the six-month intervention. Secondary outcomes included change in waist circumference and quality of life.
Methods
Study Design and Recruitment
This study utilized a sequential, control to intervention cross-over design. This study design was chosen to avoid contamination and enhance participation in the intervention period. Each study period was 22 weeks in duration. The study was announced to all agency employees via flyers posted at workplaces and announcements added to paycheck mailers. All participants provided informed consent, and this study was reviewed and approved by the University of Alabama at Birmingham Institutional Review Board to ensure the protection of human subjects. Participants were reimbursed $20 for completion of each assessment visit (baseline, end of control, end of intervention).
Participants
As a stipulation of our partnership with the local agency, study enrollment was open to all agency employees. According to the agency’s human resources director, the workforce is approximately 95% African American, 4% Caucasian, and 1% other. We recruited 39 participants. Two participants that completed the study are excluded from the analysis. One participant was prescribed weight loss medication during the control period and discontinued the use of the medication after the crossover. A second participant joined the study to improve her overall eating habits, but with a primary goal of gaining weight. Of the remaining 37 participants, 6 did not return for the control period follow-up, 2 additional participants did not attend any of the subsequent intervention sessions and 2 did not complete the active intervention. Reasons given for these 10 non-completers include subsequent job conflicts (n = 5), health issues (n = 1), or lack of interest/reason not known (n = 4). Of the 29 participants that actually began the intervention, follow up weights were obtained on 27 (67.5% of the initial cohort; 93.1% of the intervention cohort).
Control period
Participants who inquired about enrolling in the study completed a baseline assessment within one month of the inquiry. Following the baseline assessment, participants received a usual care intervention that consisted of one counseling session during one of several health fairs held at the workplace between January 18, 2006 and February 23, 2006. The counseling session included written material on approaches for adopting a healthy lifestyle to improve health conditions such as overweight/obesity, hypertension, and diabetes. Participants also received 2 newsletters during the control period, which lasted 22 weeks on average. The newsletters included one healthy recipe idea and a brief article on a behavioral approach to improve their lifestyle. At the completion of the control period, a series of repeat assessments were obtained.
Intervention period
The intervention period lasted from June 26, 2006 through November 14, 2006, for a total of 15 intervention sessions. The intervention was delivered in a group setting and led by a registered dietitian. Intervention sessions were typically 60–90 minutes in duration and covered the material from the modified EatRight intervention materials. Weekly sessions were provided either after typical working hours or during the work day. Participants chose to attend either the day session (held during the work day and located at an agency facility) or the evening sessions (conducted after work at the university).
Culturally Modified EatRight Intervention
The EatRight Program is based on the concept of “time-calorie displacement,” which emphasizes the ingestion of large quantities of high-bulk, low-energy-density foods (primarily vegetables, fruits, high-fiber grains, and cereals) and moderation in high-energy-density foods (meats, cheeses, sugars, and fats) (10,15). The program also uses basic principles of behavior modification related to dietary and physical activity habits to promote a calorie deficit and achieve moderate weight loss goals.
The modification of the EatRight material followed the approach of Ard et al (16,17) and details of the process are published elsewhere (18). In brief, the control period was used as a time to complete a formative assessment to inform the modification of the standard EatRight materials. During the formative assessment, we gathered information from a series of group meetings with agency employees using the Nominal Group Technique (NGT; 19).
Qualitative data collection was an essential first step to tailoring the materials into a usable form that fit with the cultural traditions of this area. It was our intent that the NGT capture African Americans’ views of their culture while addressing potential investigator bias. The NGT sessions were designed to generate responses from the participants to a given question. A moderator facilitated the session and asked the question and a research assistant posted responses on a flipchart at the front of the room and operated the digital voice recorders. This process included participants sharing their responses in a round-robin fashion and ranking their top three most relevant items. These responses were used to adapt the current EatRight materials into a more culturally appropriate intervention.
Based on the setting of this intervention, we wanted to deal with the impact of a high-demand job environment and its role in affecting eating behaviors. Given the target demographic, it was also considered important to address the cultural attitudes and beliefs that were prevalent within the agency regarding dietary habits, body image/appearance, wellness, and physical activity. With these objectives in mind, we wanted to identify core values of the participants and gather responses to the following two questions: “What factors about your job affect your weight?” and “What factors in your daily life affect your amount of physical activity?” Each question was directed to two small groups of participants, resulting in a total of four NGT sessions. A total of 14 participants were involved in NGT sessions; no educational materials were presented or reviewed, and no intervention was provided during the NGT sessions. The research team discussed the responses and through consensus combined similar responses/ideas into themes. The themes and supporting statements were then used to direct the modification of the standard EatRight material. The primary goal of the research team was to decrease inherent bias in the intervention, where bias represents the ethnocentric perspective of the existing material, which may be a different perspective than that of the target audience (i.e., primarily African American, middle class women). The research team used the themes and supporting statements to systematically identify differences and potential conflicts between the standard intervention and core values of the study participants. The differences and conflicts were resolved by integrating new material and/or removing previous material as necessary, resulting in the addition of new topic areas, practical examples, and intervention principles that were congruent with core values, thereby decreasing the intervention bias. For example, the research team identified a need for developing skills to handle the stress of the work environment and demands of multiple roles in daily life (e.g., bread winner, mother, care giver, supervisor, etc). As a result a new module was developed and delivered early in the intervention given the relative importance of this topic as expressed by NGT participants. Table 1 shows a list of topic areas and the associated modifications covered during the intervention sessions.
Table 1.
Lessons for Intervention Sessions
| Week | Topic | Associated NGT Theme/Responses |
Adaptations |
|---|---|---|---|
| 1* | Getting started/Stress Management | High stress level at work | Discovering how to deal with job demands and exploring alternatives to eating high-energy dense food in reaction to stress |
| 2* | Self Observation | Multiple roles: -Mother -Caretaker -Various demands at work and in social life |
Teach self-care and assertiveness training |
| 3* | Goal Setting/Meal Plan | Lack of social support for healthy behaviors | Increase self-efficacy with self-monitoring and meal planning |
| 4* | Stress Management | ||
| 5* | Dining Out | Unhealthy food environment at work and in immediate vicinity of work place | Learning about portion size, keeping healthy snacks in your desk, and making healthy fast food choices |
| 6* | Problem Solving/Portion Control | Lack of social support for healthy behaviors | Learning how to politely decline “food pushers”, deal with others’ perceptions |
| 7 | Mindful eating/Eating personality | ||
| 8 | Healthy Holidays | ||
| 9 | In-depth Goal Setting | ||
| 10* | Meal and Snack Planning/Label Reading | Social eating behaviors -Co-workers bring sweets to share -Social norms |
Encourage reciprocal determinism and observational learning (healthy interactions to influence each other) |
| 11 | Grocery Guide | ||
| 12* | Physical Activity | Time management: -No time to exercise -Watching too much TV |
Practical examples of managing time, including best time of day to exercise based on personality, identifying enjoyable activities, fitting in small amounts of physical activity, and finding places to walk near worksite |
| 13 | Review of Lifestyle Changes | ||
| 14 | Quick Cooking/Meal Assembly | ||
| 15 | Long-term planning |
session modified from original EatRight
Measures
Study participants completed one clinic visit at 3 time points to measure waist circumference (cm) 1 cm above the umbilicus using a Gullick II (spring tension) tape measure; height (cm) using a wall-mounted stadiometer; and weight (kg) in light clothing without shoes, using a Tanita digital scale (Model #BWB500A). Blood pressure was measured on the right arm using an Omron automated sphygmomanometer (Model # HEM-907XL) following an initial 5 minute rest period. Each measure was obtained twice and averaged to determine the study value. Quality of life and how it is affected by body weight was assessed using the Impact of Weight on Quality of Life questionnaire (IWQOL) (20). Venipuncture blood samples were collected after confirming a 10 hour fasting period prior to the visit. Serum samples were analyzed for glucose, insulin, and total cholesterol.
Statistical Analysis
Descriptive statistics were calculated and summarized as means, medians and frequencies for all study participants. Change in weight was determined for time points control – baseline (control weight change) and end of intervention – control (intervention weight change); a negative weight change indicates weight loss. Similar procedures were followed for waist circumference and quality of life. Negative changes in quality of life indicate worsening self-rated quality of life, while negative changes in waist circumference indicate decreasing waist size. All participants who attended at least one intervention session were included in the analysis. Last available observations were carried forward for the two participants who did not complete end of intervention measures. The primary statistical comparison was between the control change and the intervention change (net difference) using a paired t-test. All analyses were conducted in SPSS Ver. 13, and a p value of < 0.05 was deemed statistically significant.
Results
The sociodemographic characteristics of active study participants at the time of enrollment are shown at each study measurement time point in table 2. In general, this was a group of middle-aged women with at least high school educations and middle-class incomes. Most rated their health to be only good or fair. At least 27% of the study sample was taking a medication for one or more of the following conditions: hypertension (27%), diabetes mellitus (10.8%), and/or hyperlipidemia (10.8%). The majority of participants attended the daytime sessions (n = 24) and a smaller group (n = 5) chose the evening sessions. On average, daytime and evening participants attended 58% and 70% of sessions, respectively (38% of daytime participants and 40% of evening participants attended at least 75% of all sessions). There was no discernible demographic pattern of study drop out.
Table 2.
Baseline sociodemographic characteristics of study sample retained at each time point
| Characteristic | Baseline N = 37 |
Control follow-up N = 31 |
Intervention follow-up N = 27 |
|---|---|---|---|
| Age (years) | 47.5 (11.8) | 47.8 (11.6) | 48.7 (11.8) |
| Household income (%) | |||
| < $20k | 25.6 | 21.3 | 24.1 |
| $20–$39k | 38.4 | 36.4 | 34.5 |
| $40–$59k | 23.1 | 27.3 | 24.1 |
| $60–$79k | 2.6 | 3 | 3.4 |
| $80k + | 10.3 | 12.1 | 13.8 |
| Highest grade completed (%) | |||
| High school | 84.6 | 81.8 | 79.3 |
| College | 7.7 | 9.1 | 10.3 |
| Graduate | 7.7 | 9.1 | 10.3 |
| Self-reported health status (%) | |||
| Excellent | 5.1 | 6.1 | 3.4 |
| Very Good | 25.6 | 30.3 | 31 |
| Good | 61.5 | 57.6 | 58.6 |
| Fair | 7.7 | 6.1 | 6.9 |
Mean values for study related outcomes and other health indicators are shown in table 3. Baseline BMI indicated obese, stage II category, being > 35 kg/m2. There was a preponderance of central adiposity with the mean waist circumference being significantly greater than the risk cutoff of 88 cm. An increased risk of cardiometabolic disease is suggested by the higher than optimal systolic blood pressure and elevated mean fasting blood glucose and insulin. Baseline body weight also appeared to have an impact on quality of life as suggested by the total score from the IWQOL.
Table 3.
Mean values for study participants at each study visit
| Outcome | Baseline (N = 37) Mean (SE) |
Control follow up (N = 31) |
Intervention follow up (N = 27) |
|---|---|---|---|
| Weight (kg) | 97.9 (2.5) | 98.5 (2.8) | 94.8 (3.0) |
| BMI (kg/m2) | 36.4 (0.9) | 36.7 (1.1) | 35.4 (1.2) |
| Waist circumference (cm) | 111 (2.2) | 111.5 (2.4) | 107.8 (3.1) |
| Systolic blood pressure (mm/Hg) | 125.9 (3.4) | 121.7 (3.2) | 124.6 (3.8) |
| Diastolic blood pressure (mm/Hg) | 75.1 (2) | 73 (1.9) | 78.8 (2) |
| Fasting blood glucose (mg/dL) | 121.9 (8.2) | 123.5 (9.4) | 127.3 (12.4) |
| Fasting insulin (uU/dL) | 20 (2.2) | 19.8 (1.8) | 19.7 (2) |
| Total cholesterol (mg/dL) | 201.8 (5.9) | 183.1 (6.3) | 187.1 (7) |
| Quality of life (Total score) | 77.0 (17.9) | 78.2 (17.6) | 84.9 (14.4) |
The changes for the primary and secondary outcomes for this study are shown in table 4 and figure 1. During the intervention period, approximately 30% of the study sample lost at least 5% of their starting body weight (Figure 1). On average, those losing at least 5% of their body weight had a net weight loss of 9.1 ± 3.4 kg (p<0.01). A total of 74% of the sample lost weight or maintained their weight during the intervention. This is compared to 45% of the sample that gained weight during the control period. As shown in table 4, during the control period average body weight increased but subsequently decreased during the intervention. The difference in mean weight change for the two periods was more than a 3 kg weight loss in favor of the weight loss intervention. The net change in waist circumference was a decrease of more than 3 cm. Mean weight loss was directly correlated with change in waist circumference (r = 0.78, p = 0.001). There was a non-significant increase in weight related quality of life during the control period (p = 0.36). Following the intervention period, participants reported a 7.3% net increase in weight related quality of life (Figure 2). The improvement in weight related quality of life was inversely associated with changes in body weight, such that decreases in body weight were associated with larger increases in quality of life; however, this association was not statistically significant (r = -.25, p = 0.27).
Table 4.
Changes in body weight, waist circumference, and quality of life
| Outcome | Control: Change from baseline Mean (SE) |
Intervention: Change from crossover |
Net difference (end of intervention – control) |
P value for net difference |
|---|---|---|---|---|
| Weight (kg) | .7 (0.3) | −2.6 (.8) | −3.4 (.8) | <0.001 |
| Waist circumference (cm) | 0.6 (0.9) | −3.0 (0.9) | −3.6 (1.3) | 0.006 |
| Quality of life (total score) | 2.1 (2.3) | 7.9 (2.5) | 5.7 (3.4) | 0.03 |
Figure 1.
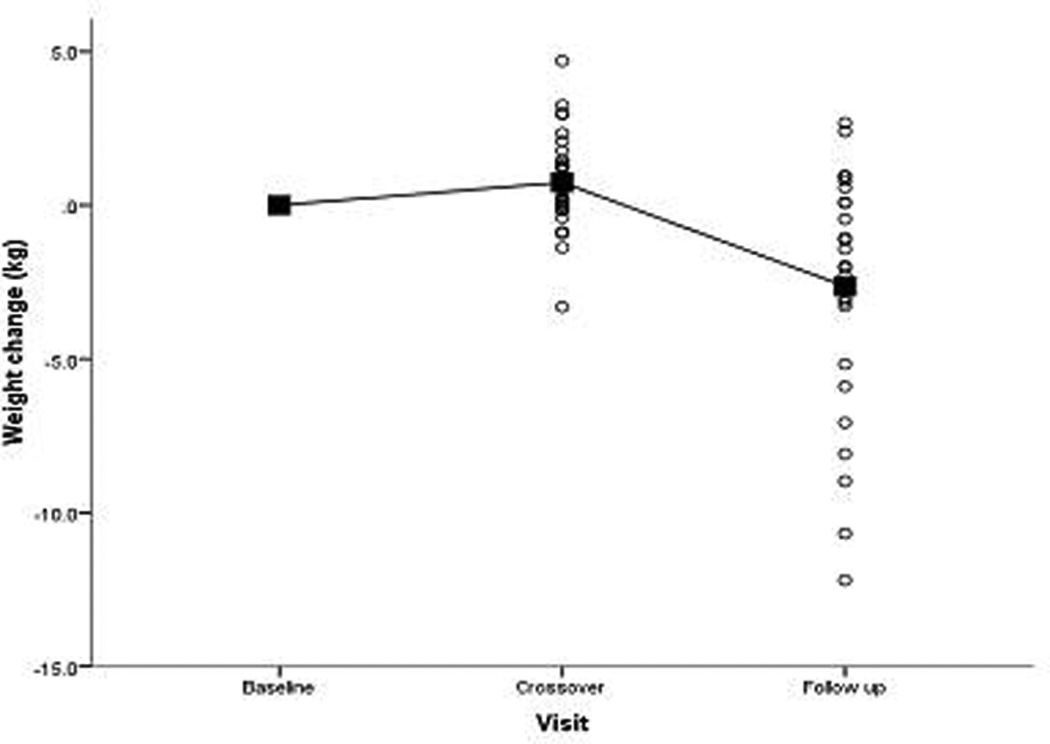
Change in weight over time
Figure 2.
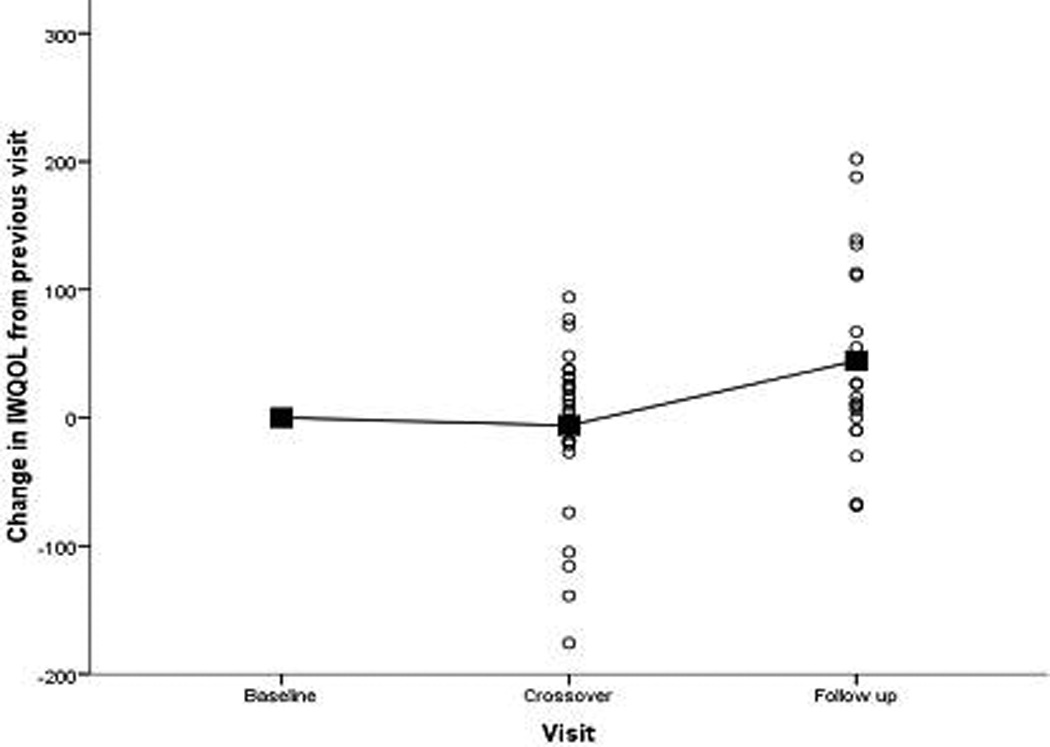
Change in quality of life over time
Discussion
In this pilot study of a culturally enhanced EatRight dietary intervention in a predominately African American workplace, we observed a significant weight loss, decrease in waist circumference, and improved quality of life. The net weight change of −3.4 kg was equal to a 3% weight loss; nearly a third of the participants lost at least 5% of their body weight during the course of the intervention. Changes in body weight were accompanied by reductions in central adiposity, measured by decreases in waist circumference. Improvements in quality of life suggest that changes in body weight or waist circumference were not the only indications of intervention success. Quality of life change was not statistically correlated with change in body weight or waist circumference, suggesting that participants obtained benefit from the intervention, to some extent, independent of the weight loss achieved.
This is the only study of which we are aware that utilizes a workplace setting to deliver a culturally enhanced behavioral intervention for weight reduction targeted to African American women. We used two specific strategies to increase the “accessibility” of the intervention to the target audience: making the intervention available via the workplace and cultural tailoring. This led to a unique behavioral intervention that directly addressed some of the challenges for African American women seeking to lose weight. It was apparent that many of the challenges faced by the participants were interactions of both culture and the workplace environment. For example, stress management skills had definite applicability at work, particularly when normal responses to stress may have included eating culturally associated comfort foods. In other instances, the workplace environment was utilized to provide adjuncts to intervention components that might not otherwise be available for African American women engaged in a weight loss program. On several occasions, we observed spontaneous demonstrations of group support, unprompted group exercise sessions, and healthier food alternatives in common areas which we believe were by-products of engaging a group of employees within the same workforce. This type of support may be particularly important for African American women who may not find this level of support for weight loss behaviors from family members or social networks (21, 22). The workplace also offers the advantage of providing multiple opportunities for engagement due to the amount of time spent at work. A supportive environment and key messages can be persistent in the workplace, providing sustained “dosing,” whereas traditionally, interventions delivered in other settings require active attendance to the designated location to receive intervention messages. On the other hand, while the workplace may be an attractive target for weight control interventions, it can also compete for participant’s time, paradoxically having a negative impact on factors such as attendance at group meetings. As an example, the mean number of intervention sessions attended per participant for those choosing to attend group sessions during work hours was lower than those attending sessions after work hours.
As compared to other attempts to target African American women in other settings, this intervention demonstrated comparable results (23). Churches or religious communities have been a frequent venue for delivering interventions for weight reduction targeted to African American women. In one of the more effective interventions, McNabb et al delivered a 14 week, church-based intervention resulting in 4.5 kg of weight loss (24). University or clinic based studies have also been reported. The Pounds Off With Empowerment trial (POWER) targeted a mostly rural African American population with type 2 diabetes mellitus and demonstrated a weight loss of 2.6 kg at 6 months in a primary health care center setting (25). Fitzgibbon et al reported a 12 week weight loss of 2.6 kg in a group of African American women participating in a faith-based weight loss intervention in a university setting (26). In the Obesity Reduction Black Intervention Trial (ORBIT), Stolley et al reported a 3 kg weight loss at 6 months and 26% of participants with 5% or greater weight loss (27). We observed a similar magnitude of weight loss with this workplace intervention, with a substantial proportion reaching 5% weight loss which is considered medically significant. Of equal importance, we observed a significant reversal in the trend of weight gain that occurred during the pre-intervention observation period, where nearly half of the study sample experienced weight gain. The mean increase in weight is consistent with weight gains observed in some other studies such as Pound of Prevention (control group gained 1.9 lb in 12 months; 28). At a minimum, prevention of weight gain in a high risk population would be a desirable outcome for a workplace intervention.
Our study falls within the framework of the research priorities delineated by the African American Collaborative Obesity Research Network (29). Deploying targeted interventions in the workplace setting has the potential to encompass several domains that may directly or indirectly affect adoption of key health behaviors. Environmental and policy changes can be easily incorporated into this type of setting. Additionally, social dynamics and interactions within the workforce can be garnered to benefit the implementation of the intervention. Having these domains intrinsically embedded within the workplace setting may offer some advantages beyond the traditional behavioral intervention model. In these instances, the group intervention setting is used to generate support (30), or more recently, the use of the internet has been employed to extend such support beyond the immediate group meetings (31). However, there may be limitations to the sustainability of the group effect because the environment otherwise does not support the behavioral changes. The workplace environment may provide a suitable setting to overcome this specific limitation by shifting a portion of the responsibility for engaging in healthy behaviors from the individual level to the organizational level (32).
Several factors limit our results and the conclusions that we may draw from these results. By virtue of the fact that we were unable to limit the study population in any way, we recruited a diverse study sample, including some who were underweight or had intentions of using medications to help promote weight loss. We were also limited in the study design to some extent because of the need to provide everyone with a chance to participate in the study intervention. Future studies will need to include randomized, controlled designs with larger samples and longer follow up. Lastly, because a substantial proportion of the sample was on medication for an associated co-morbid condition (27%), there may have been concurrent intervention provided by another entity, such as a health care provider, focused on the goal of reducing health risk. While this co-intervention might be ideal in a “real world” setting, the actual frequency of this occurrence and its impact on the outcome cannot be determined in this study.
This study demonstrated the feasibility of delivering a culturally enhanced behavioral intervention in a workplace setting that employs primarily African American women. Using a formative assessment, we tailored the principles of the UAB EatRight Lifestyle program for this setting and population. The program resulted in significant weight loss and improvements in quality of life. Our results suggest that using a dietary intervention focused on consumption of low energy dense foods in a workplace setting offers a unique opportunity to target high risk populations such as African American women and begin to efficiently reduce disparities in obesity.
References
- 1.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 2.Pronk NP, Martinson B, Kessler RC, Beck AL, Simon GE, Wang P. The Association Between Work Performance and Physical Activity, Cardiorespiratory Fitness, and Obesity. Journal of Occupational and Environmental Medicine. 2004;46(1):19–25. doi: 10.1097/01.jom.0000105910.69449.b7. [DOI] [PubMed] [Google Scholar]
- 3.Tucker LA, Friedman GM. Obesity and absenteeism: an epidemiologic study of 10,825 employed adults. Am J Health Promot. 1998;12(3):202–207. doi: 10.4278/0890-1171-12.3.202. [DOI] [PubMed] [Google Scholar]
- 4.Finkelstein E, Fiebelkorn IC, Wang G. The Costs of Obesity Among Full-time Employees. American Journal of Health Promotion. 2005;20(1):45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 5.Chapman LS. Meta-Evaluation of Worksite Health Promotion Economic Return Studies. American Journal of Health Promotion. 2003;17(3):1–10. doi: 10.4278/0890-1171-19.4.TAHP-1. [DOI] [PubMed] [Google Scholar]
- 6.Griffin-Blake CS, DeJoy DM. Evaluation of Social-cognitive Versus Stage-matched, Self-help Physical Activity Interventions at the Workplace. American Journal of Health Promotion. 20(3):200–209. doi: 10.4278/0890-1171-20.3.200. [DOI] [PubMed] [Google Scholar]
- 7.Office of Research Information and Planning. WOMEN OF COLOR: THEIR EMPLOYMENT IN THE PRIVATE SECTOR. U.S. Equal Employment Opportunity Commission. 2003. [Google Scholar]
- 8.Rolls BJ, Bell EA, Castellanos VH, Chow M, Pelkman CL, Thorwart ML. Energy density but not fat content of foods affected energy intake in lean and obese women. American Journal of Clinical Nutrition. 69(5):863–871. doi: 10.1093/ajcn/69.5.863. [DOI] [PubMed] [Google Scholar]
- 9.Rolls BJ, Drewnowski A, Ledikwe JH. Changing the Energy Density of the Diet as a Strategy for Weight Management. Journal of the American Dietetic Association. 105(5 Suppl 1):S98–S103. doi: 10.1016/j.jada.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 10.Weinsier RL, Bacon JA, Birch R. Time-calorie displacement diet for weight control: a prospective evaluation of its adequacy for maintaining normal nutritional status. Int J Obes. 1983;7(6):539–548. [PubMed] [Google Scholar]
- 11.Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007;85(6):1465–1477. doi: 10.1093/ajcn/85.6.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ledikwe JH, Rolls BJ, Smiciklas-Wright H, et al. Reductions in dietary energy density are associated with weight loss in overweight and obese participants in the PREMIER trial. Am J Clin Nutr. 2007;85(5):1212–1221. doi: 10.1093/ajcn/85.5.1212. [DOI] [PubMed] [Google Scholar]
- 13.Greene LF, Malpede CZ, Henson CS, Hubbert KA, Heimburger DC, Ard JD. Weight Maintenance 2 Years after Participation in a Weight Loss Program Promoting Low-Energy Density Foods. Obesity. 2006;14(10):1795–1801. doi: 10.1038/oby.2006.207. [DOI] [PubMed] [Google Scholar]
- 14.Duncan KH, Bacon JA, Weinsier RL. The effects of high and low energy density diets on satiety, energy intake, and eating time of obese and nonobese subjects. Am J Clin Nutr. 1983;37(5):763–767. doi: 10.1093/ajcn/37.5.763. [DOI] [PubMed] [Google Scholar]
- 15.Weinsier RL, Johnston MH, Doleys DM, Bacon JA. Dietary management of obesity: evaluation of the time-energy displacement diet in terms of its efficacy and nutritional adequacy for long-term weight control. Br J Nutr. 1982;47(3):367–379. doi: 10.1079/bjn19820048. [DOI] [PubMed] [Google Scholar]
- 16.Ard JD, Carter-Edwards L, Svetkey LP. A new model for developing and executing culturally appropriate behavior modification clinical trials for African Americans. Ethn Dis. 2003;13(2):279–285. [PubMed] [Google Scholar]
- 17.Ard JD, Durant RW, Edwards LC, Svetkey LP. Perceptions of African-American culture and implications for clinical trial design. Ethn Dis. 2005;15(2):292–299. [PubMed] [Google Scholar]
- 18.Zunker C, Cox TL, Wingo BC, Knight BN, Jefferson WK, Ard JD. Using Formative Research to Develop a Worksite Health Promotion Program for African American Women. Women & Health. 2008;48(2):189–207. doi: 10.1080/03630240802313514. [DOI] [PubMed] [Google Scholar]
- 19.Elliott TR, Shewchuk RM. Using the nominal group technique to identify the problems experienced by persons living with severe physical disabilities. Journal of Clinical Psych in Medical Settings. 2002;9(2):65–76. [Google Scholar]
- 20.Kolotkin RL, Head S, Hamilton M, Tse CK. Assessing Impact of Weight on Quality of Life. Obesity Res. 1995;3(1):49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 21.Malpede CZ, Greene LE, Fitzpatrick SL, et al. Racial influences associated with weight-related beliefs in African American and Caucasian women. Ethn Dis. 2007;17(1):1–5. [PubMed] [Google Scholar]
- 22.Barnes AS, Goodrick GK, Pavlik V, Markesino J, Laws DY, Taylor WC. Weight loss maintenance in African-American women: focus group results and questionnaire development. J Gen Intern Med. 2007;22(7):915–922. doi: 10.1007/s11606-007-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bronner Y, Boyington JE. Developing weight loss interventions for African-American women: elements of successful models. J Natl Med Assoc. 2002;94(4):224–235. [PMC free article] [PubMed] [Google Scholar]
- 24.McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care. 1997;20(10):1518–1523. doi: 10.2337/diacare.20.10.1518. [DOI] [PubMed] [Google Scholar]
- 25.Mayer-Davis EJ, D'Antonio AM, Smith SM, et al. Pounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am J Public Health. 2004;94(10):1736–1742. doi: 10.2105/ajph.94.10.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97(10):1393–1402. [PMC free article] [PubMed] [Google Scholar]
- 27.Stolley MR, Fitzgibbon ML, Schiffer L, et al. Obesity reduction black intervention trial (ORBIT): six-month results. Obesity (Silver Spring) 2009;17(1):100–106. doi: 10.1038/oby.2008.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeffery RW, French SA. Preventing weight gain in adults: design, methods and one year results from the Pound of Prevention study. Int J Obes Relat Metab Disord. 1997;21(6):457–464. doi: 10.1038/sj.ijo.0800431. [DOI] [PubMed] [Google Scholar]
- 29.Kumanyika SK, Gary TL, Lancaster KJ, et al. Achieving Healthy Weight in African-American Communities: Research Perspectives and Priorities. Obesity Res. 2005;13(12):2037–2047. doi: 10.1038/oby.2005.251. [DOI] [PubMed] [Google Scholar]
- 30.West DS, Prewitt TE, Bursac Z, Felix HC. Weight Loss of Black, White, and Hispanic Men and Women in the Diabetes Prevention Program. Obesity. 2008;16(6):1413. doi: 10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- 31.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 32.Yancey AK, Lewis LB, Sloan DC, et al. Leading by example: a local health department-community collaboration to incorporate physical activity into organizational practice. J Public Health Management and Practice. 2004;10(2):116–123. doi: 10.1097/00124784-200403000-00005. [DOI] [PubMed] [Google Scholar]


