Abstract
Women with co-occurring mental health and substance use disorders and trauma histories vary greatly in symptom severity and use of support services. This study estimated differential effects of an integrated treatment intervention (IT) across sub-groups of women in this population on services utilization outcomes. Data from a national study were used to cluster participants by symptoms and service utilization, and then estimate the effect of IT versus usual care on 12-month service utilization for each sub-group. The intervention effect varied significantly across groups, in particular indicating relative increases in residential treatment utilization associated with IT among women with predominating trauma and substance abuse symptoms. Understanding how IT influences service utilization for different groups of women in this population with complex needs is an important step toward achieving an optimal balance between need for treatment and service utilization, which can ultimately improve outcomes and conserve resources.
Keywords: Co-occurring disorders, PTSD, Integrated treatment, Interventions, Service utilization
Seven to 10 million people in the United States suffer from at least one mental health or substance use disorder (SAMHSA 2002). Women in this population are much more likely than men to also have histories of and be vulnerable to traumatic life events, such as physical or sexual abuse (Gearon et al. 2003; Goodman et al. 1997; Hanson et al. 2002; Watkins et al. 2001).
Reports of lifetime interpersonal violence—often physical and/or sexual abuse—are particularly common among women with substance use disorders and women with mental health disorders, ranging from 40% to nearly 100% (Alexander 1996; Fullilove et al. 1993), and often doubling the reported prevalence of violence among more population-based samples (Najavits et al. 1997). Women suffering from co-occurring mental health and substance use disorders are even more likely to have histories of abuse victimization and patterns of revictimization than women experiencing a single disorder, and are also at particularly high risk for ongoing or future abuse (Alexander 1996; Gearon et al. 2003; Goodman et al. 2001; Mueser et al. 1998).
Evidence suggests that people with co-occurring disorders often do not receive the specialty services that they need (Becker et al. 2005; Clark et al. 2007; Drake et al. 2004; Dickey and Azeni 1996; Harris and Edlund 2005; Kessler et al. 1997; Watkins et al. 2001). Further, there is substantial evidence that usual care for treating co-occurring disorders is often fragmented, uncoordinated, and not comprehensive, characteristics which are associated with gaps in availability and use of services, as well as suboptimal improvements in consumer outcomes (SAMHSA 2002).
A growing body of evidence suggests that an integrated approach to treatment may be associated with better outcomes than traditional, uncoordinated services among women with co-occurring mental health and substance use disorders who also have histories of abuse victimization (SAMHSA 2002; Najavits et al. 1998; NASMHPD & NASADAD 1998). A review of treatment services for co-occurring disorders suggested that integrated treatment is associated with a lower risk of dropping out of treatment and non-adherence to interventions as compared to treatment that is delivered in parallel, but separate service systems (Drake et al. 2004). Integrated treatment was also associated with less confusion among service recipients due to potentially conflicting messages about treatment and recovery being conveyed, respectively, by the mental health and substance abuse services systems (Drake et al. 2004). Women in this population receiving care from providers who are trained in working with trauma survivors and who take incremental steps in treating their co-occurring disorders and trauma symptoms may respond more positively and, in turn, have more marked improvements in their outcomes (Harris 1994).
This enhanced approach to treatment—integrated, coordinated, and trauma-informed counseling and other services—was studied in the Women, Co-occurring Disorder and Violence Study (WCDVS) from 1998–2003. Early evaluations of WCDVS demonstrated promising results for 6- and 12-month clinical outcomes associated with integrated treatment (IT) as compared to usual care. A meta-analysis of program-level effects at the 6-month follow-up indicated that intervention sites showed more improvement in mental health and substance abuse outcomes than comparison sites (Cocozza et al. 2005). Hierarchical linear models of program- and individual-level effects of IT demonstrated that participants at intervention sites showed greater improvement in mental health, substance abuse, and post-traumatic stress symptoms at 6 months as compared to participants at comparison sites, even when controlling for the effect of most individual-level characteristics (Morrissey et al. 2005a). Average improvements in mental health and PTSD outcomes among women at intervention sites continued to increase through the 12-month follow-up, while the substance abuse outcomes leveled off, maintaining 6-month improvements (Morrissey et al. 2005b).
Two analyses estimated follow-up health service use and total associated costs among WCDVS participants (Domino et al. 2005a, b). Analyses of six- and 12-month service outcomes both indicated no statistically significant difference in total average costs between the group of participants receiving IT and the group receiving usual care. On average, participants in the IT group used more outpatient group counseling than participants in the usual care group at 6-month follow-up (Domino et al. 2006).
While evidence for the average effects of IT was encouraging, it did not indicate whether IT was associated with different outcomes for different types of women in the target population. Cusack et al. (2008) evaluated the WCDVS data to determine whether the intervention affected clinical outcomes differentially across sub-groups of women according to symptom severity. The investigators used k-means cluster analysis to organize women into sub-groups according to their baseline PTSD and substance abuse severity, and then predicted frequency of lifetime traumatic events, age at onset of mental health problems and poor physical health, and response to the WCDVS intervention. Women in clusters with severe co-morbidity and severe PTSD, respectively, had the greatest number of traumatic events throughout their lifetimes. Onset of mental health disorders was earliest among women whose predominant symptom was severe PTSD and among women who suffered from severe PTSD and severe drug and alcohol problems. Poor physical health ratings were worst for those clusters of women as well. Furthermore, Cusack et al. (2008) estimated that women with severe PTSD and substance abuse symptoms, and who were in IT versus usual care, had the greatest improvements in their post-traumatic stress symptoms.
What's unclear from this earlier work is whether a woman's symptomatology or pattern of service use prior to the IT intervention moderated her service use efficiency. The study intervention was designed to treat women's disorders and trauma symptoms, so it may be that differences in the effect of the intervention on service utilization depended on baseline symptom severity. Existing empirical evidence supports the expectation that different populations of people with co-occurring disorders use certain services differently depending on the severity of their psychiatric and substance abuse symptoms (McGovern et al. 2007; Cusack et al. 2008; Keyser et al. 2008).
On the other hand, services utilization theories—in particular, the Behavioral Model of Health Services Use (Andersen 1995) and the Pathways to Care in the Community model for mental health services use (Goldberg and Huxley 1980)—suggest that factors other than symptoms (e.g., predisposing characteristics, enabling resources) also drive people to seek, access, and engage in services differently. Services utilization behaviors before IT—independent of symptom severity—may have been what most strongly moderated the effect of IT on service utilization outcomes.
This study was driven by a hypothesis that there were significant empirical differences in the effect of IT on service utilization outcomes according to baseline symptom severity and according to baseline service use patterns among women with co-occurring disorders and histories of abuse. Furthermore, based on empirical evidence that many people with co-occurring disorders often underutilize needed targeted services even though their need for care is high, we expected that service use patterns prior to study participation would have stronger moderating effects on the relationship between the intervention and service use outcomes than would symptomatology.
This study adds new evidence about heterogeneous effects of IT on service utilization for two common treatment modalities used by this population—outpatient counseling, which was the primary service indicated in the WCDVS intervention, and residential substance abuse treatment, another common, more intensive, mode of treatment. Existing evidence suggests that this IT intervention improved clinical outcomes for women in this study population, more for some women than others depending on their symptom profiles (Cusack et al. 2008). How the intervention changed service utilization and efficiency for different sub-groups of women was examined in this study, adding to a more comprehensive picture of its effectiveness. The findings of this study will provide more information about who responded well to the intervention, which can then be used to improve how and to whom this type of treatment should be directed in the community. This new knowledge is particularly relevant in the context of treatment services that are often provided in public service systems with highly constrained resources.
Methods
WCDVS Design
From 1998 through 2003, the WCDVS implemented a quasi-experimental treatment protocol to serve the complex needs of women with co-occurring disorders and histories of abuse victimization (McHugo et al. 2005; Cocozza et al. 2005; Morrissey et al. 2005a, b). Nine intervention sites with varied program and treatment modalities implemented integrated intervention programs. Four core requirements for the content of the interventions were: (1) to provide comprehensive intervention services with eight specific service elements, including outreach and engagement, parenting skills training, resource coordination and advocacy, and crisis intervention; (2) to implement a set of services that were integrated, both clinically and organizationally (i.e., a site needed to be coordinated with other agencies and individual providers participating in the care of study participants); (3) to provide services that were trauma-informed, so that potential circumstances and symptoms specific to having been a victim of abuse were to be acknowledged and addressed in the intervention services; and, (4) to incorporate CSR involvement into their intervention services. Specifically, [C]onsumers of mental health services, [S]urvivors of trauma, and women in [R]ecovery (CSR) were to be included in the development, implementation, and evaluation of each site's intervention services (McHugo et al. 2005).
Each of the nine study sites contributed an intervention program and a comparison program that provided usual care in the same or an adjacent community. Women were enrolled in a quasi-experimental or non-random manner into both programs and followed for 12 months. Within that interval, no minimum or maximum number or duration of intervention services was prescribed. Service use thus reflected real-life treatment engagement patterns where, for a variety of reasons, some women continue service use for extended periods while others disengage shortly after initiating. Those variations were captured in the study data.
WCDVS Participants
The study sample at baseline included 2,729 eligible women. Overall, these women had complex combinations of mental and physical health problems, trauma histories, and other, complicating life circumstances (Becker et al. 2005). At baseline, participants were, on average, high-intensity users of addiction treatment, and over half were living in residential substance abuse treatment facilities (Becker et al. 2005). Trauma experiences among participants were commonly severe, the majority reporting having been victims of physical abuse, sexual abuse, emotional abuse, neglect, and often, some combination those. Complicating their disorders and trauma symptoms, many women in this population reported having poor physical health status—nearly half reported a current serious health problem, and only 22% considered their current health to be excellent or good (Larson et al. 2005).
Along with a constellation of health problems and abuse victimization, many WCDVS participants faced other life circumstances that put them at a general disadvantage and likely made treatment and recovery more challenging. The majority was under-educated and under-employed; nearly half did not finish high school, and only 12% reported working either full- or part-time (Becker et al. 2005). Twenty percent of participants reported being in jail or a correctional facility during the 3 months prior to enrolling in WCDVS. Many of the women were unstable parents; of the 87% who had children, 40% had lost custody of their children.
Measures
Outcome Variables
Participants' use of treatment services was assessed at baseline, and at three-, six-, nine-, and 12-month follow-ups. Outpatient counseling (group and individual) and residential treatment were selected as outcome variables, as they reflect two important modalities of treatment for substance abuse and mental health disorders. In particular, outpatient counseling was a fundamental component of IT and considered to be a key service associated with improving outcomes among women in this population. Residential substance abuse treatment, on the other hand, is a clinically- and resource-intensive approach that is commonly used for treating people with severe addictions and co-occurring disorders (Greenfield et al. 2004; Chen et al. 2006).
Outpatient counseling and residential treatment use were measured as cumulative, aggregated counts of counseling visits and days in residential treatment, respectively, across the waves of follow-up and through 12 months. The interview instrument asked participants to report on service use in the last 3 months or since last interview, so service use among participants with any missing intermediate interviews was calculated for that interim period.
Clustering Variables: Baseline Symptom Severity
Several well-validated, widely used survey instruments were employed in WCDVS to measure women's disorder-related symptoms. These instruments were used for the baseline symptom severity clustering in this study and in prior research (Cusack et al. 2008). Mental health symptoms were measured using the Global Severity Index (GSI) from the Brief Symptom Inventory (Derogatis 1993), a well-validated survey instrument for assessing mental health status, functioning, and symptoms. The GSI consists of 53-items with response categories ranging from 0–4 to reflect increasing symptom severity in the past 7 days.
Post-traumatic stress symptoms in WCDVS participants were measured using the Posttraumatic Stress Diagnostic Scale, which assesses 17 key symptoms associated with the experience of PTSD, with response categories ranging from 0–3 to reflect increasing severity. Established cut, points exist to categorize PTSD symptom severity, so that Mild = 1–10, Moderate = 11–20, Moderate-Severe = 21–35, and Severe = 36–51 (Foa 1995; Foa et al. 1997).
Substance abuse behavior was measured using the Addiction Severity Index (ASI), a self-report of substance use and perceived problem seriousness in the past 30 days (McLellan et al. 1992). The ASI includes two composite scores-ranging from 0–1 as severity increases—one each for alcohol (ASI-A) and drugs (ASI-D). Normative cut-points do not exist for the ASI, and scores have been demonstrated to vary significantly by study population (McLellan et al. 1996). Therefore, we used the baseline mean values in this study population as a cut-point to distinguish between high and low addiction severity for for the alcohol and drug measures.
In the current sample, the GSI was highly correlated with the PTSD measure (r = 0.7687, P < 0.0001). PSTD was chosen to represent general mental health symptoms over GSI in the cluster grouping for two reasons. First, PTSD was a distinguishing characteristic that made this intervention unique from other interventions that deliver integrated treatment for co-occurring disorders where abuse victimization and consequent PTSD are not specifically addressed. Therefore, given that it was highly correlated with GSI, and because PTSD was a defining characteristic of interest in the intervention, it was selected for defining sub-groups by symptoms at baseline. Second, the sub-group analysis of clinical outcomes by Cusack et al. (2008) also used PTSD as the mental health clustering measure, thereby increasing the comparability of our results with theirs. Sixty-six observations had missing values for PTSD scores. The GSI scores were regressed on PTSD scores using participants with non-missing observations for both variables (R2 = 0.58), and the predicted values were calculated and imputed for the 66 missing values. Sensitivity tests showed that the results were consistent between the imputed and listwise-deleted samples.
Clustering Variables: Baseline Service Use
A second set of clusters was constructed to categorize WCDVS participants according to baseline service use patterns. Service utilization theory (Andersen 1995; Goldberg and Huxley 1980) suggests that factors other than symptoms (e.g., predisposing characteristics, enabling resources) drive people to seek, access, and engage in services use differently. Service utilization behaviors prior to the receipt of IT, therefore, may have been what most strongly influenced engagement in IT and its consequent effect on service use outcomes. Clustering women according to their service behavior prior to the intervention—regardless of symptomatology—allowed us to measure that particular moderating effect. Four main service use and cost dimensions were examined: (1) outpatient individual and group counseling, (2) residential treatment use, (3) psychotropic medication costs, and (4) external medical costs. These four dimensions reflect a broad scope of services—psychiatric, psychotherapeutic, substance abuse rehabilitation, and medical care—that study participants reported using. Cost inputs were used for the medical-related services as a natural measure of intensity of use, capturing important variation for medical services/treatment that is not reflected as well in simple counts of utilization.
The two baseline service utilization measures were derived directly from the study interview data. Outpatient counseling use was measured as participants' self-reported frequency of individual or group counseling visits in the 3 months prior to study entry. Residential treatment use was measured as participants' self-reported number of days spent in a residential treatment facility in the 3 months prior to study entry.
The two service cost measures were modeled directly after cost estimation for this study population in analyses by Domino et al. (2005a, b). As exact medication and dosing information was not available in these study data, costs for participant-reported psychotropic medications were calculated using cost data from the 2000 Medical Expenditure Panel Survey (MEPS 2000) for a typical, female psychotropic medication user with either a psychiatric or substance abuse indication, and assuming a 30-day prescription. External medical costs comprised costs associated with inpatient hospitalizations, emergency department (ED) visits, and outpatient medical visits. Cost per day in psychiatric and general medical hospitals were based on 1999 Medicare cost reports; the cost for an ED visit was based on MEPS 2000 data, calculated for the cost for adult women with Medicare or private insurance coverage; and outpatient medical visit costs were based on Medicare allowable costs. All costs reflected variations by state, region, or city of the study site as available in the source data.
Control Variables
A set of relevant covariates was included in the analyses. Age, race, education, and having a serious physical illness or disability were controlled for as predisposing factors for service utilization. The following disabling factors were included as dichotomous control dummy variables: participant reporting currently being a victim of physical or emotional abuse (within past 6 months), participant feeling unsafe with someone she knows well, or participant feeling afraid of someone with whom she lives or who lives nearby. Dummy variables were constructed to indicate whether participants had health insurance (public or private) and whether they were court-ordered to participate in treatment, both considered enabling factors for service utilization. Having a perceived unmet need for care was also included as a control dummy variable, indicated by participants' self-reports of having felt they needed services but hadn't received in the past 3 months for at least one service type—ranging from mental health, substance abuse, or trauma services, to case management services or medical services.
A small number of observations were dropped due to missing data on race (n = 1), education (n = 3), court-ordered treatment (n = 3), and perceived need for care (n = 19), yielding an analysis sample of 2,001 individuals.
Clustering Methodology
A combination of hierarchical and k-means clustering methods were used to organize study participants at baseline into distinct sub-groups on two sets of baseline dimensions—symptom severity and service use/costs. An advantage of a clustering approach is that, by definition, categories are no longer symmetrical as in the Four Quadrant model that dichotomizes and cross-classifies mental health and substance abuse symptom severity into low–low, low–high, high-low, and high–high categories (McGovern et al. 2007; Larkin 2007). Instead participants are partitioned into groups by algorithms that cluster individuals who are most alike on the dimensions of interest. For this study, the number of clusters and their starting centroids were first obtained using an agglomerative, hierarchical method in which single observations are progressively grouped into larger clusters of like observations; and second, the clustering solution was then improved by optimizing assignment of observations to clusters iteratively using k-means clustering (Khattree and Naik 1999; Milligan and Cooper 1985). The full baseline sample of participants was used to generate the clusters versus the 12-month sample to maximize the precision of the clustering results.
Variation in the value ranges of input variables was large (Table 1). To avoid more relative influence being placed on variables with large ranges during cluster assignment, but also to retain natural variability in the data, input variables for both the symptom and services clustering were first rescaled to generate potential ranges of 0–100 for all input variables. This approach placed input variables on a common scale while leaving relative variability before and after transformation unchanged, and performed best in recovering the underlying structure of the cluster as compared to other approaches in analyses by Milligan and Cooper (1988). As a sensitivity analysis, we next ran both cluster analysis and the regression analyses for the service cluster constructs a second time with the revised data, this time dropping the four participants with outlying values for baseline external medical costs.
Table 1. Baseline mean values (SD) for clustering variables.
| Variable | Percent with any use | Rescaled values (0–100)a | Raw scale values | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Mean | SD | Mean | SD | Range | ||
| Addiction Severity Index—alcohol | 20.18 | 03.19 | 0.20 | 0.30 | 0–1 | |
| Addiction Severity Index—drugs | 16.90 | 15.59 | 0.17 | 0.16 | 0–0.70 | |
| Post-traumatic symptom scale | 46.17 | 22.89 | 23.94 | 11.77 | 0–51 | |
| Outpatient counseling visits | 60.94 | 11.63 | 17.36 | 15.12 | 22.57 | 0–130 |
| Residential treatment days | 54.42 | 19.97 | 28.86 | 18.57 | 26.84 | 0–93 |
| Psychotropic medication costs | 62.06 | 15.55 | 16.32 | $362 | $380 | $0-$2,324 |
| External medical costs | 75.26 | 3.39 | 7.77 | $2,953 | $6,769 | $0-$159,840 |
n = 2,729
Clustering input variables were rescaled to generate potential ranges of 0–100 by dividing each observed value by the maximum value observed in the sample for each respective variable and then multiplying by 100
In the first stage of the clustering analysis, the Ward's clustering algorithm, which attempts to minimize the sum of squared distances between observations within a cluster, was used to assign each observation as its own cluster and then continued to link individual clusters together to form larger clusters based on squared Euclidean distance (Milligan 1980). Dendrograms (i.e., tree diagrams) were generated from the results of the Ward's analyses and inspected to identify the best candidate cluster solutions. Greater vertical distance between a given cluster and the remaining clusters indicated more distinct groupings, and was used to identify optimal clustering. For the symptom severity construct, six- and seven-cluster solutions were identified to test for optimal clustering. For the four-variable service construct, four- and five-cluster solutions were selected.
In the second stage of the cluster analysis, centroids (i.e., mean values) from the final Ward's cluster solutions for the symptom and service constructs were used as starting seeds for k-means cluster analysis. K-means analysis is an iterative partitioning approach, assigning observations to clusters to minimize the within-cluster distances and maximize the distance between cluster centroids (Khattree and Naik 1999).
The final stage of the cluster analysis was to validate the selected cluster solutions. The stability of cluster solutions was assessed by (a) randomly dividing the study sample in two, (b) performing cluster analysis on sub-sample 1, (c) performing cluster analysis on sub-sample 2, and(d) performing cluster analysis on sub-sample 2 again, the second time using the final centroids generated from the analysis of sub-sample 1 as starting points. The stability of results between the two analyses of sub-sample 2 was assessed using Cohen's kappa statistic (Shrout 1998).
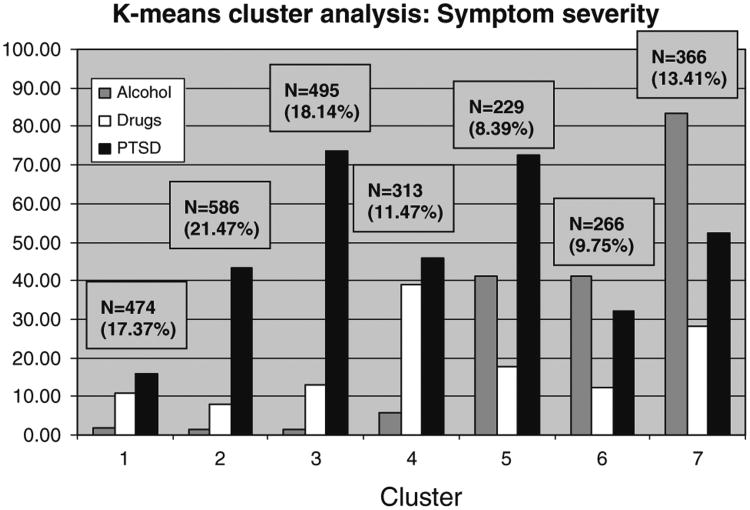
For the symptom clustering construct, the Cohen's kappa statistics suggested that the seven-cluster symptom grouping (Fig. 1) was more reliable than a six-cluster symptom grouping (seven-cluster solution: k = 0.70, P < 0.0001; six-cluster solution: k = 0.64, P < 0.0001). Approximately 17% of participants had relatively low symptoms on substance abuse and PTSD dimensions at baseline (C1-Sx). About 21% experienced moderate-severe PTSD, but low alcohol and drug addiction symptoms (C2-Sx). Nearly 18% of participating women had severe PTSD and low alcohol and drug addiction symptoms (C3-Sx), while 11% of women were characterized by high drug addiction and moderate-severe PTSD (C4-Sx). About 8.5% of women had high alcohol addiction and severe PTSD (C5-Sx), and another 10% of women had high alcohol addiction and moderate PTSD (C6-Sx). The remaining 13% of women (C7-Sx) were characterized by severe co-morbid symptoms for alcohol, drugs, and PTSD.
Fig. 1. Clusters by baseline symptom severity. C1 low symptoms, C2 moderate-severe PTSD, C3 severe PTSD, C4 drug/moderate-severe PTSD, C5 alcohol/Severe PTSD, C6 alcohol/moderate PTSD, C7 severe co-morbid.
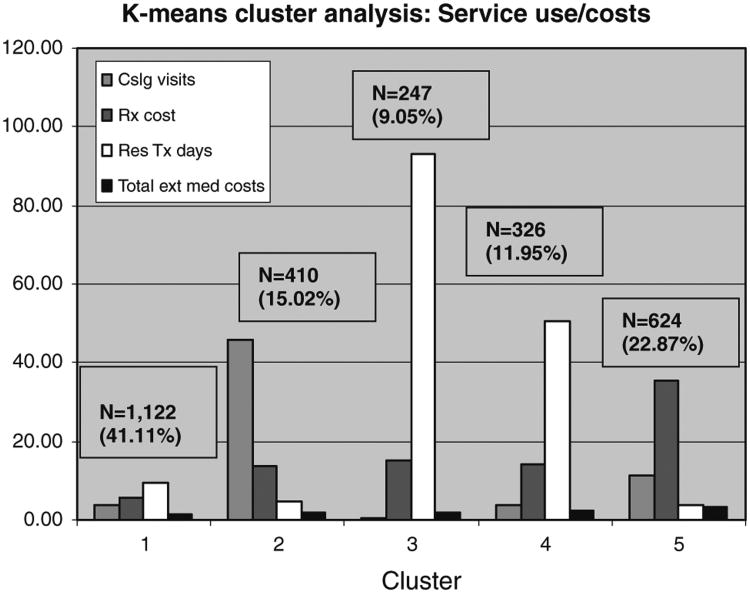
For the service clustering construct, the Cohen's kappa statistics for the four- and five-cluster solutions (k = 0.32, P < 0.0001 and k = 0.84, P < 0.0001, respectively) indicated that the five-cluster solution (Fig. 2) produced more stable results. Forty-one percent of participants had low usage for group or individual outpatient counseling and days in residential treatment, as well as low costs associated with psychotropic medication use and external medical services in the 3 months prior to baseline (C1-Serv). Approximately 15% reported using high levels of counseling and low use of residential treatment, with average costs for psychotropic medication and external medical services (C2-Serv). Approximately 9% of women in the study were characterized as being very high users of residential treatment, having spent most of the pre-baseline period in that setting (C3-Serv). Another 12% of participants were moderately high users of residential treatment, having spent an average of about half of the pre-baseline period in that setting (C4-Serv). Finally, almost 23% of participants had high costs for psychotropic medication and external medical services, along with average use of counseling and low use of residential treatment (C5-Serv).
Fig. 2. Clusters by baseline service use/costs. C1 low service use, C2 high counseling use, C3 high residential treatment use, C4 moderate residential treatment use, C5 high drug and medical costs.
The distribution of study participants in the final analytic sample across baseline symptom and service clusters comprised unique groups of women. Nearly half of the women in the low symptom cluster (C1-Sx) were also in the low service use cluster (C1-Serv), and conversely 21% of women who were in the low service use were also in the low-severity symptom cluster. Otherwise, the participants were distributed fairly evenly across symptom and service clusters, resulting in unique sub-groups of study participants across the two clustering constructs.
Selection Bias
Given that treatment assignment was not randomized and that there was some loss to follow-up at 6- and 12-month follow-ups, logistic regression analyses were estimated to test for selection and attrition biases among the study population. In the final analytic sample, African-American women were statistically significantly more likely to be in the intervention group than White women (OR = 1.653, P < 0.001). Women who were court-ordered to receive treatment for at least one of their disorders were also more likely to be in the intervention group than women who were not court-ordered to receive treatment (OR = 1.49, P < 0.001). Participants' remaining in the study at 12 months was associated with certain characteristics—being relatively young, less educated, or African-American was associated with increased odds of dropping out, as was relatively severe PTSD and drug addiction scores. There was no statistically significant difference in study attrition by 12 months for women in the intervention group versus the usual care group (OR = 1.20, P = 0.077).
Analytic Methods
Dependent variables reflecting days or visits were analyzed using count data models. Vuong and other specification tests indicated that the zero-inflated negative binomial model, which models the proportion of observations with zero counts separately from the level of use, were preferred for all models over Poisson models. The same set of covariates was used for both parts of the regression models that first estimated the likelihood of having any utilization, and next the level of utilization conditional on having had any utilization.
The primary independent variable was treatment group assignment, modeled as a dummy indicator variable. The differential effect of IT in contrast to the comparison arm was measured using an intention-to-treat approach, thereby including all women in the analytic sample as long as they completed baseline and 12-month interviews, but regardless of whether they followed through with treatment. Effects were measured across each cluster using two respective vectors of cluster dummy variables and two vectors of cluster-treatment group interaction variables: (1) baseline symptom severity cluster dummy variables, each interacted with the treatment variable and (2), baseline service use/cost clusters, interacted with the treatment variable.
Because of the difficulty in interpreting coefficients from count data models, differential effects of IT versus usual care were calculated for clusters with significant treatment effects for a representative woman of mean age, 36.67 years old, who had not completed high school, reported having a serious physical illness or disability, was currently at risk for abuse, had some type of medical insurance, no perceived unmet need for care, and was recruited at a study site that provided mental health and substance abuse services in a residential treatment setting.
Results
Of the 2,026 women who completed 12-month interviews, 2,001 were included in the final analytic sample. (Twenty-five observations were dropped due to missing data as described earlier.) Table 2 presents descriptive statistics for the analytic sample, and baseline values for the symptom severity and service use clustering domains are presented in Table 1.
Table 2. Baseline sample characteristics by IT/comparison group.
| Overall study sample (N = 2,001) | IT group (N = 999) | Comparison group (1,002) | |
|---|---|---|---|
| Age | 36.7 | 36.6 | 36.7 |
| Race | |||
| White | 56.8% | 54.2%* | 59.4% |
| African | 27.1% | 31.9%** | 22.3% |
| American | |||
| Hispanic | 17.2% | 16.6% | 17.9% |
| Other | 18.3% | 17.4% | 19.3% |
| Education—mean # years | 11.6 | 11.5 | 11.7 |
| Physical illness or disability | 50.9% | 50.0% | 51.9% |
| Currently at risk for abuse | 71.9% | 73.4% | 70.4% |
| Any health insurance | 69.9% | 69.7% | 70.0% |
| Court-ordered treatment | 33.8% | 37.9%** | 29.7% |
| Perceived unmet need for care | 43.5% | 41.9% | 45.1% |
Z-score probabilities for intervention versus comparison group calculated for each variable using logistic regression
Significant at 5% level;
significant at 1% level
Among women characterized primarily by moderate-severe PTSD at baseline (C2-Sx), those in the IT group had statistically significantly fewer outpatient counseling visits at the 12-month follow-up than women in this cluster who received usual care (Table 3). A representative woman in sub-group C2-Sx who was in the IT treatment group would have received almost 25% fewer counseling visits during the year than her counterpart in the usual care group (35 visits, IT representative; 46 visits, usual care counter-factual). No other sub-groups showed significant differences in follow-up counseling use associated with IT versus usual care, including any of the service clusters (Table 4).
Table 3. Effect of IT on 12-month counseling visits by symptom clustersa,b.
| Probability of counseling use | Coefficient (SE) | Level of counseling use for users | Coefficient (SE) |
|---|---|---|---|
| Low symptom severity (C1-Sx) × IT | 0.057 | Low symptom severity (C1-Sx) × IT | 0.087 |
| (0.352) | (0.114) | ||
| Moderate-severe PTSD (C2-Sx) × IT | 0.245 | Moderate-severe PTSD (C2-Sx) × IT | −0.227** |
| (0.414) | (0.087) | ||
| Severe PTSD (C3-Sx) × IT | 0.180 | Severe PTSD (C3-Sx) × IT | 0.116 |
| (0.487) | (0.087) | ||
| Drugs & moderate-severe PTSD (C4-Sx) × IT | −0.347 | Drugs & moderate-severe PTSD (C4-Sx) × IT | −0.026 |
| (0.368) | (0.145) | ||
| Alcohol & severe PTSD (C5-Sx) × IT | −0.288 | Alcohol & severe PTSD (C5-Sx) × IT | 0.080 |
| (0.611) | (0.160) | ||
| Alcohol & moderate PTSD (C6-Sx) × IT | −0.128 | Alcohol & moderate PTSD (C6-Sx) × IT | −0.037 |
| (0.476) | (0.156) | ||
| Severe comobidity (C7-Sx) × IT | −0.080 | Severe comobidity (C7-Sx) × IT | −0.229 |
| (0.401) | (0.132) | ||
| Constant | −0.099 | Constant | 3.747** |
| (0.650) | (0.211) |
n = 2,001; Robust standard errors in parentheses
Significant at 5%;
significant at 1%
Zero-inflated negative binomial models
All models controlled for site-level fixed effects and selected person-level characteristics
Table 4. Effect of IT on 12-month counseling visits by service clustersa,b.
| Probability of counseling use | Coefficient (SE) | Level of counseling use for users | Coefficient (SE) |
|---|---|---|---|
| Low service use (C1-Serv) × IT | −0.220 (0.205) | Low service use (C1-Serv) 9 IT | −0.018 (0.079) |
| High counseling use (C2-Serv) × IT | 0.246 (0.518) | High counseling use (C2-Serv) × IT | −0.168 (0.097) |
| High residential treatment use (C3-Serv) × IT | −1.891 (1.177) | High residential treatment use (C3-Serv) × IT | 0.094 (0.152) |
| Moderate residential treatment days (C4-Serv) × IT | 0.755 (0.518) | Moderate residential treatment days (C4-Serv) × IT | −0.044 (0.149) |
| High psychotropic drug & external medical costs (C5-Serv) × IT | 0.251 (0.534) | High psychotropic drug & external medical costs (C5-Serv) × IT | 0.136 (0.073) |
| Constant | 0.265 (0.577) | Constant | 3.466** (0.184) |
n = 2,001; Robust standard errors in parentheses
Significant at 5%,
significant at 1%
Zero-inflated negative binomial models
All models controlled for site-level fixed effects and selected person-level characteristics
Several sub-groups of women in both the symptom and service clustering models demonstrated significant differences in follow-up residential treatment use according to treatment group assignment, for all of whom IT was associated with more residential treatment use than usual care. Women who had low-severity symptoms at baseline (C1-Sx) who were in the IT group had significantly more residential treatment days at follow-up as compared to their counterparts in the usual care group (Table 5). A representative woman in C1-Sx who was in IT had a predicted 118 days of residential treatment at follow-up as compared to 89 days if she was in the usual care group. Similar effects of IT on residential treatment use were seen among sub-groups of women characterized predominantly by moderate-severe PTSD (113 days for an average IT participant versus 82 days for an average usual care participant); women characterized by drug addiction and PTSD (123 days for IT versus 95 days for usual care); and women characterized by severe comorbidity for drugs, alcohol and PTSD (141 days for IT versus 105 days).
Table 5. Effect of IT on 12-month residential treatment days by symptom clustersa,b.
| Probability of residential treatment use | Coefficient (SE) | Level of residential treatment use for users | Coefficient (SE) |
|---|---|---|---|
| Low symptom severity (C1-Sx) × IT | 0.468 (0.280) | Low symptom severity (C1-Sx) × IT | 0.352** (0.100) |
| Moderate-severe PTSD (C2-Sx) × IT | 0.057 (0.263) | Moderate-severe PTSD (C2-Sx) × IT | 0.332** (0.105) |
| Severe PTSD (C3-Sx) × IT | 0.286 (0.273) | Severe PTSD (C3-Sx) × IT | 0.262 (0.138) |
| Drugs & moderate-severe PTSD (C4-Sx) × IT | 0.368 (0.386) | Drugs & moderate-severe PTSD (C4-Sx) × IT | 0.284** (0.102) |
| Alcohol & severe PTSD (C5-Sx) × IT | 0.405 (0.412) | Alcohol & severe PTSD (C5-Sx) × IT | 0.082 (0.193) |
| Alcohol & moderate PTSD (C6-Sx) × IT | 0.719 (0.383) | Alcohol & moderate PTSD (C6-Sx) × IT | 0.233 (0.142) |
| Severe comobidity (C7-Sx) × IT | 0.206 (0.356) | Severe comobidity (C7-Sx) × IT | 0.309** (0.101) |
| Constant | −2.724** (0.528) | Constant | 4.640** (0.207) |
n = 2,001; Robust standard errors in parentheses
Significant at 5%,
significant at 1%
Zero-inflated negative binomial models
All models controlled for site-level fixed effects and selected person-level characteristics
Unique effects of IT were also detected for two service clusters (Table 6). Among women characterized as low-intensity service users at baseline, women who were in the IT group used more days in residential treatment over one year of follow up than women in the usual care group (126 days for an average woman in the IT group versus 96 days for an average woman in the usual care group). Among women in the sub-group characterized by moderate residential treatment use at baseline (C4-Serv), those in the IT group used more days of residential treatment at follow-up as compared to women in the usual care group (140 days for IT versus 112 for usual care).
Table 6. Effect of IT on 12-month residential treatment days by service clustersa,b.
| Probability of residential treatment use | Coefficient (SE) | Level of residential treatment use for users | Coefficient (SE) |
|---|---|---|---|
| Low service use (C1-Serv) × IT | 0.800** | Low service use (C1-Serv) × IT | 0.369** |
| (0.203) | (0.073) | ||
| High counseling use (C2-Serv) × IT | 0.415 | High counseling use (C2-Serv) × IT | 0.248 |
| (0.354) | (0.133) | ||
| High residential treatment use (C3-Serv) × IC | −0.310 | High residential treatment use (C3-Serv) × IT | 0.080 |
| (0.407) | (0.117) | ||
| Moderate residential treatment days (C4-Serv) × IT | 1.100** | Moderate residential treatment days (C4-Serv) × IT | 0.248** |
| (0.380) | (0.093) | ||
| High psychotropic drug & external medical | 0.187 | High psychotropic drug & external medical | 0.261 |
| costs (C5-Serv) × IT | (0.252) | costs (C5-Serv) × IT | (0.141) |
| Constant | −3.692** | Constant | 4.623** |
| (0.503) | (0.140) |
n = 2,001; Robust standard errors in parentheses
Significant at 5%,
significant at 1%
Zero-inflated negative binomial models
All models controlled for site-level fixed effects and selected person-level characteristics
Certain model covariates had significant effects on participants' use of counseling and residential treatment at follow-up. One effect that was common to both clustering approaches for the counseling use outcome was that women who were court-ordered to engage in treatment had significantly more counseling visits than women who were not mandated to treatment. Other effects that were common to both clustering approaches included negative effects of current abuse and court orders to treatment on use of residential treatment, and positive effects of having insurance on use of residential treatment. There was also a predictive influence in each model associated with the study site at which participants were recruited. While site-level effects would be important for understanding how treatment and participant outcomes varied across study sites, they were included here as controls to isolate the effect of the intervention across different sub-groups of women.
The sensitivity analyses for the service clusters with the outliers removed indicated significant IT effects for two clusters that were not detected in the models with the outliers left in place—removing outliers resulted in unique IT effects for participants with high baseline counseling (a negative effect on follow-up counseling use) and for participants with high drug and medical costs (a positive effect on residential treatment use). Ultimately, the models with the outlying values for medical costs are preferred, as they retain the actual distributions of service use and cost patterns as they occurred in these study data and as they often do in health services data more generally, where a small percentage of people have very high levels of use/costs.
Discussion
This study adds to the evidence for differential effects of IT by examining post-intervention service use as conditioned by the intervention across distinct clusters of women. Women with co-occurring disorders and histories of abuse traditionally have considerable unmet need for specialized, integrated treatment services (SAMHSA 2002). The IT intervention has been shown to improve outcomes while not significantly increasing costs of services utilization. The challenge is to understand how best to provide these intervention services, by first identifying differences in the effect of the intervention across this heterogeneous group of consumers.
The intervention appeared to increase the efficiency of service use for some women in this study population—in other words, moving them toward an optimal balance between need for services based on symptomatology and intensity and mix of service use. The intervention was associated with reductions in counseling use for some women in this study population and increases in residential treatment use for others. Reductions in counseling use may have been evident because the women received trauma-informed, integrated counseling that addressed multiple needs—including trauma symptoms—in a single service setting rather than having to access a collection of separate services across various, fragmented service settings. Increases in time spent in residential treatment may have, for many, indicated improvements in service use efficiency by increasing their use of targeted services to better meet their treatment needs. The effect of IT on changes in efficiency of service utilization was variable across sub-groups, however, depending upon women's symptomatology and utilization patterns upon entering treatment.
Women who were characterized by low symptom severity at baseline and who were in the IT group may have actually used services inefficiently, as they used relatively high levels of residential treatment at follow-up as compared to their counterparts in the usual care group. Cusack et al. analyses (2008) found that IT had no effect on clinical outcomes among women who had low symptom severity at baseline, though their cluster assignments did not correspond exactly to those generated in these analyses. Together, these findings suggest that there was a mismatch between symptoms and service intensity for these women; their needs might have been better met by less intensive outpatient and support services. It is also possible, however, that higher relative use of residential treatment among women with low symptoms in the intervention group could reflect better treatment engagement, particularly if women in the control group used fewer days due to detrimental circumstances such as substance abuse relapse. That said, there is no reason to expect that the women with low symptom severity in the intervention group differed in a systematic way from their counterparts in the usual care group in terms of relapse risk or other characteristics other than their study group assignment.
Among women whose predominating symptom at baseline was moderate-severe PTSD, on the other hand, these study results suggest that IT was associated with more efficient service use. Women in this cluster who were assigned to IT used less outpatient counseling and more residential treatment at follow-up relative to their counterparts in the usual care group. Considering that women with this symptom profile were demonstrated in earlier work to be the major beneficiary of IT regarding clinical improvements (Cusack et al. 2008), a shift from outpatient counseling use among these women to more days in residential treatment was likely beneficial to their clinical functioning, thereby indicating improvement in the efficiency of intensity and mix of their service use.
Interestingly, no differences in the effect of the intervention on outpatient counseling use at 12 months were detected when women were clustered according to their baseline service patterns. In this case, baseline service use behaviors alone appeared not to moderate the intervention effect in the same way that symptomatology did, which for the counseling use outcome countered our expectation for its superior predictive value of effect measure modification.
The IT intervention was associated with more days spent in residential treatment as compared to usual care for several other sub-groups of women. Among two subgroups of women who suffered severe symptoms of substance abuse and PTSD—women with high drug addiction and PTSD, and women with severe comorbidity for drugs, alcohol and PTSD—and who were in the IT group, a relative increase in use of residential treatment appeared to indicate an appropriate increase in their service use, particularly considering women with these symptom profiles had active substance abuse problems for which residential treatment may be most appropriate and that they demonstrated significant clinical improvements in analyses by Cusack et al. (2008).
Similar IT effects on residential treatment use were also demonstrated by certain sub-groups of women when characterized by their baseline service use patterns. Women who were low-intensity service users and in the IT group used more residential treatment at follow up than their counterparts in the usual care group. This cluster of women may have been under-served in the pre-intervention period, particularly considering almost 80% of them had some combination of severe substance abuse or trauma symptoms at baseline. If so, relative increases in their use of residential treatment likely reflected an appropriate shift in service utilization to meet their treatment needs. Additional analysis of the changes in symptomatology at follow up specifically for women with low baseline service use would add more context for their increased use of residential treatment, particularly considering it is a highly resource-intensive modality of treatment (Dickey and Azeni 1996; Barnett and Swindle 1997; Roebuck et al. 2003) and interrupts women's lives and roles in their communities.
Women who used moderate levels of residential treatment at baseline and were in the IT group spent more days in residential treatment by 1 year than similar women in usual care. The large majority of women in this sub-group characterized by moderate residential treatment use at the start of the study also had some combination of severe symptoms at baseline, which suggests that relatively higher intensity use of this targeted type of treatment was likely appropriate and demonstrated improved efficiency in their service utilization. This finding also suggests that the intervention worked to boost or sustain the use of residential treatment for women who were already engaged in it in a way that usual care did not.
A key contribution of this study is the identification of differential effects of the IT intervention on service utilization within a heterogeneous population of women with co-occurring disorders and histories of abuse, adding to the existing evidence for its heterogeneous effects on clinical outcomes (Cusack et al. 2008). The assumption of a homogeneous treatment response is often unreasonable without empirical evidence to support it (Manski 2001). Therefore, differential treatment response should be estimated according to important moderators—in this case, symptomatology and service utilization patterns—in an effort to work toward maximizing the benefits of treatment for different types of women in this population. Both average effects of IT within the population and sub-group effects of IT according to defining characteristics can help policymakers understand how IT works in the population at large, as well as by whom specifically it is used most and least efficiently. Integrated treatment like the intervention studied here is resource intensive and should be targeted to people who have a demonstrated need for it according to their symptomatology and/or service use patterns. Conversely, other people who are functioning well could benefit equally from less intensive usual care services.
There are limitations to this study that are important to consider. First, a quasi-experimental study design can introduce biases through unbalanced treatment groups and differential attrition as described earlier. A benefit of non-random recruitment is that the resultant study groups were more representative of women who, in the real world, may be targeted to receive IT services and others who remain in settings where they receive usual care. Secondly, making the assumption that treatment assignment was the equivalent of treatment receipt may have biased results if participants in the usual care group were actually receiving IT-type services. There is evidence, however, that differences in intervention and comparison program content in this study were associated with differential improvements in outcomes attributed to the intervention (Cocozza et al. 2005). Further, unmeasured receipt of IT-type services by participants in the usual care group would attenuate the intervention effect, biasing the estimates downwards and producing conservative results.
The shortcoming of using an arbitrary number of clusters was mitigated by use of specification tests and other analytic tools for assessing the sensitivity of the cluster results. This included conducting several iterations of the clustering process using different variable scaling approaches, and re-generating effect estimates after combining similar clusters to detect any differences in the effect of IT on sub-groups of study participants.
While insurance variables are invariably endogenous, endogeneity bias is arguably minimal in these analyses for two reasons. Model estimates of the effect of IT on outcomes were not significantly different when estimated without a control for insurance status. Second, the presence of a covariate for serious physical illness or disability is an exogenous variable that likely accounted for some of the unique effect of insurance status.
While the characterization of women's symptomatology or service use at baseline in part drove changes in counseling or residential treatment utilization over time, there is no reason to expect that the influence of their baseline profiles would have operated differentially across study groups within the respective clusters. Therefore, unique effects on counseling and residential treatment use that were demonstrated in the IT group versus the usual care group for different sub-groups of women according to their baseline profiles are likely attributable to the intervention and not artifacts of selection bias or regression toward the mean.
Women who are characterized primarily by PTSD, severe drug addiction and PTSD, or severe comorbidity generally responded to the intervention by using more residential treatment than their counterparts in usual care. When considering this new evidence about service use by women with these symptom profiles along with existing evidence of IT improving their clinical functioning (Cusack et al. 2008), IT in residential treatment settings should be encouraged for women with these symptom profiles. Women with histories of low service use also responded to the intervention by using more residential treatment, a central mode of treatment for people with co-occurring disorders. For these groups of women, the increase likely signaled a shift to more efficient service use by increasing their use of targeted treatment for co-occurring disorders.
The findings presented here provide useful information for service providers and the agencies in which they work. Expected number of services provided is an important measure for provider and agency planning related to capacity, staffing, and other resources. This will be particularly important for agencies that provide integrated treatment in residential settings, as IT was associated with more time spent in residential treatment for several groups of women in this study population.
Practitioners who treat women in this population can use this information to encourage engagement in integrated treatment in residential settings among women in the population with active symptoms of addiction and PTSD. There is also an opportunity based on these findings for service providers without diagnostic expertise to identify consumers in this population who are not using treatment services regularly, and attempt to link them to integrated treatment with the expectation that it may lead to their using more residential care. In the interest of maximizing scarce public resources, program directors and policymakers can use this evidence to focus their targeting of this effective though resource-intensive type of integrated treatment toward the women in this population for whom it appeared to work best—those with severe substance abuse and PTSD symptoms. Finally, the evidence presented here presents an opportunity for future research that would look more closely at the provision of integrated treatment in residential settings, and identify factors within those contexts that are associated with optimal clinical and service outcomes among women with co-occurring disorders and trauma.
Alternatives should be considered for women in this population with low-severity baseline symptoms, as they had relatively large increases in their use of residential treatment and, in other work (Cusack et al. 2008), were found to have no change in clinical symptoms. Particularly considering that resources for mental health and substance abuse treatment are constrained, efforts should be made to direct women with this symptomatology to use less resource-intensive outpatient services.
Despite a body of evidence demonstrating the benefits of IT without significantly increased costs, this type of integrated, trauma-informed care is not readily available in most communities. Until it is diffused more widely, professionals involved in the planning, implementation, and administration of treatment services for people with co-occurring disorders should consider targeting IT to the sub-groups of women represented in this study population who appeared to benefit most from the intervention in terms of efficient use of appropriate treatment services.
Contributor Information
Allison R. Gilbert, Email: allison.gilbert@duke.edu, Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine, DUMC Box 3071, Durham, NC 27710, USA.
Marisa E. Domino, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Joseph P. Morrissey, Departments of Health Policy and Management and Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Bradley N. Gaynes, Department of Psychiatry, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
References
- Alexander MJ. Women with co-occurring addictive and mental disorders: An emerging profile of vulnerability. American Journal of Orthopsychiatry. 1996;66(1):61–70. doi: 10.1037/h0080155. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Barnett PG, Swindle RW. Cost-effectiveness of inpatient substance abuse treatment. Health Services Research. 1997;32(5):615–629. [PMC free article] [PubMed] [Google Scholar]
- Becker MA, Noether CD, Larson MJ, Gatz M, Brown V, Heckman JP, et al. Characteristics of women engaged in treatment for trauma and co-occurring disorders: findings from a national multisite study. Journal of Community Psychology. 2005;4(33):429–443. [Google Scholar]
- Chen S, Barnett PG, Sempel JM, Timko C. Outcomes and costs of matching the intensity of dual-diagnosis treatment to patients' symptom severity. Journal of Substance Abuse Treatment. 2006;31(1):95–105. doi: 10.1016/j.jsat.2006.03.015. [DOI] [PubMed] [Google Scholar]
- Clark RE, Samnaliev M, McGovern MP. Treatment for co-occurring mental and substance use disorders in five state Medicaid programs. Psychiatric Services. 2007;58:942–948. doi: 10.1176/ps.2007.58.7.942. [DOI] [PubMed] [Google Scholar]
- Cocozza JJ, Jackson E, Hennigan K, Morrissey JP, Reed BG, Fallot R, et al. Outcomes for women with co-occurring disorders and trauma: Program-level effects. Journal of Substance Abuse Treatment. 2005;28(2):109–119. doi: 10.1016/j.jsat.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Cusack KJ, Morrissey JP, Ellis AR. Targeting trauma-related interventions and improving outcomes for women with co-occurring disorders. Administration and Policy in Mental Health. 2008;35(3):147–158. doi: 10.1007/s10488-007-0150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L. A brief form of the SCL-90-R: A self-report symptom inventory designed to measure psychological stress: Brief system inventory (BSI) Minneapolis: National Computer Systems; 1993. [Google Scholar]
- Dickey B, Azeni H. Persons with dual diagnoses of substance abuse and major mental illness: Their excess costs of psychiatric care. American Journal of Public Health. 1996;86(7):973–977. doi: 10.2105/ajph.86.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domino ME, Morrissey JP, Chung S, Huntington N, Larson MJ, Russell LA. Service use and costs for women with co-occurring mental and substance use disorders and a history of violence. Psychiatric Services. 2005a;56(10):1223–1232. doi: 10.1176/appi.ps.56.10.1223. [DOI] [PubMed] [Google Scholar]
- Domino ME, Morrissey JP, Chung S, Nadlicki T. Changes in service use during a trauma-informed intervention for women. Women and Health. 2006;44(3):105–122. doi: 10.1300/J013v44n03_06. [DOI] [PubMed] [Google Scholar]
- Domino M, Morrissey JP, Nadlicki-Patterson T, Chung S. Service costs for women with co-occurring disorders and trauma. Journal of Substance Abuse Treatment. 2005b;28(2):135–143. doi: 10.1016/j.jsat.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser KT, Brunette MF, McHugo GJ. A review of treatments for people with severe mental illnesses and co-occurring substance abuse disorders. Psychiatric Rehabilitation Journal. 2004;27(4):360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- Foa E. Posttraumatic stress diagnostic scale manual. Minneapolis: National Computer Systems; 1995. [Google Scholar]
- Foa E, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttramatic stress disorder: The posttraumatic diagnostic scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Fullilove MT, Fullilove RE, Smith M, Winkler K, Michael C, Panzer PG, et al. Violence, trauma, and post-traumatic stress disorder among women drug users. Journal of Traumatic Stress. 1993;6(4):533–543. [Google Scholar]
- Gearon JS, Kaltman SI, Brown C, Bellack AS. Traumatic life events and PTSD among women with substance use disorders and schizophrenia. Psychiatric Services. 2003;54(4):523–528. doi: 10.1176/appi.ps.54.4.523. [DOI] [PubMed] [Google Scholar]
- Goldberg D, Huxley P. Mental illness in the community: the pathway to psychiatric care. New York: Tavistock Publications, Ltd; 1980. [Google Scholar]
- Goodman LA, Rosenberg SD, Muese K, Drake RE. Physical and sexual assault history in women with serious mental illness: Prevalence, correlates, treatment, and future research directions. Schizophrenia Bulletin. 1997;23(4):685–696. doi: 10.1093/schbul/23.4.685. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Salyers MP, Mueser KT, Rosenberg SD, Swartz M, Essock SM, et al. Recent victimization in women and men with severe mental illness: Prevalence and correlates. Journal of Traumatic Stress. 2001;14:615–632. doi: 10.1023/A:1013026318450. [DOI] [PubMed] [Google Scholar]
- Greenfield L, Burgdorf K, Chen X, Porowski A, Roberts T, Herrell J. Effectiveness of long-term residential substance abuse treatment for women: Findings from three national studies. American Journal of Drug and Alcohol Abuse. 2004;30(3):537–550. doi: 10.1081/ada-200032290. [DOI] [PubMed] [Google Scholar]
- Hanson T, Hesselbrock M, Tworkowski SH, Swan S. The prevalence and management of trauma in the public domain: An agency and clinician perspective. The Journal of Behavioral Health Services & Research. 2002;29:365–380. doi: 10.1007/BF02287344. [DOI] [PubMed] [Google Scholar]
- Harris M. Modifications in service delivery and clinical treatment for women diagnosed with severe mental illness who are also the survivors of sexual abuse trauma. Journal of Mental Health Administration. 1994;21(4):397–406. doi: 10.1007/BF02521358. [DOI] [PubMed] [Google Scholar]
- Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services. 2005;56(8):954–959. doi: 10.1176/appi.ps.56.8.954. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner RA, Nelson CB, Schlenberg J, Anthony JC. Lifetime co-occurrence of DSM III-R alcohol abuse and dependence with other psychiatric disorders in the national comorbidity survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Keyser DJ, Watkins KE, Vilamovska A, Pincus HA. Improving service delivery for individuals with do-occurring disorders: New perspectives on the quadrant model. Psychiatric Services. 2008;59:1251–1253. doi: 10.1176/ps.2008.59.11.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattree R, Naik D. Multivariate data reduction and discrimination with SAS software. Cary: SAS Institute, Inc; 1999. [Google Scholar]
- Larkin S. Origins of the quadrant model for persons with co-occurring disorders. Psychiatric Services. 2007;58(12):1607–1608. doi: 10.1176/ps.2007.58.12.1607. [DOI] [PubMed] [Google Scholar]
- Larson MJ, Miller L, Becker M, Richardson E, Kammerer N, Thom J, et al. Physical health burdens of women with trauma histories and co-occurring substance abuse and mental disorders. The Journal of Behavioral Health Services & Research. 2005;32(2):128–140. doi: 10.1007/BF02287262. [DOI] [PubMed] [Google Scholar]
- Manski CF. New developments in evaluating social programs. The American Economic Review. 2001;91(2):103–106. [Google Scholar]
- McGovern MP, Clark RE, Samnaliev M. Co-occurring psychiatric and substance use disorders: A multi-state feasibility study of the quadrant model. Psychiatric Services. 2007;58:949–954. doi: 10.1176/ps.2007.58.7.949. [DOI] [PubMed] [Google Scholar]
- McHugo GJ, Kammerer N, Jackson EW, Markoff LS, Gatz M, Larson MJ, et al. Women, co-occurring disorders, and violence study: Evaluation design and study population. Journal of Substance Abuse Treatment. 2005;2:91–107. doi: 10.1016/j.jsat.2004.08.009. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner J, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Woody G, Metzger D. Evaluating the effectiveness of addiction treatments: Reasonable expectations, appropriate comparisons. The Milbank Quarterly. 1996;74:51–85. [PubMed] [Google Scholar]
- Milligan GW. An examination of the effect of six types of error perturbation on fifteen clustering algorithms. Psychometrika. 1980;45:325–342. [Google Scholar]
- Milligan GW, Cooper MC. An examination of procedures for determining the number of clusters in a data set. Psychometrika. 1985;50:159–179. [Google Scholar]
- Milligan GW, Cooper MC. A study of standardization of variables in cluster analysis. Journal of Classification. 1988;5:181–204. [Google Scholar]
- Morrissey JP, Ellis AR, Gatz M, Amaro H, Reed BG, Savage A, et al. Outcomes for women with co-occurring disorders and trauma: Program and person-level effects. Journal of Substance Abuse Treatment. 2005a;28(2):21–33. doi: 10.1016/j.jsat.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits L. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatric Services. 2005b;56(10):213–222. doi: 10.1176/appi.ps.56.10.1213. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Goodman LB, Trumbetta SL, Rosenberg SD, Osher C, Vidaver R, et al. Trauma and posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 1998;66(3):493–499. doi: 10.1037//0022-006x.66.3.493. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and post-traumatic stress disorder in women: A research review. The American Journal of Addictions/American Academy of Psychiatrists in Alcoholism and Addictions. 1997;6:273–283. [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. Seeking safety: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance abuse. Journal of Trauma Stress. 1998;11(3):437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- National Association of the State Mental Health Program Directors & National Association of State Alcohol and Drug Abuse Directors. National dialogue on co-occurring mental health and substance abuse disorders. 1998 Retrieved from www.nasadad.org/Departments/Research/ConsensusFramework/national_dialogue_on.htm.
- Roebuck MC, French MT, McLellan AT. DATStats: Results from 85 studies using the Drug Abuse Treatment Cost Analysis Program (DATCAP) Journal of Substance Abuse Treatment. 2003;25:51–57. doi: 10.1016/s0740-5472(03)00067-9. [DOI] [PubMed] [Google Scholar]
- Shrout PE. Measurement reliability and agreement in psychiatry. Statistical Methods in Medical Research. 1998;7:301–317. doi: 10.1177/096228029800700306. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Agency, US Department of Health and Human Services. Report to Congress on the prevention and treatment of co-occurring substance abuse disorders and mental disorders. 2002. [Google Scholar]
- Watkins KE, Burnam A, Kung FY, Paddock S. A national survey of care for persons with co-occurring mental health and substance abuse disorders. Psychiatric Services. 2001;52(8):1062–1068. doi: 10.1176/appi.ps.52.8.1062. [DOI] [PubMed] [Google Scholar]