Abstract
Purpose
Evaluating disparities in health care is an important aspect of understanding differences in disease risk. The purpose of this study is to describe methodology for estimating such disparities, with application to a large multi-ethnic cohort study.
Methods
The Multi-Ethnic Study of Atherosclerosis (MESA) includes 6814 participants aged 45–84 years free of cardiovascular disease. Prevalence ratio (PR) regression was used to model baseline lipid lowering medication (LLM) or anti-hypertensive medication use at baseline as a function of gender, race, risk factors and estimated pre-treatment biomarker values.
Results
Hispanics and African-Americans had lower prevalence of medication use than non-Hispanic whites, even at the same risk factor profile. This became non-significant after adjustment for socio-economic status. Although gender did not influence the prevalence of LLM use (PR=1.09, 95% CI 0.95 to 1.25), there were differences in the association of diabetes and HDL with LLM use by gender. Men were significantly less likely to be on anti-hypertensive medications than women (PR=0.86, 95% CI 0.80 to 0.92, p<0.001) and this was not explained by risk factors or socioeconomic status. Lack of health insurance strongly influenced medication use, controlling for risk factors and other markers of socio-economic status.
Conclusions
Disparities exist in the treatment of cholesterol and hypertension. Hispanics and African Americans had less use of LLM, men had less use of anti-hypertensives. Risk factors have differential associations with medication use depending on gender. Methods described in this paper can provide improved disparity estimation in observational cohort studies.
Keywords: disparities, medication, statistical methods, statins, anti-hypertensives
Introduction
The ability to evaluate disparities in health care delivery is an important aspect of understanding differences in subsequent disease risk. African Americans and Hispanic Americans have higher risk of cardiovascular disease (CVD) relative to whites, and higher prevalence of many cardiovascular risk factors including hypertension, diabetes, and obesity [1]. It is less clear whether there are disparities in treatment for these conditions, and if so, whether there is an explanation for these disparities such as socioeconomic status. We consider a disparity to exist if, at a given risk factor profile, one subset of participants is less likely to receive a recommended treatment.
Large population based observational cohort studies such as the Multi-Ethnic Study of Atherosclerosis (MESA) offer an excellent resource for exploring such disparities. The MESA cohort covers a broad age range (45–84 at entry), is gender balanced, includes four racial/ethnic groups (Caucasians, Chinese-Americans, African Americans, and Hispanics), and was conducted with standardized assessments. All participants were free of clinically apparent cardiovascular disease at study entry, and thus a study sample eligible for primary prevention. However, methodologic challenges also exist when studying disparities in the cohort setting. Many of the MESA participants are receiving medical therapies, with almost 40% of participants on anti-hypertensive medications at baseline (2000–2002), and 16% on lipid lowering medication. These numbers rise to approximately one half and one third of the population by the fourth follow-up examination respectively (2005–2007). Participants not on medications at baseline but who begin treatment later in the study (“new users”) may have been influenced by the fact that we reported baseline results (including blood pressure and cholesterol) to both participants and their physicians. Estimated rates of new users may thus be higher and more equally distributed across racial/ethnic and socioeconomic groups than in the general population. For example, examination of such participants who started on a new medication after the baseline exam would underestimate any disparities due to lack of access to regular health care or disparities in screening. Thus, for purposes of evaluating disparities it is more desirable to examine rates of medication use at the time that participants enter the study. However, for participants taking medications at baseline, we have confounding by indication since we do not have a measurement of their pre-treatment biomarker values.
One option is to examine utilization patterns without accounting for pre-treatment biomarker values [2]. However it is unclear then how much the differences reflect actual disparities (different rates of use at the same risk factor profile) versus differences due to differing risk factor profiles. For instance, African Americans are known to have higher rates of hypertension compared to non-Hispanic whites, and thus they have (and should have) a greater prevalence of anti-hypertensive medication use. What is less clear, however, is whether they are more likely (or less likely) to be treated at a given level of untreated blood pressure and risk factor profile. In other words, it is unclear whether there is a disparity as opposed to merely a difference. Another approach to this question is to focus on the prevalence of untreated hypertension/dyslipidemia—that is, the proportion of the population meeting the criteria for treatment but not receiving it [3–7]. This is a valid approach, however, it leaves open the possibility of residual confounding by the level/severity of the untreated hypertension/dyslipidemia. That is, even though everyone is above the threshold for the diagnosis, there may remain large differences in the magnitude of the blood pressure/cholesterol that are not accounted for by this method.
In this paper we use a modeling approach described previously [8] to estimate pre-treatment cholesterol and blood pressure values for those on medications at baseline. We then fit models for the prevalence of medication use that control for estimated pre-treatment values of the underlying biomarker of interest. Differences by covariates such as gender or race/ethnicity then reflect differences in medication use conditional on the underlying biomarker. We use these models to examine gender and racial/ethnic disparities in medication use in MESA, as well as to compare risk factor associations with medication use across gender/ethnicity groups.
Methods
The Multi-Ethnic Study of Atherosclerosis
MESA is designed to study the prevalence, risk factors and progression of subclinical cardiovascular disease in a multi-ethnic population. A detailed description of the study design and methods has been published previously [9]. Briefly, 6814 participants aged 45–84 years who identified themselves as White, African-American, Hispanic, or Chinese were recruited from six U.S. communities from 2000–2002. All participants were free of clinically apparent cardiovascular disease. The communities were Forsyth County, NC; Northern Manhattan and the Bronx, NY; Baltimore City and Baltimore County, MD; St. Paul, MN; Chicago, IL; and Los Angeles County, CA. Each field center developed its recruitment procedures according to the characteristics of its community and available resources, including lists of residents, dwellings, and telephone exchanges. Supplemental resources, including lists of Medicare beneficiaries and referrals by participants, were used in the last stages of enrollment to meet goals for the elderly and minorities. Each site recruited an approximately equal number of men and women, according to pre-specified age and race/ethnicity proportions. All participants gave informed consent.
Information on demographics, smoking, medical conditions, and family history, were collected via questionnaire at the initial examination. Height and weight were measured at the baseline exam, and blood was drawn for measurements including lipids, inflammation, fasting glucose, and fibrinogen. Resting blood pressure was measured three times in the seated position, and the average of the last two measurements was used in analysis. Medication use was determined by questionnaire. Additionally, the participant was asked to bring to the clinic containers for all medications used during the two weeks prior to the visit. The interviewer then recorded the name of each medication, the prescribed dose, and frequency of administration from the containers. The participant was also queried about how many pills they had taken over the past two weeks on average per day/week/month. All analyses described in this paper use the information transcribed from the containers.
Statistical Methods
For participants taking lipid lowering medication at baseline their pre-treatment cholesterol levels were estimated using techniques that have been described previously [8]. Similarly, we also estimate pre-treatment blood pressure for those taking anti-hypertensive medication at baseline. Briefly, pre-treatment values are estimated based on type of drug, observed cholesterol/blood pressure, and demographics. The model used is derived from the subset of new drug users throughout the study (that is, using the pre and post treatment values for the new users). This model is then applied to the subset of participants already taking medication at baseline (a mutually exclusive subset from the new user subset on which the model is estimated). For cholesterol the imputation model included: observed on-treatment cholesterol, age, gender, race/ethnicity, diabetes, anti-hypertensive medication use (yes/no), HDL cholesterol, triglycerides, indicators for each type of lipid lowering medication (atorvastatin, fluvastatin, lovastatin, pravastatin, simvastatin, rosuvastatin, fibrates, resins, niacin, ezetimibe). For each of the statins except rosuvastatin we also indicated average versus high dose. We imputed total cholesterol rather than LDL cholesterol since total cholesterol was measured, and LDL was estimated via the Friedewald equation [10] and is missing for specimens with triglyceride >400mg/dl.
The model to impute pre-treatment blood pressures was developed to include: observed on-treatment systolic and diastolic blood pressures, age, gender, race/ethnicity, body mass index, diabetes, HDL and total cholesterol, smoking status (never/former/current), indicators for each class of anti-hypertensive medication (beta blockers, calcium channel blockers, diuretics, ACE inhibitors/angiotensin II receptor blockers, vasodilators), all two-way interactions between different medication types, and two way interaction between each of gender and race/ethnicity with each medication type. To incorporate the additional variability inherent in having to estimate the pre-treatment biomarker values, we use multiple imputation techniques following the algorithm of Van Buuren et al. [11] as implemented and described by Royston [12, 13]. For each biomarker (either cholesterol or systolic and diastolic blood pressures) 10 imputations are created. Models using the biomarkers are repeated 10 times and results are pooled using a set of rules proposed by Rubin [14].
Two sets of regression models for the prevalence of medication use at baseline were developed: one for use of anti-hypertensive medications, one for the use of lipid lowering medications. A first model for each endpoint included age, gender, race/ethnicity, estimated pre-treatment blood pressures (or cholesterol for the lipid lowering model), diabetes, cholesterol (or hypertension), body mass index, and smoking status. A second model included income, education, and health insurance to explore the extent to which differences in socioeconomic status may explain the disparities. The interactions of each risk factor with gender and race/ethnicity were tested, and models exploring the relationship of risk factors with medication use were subsequently stratified into groups by gender and race/ethnicity. For these models we used a form of prevalence ratio regression, a generalized linear model with a log link, Gaussian error structure, and robust standard errors. This is preferable to logistic regression here because the endpoints (medication use) are not rare, and odds ratios would not approximate the relative risks.
Results
In Table 1 we describe the baseline characteristics of the MESA participants. Overall 16% of the cohort was taking lipid lowering medication, and 37% were taking anti-hypertensive medications. These percentages varied by both gender and race/ethnicity. The highest percentage of lipid lowering medication use was among Caucasian men at 19.9%, but for the other three racial/ethnic groups women had a slightly higher prevalence of use than men, ranging from 13.8% for Hispanic women to 17% for African-American women. A large percentage of those with high cholesterol were untreated. This percentage ranged from 22.5% in African-American men, to almost 50% in Hispanic women. The prevalence of anti-hypertensive medication use was highest among African-American men (53.1%) following by African-American women (46.9%), and the lowest prevalence was among Chinese men (28.2%) and women (29.3%). Approximately 17–30% of those with hypertension were not treated, with lowest rates of untreated hypertension in black women, and the highest in Chinese men.
Table 1.
Participant Characteristics by Gender and Race/Ethnicity: The Multi-Ethnic Study of Atherosclerosis, 2000–2002
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| White N=1363 |
Chinese- American N=413 |
African- American N=1050 |
Hispanic N=775 |
White N=1259 |
Chinese- American N=390 |
African- American N=843 |
Hispanic N=721 |
|
| LLM Use (%) Dyslipidemia (%) %Dyslipidemia untreated |
16.7 28.5 41.1 |
16.0 22.5 29.0 |
17.0 26.0 34.4 |
13.8 27.5 49.8 |
19.9 27.2 26.4 |
12.8 19.0 32.4 |
15.5 19.9 22.2 |
12.3 20.8 40.7 |
| Obs. cholesterol (mg/dl) Pre-tx cholesterol (mg/dl) |
202 209 |
195 201 |
196 202 |
202 207 |
189 197 |
190 193 |
182 186 |
194 197 |
| Anti-htn med use (%) Hypertension (%) % Hypertension untreated |
32.3 43.0 24.8 |
29.3 40.4 27.5 |
53.1 63.8 16.9 |
34.6 46.6 25.8 |
33.9 44.4 23.8 |
28.2 40.5 30.4 |
46.9 59.3 21.0 |
30.4 41.6 27.0 |
| Observed SBP (mmHG) Pre-tx SBP (mmHG) |
123 126 |
125 127 |
133 137 |
127 130 |
124 127 |
124 126 |
130 134 |
126 128 |
| Observed DBP (mmHG) Pre-tx DBP (mmHG) |
67 69 |
69 70 |
72 75 |
68 69 |
74 76 |
75 80 |
77 80 |
75 76 |
| Age (mean, yrs) | 62.5 | 62.3 | 62.1 | 61.4 | 62.7 | 62.4 | 62.2 | 61.1 |
| Body Mass Index (kg/m2) | 27.5 | 23.9 | 31.3 | 30.0 | 27.9 | 24.1 | 28.7 | 28.8 |
| Diabetes (%) | 4.6 | 12.4 | 16.1 | 16.4 | 7.6 | 13.9 | 19.3 | 19.0 |
| Smoking Status (%) Never Former Current |
48.6 39.6 11.8 |
96.1 2.2 1.7 |
52.0 31.8 16.2 |
67.4 21.8 10.8 |
39.6 49.3 11.2 |
53.2 37.0 9.8 |
36.8 42.9 20.3 |
39.5 44.0 16.5 |
| Education (%) <highschool Highschool graduate College Graduate school |
5.7 53.3 20.1 20.9 |
32.5 40.9 18.2 8.5 |
11.8 54.2 17.2 16.7 |
47.7 45.2 4.5 2.6 |
4.1 37.0 24.5 34.5 |
16.7 31.4 27.5 24.4 |
12.6 53.6 17.4 16.3 |
41.3 45.8 6.7 6.2 |
| Family Income (%) <$25k $25k–$49k $50k–$99k $100k+ |
21.1 29.6 30.4 18.8 |
55.4 21.1 16.2 7.4 |
35.6 34.6 23.8 6.0 |
55.7 31.1 12.4 0.8 |
10.9 23.6 35.2 30.3 |
43.4 22.9 20.8 12.9 |
24.2 29.1 35.5 11.3 |
42.9 34.5 18.6 4.1 |
| Insurance (%) No Health Insurance Medicare Private Insurance Medicaid/VA/other |
2.1 39.7 55.9 2.3 |
18.9 33.2 40.4 7.5 |
6.6 37.8 52.4 3.2 |
19.5 28.4 44.3 7.8 |
3.3 39.4 53.9 3.4 |
19.5 32.4 42.7 5.4 |
5.8 36.7 50.2 7.4 |
16.4 30.4 46.2 7.0 |
| Usual Source of Care (%) Doctor’s office/clinic Emergency Room Other |
98.1 0.3 1.6 |
93.0 1.2 5.8 |
95.5 2.0 2.5 |
86.1 8.8 5.1 |
96.0 1.3 2.7 |
94.1 1.6 4.4 |
90.1 3.5 6.4 |
83.3 8.2 8.5 |
LLM=lipid lowering medication; Obs. =observed level of biomarker; Pre-tx=estimated pre-treatment value of biomarker; Htn=hypertension; med=medication. Dyslipidemia defined as total cholesterol over 240 or taking lipid lowering medications. Untreated hypertension defined as systolic blood pressure (SBP) over 140 mmHg and/or diastolic blood pressure (DBP) over 90 mmHg and not taking anti-hypertensive medications. Pre-treatment values are estimated, using the methods described in this paper—the means are calculated using the observed cholesterol for those not on treatment, and the estimated pre-treatment value for those on treatment.
Adjusted prevalence ratios for medication use are presented in Table 2. After adjusting for risk factors including estimated pre-treatment cholesterol there is no apparent gender disparity in the use of lipid lowering medications. Both Hispanics and African Americans were significantly less likely to be taking a lipid lowering medication at the same level of risk factors (Hispanics: PR 0.75, 95% CI 0.61 to 0.91; African-Americans: PR 0.84, 95% CI 0.73 to 0.97, p=0.02). These differences were attenuated and became non-significant after additional adjustment for socio-economic factors, primarily health insurance. All minority groups were far more likely to be uninsured than non-Hispanic whites (Chinese 19%, Hispanics 18%, African American 6% versus non-Hispanic Whites with 2.7% uninsured). The prevalence of anti-hypertensive medication use was significantly lower among men than women (Table 1). This difference was not explained by risk factors, estimated pre-treatment blood pressure, or socio-economic variables. Differences in anti-hypertensive medication use across race/ethnicities were slight and overall non-significant, conditional on the same risk factor profile.
Table 2.
Medication Use by Race/ethnicity and Gender: The Multi-Ethnic Study of Atherosclerosis, 2000–2002
| Lipid Lowering Medications |
Anti-hypertensive Medications |
||||
|---|---|---|---|---|---|
| PR (95% CI) | p-value | PR (95% CI) | p- value |
||
| Adjusted for age, diabetes, hypertension or high cholesterol, BMI, HDL, current smoking, family history of MI, clinic site, and the pre-treatment biomarker* |
Gender: women men Race/ethnicity: white Chinese-American African-American Hispanic |
Ref 1.09 (0.95, 1.25) Ref 1.26 (0.97, 1.62) 0.84 (0.73, 0.97) 0.75 (0.61, 0.91) |
0.20 0.08 0.02 0.004 |
Ref 0.86 (0.80, 0.92) Ref 0.99 (0.88, 1.11) 1.08 (1.00, 1.16) 0.92 (0.84, 1.01) |
<0.001 0.89 0.05 0.07 |
| Previous model plus insurance, education and income |
Gender: women men Race/ethnicity: white Chinese-American African-American Hispanic |
Ref 1.07 (0.94, 1.23) Ref 19 (1.02, 1.62) 0.87 (0.74, 1.02) 0.85 (0.68, 1.06) |
0.30 0.03 0.09 0.14 |
Ref 0.85 (0.79, 0.92) Ref 1.00 (0.88, 1.12) 1.05 (0.97, 1.14) 0.93 (0.84, 1.03) |
<0.001 0.95 0.19 0.15 |
models for lipid lowering medications adjust for estimated pre-treatment cholesterol, and models for anti-hypertensive medications adjust for estimated pre-treatment systolic and diastolic blood pressures; BMI=body mass index; MI=myocardial infarction; PR=prevalence ratio; CI=confidence interval; Hypertension defined as systolic blood pressure (SBP) over 140 mmHg and/or diastolic blood pressure (DBP) over 90 mmHg ; high cholesterol defined as a total cholesterol over 200mg/dl or taking lipid lowering medication.
For lipid lowering medication use we found several gender interactions, specifically with diabetes (p=0.004) and HDL cholesterol (p=0.015) after adjustment for the other risk factors (Table 3). Diabetes was much more strongly associated with the use of lipid lowering therapy among women than among men regardless of race/ethnicity. In fact, in White and Hispanic men diabetes was not associated with more lipid lowering therapy. HDL cholesterol was associated with lower rates of lipid lowering therapy only among white women.
Table 3.
Risk Factors and the Prevalence of Lipid Lowering Medication Use by Gender and Race/Ethnicity: The Multi-Ethnic Study of Atherosclerosis, 2000–2002
| White | Chinese-American | African-American | Hispanic | |||||
|---|---|---|---|---|---|---|---|---|
| WOMEN | PR (95% CI) | p- value |
PR (95% CI) | p- value |
PR (95% CI) | p-value | PR (95% CI) | p-value |
| Age (yrs) | 1.13 (1.05, 1.20) | <0.001 | 1.13 (0.99,1.28) | 0.07 | 1.06 (0.98,1.14) | 0.14 | 1.20 (1.10,1.32) | <0.001 |
| Hypertension | 1.36 (1.04,1.78) | 0.026 | 1.09 (0.60,1.99) | 0.78 | 2.21 (1.40,3.50) | 0.001 | 1.55 (0.95,2.53) | 0.08 |
| HDL (10 mg/dl) | 0.88 (0.80,0.97) | 0.014 | 1.02 (0.87,1.20) | 0.76 | 0.96 (0.87,1.07) | 0.48 | 1.01 (0.85,1.19) | 0.95 |
| BMI (kg/m2) | 1.01 (0.99,1.04) | 0.23 | 1.04 (0.98,1.10) | 0.19 | 0.99 (0.97,1.02) | 0.54 | 1.01 (0.96,1.05) | 0.72 |
| Diabetes | 1.65 (1.15,2.36) | 0.006 | 2.60 (1.54,4.40) | <0.001 | 1.66 (1.19,2.32) | 0.003 | 1.43 (0.95,2.16) | 0.09 |
| Current smoking | 1.18 (0.82,1.70) | 0.36 | NA | 0.92 (0.59,1.43) | 0.70 | 0.58 (0.20,1.70) | 0.32 | |
| Family History MI | 1.12 (0.86,1.46) | 0.40 | 1.10 (0.61,1.98) | 0.76 | 1.12 (0.84,1.48) | 0.43 | 1.38 (0.95,2.02) | 0.09 |
| Pre-tx chol | 1.09 (1.07,1.12) | <0.001 | 1.13 (1.08,1.19) | <0.001 | 1.11 (1.08,1.15) | <0.001 | 1.12 (1.09,1.16) | <0.001 |
| MEN | PR (95% CI) | p-value | PR (95% CI) | p-value | PR (95% CI) | p-value | PR (95% CI) | p-value |
| Age (yrs) | 1.05 (0.99,1.12) | 0.12 | 1.23 (1.01,1.50) | 0.037 | 1.09 (0.97,1.22) | 0.16 | 1.15 (1.02,1.30) | 0.023 |
| Hypertension | 2.15 (1.57,2.96) | <0.001 | 1.53 (0.75,3.11) | 0.24 | 2.17 (1.22,3.87) | 0.009 | 1.46 (0.76,2.80) | 0.25 |
| HDL (10 mg/dl) | 1.02 (0.96,1.10) | 0.52 | 0.96 (0.78,1.19) | 0.72 | 0.99 (0.87,1.14) | 0.94 | 1.06 (0.86,1.31) | 0.59 |
| BMI (kg/m2) | 1.02 (0.99,1.04) | 0.19 | 1.09 (1.00,1.17) | 0.040 | 1.03 (0.99,1.08) | 0.13 | 1.03 (0.99,1.07) | 0.20 |
| Diabetes | 0.76 (0.32,1.80) | 0.54 | 1.95 (1.03,3.69) | 0.042 | 1.44 (0.95,2.19) | 0.09 | 1.13 (0.57,2.26) | 0.73 |
| Current smoking | 0.79 (0.50,1.25) | 0.31 | 1.29 (0.39,4.29) | 0.68 | 1.20 (0.70,2.06) | 0.51 | 0.84 (0.35,2.01) | 0.70 |
| Family History MI | 1.30 (1.03,1.62) | 0.025 | 2.05 (0.93,4.54) | 0.08 | 1.25 (0.89,1.75) | 0.20 | 0.94 (0.54,1.63) | 0.83 |
| Pre-tx chol | 1.09 (1.05,1.12) | <0.001 | 1.12 (1.03,1.23) | 0.013 | 1.09 (1.04,1.15) | <0.001 | 1.08 (1.02,1.14) | 0.006 |
PR=prevalence ratio; CI=confidence interval; MI=myocardial infarction; Pre-tx chol=estimated pre-treatment value of cholesterol, with PR expressed per 10mg/dl; Hypertension defined as systolic blood pressure (SBP) over 140 mmHg and/or diastolic blood pressure (DBP) over 90 mmHg
The correlates of anti-hypertensive medication use also vary by race/ethnicity (Table 4). Significant differences by race/ethnicity were found in the associations for body mass index (p<0.001), estimated pre-treatment blood pressures (p<0.001 for systolic, p=0.057 for diastolic), and age (p=0.048). Among African-American participants body mass index was less strongly associated with prevalence than among the other race/ethnic groups. Among African-American participants, the prevalence of anti-hypertensive medication use increased less steeply with increasing estimated pre-treatment systolic blood pressures than for the other race/ethnic groups. In addition the use of anti-hypertensive medications increased with age in both men and women, though this was significantly steeper in men (p=0.023) for each race/ethnic group.
Table 4.
Risk Factors and the Prevalence of Anti-Hypertensive Medication Use by Gender and Race/Ethnicity: The Multi-Ethnic Study of Atherosclerosis, 2000–2002
| White | Chinese-American | African-American | Hispanic | |||||
|---|---|---|---|---|---|---|---|---|
| WOMEN | PR (95% CI) | p-value | PR (95% CI) | p- value |
PR (95% CI) | p-value | PR (95% CI) | p-value |
| Age (yrs) | 1.10 (1.05,1.15) | <0.001 | 1.11 (1.02,1.21) | 0.011 | 1.08 (1.05,1.11) | <0.001 | 1.09 (1.04,1.16) | 0.002 |
| High Cholesterol | 0.90 (0.79,1.03) | 0.14 | 1.27 (0.97,1.67) | 0.09 | 0.99 (0.90,1.10) | 0.89 | 0.97 (0.82,1.15) | 0.73 |
| HDL (10 mg/dl) | 0.97 (0.92,1.02) | 0.26 | 0.93 (0.84,1.03) | 0.15 | 0.98 (0.95,1.02) | 0.26 | 1.02 (0.96,1.09) | 0.55 |
| BMI (kg/m2) | 1.03 (1.02,1.05) | <0.001 | 1.01 (0.98,1.05) | 0.45 | 1.01 (1.00,1.02) | 0.001 | 1.03 (1.01,1.04) | <0.001 |
| Diabetes | 1.36 (1.06,1.74) | 0.015 | 1.29 (0.90,1.85) | 0.17 | 1.38 (1.24,1.53) | <0.001 | 1.49 (1.24,1.80) | <0.001 |
| Current smoking | 0.83 (0.60,1.13) | 0.23 | 0.68 (0.18,2.53) | 0.56 | 0.87 (0.74,1.03) | 0.11 | 0.93 (0.66,1.30) | 0.65 |
| Family History MI | 1.18 (1.03,1.35) | 0.016 | 0.85 (0.56,1.28) | 0.43 | 1.09 (1.00,1.20) | 0.06 | 1.31 (1.11,1.56) | 0.002 |
| Pre-tx SBP* Pre-tx DBP* |
1.08 (1.03,1.14) 1.26 (1.13,1.39) |
0.003 <0.001 |
1.12 (1.01,1.25) 1.20 (0.97,1.48) |
0.026 0.09 |
1.06 (1.02,1.10) 1.15 (1.07,1.23) |
0.001 <0.001 |
1.07 (1.00,1.15) 1.27 (1.11,1.46) |
0.043 <0.001 |
| MEN | PR (95% CI) | p-value | PR (95% CI) |
p- value |
PR (95% CI) | p-value | PR (95% CI) | p-value |
| Age (yrs) | 1.13 (1.08,1.18) | <0.001 | 1.19 (1.07,1.33) | 0.002 | 1.12 (1.08,1.16) | <0.001 | 1.15 (1.08,1.23) | <0.001 |
| High Cholesterol | 1.11 (0.97,1.28) | 0.13 | 1.08 (0.81,1.45) | 0.59 | 1.05 (0.93,1.19) | 0.46 | 1.20 (0.98,1.48) | 0.08 |
| HDL (10 mg/dl) | 1.00 (0.94,1.06) | 0.94 | 1.00 (0.88,1.13) | 0.99 | 0.96 (0.91,1.01) | 0.14 | 0.97 (0.88,1.06) | 0.48 |
| BMI (kg/m2) | 1.03 (1.01,1.05) | 0.002 | 1.04 (0.98,1.10) | 0.26 | 1.01 (0.99,1.02) | 0.44 | 1.03 (1.00,1.05) | 0.026 |
| Diabetes | 1.40 (1.16,1.68) | <0.001 | 1.31 (0.90,1.90) | 0.15 | 1.27 (1.11,1.45) | 0.001 | 1.56 (1.26,1.94) | <0.001 |
| Current smoking | 1.05 (0.83,1.33) | 0.67 | 1.03 (0.59,1.80) | 0.91 | 0.94 (0.78,1.12) | 0.48 | 0.85 (0.61,1.18) | 0.33 |
| Family History MI | 1.07 (0.93,1.23) | 0.33 | 0.82 (0.46,1.45) | 0.58 | 1.16 (1.02,1.32) | 0.026 | 1.00 (0.82,1.24) | 0.97 |
| Pre-tx SBP* Pre-tx DBP* |
1.09 (1.03,1.15) 1.23 (1.09,1.39) |
0.003 0.001 |
1.11 (0.97,1.27) 1.22 (0.93,1.61) |
0.14 0.16 |
1.03 (0.98,1.09) 1.26 (1.13,1.41) |
0.24 <0.001 |
1.06 (0.98,1.16) 1.28 (1.07,1.53) |
0.15 0.007 |
PR=prevalence ratio; CI=confidence interval; MI=myocardial infarction; Pre-tx SBP and DBP are estimated pre-treatment values, with prevalence ratios expressed per 10 mmHg increment; high cholesterol defined as a total cholesterol over 200mg/dl or taking lipid lowering medication.
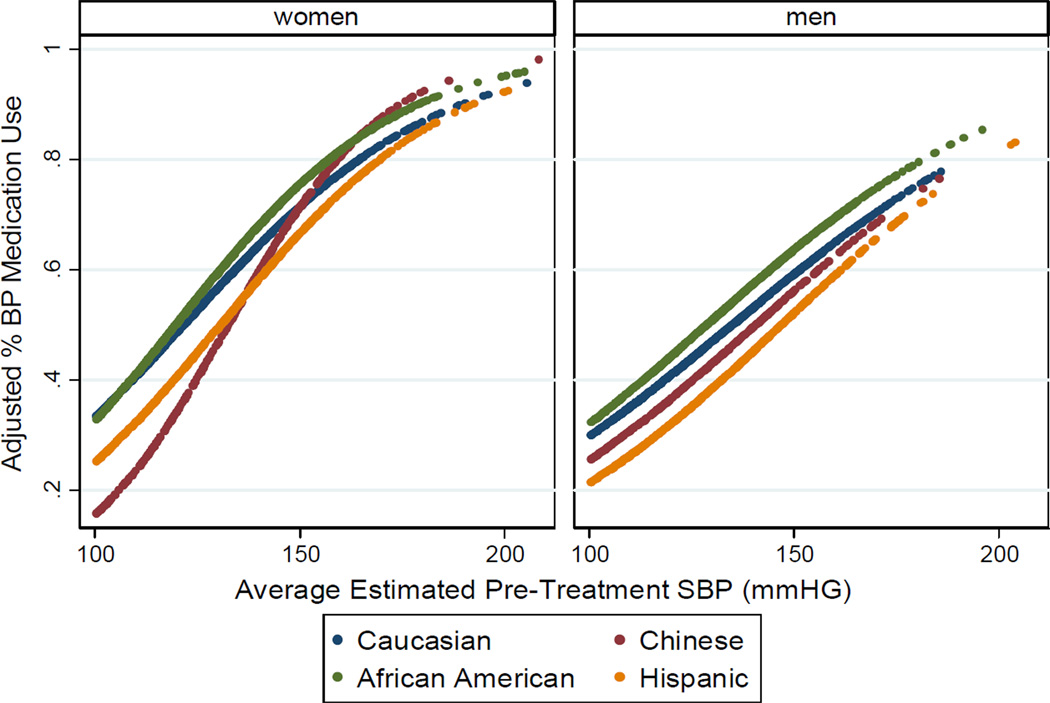
In Figures 1 and 2 we display the prevalence of medication use across pre-treatment biomarker values, adjusted to a common risk factor profile. Once cholesterol levels are in the elevated range (>200 mg/dl) Hispanics are clearly less often on lipid lowering treatment than other race/ethnicities for both men and women. Non-hispanic white men were much more likely to be on treatment than their minority counterparts. For anti-hypertensive medication, African-American men consistently have the highest prevalence of use, Hispanics the lowest. For women, the prevalence increases more sharply with blood pressure than for men, especially for Chinese women. It is important to note that the percentages in the figures represent estimates of what would be observed if all the gender/ethnicity groups had the same risk factor profile, and do not reflect actual rates in the population. The comparisons between the curves are thus a graphical illustration of disparities rather than of observed differences.
Figure 1. Adjusted Prevalence of Lipid Lowering Medication Use by Gender and Race/Ethnicity: Multi-Ethnic Study of Atherosclerosis 2000–2002.
The adjusted prevalence of lipid lowering medication use is displayed as a function of estimated pre-treatment cholesterol for each gender and race/ethnicity. Estimated prevalence is based on a logistic regression model and is adjusted to an average age of 62, HDL of 55 mg/dl, non-smoking, non-hypertensive, non-diabetic population without family history. These are thus estimates of what would be observed if all the gender/ethnicity groups had the same risk factor profile, and do not reflect actual rates in the population.
Figure 2. Adjusted Prevalence of Anti-Hypertensive Medication Use by Gender and Race/Ethnicity: Multi-Ethnic Study of Atherosclerosis 2000–2002.
The adjusted prevalence of anti-hypertensive medication use is displayed as a function of estimated pre-treatment systolic blood pressure for each gender and race/ethnicity. Estimated prevalence is based on a logistic regression model and is adjusted to an average age of 62, HDL of 55 mg/dl, non-smoking, non-dyslipidemic, non-diabetic population without family history. These are thus estimates of what would be observed if all the gender/ethnicity groups had the same risk factor profile, and do not reflect actual rates in the population.
Among the socioeconomic variables, lack of health insurance was by far the most influential for both anti-hypertensive medication use (PR 0.75, 95% CI 0.66–0.87, p<0.001) and lipid lowering medication use (PR 0.14, 95% CI 0.03–0.63, p=0.010). Education was not significant in either model, and income was associated only with lipid lowering medication. As previously described, in MESA results of the various tests including blood pressure and lipids were reported to both the participant’s and their physicians. To assess the extent to which access to regular risk factor evaluation might explain the disparities, we also fit models examining new users of medication by the second follow-up examination (n=517 new users of lipid lowering medication, n=455 new users of anti-hypertensive medication). For anti-hypertensive medication use the differences between genders disappeared, suggesting that lack of regular blood pressure evaluation may be responsible for observed disparities. For new users of lipid lowering medications, the differences between race/ethnic groups persisted, with both African-American and Hispanic participants having significantly lower prevalence of medication use. This suggests that it is not screening for the cholesterol level that is explaining the difference. In this model men also had a higher prevalence of use, in comparison to the baseline model which showed no difference by gender.
Discussion
The results of this study highlight both the methodology used and the epidemiology of disparities in medication use. In terms of the methodology, the estimation of the pre-treatment biomarker values allows better control of confounding by indication, and allows more informative graphical presentation of results compared with standard methods. Ignoring the underlying pre-treatment biomarker values confounds differences in the prevalence of the underlying condition (e.g. high blood pressure or high cholesterol) with disparities in the prevalence of medication use at a given level of the condition. Attempting to control for this using observed on-treatment biomarker values is also problematic since this is conditioning on an effect of the medication itself. As mentioned earlier, another valid approach would have been to model the prevalence of medication use within the subset of participants with hypertension or dyslipidemia. However, even above the threshold for defining hypertension or high cholesterol there may still be large differences in the distribution of blood pressure and cholesterol respectively. This leaves open the possibility of residual confounding within the range of hypertension/dyslipidemia, and does not allow the further exploration (either graphically or in the model) of the slope of the associations with the magnitude of the biomarker. Finally, relying exclusively on a new user analysis may obscure important disparities that are due to access to regular health care and screening. Thus, the methodology described here allows additional insights into disparities from large cohort studies compared to existing approaches.
We did find evidence of some disparities in medication use. In terms of lipid lowering medications, our results indicate that Hispanics and to a lesser extent African-Americans may be undertreated. This seemed to be largely a result of socio-economic factors, and may reflect access to care. Although present for both genders, this disparity was particularly apparent among men. It has been reported that African Americans and Hispanics are much less likely than non-Hispanic white Americans to be screened and treated for lipid abnormalities and other cardiovascular risk factors [5, 14, 15]. In the new user model the racial differences persisted, suggesting that for our population differential knowledge of cholesterol level does not explain the disparity. This again points to socio-economic status and the ability to affordably obtain the treatment as the root of the disparity. In the new user model men also had a higher prevalence of use, in comparison to the baseline model which showed no gender disparity. This may indicate that once men are evaluated for their cholesterol they are more likely to be treated at the same risk factor level, but that outside the study they are not being evaluated as often as women.
With respect to blood pressure lowering medications, Hispanics again consistently had the lowest prevalence of use even at the same risk factor profile. Men were significantly less likely to be on anti-hypertensive medications than women and this was not explained by risk factors or socioeconomic status. These findings are consistent with Cutler et al [17] who reported that women had better hypertension awareness, treatment and control, but that blood pressure trends over time were more favorable in men. Additionally they found that Mexican Americans had the lowest rates of treatment and control. Interestingly, when the new user model was used the differences between race and gender groups disappeared. This suggests that knowledge of high blood pressure (reported to participants and their physicians after each exam) removed the disparity that was apparent at baseline.
There were also some disparities in terms of how risk factors were associated with treatment prevalence (conditional on all the other risk factors). For example, the association of diabetes with lipid lowering medication use varied by gender, despite the fact that guidelines for cholesterol treatment do not differ by gender with respect to diabetes. There was a difference in how body size related to treatment prevalence, whereby among African-American participants body size was not as strongly associated with anti-hypertensive medication use compared to among other races.
It is important to note that the prevalent users would include participants who had previously been treated but did not tolerate the therapy, or did not respond to therapy, and who subsequently discontinued use. Additionally, the participants had to have the medication containers to bring with them to the clinic visit, and hence had to have filled their prescription at some point. Thus the disparities seen at baseline refer more to “use patterns” as opposed to “prescribing patterns”.
In summary, our study suggests that more regular evaluation of blood pressure, for men in particular, could reduce the observed disparities in anti-hypertensive medication use by increasing awareness. Further, it suggests that insurance coverage for lipid lowering medications could improve medication use in vulnerable populations, particularly Hispanics and African Americans. Finally, the methodology described here can be used to validate or expand on these observations in other large cohort studies.
Key Points.
Disparities exist in the treatment of cholesterol and hypertension.
Hispanics were significantly less likely to be on LLM at the same level of risk factors. Men have lower prevalence of anti-hypertensive use than women. Risk factors have differential associations with medication use depending on gender.
Both lipid lowering and anti-hypertensive medication use appear to be strongly influenced by socioeconomic factors, particularly lack of health insurance.
Estimation of disparities is important but challenging in an observational cohort study. Methods described in this paper can provide additional insights.
Acknowledgments
Funding Sources: Analysis and methods development for this project was supported by R01 HL 103729-01A1 from the National Heart, Lung, and Blood Institute. The MESA study was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute.
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
This work has not been presented or published previously. None of the authors have any conflict of interest to report.
References
- 1.Singh V, Deedwania P. Dyslipidemia in Special Populations: Asian Indians, African Americans, and Hispanics. Current Atherosclerosis Reports. 2006;8:32–40. doi: 10.1007/s11883-006-0062-4. [DOI] [PubMed] [Google Scholar]
- 2.Qato DM, Lindau S, Conti RM, Schumm LP, Alexander GC. Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiology and Drug Safety. 2010;19:834–842. doi: 10.1002/pds.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, Psaty BM. Dyslipidemia Prevalence, Treatment, and Control in the Multi-Ethnic Study of Atherosclerosis (MESA): Gender, Ethnicity, and Coronary Artery Calcium. Circulation. 2006;113:647–656. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 4.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. International Journal of Cardiology. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Nelson K, Norris K, Mangione CM. Disparities in the Diagnosis and Pharmacologic Treatment of High Serum Cholesterol by Race and Ethnicity. Archives of Internal Medicine. 2002;162:929–935. doi: 10.1001/archinte.162.8.929. [DOI] [PubMed] [Google Scholar]
- 6.Mann D, Reynolds K, Smith D, Muntner P. Trends in Statin Use and Low-Density Lipoprotein Cholesterol Levels Among US Adults: Impact of the 2001 National Cholesterol Education Program Guidelines. The Annals of Pharmacotherapy. 2008;42:1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 7.O'Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164(12):1313–1318. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- 8.McClelland R, Kronmal R, Haessler J, Blumental R, Goff DJ. Estimation of risk factor associations when the response is influenced by medication use: an imputation approach. Statistics in Medicine. 2008;27(24):5039–5053. doi: 10.1002/sim.3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacobs DR, Kronmal R, Liu K, Clark Nelson J, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. American Journal of Epidemiology. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 10.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry. 1972;18:499–502. [PubMed] [Google Scholar]
- 11.Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine. 1999;18:681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 12.Royston P. Multiple imputation of missing values. The Stata Journal. 2004;4(3):227–241. [Google Scholar]
- 13.Royston P. Multiple imputation of missing values: update of ice. The Stata Journal. 2005;5(4):527–536. [Google Scholar]
- 14.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: Wiley; 1987. [Google Scholar]
- 15.Ferdinand KC. Managing Cardiovascular Risk in Minority Patients. Journal of the National Medication Association. 2005;97:459–466. [PMC free article] [PubMed] [Google Scholar]
- 16.Jha AK, Varosy PD, Kanaya AM, Hunninghake DB, Hlatky MA, Waters DD, Furberg CD, Shlipak MG. Differences in medical care and disease outcomes among black and white women with heart disease. Circulation. 2003;108:1089–1094. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 17.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in Hypertension Prevalence, Awareness, Treatment, and Control Rates in United States Adults Between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]