Abstract
BACKGROUND
The majority (59 to 86%) of hospital-acquired urinary tract infections (UTIs) are catheter-associated urinary tract infections (CAUTI). As of 2008, claims data are used to deny payment for hospital-acquired conditions such as CAUTI and to publicly report hospital performance.
OBJECTIVES
To examine rates of UTIs in adults that are coded in claims data as hospital-acquired and catheter-associated and evaluate how often non-payment for CAUTI lowers hospital payment.
DESIGN
Before-and-after study of all-payer cross-sectional claims data
SETTING
96 nonfederal acute-care Michigan hospitals
PATIENTS
Non-obstetric adults discharged in 2007 (N=757531) and 2009 (N=781343)
MEASUREMENTS
Hospital rates of UTIs (categorized as catheter-associated and/or hospital-acquired), and frequency of reduced payment for hospital-acquired CAUTIs.
RESULTS
Hospitals frequently requested payment for non-catheter-associated UTIs as secondary diagnoses: 10.0% of discharges (95% CI: 9.5 to 10.5) in 2007, 10.3% (CI: 9.8 to 10.9) in 2009. Hospital rates of CAUTI were very low: 0.09% (CI: 0.06 to 0.12) in 2007; 0.14% (CI: 0.11 to 0.17) in 2009. In 2009, 2.6% (CI: 1.6 to 3.6) of hospital-acquired UTIs were described as catheter-associated. Non-payment for hospital-acquired CAUTIs lowered payment for 25 of 781343 (0.003%) hospitalizations in 2009.
LIMITATIONS
Data are from only one state and involved only one year before-and-after non-payment for complications. Hospital prevention practices were not examined.
CONCLUSIONS
CAUTI rates determined by claims data appear inaccurate and are much lower than expected from epidemiologic surveillance data. The financial impact of current non-payment policy for hospital-acquired CAUTI is low. Claims data is currently not a valid dataset for comparing hospital-acquired CAUTI rates for the purpose of public reporting or imposing financial incentives or penalties.
Introduction
Since October 2008, the Centers for Medicare and Medicaid Services (CMS) no longer pay hospitals to treat specific “reasonably preventable” hospital-acquired complications as part of a value-based purchasing plan to encourage hospitals to improve patient safety and also to reduce Medicare spending (1–3). Administrative discharge claims data (submitted by hospitals to request payment) are now used to deny payment for these complications, and to publicly report and compare hospitals by complication rates.
CMS rules are complex for identifying these complications in administrative discharge data (4, 5). For example, for the first complication chosen for non-payment (hospital-acquired catheter-associated urinary tract infection, CAUTI), 3 codes must each be listed accurately to trigger non-payment for the urinary tract infection: 1) a diagnosis code for urinary tract infection (UTI); 2) the code for urinary catheter-associated inflammation or infection (996.64); and 3) both the UTI and the catheter-association codes need to be labeled as not present-on-admission (indicating the CAUTI was hospital-acquired). Even if a hospital-acquired condition is identified, hospitals can continue to receive extra payment if other patient comorbidities (such as heart failure) are listed as diagnoses (6). Accordingly, how hospitals describe CAUTIs and comorbidities using diagnosis codes in claims data will influence the financial impact of non-payment for hospitals and payers. Public reporting of hospital-acquired CAUTI rates on HospitalCompare also follows similar coding conventions as the rules for payment. Case examples of how a UTI diagnosis impacts hospital payment and public reporting are provided in Appendix Text 1 and Appendix Table 1.
Surveillance data suggest that there are 4.5 hospital-acquired infections per 100 admissions and that 32% of these have a urinary tract source (7). The majority of hospital-acquired UTIs (59 to 86%) are catheter-associated (8–10). Based on prior work (4), we hypothesized, however, rare application of the catheter code in claims data to describe UTIs as catheter-associated. We designed a statewide study to investigate hospital rates of non-catheter associated UTIs (ncUTIs) and CAUTIs before-and-after implementation of non-payment for hospital-acquired CAUTI from claims data and also assessed the financial impact of non-payment for hospital-acquired CAUTIs.
Methods
Study Design
We conducted a retrospective before-and-after study using administrative data for all adult discharges from acute-care hospitals in the State of Michigan in 2007 and 2009 using the Healthcare Cost and Utilization Project State Inpatient Dataset, sponsored by the Agency for Healthcare Research and Quality (11). This claims dataset contained all data from inpatient discharge abstracts generated by hospitals to request payment for each discharge in 2007 and 2009. Data were translated into a uniform format to facilitate comparisons and protect patient identity. The claims data were generated by hospital coders who reviewed medical records to guide selection of diagnosis, procedure, and demographic codes to describe each hospitalization, in accordance with federal guidelines (12). Hospitals submitted Michigan discharge data first to the Michigan Health & Hospital Association. The Association decided which data elements could be released publicly through the Healthcare Cost and Utilization Project Central Distributor. There were few missing data elements in the released information (Figure 1). This study received approval from the human subjects review board at the University of Michigan.
Figure 1. Data Inclusion and Exclusion Criteria.
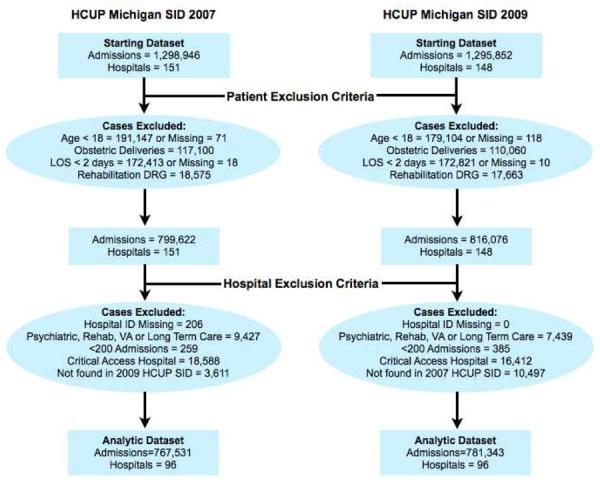
Abbreviations: HCUP Healthcare Cost and Utilization Project; SID - State Inpatient Dataset; LOS - Length of Stay: DRG - Diagnosis-related Group; Rehab - Rehabilition: VA - Veterans Affairs.
Study Population
Figure 1 depicts application of patient and hospital inclusion and exclusion criteria that were used to construct the analytic data set. Our study population included non-obstetric adult patients (≥18 years old) who had a hospital length-of-stay greater than 1 day. We performed analyses specific to Medicare patients and analyses for an all-payer population as the policy that had been initiated only for Medicare has expanded to other payers including state Medicaid programs (13) and BCBS nationwide (14).
We excluded hospitals not affected by the Hospital-Acquired Conditions Initiative (HACI), such as long-term care, rehabilitation, psychiatric facilities, critical access hospitals, Veterans hospitals, and children's hospitals. When comparing hospital rates of ncUTIs and CAUTIs, we included only hospitals with data available in both 2007 and 2009 and with ≥200 adult discharges. We identified safety-net hospitals as those with a Medicaid caseload greater than or equal to one standard deviation above the state average (15–19).
UTI Identification as Catheter-associated, and/or Hospital-acquired
Non-catheter-associated urinary tract infections (ncUTIs) were identified by having at least one of 10 UTI diagnosis codes (Appendix Table 2), without an additional catheter-association code (996.64). Catheter-associated UTIs (CAUTIs) were identified by the code for urinary catheter-associated inflammation or infection (996.64), with or without an additional UTI code in accordance with the Medicare HACI policy.
The present-on-admission variable to identify a diagnosis as present-on-admission versus hospital-acquired (detailed in Appendix Table 3) was mandated nationally for discharges after 1 October 2007. Thus, we were able to identify ncUTIs and CAUTIs as hospital-acquired or present-on-admission in the post-policy 2009 dataset. Hospital-acquired ncUTIs and CAUTIs were identified in the 2009 dataset with the present-on-admission indicator coded as N (not present on admission), or U (could not be determined due to insufficient documentation, which also results in non-payment). To identify hospital-acquired CAUTIs, the catheter code 996.64 also had its associated present-on-admission indicator coded as N or U.
Assessing Hospital Rates of ncUTIs and CAUTIs
We assessed and compared each hospital's rates of ncUTIs and CAUTIs as secondary diagnoses in both 2007 and 2009, and as hospital-acquired or present-on-admission conditions in 2009. A hospital's rates for ncUTIs and CAUTIs were calculated as the percentage of each hospital's adult discharges with these diagnoses. An analysis (in Appendix Text 2 and Appendix Table 4) was also performed regarding how many hospital-acquired CAUTIs were noted in the first 8 secondary diagnoses, as is the current standard for public reporting (6).
Assessing Impact of CAUTIs on hospital payment
Using the post-policy 2009 dataset, we assessed how often non-payment for hospital-acquired CAUTIs impacted the payment received by the hospital. This analysis was performed using the 3M MS Grouper Software that applies the diagnosis-related group (DRG) that determines hospital payment for each hospitalization record, using an algorithm that incorporates diagnosis and procedure codes, and patient characteristics. First we obtained the DRG assigned at baseline using all the secondary diagnoses in the 2009 dataset, with minor modifications to assure the same DRG version was applied to all discharges in the year. Then we modified hospital-acquired CAUTI cases (which could not increase payment) to be coded as present-on-admission CAUTI cases (which may lead to a higher paying DRG), and then used the software to reassign the DRG. We identified hospitalizations where non-payment for the hospital-acquired CAUTI impacted payment by a change in DRG.
Statistical Analyses
Descriptive statistics and 95% confidence intervals are reported. A paired t-test was used to compare pre-policy (2007) with post-policy (2009) hospital UTI rates. Analyses were conducted in Stata/MP 11.2 (Stata Corp., College Station, TX).
Role of Funding Source
This study was funded by the Blue Cross Blue Shield of Michigan Foundation, which provided some recommendations on the study design as part of the grant's review, but was not involved in the conduct, interpretation or reporting of the results.
Results
Cohort Characteristics
There were 767,531 adult discharges at 96 Michigan hospitals in 2007 and 781,343 discharges in these same hospitals in 2009 (Figure 1). The Table compares hospital-level rates and characteristics for discharges with ncUTI and CAUTI diagnoses.
Hospital Rates of Catheter-Associated and/or Hospital-Acquired UTIs
All 96 hospitals requested payment for secondary-diagnosis non-catheter-associated UTIs. The rate for this diagnosis (i.e., the proportion of the hospital's adult discharges with the indicated diagnosis) ranged from 5.2 to 17.1% (mean: 10.0; CI: 9.5, 10.5) of each hospital's discharges in 2007 and 5.0 to 20.2% (mean: 10.3; CI: 9.8, 10.9) of the discharges in 2009. Hospital rates of secondary diagnosis CAUTIs ranged from 0 to 1.10% (mean: 0.09; CI: 0.06, 0.12) of discharges in 2007, and 0 to 0.95% (mean: 0.14; CI: 0.11, 0.17) in 2009.
Figure 2 (top) illustrates how individual hospital rates of ncUTIs (gray bars) and CAUTIs (black bars) compared for state of Michigan hospitals in 2009. Of note, there were 18 hospitals (19%) in 2007 and 8 (8%) in 2009 that did not use the catheter-association code for any hospitalization record (including the principal diagnosis); these hospitals had a similar proportion of discharges (8.6% in 2007, 8.7% in 2009) with a secondary diagnosis of non-catheter associated UTI. The majority (57%) of hospitals in 2007 and 48% in 2009 requested payment for 5 or fewer CAUTIs as secondary diagnoses.
Figure 2. Michigan hospital ratesa In 2009 (top) and change In rates from 2007 to 2009 (bottom).
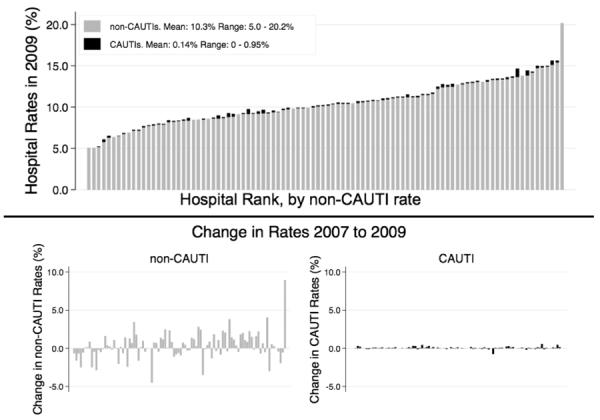
non-CAUTI: Non-catheter-associated Urinary Tract Infection; CAUTI: Cathater-associated Urinary Trad Infection.
aHospital's rate of diagnosis calculated as the percentage of each hospital's adult discharges with the indicated diagnosis.
Figure 2 (bottom) illustrates the changes for individual hospital rates of ncUTIs and CAUTIs, from 2007 (pre-policy) to 2009 (post-policy). The average hospital difference in ncUTI rates pre- and post-policy was 0.3% (CI: −0.01, 0.7). Hospital rates of CAUTI as a secondary diagnosis increased by only 0.05% on average (CI: 0.02, 0.08). Compared with 85 non-safety-net hospitals (Appendix Table 5), the 11 safety-net hospitals had similar rates of ncUTIs and CAUTIs in 2009.
In 2009, most ncUTIs were described as present-on-admission (see Table). The mean rate across hospitals for present-on-admission ncUTI diagnosis was 8.5% (CI: 7.9 to 9.1) while only 1.3% (CI: 1.1 to 1.5) of discharges were described as hospital-acquired ncUTIs. Of note, hospitals did not provide a valid code to identify a UTI as present-on-admission or not for 0.5% of the diagnoses (CI: 0.1–0.9).
Hospital-acquired CAUTIs were uncommon in claims data; the mean rate of hospital discharges with this diagnosis was 0.03% (CI: 0.02, 0.04). Forty-five hospitals (47%) coded zero Medicare hospitalizations with a diagnosis of hospital-acquired catheter-associated UTI. Of all hospital-acquired UTIs (including ncUTIs and CAUTIs), a minority (mean 2.6%, CI 1.6, 3.6) were described as CAUTIs.
The Appendix Figure illustrates how the proportion of ncUTIs (top) and CAUTIs (bottom) identified as hospital-acquired or present-on-admission varied by each hospital. Focusing on hospital-acquired events only, Figure 3 illustrates hospital rates of hospital-acquired ncUTIs (gray bars) and hospital-acquired CAUTIs (black bars), in order of CAUTI rates. Hospital-acquired CAUTI rates in 2009 ranged from 0% of discharges in 39 (41%) hospitals to 0.34% of discharges, with hospital rates of 0%, 0.02%, and 0.04% of discharges identifying the second, third and fourth quartiles of hospital rates. Depending on the number of annual discharges, a single case of hospital-acquired CAUTI could move a hospital from the lowest (i.e., best) quartile of infection rates to the second, third or fourth quartile of CAUTI rates. Comparing the hospital-acquired rates for ncUTIs (gray bars) and CAUTIs (black bars) of Figure 3 illustrates that hospital rates of hospital-acquired ncUTIs have little correlation with rates of hospital-acquired CAUTIs.
Figure 3. Hospital ratesa of hospital-acquired catheter-associated UTIs and hospital-acquired non-catheter-associated UTIs in 2009.
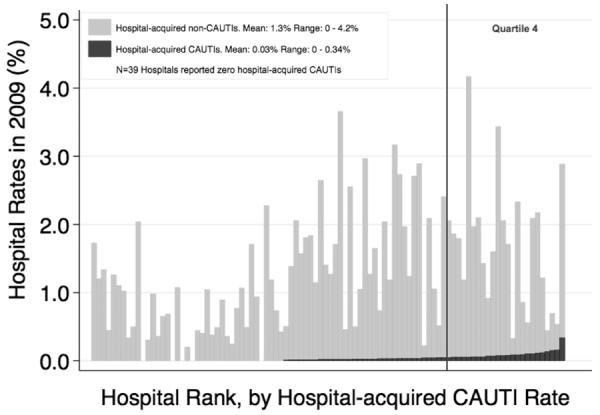
non-CAUTI: Non-catheter-associated Urinary Tract Infection; CAUTI: Catheter-associated Urinary Tract Infection.
aHospital's rate of diagnosis calculated as the percentage of each hospital's adult discharges with the indicated diagnosis.
Impact of CAUTIs and UTIs on hospital payment
In 2009, 321 hospitalizations listed a CAUTI as hospital-acquired. Hospitals listed a mean of 18.7 secondary diagnoses for patients discharged with a hospital-acquired CAUTI (Table). Accounting for secondary diagnoses that generate higher payment, non-payment for hospital-acquired CAUTI impacted hospital payment (i.e., lowered hospital payment) for 25 of 781,343 (0.003%) hospitalizations. Twenty-two of these instances occurred in non-safety-net hospitals (7.4% of 296 cases of hospital-acquired CAUTI) and 3 occurred in safety-net hospitals (12.0% of 25 cases of hospital-acquired CAUTI).
We estimated the dollar impact of non-payment for these 25 hospitalizations with hospital-acquired CAUTI using an average base Medicare payment of $8700 that was in place at the University of Michigan in 2009. Based on these estimates, the hospital would have lost $132,675 as a result of non-payment of hospital-acquired CAUTI. This amount is 0.06% of annual payments (of the total $215,000,000 by the Acute Inpatient Prospective Payment System). As the base payment for the University of Michigan may be higher than most community hospitals, our estimates represent an upper limit of potential payment loss for hospital-acquired CAUTI events.
We also explored how often payment for any type of UTI as a secondary diagnosis impacted hospital payment, given other patient comorbidities, by replacing all the UTI diagnosis codes with a diagnosis code that does not count as either a comorbidity or complication. In 2009, modification of the UTI secondary diagnosis codes to a non-paying diagnosis code resulted in a lower-paying DRG for 7,632 cases (9.1% of 84,290 UTI and CAUTI total, 1% of all hospitalizations); 642 of these occurred in safety-net hospitals (9.3% of 6,937) and 6,990 occurred in non-safety-net hospitals (9.0% of 77,353).
Discussion
Hospital-acquired CAUTI was the first condition chosen for non-payment due to its anticipated impact on large numbers of hospitalizations. Epidemiologic surveillance studies suggest urinary tract sources are the most common of all nosocomial infections (20, 21) and medical record reviews demonstrate frequent urinary catheter use among Medicare patients (1). We showed, however, that the current hospital discharge dataset rarely identifies catheter-associated UTIs. The impact of a non-payment policy based on these data is small. The accuracy of reporting from the dataset is suspect. Moreover, we conclude that the current hospital discharge dataset is not an accurate or valid dataset for comparing hospital-acquired CAUTI rates for the purpose of public reporting or imposing financial incentives or penalties.
Although diagnosis codes for UTIs are commonly listed as secondary diagnoses (~10% of discharges), very few UTIs are identified in the claims data as catheter-associated UTIs by the addition of the 996.64 code. In contrast to epidemiologic studies that report the majority (22) (59–86% (8, 9, 23)) of hospital-acquired UTIs are catheter-associated, only 2.6% of all hospital-acquired UTIs were described in the claims data as catheter-associated. Rates of CAUTIs from claims data were also much lower than anticipated for Medicare patients who have high rates of urinary catheter use during hospitalization (40%, according to the Medicare Patient Safety Monitoring System (1)). CAUTIs are very common among catheterized patients. Studies show a risk of 3 to 10% for developing bacteriuria per day of catheterization (22, 24, 25) and that 9.9% of patients with indwelling catheters develop CAUTIs (8).
Medical record reviews and details of hospital coder instructions (12) help explain why so few UTIs are described as catheter-associated in administrative discharge claims data. Medical record reviews (4) have supported that a large proportion of UTIs (46%) are catheter-associated (including 35% of UTIs being hospital-acquired CAUTIs). Yet, urinary catheter use is most often evident only in nursing notes, which unlike physician notes, cannot be used by hospital coders to generate diagnoses for billing (12). In order for the hospital coder to identify the UTI as a catheter-associated UTI, it must be clearly identified as a catheter-associated UTI in the notes of a provider (e.g., physician, physician-assistant, or nurse practitioner). If a hospital coder suspects the UTI occurred after admission, the hospital coder must contact the provider for clarification of the status upon admission if not clear from the provider's notes. Thus, it is not surprising that very few hospital-acquired CAUTI events are documented in the claims data used for triggering non-payment and public reporting.
Another weakness of using claims data for public reporting involves the fact that billing coders are not trained or expected to collect and report diagnoses in a manner equivalent to generating a disease surveillance dataset. Coders are trained to code all diagnoses required for CMS reporting guidelines and are careful to report diagnoses that impact a patient's risk of mortality and severity of illness. Currently, there is no CMS reporting requirement for coders to list all hospital-acquired conditions in claims data. Because UTIs may not clearly impact a patient's mortality or severity of illness (particularly in comparison to other diagnoses), UTI diagnoses may not always be listed in claims data. Although several states have mandatory reporting requirements for certain hospital-acquired conditions such as infections, this reporting is usually done in separate databases than the claims dataset currently used for triggering non-payment and public reporting.
The decrease in CAUTI events intended by the policy was not seen, comparing CAUTI events in Michigan from 2007 to 2009. In fact, there was a small but clinically insignificant increase in both ncUTIs and CAUTIs as secondary diagnoses. Increases in ncUTI and CAUTI rates in the claims dataset could occur as an unintended consequence of the non-payment policy, because hospitals do have an incentive to document and describe all conditions that are “present-on-admission” to avoid potential non-payment for this condition if described later in the hospitalization.
There was limited financial impact for non-payment of hospital-acquired CAUTI. Even when we assessed a “worst case scenario” of nonpayment for all UTI diagnoses, only 1% of all hospitalizations would have had reduced hospital payment. Simply put, although UTI is a common diagnosis, it is not a large target for financial savings by non-payment given the other comorbidities of patients with UTIs.
Our assessment of impact of non-payment for hospital-acquired CAUTI is limited to analysis by claims data in Michigan in the first year after implementation of the Hospital-acquired Conditions Initiative. We acknowledge that such policies can have important clinical impacts not described in claims data, such as focusing hospitals' infection prevention efforts for prevention of CAUTI (26). Efforts at decreasing inappropriate urinary catheter use can also decrease other non-infection related risks, such as catheter-associated discomfort (27) and immobility risks (i.e., thromboembolic disease and pressure ulcers (28)). It also may take more than 1 year to see an impact on CAUTI rates and coding practices regarding UTIs. To assess generalizability of CAUTI rates from Michigan claims data to other states (given concerns that the Keystone CAUTI Bladder Bundle Initiative in Michigan could be responsible for low CAUTI rates in this state), we have studied the urinary catheter-association code use in claims data nationwide and found it to be similarly very low (4).
In conclusion, the financial impact of non-payment for hospital-acquired CAUTI is low due to rare use of the catheter code and other comorbidities that generate similar payment. However, the most important finding of this study is that one of the most common nosocomial infections – hospital-acquired CAUTI – is only rarely documented in the claims dataset chosen for implementing non-payment and public reporting of hospital-acquired conditions. In fact, using claims data for comparing hospitals has potential for unfair hospital penalty because hospitals with higher CAUTI rates in claims data may simply do a better job documenting catheter use and describing UTIs correctly as catheter-associated or hospital-acquired events in provider notes used by hospital coders to generate claims data. By 2015, rates of hospital-acquired events will be used to compare hospital performance nationwide to reduce payment for all Medicare hospitalizations for hospitals within the worst quartile of performance (29). Thus, the time has come to either improve the procedures for reporting hospital-acquired events in the claims dataset to increase accuracy, or to abandon claims data for this purpose and change to datasets with more rigorous and standardized assessment regarding nosocomial events for comparing hospitals, such as surveillance data submitted to the National Healthcare Safety Network.
Acknowledgments
We appreciate the insight provided by Gwendolyn Blackford, BS, RHIA, regarding processes used and regulations followed by hospital coders while assigning diagnosis codes. We are appreciative to Jack Hughes, MD, for his helpful suggestions, and to 3M for making the MS Grouper Software available to assess changes in hospital payment. We also thank Andrew Hickner, MSI, for providing assistance with references and manuscript editing. We thank Casey Crimmins, CPA, BGS, with the University of Michigan Department of Finance for providing crucial information to calculate the example of financial impact for the University of Michigan.
Financial Support: The study was funded by a generous grant from the Blue Cross Blue Shield of Michigan Foundation. Some of the authors have also received support from the Agency for Healthcare Research and Quality (Award 1R010HS018344-01A1 to L.M., Award 1K08-HS019767-01, to J.M.) and the National Institute of Diabetes and Digestive and Kidney Diseases (Award R21-DK078717, to S.S.), and the National Institute of Nursing Research (Award R01-NR010700, to S.S.). J.M. is also a recipient of the National Institutes of Health Clinical Loan Repayment Program for 2009–2012.
Disclosures/Funding: Blue Cross Blue Shield Foundation of Michigan
Appendix Text 1. How Coding of Hospital-acquired Complications Impacts Hospital Payment and Public Reporting
To illustrate how coding of hospital-acquired complications impacts hospital payment and public reporting (online by HospitalCompare.org), consider a patient admitted for pneumonia with comorbid heart failure who developed a hospital-acquired catheter-associated UTI during admission. In Appendix Table 1, we outline 5 potential ways this hospitalization could be described using diagnosis codes in the claims data used to obtain hospital payment and now also used to publicly report hospital rates of certain hospital-acquired conditions (such as hospital-acquired CAUTI) online using HospitalCompare.
In scenario A, a diagnosis of pneumonia is listed, but no additional diagnoses are listed. The hospital receives payment for “Simple Pneumonia & Pleurisy without comorbidity or complications” (DRG 195), and this record would not be recognized for having a case of hospital-acquired CAUTI for public reporting because neither the UTI code nor catheter-association code were listed.
In scenarios B and C, the UTI code is listed as a secondary diagnosis without a catheter-association code, and regardless of whether the UTI is described as hospital-acquired (scenario B) or incorrectly as present-on-admit (scenario C), the UTI counts as a condition that leads to a higher paying DRG (194: Pneumonia with comorbidity or complication), which yields more than $2000 in additional hospital payment. There would also be no public reporting of a hospital-acquired condition from this hospitalization because the catheter-association code was not employed.
In scenario D, because both the UTI and catheter-association codes are listed and described as hospital-acquired, the coding criteria have been met for describing a hospital-acquired CAUTI. Therefore, neither code count towards a higher-paying DRG; thus, the hospital receives the same payment as though zero secondary diagnoses were listed. Also, this record would be recognized as containing a hospital-acquired condition for public reporting.
Yet, in scenario E, in addition to listing both the hospital-acquired UTI and catheter-association codes, the hospital coder described the patient's comorbid heart failure with an additional secondary diagnosis code. Therefore, even though the UTI and catheter association code were recognized as complications and did not count as payment-increasing comorbidities (and were recognized as a complication for public reporting), the heart failure code counts toward the higher-paying DRG yielding higher hospital payment.
Appendix Figure 1. Hospital ratesa of non-catheter-associated UTIs and catheter-associated UTIs In 2009 as hospital-acquired and present-on-admission events.
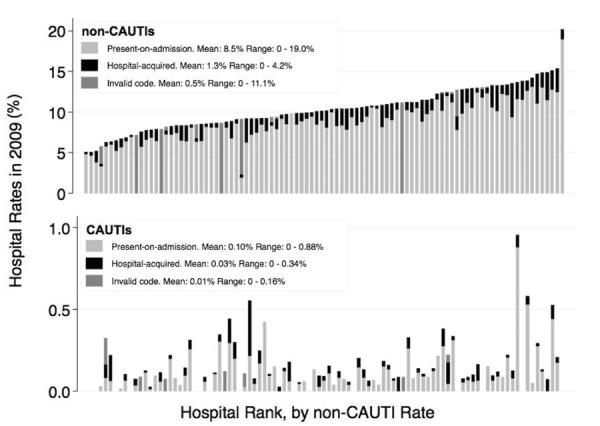
Four Michigan hospitals listed invalid POA codes for all diagnoses and all hospitalizations in the 2009 HCUP-ID dataset (black bars). Because an invalid POA code generates an error, invalid codes would be corrected by hospitals prior to final submission to payers.
UTI: Urinary Tract Infection; non-CAUTI: Non-catheter-associated Urinary Tract Infection; CAUTI: Catheter-associated Urinary Trad Infecton.
aHospital's rate of diagnosis calculated as the percentage of each hospital's adult discharges with the indicated diagnosis.
Appendix Table 1.
How Coding of Hospital-acquired Complications Impacts Hospital Payment and Public Reporting
| Coding Scenario |
Secondary diagnosis ICD-9-CMs listed in discharge claims data, in addition to principal diagnosis 481 “pneumococcal pneumonia” |
Status of diagnosis at admission (as coded with POA indicator variable) |
Hospital Paymenta |
Would a hospital-acquired complication be publicly reported from this record? |
|---|---|---|---|---|
| A | No secondary diagnoses listed | Not Applicable | $6365 | No |
| B | Urinary tract infection (599.0) | Hospital-acquired | $8749 | No |
| C | Urinary tract infection (599.0) | Present-on-Admission | $8749 | No |
| D | Urinary tract infection (599.0) | Hospital-Acquired | $6365 | Yes |
| Infection and inflammatory reaction due to indwelling urinary catheter (996.64) |
Hospital-Acquired | |||
| E | Urinary tract infection (599.0) | Hospital-Acquired | $8749 | Yes |
| Infection and inflammatory reaction due to indwelling urinary catheter (996.64) |
Hospital-Acquired | |||
| Systolic Heart failure (428.22) | Present-on-Admission |
Payments are calculated assuming base rate of $8700, the base rate for admissions with a cost weight of 1.0 to the University of Michigan in 2009.
Appendix Table 2.
ICD-9-CM Diagnosis Codes Used to Identify Urinary Tract Infections (1–3) ICD-9-CM diagnosis codes chosen to identify urinary tract infections for non-payment, when combined with the catheter-association code 996.64 and listed as “not present-on-admission.”
| Code | Description |
|---|---|
| 112.2 | Candidiasis of other urogenital site |
| 590.10 | Acute pyelonephritis, without lesion of renal medullary necrosis |
| 590.11 | Acute pyelonephritis, with lesion of renal medullary necrosis |
| 590.2 | Renal and perinephric abscess |
| 590.3 | Pyeloureteritis cystica |
| 590.80 | Pyelonephritis, unspecified |
| 590.81 | Pyelitis or pyelonephritis in diseases classified elsewhere |
| 595.0 | Acute cystitis |
| 597.0 | Urethral abscess |
| 599.0 | Urinary tract infection, site not specified |
Note: Cases of CAUTIs as the primary reason for admission were identified by having the catheter code (ICD-9-CM: 996.64) listed as the first diagnosis, or having a UTI code listed as the first diagnosis and a catheter code listed among the secondary diagnoses. Cases of UTI as a secondary diagnosis (meaning not the primary reason for admission) were identified with a secondary diagnosis UTI code without the catheter code. Secondary diagnosis catheter-associated UTIs were identified by the catheter code without a UTI ICD-9-CM code as principal diagnosis.
Source: International Classification of Diseases, Ninth Revision, Clinical Modification Codes
Appendix Table 3.
Use of Present-on-admission (POA) Indicator to Identify Hospital-acquired Conditions
| POA indicator coding |
Meaning of this code | Payment decision by CMS for conditions listed with this POA status |
|---|---|---|
| Y | Diagnosis was present at time of inpatient admission. | |
| W | Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. |
CMS will pay the CC/MCC DRG for those selected HACs that are coded as Y or W for the POA Indicator. |
| N | Diagnosis was not present at time of inpatient admission. | |
| U | Documentation insufficient to determine if the condition was present at the time of inpatient admission. |
CMS will not pay the CC/MCC DRG for those selected HACs that are coded as N or U for the POA Indicator. |
| 1 | This is listed for certain diagnoses for which hospitals are not required to list the present-on-admission status. |
Exempt from POA reporting, does not alter Medicare payment. |
Note: Details regarding POA coding transitions and edits were accounted for during the analysis, such as how exempt coding was handled each year for Michigan. Invalid coding for UTIs included missing, exempt, and any other coded value beyond the accepted valid codes of N, Y, W, or U.
Appendix Text 2. Do the First 8 Secondary Diagnoses Capture Most of the Hospital-acquired CAUTI Events?
Current public reporting of hospital-acquired CAUTI rates for U.S. hospitals on HospitalCompare.org only utilizes data from the first 8 secondary diagnoses that are submitted to CMS for payment. This practice is anticipated to be expanded in 2012 (4) to include data from 25 secondary diagnoses. To assess the difference of using only the first 8 compared to all secondary diagnoses for identifying hospital-acquired CAUTI events, we compared hospital-acquired CAUTI event numbers using the first 8 secondary diagnoses versus from all 29 secondary diagnoses for Michigan hospitalizations. Although hospital-acquired CAUTI events were rarely coded in either the first 8 or all 29 secondary diagnoses, the first 8 secondary diagnoses only captured 180 (56%) of all (321) hospital-acquired CAUTI events in the state of Michigan in 2009 for an all payer population, and only 118 (55%) hospital-acquired CAUTI events for Medicare patients (Appendix Table 4).
Appendix Table 4.
Do the First 8 Secondary Diagnoses Capture Most of the Hospital-acquired CAUTI Events?
| Michigan hospitalizations in 2009 with a hospital-acquired CAUTIa |
||
|---|---|---|
| First 8 secondary diagnoses (Diagnoses 2–9) |
All secondary diagnoses (Diagnoses 2–30) |
|
| All Payer Hospitalizations N(%) | 180 (56.1) | 321 (100.0) |
| Medicareb Hospitalizations N(%) | 118 (54.9) | 215 (100.0) |
Abbreviations: CAUTI - catheter-associated Urinary Tract Infection,
Source: 2009 Michigan HCUP State Inpatient Dataset.
Medicare defined as primary or secondary payer is Medicare.
Appendix Table 5.
2009 Hospital Rates of UTI by Category for Safety-net Hospitals Compared to Non-safety-net Hospitalsa
| Safety-net Hospitals | Non-safety-net Hospitals | |
|---|---|---|
| Hospital N (%) | 11 (11.5) | 85 (88.5) |
| Hospitalization N (%) | 68,182 (9.6) | 713,161 (91.3) |
| Urinary Tract Infection Category | N (%) | Mean Hosp. Rate (95% CI), % |
N (%) | Mean Hosp. Rate (95% CI), % |
|---|---|---|---|---|
| Non-catheter-associated UTIs | 6,848 (10.0) | 9.4 (7.6, 11.1) | 76,147 (10.7) | 10.5 (9.9, 11.0) |
| Catheter-associated UTIs | 89 (0.10) | 0.10 (0.03, 0.17) | 1,206 (0.2) | 0.15 (0.11, 0.18) |
| Hospital-acquired non-catheter-associated UTIs | 878 (1.3) | 0.9 (0.5, 1.4) | 12,643 (1.8) | 1.4 (1.2, 1.6) |
| Hospital-acquired catheter-associated UTIs | 25 (0.04) | 0.02(0.001, 0.05) | 296 (0.04) | 0.04 (0.03, 0.05) |
Source: 2009 Michigan HCUP State Inpatient Dataset.
References
- 1.Medicare program; proposed changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates; proposed rules. Fed Regist. 2008;73(84):23547–62. [Google Scholar]
- 2.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Fed Regist. 2008;73(161):48473–91. [PubMed] [Google Scholar]
- 3.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2008 rates. Fed Regist. 2007;72(162):47129–8175. [PubMed] [Google Scholar]
- 4.Chan S, Halim S, Rupp M, Wrobel M. CMS's experience in Publicly Reporting Hospital Acquired Conditions. AcademyHealth; Seattle, WA: Jun 12, 2011. [Google Scholar]
Footnotes
- Society of General Internal Medicine, Annual Meeting, 2010.
- AcademyHealth, Annual Research Meeting, 2010.
References
- 1.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2008 rates. Fed Regist. 2007;72(162):47129–8175. [PubMed] [Google Scholar]
- 2.Medicare program; proposed changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates; proposed rules. Fed Regist. 2008;73(84):23547–62. [Google Scholar]
- 3.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Fed Regist. 2008;73(161):48473–91. [PubMed] [Google Scholar]
- 4.Meddings J, Saint S, McMahon LF., Jr Hospital-acquired catheter-associated urinary tract infection: documentation and coding issues may reduce financial impact of Medicare's new payment policy. Infect Control Hosp Epidemiol. 2010;31(6):627–33. doi: 10.1086/652523. [DOI] [PubMed] [Google Scholar]
- 5.Saint S, Meddings JA, Calfee D, Kowalski CP, Krein SL. Catheter-associated urinary tract infection and the Medicare rule changes. Ann Intern Med. 2009;150(12):877–84. doi: 10.7326/0003-4819-150-12-200906160-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McNair PD, Luft HS, Bindman AB. Medicare's policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood) 2009;28(5):1485–93. doi: 10.1377/hlthaff.28.5.1485. [DOI] [PubMed] [Google Scholar]
- 7.Klevens RM, Edwards JR, Richards CL, Jr., Horan TC, Gaynes RP, Pollock DA, et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122(2):160–6. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haley R, Hooton T, Culver D, Stanley R, Emori TG, Hardison CD, et al. Nosocomial Infections in U.S. Hospitals, 1975-1976: estimated frequency by selected characteristics of patients. Am J Med. 1981;70:947–59. doi: 10.1016/0002-9343(81)90561-1. [DOI] [PubMed] [Google Scholar]
- 9.Krieger J, Kaiser D, Wenzel R. Urinary tract etiology of bloodstream infections in hospitalized patients. J Infect Dis. 1983;148(1):57–62. doi: 10.1093/infdis/148.1.57. [DOI] [PubMed] [Google Scholar]
- 10.Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–63. doi: 10.1086/650482. [DOI] [PubMed] [Google Scholar]
- 11.Healthcare Cost and Utilization Project, State Inpatient Datset for Michigan. Agency for Healthcare Research and Quality; Rockville, MD: [Accessed May 30, 2012]. http://www.hcupus.ahrq.gov/sidoverview.jsp. [Google Scholar]
- 12.ICD-9-CM Official Guidelines for Coding and Reporting. Centers for Medicare and Medicaid Services (CMS) and the National Center for Health Statistics (NCHS); [Accessed May 1, 2012]. Effective October 1, 2009 http://www.cdc.gov/nchs/data/icd9/icdguide09.pdf. [Google Scholar]
- 13.Medicaid program; payment adjustment for provider-preventable conditions including health care-acquired conditions. Fed Regist. 2011;76(108):32816–38. [PubMed] [Google Scholar]
- 14.Blue Cross and Blue Shield announce system-wide payment policy for “never events”. The Remington Report. 2010 May-Jun; [Google Scholar]
- 15.McHugh M, Martin TC, Orwat J, Dyke KV. Medicare's policy to limit payment for hospital-acquired conditions: the impact on safety net providers. J Health Care Poor Underserved. 2011;22(2):638–47. doi: 10.1353/hpu.2011.0058. [DOI] [PubMed] [Google Scholar]
- 16.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76(3):351–70. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaskin DJ, Hadley J, Freeman VG. Are urban safety-net hospitals losing low-risk Medicaid maternity patients? Health Serv Res. 2001;36(1 Pt 1):25–51. [PMC free article] [PubMed] [Google Scholar]
- 18.Hadley J, Cunningham P. Availability of safety net providers and access to care of uninsured persons. Health Serv Res. 2004;39(5):1527–46. doi: 10.1111/j.1475-6773.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA. 2008;299(18):2180–7. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 20.Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113(Suppl 1A):5S–13S. doi: 10.1016/s0002-9343(02)01054-9. [DOI] [PubMed] [Google Scholar]
- 21.Edwards JR, Peterson KD, Andrus ML, Tolson JS, Goulding JS, Dudeck MA, et al. National Healthcare Safety Network (NHSN) Report, data summary for 2006, issued June 2007. Am J Infect Control. 2007;35(5):290–301. doi: 10.1016/j.ajic.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–26. doi: 10.1086/651091. [DOI] [PubMed] [Google Scholar]
- 23.Pennsylvania Department of Health [Accessed June 8, 2012];Healthcare Associated Infections in Pennsylvania, 2010 Report. http://www.portal.state.pa.us/portal/server.pt/community/healthcare_associated_infections/14234.
- 24.Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7(2):342–7. doi: 10.3201/eid0702.010240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garibaldi RA, Mooney BR, Epstein BJ, Britt MR. An evaluation of daily bacteriologic monitoring to identify preventable episodes of catheter-associated urinary tract infection. Infect Control. 1982;3(6):466–70. doi: 10.1017/s0195941700056599. [DOI] [PubMed] [Google Scholar]
- 26.Stone PW, Pogorzelska M, Graham D, Jia H, Uchida M, Larson E. California Hosopitals' Response to State and Federal Policies Related to Health Care-Associated Infections. Policy Polit Nurs Pract. 2011;12(2):73–81. doi: 10.1177/1527154411416129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saint S, Lipsky BA, Baker PD, McDonald LL, Ossenkop K. Urinary catheters: what type do men and their nurses prefer? J Am Geriatr Soc. 1999;47(12):1453–7. doi: 10.1111/j.1532-5415.1999.tb01567.x. [DOI] [PubMed] [Google Scholar]
- 28.Saint S, Lipsky BA, Goold SD. Indwelling urinary catheters: a one-point restraint? Ann Intern Med. 2002;137(2):125–7. doi: 10.7326/0003-4819-137-2-200207160-00012. [DOI] [PubMed] [Google Scholar]
- 29.Affordable Care Act Section 3008: Payment Adjustment for Hospital Acquired Conditions. Pub L No. 111-148, 124 Stat 122. [Google Scholar]


