Abstract
One hundred forty-six patients, ranging in age from 15 to 50 and presenting with a moderate to severe dentofacial disharmony requiring orthodontics and orthognathic surgery, were randomly assigned to 2 preparation strategy groups: standard presurgical consultation with or without a computerized treatment simulation presentation. The demographic profiles of the 2 groups were similar. Viewing a treatment simulation did not have a significant effect on the anticipation of social/interpersonal or general health problems in the first month after surgery. These 2 areas of concern were significantly related to psychological well-being. Psychologically distressed patients, whether or not they saw a simulation, expected significantly more problems in social/interpersonal relations and in general health during the first month after surgery. A treatment simulation presentation did affect patients’ overall expectations of problems in the first month after surgery and their concerns about symptom recovery. However, the impact of the presentation was related to the patient’s psychological well-being. In the standard presurgical consultation group, the average anticipated level of overall problems and discomfort during recovery was significantly higher for patients who reported elevated psychological distress than for those who did not. In the treatment simulation group, the average level of concern was similar for those patients who reported distress and those who did not. Preparation strategy was not significantly related to the long-term expectation of improvement after treatment. Long-term expectation of treatment improvement was related to psychological distress and gender. Men tended to report similar expectations regardless of psychological well-being, while women who were distressed anticipated significantly more improvement overall, in self-image, and in general health after treatment than women who were not distressed.
Patient preparation for surgery is a critical phase of the treatment process for orthognathic surgery for a variety of reasons. First, patients who have neutral or negative expectations regarding the outcome of treatment tend to have more symptoms after surgery, while those with positive treatment expectations tend to minimize or ignore unfavorable symptoms.1–3 Second, surgery patients, including orthognathic surgery patients, are more likely to express dissatisfaction or to experience a negative mood or anxiety postoperatively if some “unexpected” event happens, for example, experiencing more pain or swelling than had been anticipated4–6 or a feeling of being “unprepared.”6–8 And third, physiologic and biologic recovery after surgery can be negatively affected if the patient had high levels of anxiety or stress before surgery.9,10
Patient preparation for orthognathic surgery can take multiple formats. In addition to the written materials and the verbal exchanges between the patient and doctor, new communication tools such as educational videodiscs and interactive CD-ROMs allow patients to visualize treatment options and to learn about the surgical procedure and its consequences and risks. Another relatively recent preparation strategy is a visual treatment simulation. This technique allows the patient to see a simulated computer image of their appearance after surgery. Presentations of treatment simulations can potentially improve clinical communication and consultation between orthodontist and oral surgeon, improve clinical decision-making, make care more patient-based, and enhance patient understanding of treatment.11–13 More than any other preparation strategy for orthognathic surgery, this approach provides a personalized visual reference of “future” to “now,” particularly when the simulation is presented beside or superimposed upon the presurgery facial profile. The post-surgery simulation acts as a cognitive intervention by focusing the patient’s attention on the outcome of treatment, rather than serving as an informational intervention that provides specific details about the surgical or recovery process.
Despite these advantages, many clinicians still have concerns about the use of computer-generated treatment simulations. First, does the presentation of a treatment simulation to a patient and his/her family increase the clinician’s medicolegalliability? Sarver13 raised several specific concerns related to orthognathic surgery regarding implied guarantees and their potential legal implications. Claims of implied contract, failure to instruct, and malpractice are certainly possible, as illustrated in an article from the Stanford Law School and the Division of Otolaryngology/Head & Neck Surgery.14 But Chavez et al14 point out that “a careful analysis of the law reveals that surgeons who carefully and conservatively use computer imaging and adopt a few simple precautions substantially reduce their vulnerability to legal claims.”14p1601
A second concern is whether the presentation alters the patient’s expectations in an unfavorable way with regard to outcome. Patient reaction to the use of this technology is not well understood. In a randomized clinical trial of patients who sought a treatment consultation for a dentofacial disharmony, patients were assigned to 2 groups: treatment simulation plus standard case presentation (TS), or standard case presentation only (SC). Those in the TS group ranked the treatment simulation as the most helpful part of the presentation.15 This finding supports Ackerman and Proffit’s16 suggestion and patient recall data17 that this technology can enhance informed consent by increasing the patient/parent’s role in decision-making. Patients in the TS group did not differ from those in the SC group in their long-term expectations of changes in oral function, general well-being, or general health. The TS group did, however, have significantly elevated expectations of improvement in self-image.15 This effect on self-referent attitudes is not unexpected. Previous studies have reported that videotape feedback has an effect on self-assessments of social ease and physical attractiveness18,19 and self-attribution.20 Interestingly, subjects who were depressed responded with negative self-valuations after videotape feedback, while normal controls responded positively.20 This raises the question of whether an individualized treatment simulation presentation would have a different impact on an orthognathic surgery patient who was experiencing psychological distress at the time of the consultation, versus one who was not.
Although very few orthognathic surgery candidates present with frank psychopathology, a higher-than-expected proportion of patients both at an academic care center and a private practice experienced a clinically elevated level of psychological distress.21,22 Primarily this distress represented adjustment disorders, eg, emotional problems, depressed mood, or anxious mood, rather than major psychiatric disorders. But the level of distress in over 20% of the patients was sufficiently elevated as indicated by the “positive diagnosis” criteria of the Revised Symptom Check-list-90 to warrant a referral and possibly counseling with a mental health specialist.
The purpose of this study, designed as a 2-arm, parallel-group, stratified-block, randomized clinical trial, was to assess whether an individualized treatment simulation presented as part of the presurgical consultation would affect patients’ long- and short-term expectations. The primary hypothesis was that treatment simulation presentations given shortly before surgery would increase patients’ long-term expectations from treatment but have no effect on expectations of problems/discomfort in the short-term postsurgical period.
Methods
Subjects
Patients between 15 and 50 years of age with developmental anteroposterior and/or vertical problems who were scheduled for a presurgery consultation with a faculty surgeon in the Department of Oral and Maxillofacial Surgery at the University of North Carolina (UNC) or with a surgeon in private practice in Seattle, Washington, between July 1995 and June 1999 were eligible to participate in this project. Patients with asymmetry were excluded.
Patients were asked to participate at their initial presurgical consultation appointment with the oral and maxillofacial surgeon. The project was approved by the Institutional Review Board at UNC and the University of Washington (the latter served as the administrative unit for the project in Seattle), and all participating subjects signed informed consent. Two hundred twenty patients (83 from Seattle and 137 from UNC) agreed to participate in this project. To insure a common knowledge base prior to the presurgical consultation, patients viewed a videodisc (Videodiscovery, Seattle, Washington, 1987) that provided information about their surgery, diet, anesthesia, pain and swelling, and potential postsurgical problems. Patients were randomly allocated using a stratified block randomization, with the center (UNC or Seattle) and gender (male or female) as strata. Within each stratum, patients were allocated to a standard presurgery consultation or a standard consultation plus individualized treatment simulation presentation group in blocks of 8 patients each.
A digital image of the profile was taken and a treatment simulation prepared for patients in the TS group. At a session 1 to 2 months before surgery, an individualized surgical simulation planned by the attending orthodontist and/or surgeon was shown to the patient by a research associate. A checklist was used to ensure that the information communicated to the 2 groups of patients about the effect of surgery was as similar as possible.
Instruments
Prior to the treatment simulation presentation, patients were asked to complete the Revised Symptom Checklist-90 (SCL-90-R).23 The SCL-90-R is a 90-item self-report used to assess a patient’s current level of psychological distress. Each item is rated using a 5-point scale, from “not at all (0)” to “extremely (4),” as a response to the question “Within the past 7 days, how much were you distressed by …?” Two measures of psychological well-being were used. As an overall measure of psychological distress that combined information on the number of symptoms and the intensity of perceived distress, the Global Severity Index (GSI) was calculated and converted, using the nonpsychiatric gender-specific patient norms, to a standardized T-score.23 Another indication of the level of current psychological distress is represented by “positive diagnosis,” an epidemiologic screening measure for psychiatric disorder. An individual was considered to have a clinically significant level of distress if the T-GSI score was above a T-score of 63, or if 2 dimensions on the SCL-90-R exceeded a T-score of 63. “Positive diagnosis” represents an elevation in distress that serves as an, indicator for referral to a mental health professional.
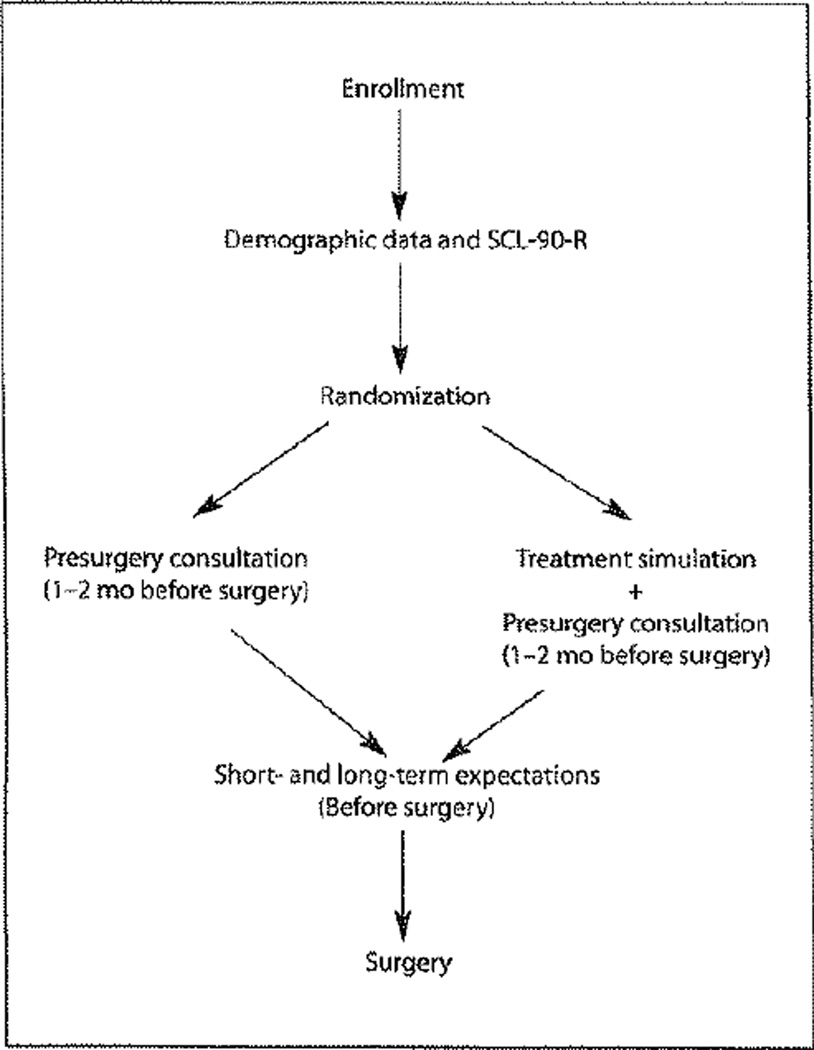
Two to 4 weeks after the presurgery consultation, questionnaires to assess short-term expectations (STE) and long-term expectations (LTE) of treatment, adapted from Kiyak’s conceptualizations,5 were completed by each patient. The STE questionnaire lists 20 items that may cause discomfort or difficulty during the first month after surgery. Each item is rated using a 7-point scale, from “expect no discomfort (1)” to “expect much discomfort (7)” (Table 1). The LTE questionnaire, a 23-item form, asks subjects to rate the change that they expect after all treatment is completed (Table 2). Each item is rated using a 7-point scale ranging from “will be worse after treatment (−1),” to “no change (0),” to “will be much better (+5).” The data collection and randomization sequence are illustrated in Fig 1.
Table 1.
Subjects’ expected levels of discomfort after surgery
| Short-term expectations (STE) |
Expected amount of discomfort* | |||||
|---|---|---|---|---|---|---|
| None | Some | Moderate or worse | ||||
| n | % | n | % | n | % | |
| Postsurgical discomfort | ||||||
| Swelling | 1 | 0.7 | 18 | 12.3 | 127 | 87.0 |
| Chewing | 1 | 0.7 | 22 | 15.1 | 123 | 84.3 |
| Biting | 1 | 0.7 | 24 | 16.4 | 121 | 82.9 |
| Numbness | 2 | 1.4 | 49 | 33.6 | 95 | 65.1 |
| Speaking | 5 | 3.5 | 51 | 37.2 | 86 | 59.3 |
| Facial pain | 4 | 2.7 | 62 | 42.5 | 80 | 54.8 |
| Social concerns | ||||||
| Being in public | 11 | 7.5 | 53 | 36.3 | 82 | 56.2 |
| Social interaction | 27 | 18.6 | 73 | 50.3 | 45 | 31.0 |
| Social life | 29 | 20.0 | 74 | 51.0 | 42 | 29.0 |
| Work/school | 18 | 12.3 | 89 | 61.0 | 39 | 26.7 |
| Depression | 31 | 21.2 | 77 | 52.7 | 38 | 26.0 |
| General health | ||||||
| Swallowing | 21 | 14.4 | 72 | 49.3 | 53 | 36.3 |
| Sleeping | 19 | 13.0 | 75 | 51.4 | 52 | 35.6 |
| TMJ pain | 31 | 21.2 | 65 | 44.5 | 50 | 34.3 |
| Sinus | 45 | 30.8 | 70 | 48.0 | 31 | 21.2 |
| Headaches | 41 | 28.3 | 81 | 55.9 | 23 | 15.9 |
| Breathing | 59 | 40.4 | 67 | 45.9 | 20 | 13.7 |
| Popping/clicking | 59 | 40.7 | 70 | 48.3 | 16 | 11.0 |
None = score of 1; some = score of 2,3, or 4; moderate = score of 5,6, or 7.
The subscales for the STE (and LTE) were developed using an exploratory factor analysis with squared multiple correlations as prior communality estimates. Subscales were extracted using the principal factor method followed by a promax (oblique) rotation. Criteria for retaining subscales included a Scree test with eigenvalues of 1 or more, contribution of at least 5% of the common variance, and interpretability of the subscale.14 In interpreting the rotated factor pattern for the 2 questionnaires, an item was assigned to a specific subscale if the factor loading was .40 or greater on that subscale.
Table 2.
Subjects’ long-term expectations for improvement after treatment
| Long-term expectations (LTE) |
Expected change* | |||||
|---|---|---|---|---|---|---|
| Will be worse | No or little improvement |
Moderate improvement |
||||
| n | % | n | % | n | % | |
| Oral function | ||||||
| Fit of teeth | 0 | 0.0 | 14 | 9.5 | 133 | 90.5 |
| Front teeth together | 0 | 0.0 | 20 | 13.7 | 126 | 86.3 |
| Back teeth together | 0 | 0.0 | 29 | 19.9 | 117 | 80.1 |
| Chewing | 4 | 2.8 | 33 | 22.8 | 108 | 74.5 |
| Biting | 3 | 2.1 | 38 | 25.6 | 106 | 72.1 |
| Self-image | ||||||
| Appearance of teeth | 0 | 0.0 | 24 | 16.3 | 123 | 86.7 |
| Appearance of face | 0 | 0.0 | 32 | 21.9 | 114 | 78.1 |
| General appearance | 0 | 0.0 | 53 | 36.3 | 93 | 63.7 |
| Out in public | 2 | 1.4 | 77 | 52.4 | 68 | 46.3 |
| Confidence | 2 | 1.37 | 79 | 54.1 | 65 | 44.5 |
| Speaking | 2 | 1.4 | 81 | 55.1 | 64 | 43.5 |
| Feelings about self | 0 | 0.0 | 85 | 57.8 | 62 | 42.2 |
| Socializing | 0 | 0.0 | 103 | 70.6 | 43 | 29.5 |
| Social life | 1 | 0.7 | 110 | 75.9 | 34 | 23.5 |
| General health | ||||||
| Popping/clicking | 1 | 0.7 | 75 | 51.4 | 70 | 48.0 |
| Jaw pain/damage | 5 | 3.4 | 90 | 61.2 | 52 | 35.4 |
| Headaches | 0 | 0.0 | 101 | 68.7 | 46 | 31.3 |
| General health | 1 | 0.7 | 101 | 68.7 | 45 | 30.6 |
| Breathing | 0 | 0.0 | 115 | 78.8 | 31 | 21.2 |
| Work/school | 2 | 1.4 | 114 | 78.1 | 30 | 20.6 |
| Sleeping | 1 | 0.7 | 117 | 80.1 | 28 | 19.2 |
| Sinus | 3 | 2.1 | 117 | 80.1 | 26 | 17.8 |
| Please family | 0 | 0.0 | 129 | 89.0 | 16 | 11.0 |
Worse = score of −1; no or little = score of 0,1, or 2; moderate = score of 3,4, or 5.
Fig 1.
Data collection and randomization sequence. Patient enrollment, demographic and psychological well-being data, and the presurgery consultation occurred 1 to 2 months before surgery. Subjects were mailed the STE and LTE questionnaires 1 week after the consultation and asked to return the questionnaires prior to surgery.
Questionnaire analysis
The results of the STE and LTE questionnaires were analyzed separately. For each participant, the average of all items on each questionnaire was calculated, as well as an average score for each subscale of the LTE and STE questionnaires. The 3 subscales for STE identified by a factor analysis24 were labeled postsurgical discomfort, social well-being concerns, and general health. The 3 subscales for LTE were labeled oral function, self-image, and general health. In this sample, Cronbach’s alpha ranged from .85 to .89 for STE and .79 to .89 for LTE. Patients were paid $10 if they returned their questionnaires before surgery.
Subject dropout
Sixty-three (76%) subjects from Seattle and 83 (61%) from UNC of the 220 who agreed to participate completed all of the presurgical data collection phases. Nine patients refused to complete the SCL-90-R. The 65 subjects who did not complete the presurgery study protocol either did not return for the presurgery consultation visit or there was insufficient time between the initial presurgical consultation and surgery to complete the protocol. The excluded patients were similar to those who completed the data collection phase in age (P = .70), gender (P = .65), and percent randomized to a treatment simulation (P = .06).
Data analysis
The similarity of the participants in the 2 preparation groups and the 2 centers was assessed with Mantel Haenszel chi-square statistics for gender and race and unpaired t tests for age at surgery. The effect of the treatment simulation, center, gender, and positive diagnosis for psychological distress on the LTE and STE total and subscale scores were analyzed using factorial analysis of variance. All possible pairwise interaction terms between the explanatory variables were included in the initial model. Interactions with P values greater than .10 were eliminated, and reduced models were analyzed. Contrasts for specific group comparisons within a significant interaction were performed using predicted population marginals.
Pearson correlation coefficients were calculated between the STE and LTE sub-scales and the GSI and age at the time of surgery to evaluate simple bivariate relationships. Partial correlations were calculated among the expectation measures, partialing out the effects of psychological distress (T-GSI scores). The level of significance was set at .05 for all analyses.
Results
Participants
Participants were predominantly white (88%) and female (69%). Thirty-three percent of the patients were psychologically distressed, as indicated by a “positive diagnosis” on the SCL-90-R. Eighteen percent reported previous or current psychological therapy, and 10% reported past or current use of medication for psychological problems. Approximately three fourths of the participants reported a household income greater than $40,000. Patients at the 2 centers were very similar in their demographic characteristics (Table 3), except that the percentage of patients older than 25 was much higher in Seattle. The patients in Seattle ranged in age from 15 to 52 and the median age was 32; while at UNC the age range was 15 to 53, but the median age was only 21. The patients randomized to the standard presurgical consultation were similar in gender and age to those randomized to the treatment simulation presentation group. The 2 preparation groups differed significantly in the percentage of non-Caucasians and were marginally different in the percentage of psychologically distressed participants (Table 3).
Table 3.
Demographic characteristics of the participants in the 2 centers and in the 2 preparation groups
| Demographic characteristic |
Center | P value | Preparation strategy | |||
|---|---|---|---|---|---|---|
| Standard presentation |
Treatment simulation presentation |
P value | ||||
| UNC | UW | |||||
| Psychologically distressed | 30% | 37% | .40 | 39% | 24% | .06 |
| Older than 25 | 38% | 68% | .0001 | 52% | 45% | .40 |
| Female | 70% | 67% | .68 | 66% | 73% | .40 |
| Caucasian | 85% | 93% | .14 | 83% | 95% | .02 |
| Previous orthognathic surgery | 6% | 11% | — | 9% | 7% | — |
| Previous/current counseling | 14% | 25% | — | 16% | 22% | — |
UNC = University of North Carolina; UW = University of Washington.
Overall expectations
Substantially more patients in both preparation groups expected to experience postsurgical discomfort than problems in general health or in social or interpersonal areas in the first month after surgery. Over 80% of the patients anticipated at least moderate discomfort from facial swelling and difficulties with mastication (biting and chewing). Only 65% expected facial numbness to cause a moderate problem (Table 1).
More than three fourths of the patients expected at least moderate improvement in oral function and profile appearance at the end of treatment. More than 40% expected at least a moderate improvement in general appearance, self-confidence, feelings about themselves, and confidence when out in public (Table 2).
The correlations between the short- and long-term expectations (Table 4) were statistically significant, but the common variance explained was low—less than 15%. In general, patients who anticipated more overall problems and had more concerns about social/interpersonal relations and general health in the first month or so after surgery also expected greater improvement as a result of treatment.
Table 4.
Spearman correlations among expectations
| Short-term expectations |
Long-term expectations | |||
|---|---|---|---|---|
| Overall | Function | Self-image | General health |
|
| Overall | 0.35* | 0.23* | 0.27* | 0.26* |
| Postsurgical discomfort | 0.17* | 0.28* | 0.07 | 0.07 |
| Social concerns | 0.25* | 0.11 | 0.3* | 0.13 |
| General health | 0.37* | 0.19* | 0.27* | 0.37* |
r values ≥ 10.161 statistically significant at 0.05.
Associations with expectations
Patients experiencing psychological distress tended to expect more problems overall immediately after surgery and had more social and interpersonal concerns as well as general health concerns. Interestingly, psychological distress was not related to the expectation of postsurgical discomfort (Table 5). Distress was also associated (although at quite a low level) with all of the long-term expectations except oral function improvement. Psychological well-being did not account for the positive relationship between short- and long-term expectations. The correlation coefficients were reduced only slightly when global psychological symptom severity was controlled by partial correlation.
Table 5.
Spearman correlations between expectations, psychological distress, and age at surgery
| Expectations | Psychological distress |
Age at surgery |
|---|---|---|
| Short-term | ||
| Overall | 0.24* | −0.11 |
| Postsurgical discomfort | 0.11 | 0.05 |
| Social concerns | 0.25* | −0.12 |
| General health | 0.26* | −0.09 |
| Long-term | ||
| Overall | 0.19* | −0.21* |
| Function | 0.11 | −0.06 |
| Self-image | 0.16* | −0.27* |
| General health | 0.21* | −0.15 |
r value ≥ 10.161 statistically significant at 0.05.
Psychological distress is statistically associated with some long- and short-term expectations, although the extent of the distress explains very little (< 5%) of the variability in expectations. Higher expectations of overall, social, and general health problems in the first month after surgery and greater expectation of overall and personal health improvement after treatment were associated with elevated distress. Age was not correlated with short-term expectations. Younger patients tended to expect greater improvement overall and in self-image.
Age was not associated with any of the short-term expectations. Age was significantly associated with long-term expectations. Younger patients tended to expect more overall long-term benefit from treatment and more social/interpersonal benefit than their older counterparts (Table 5).
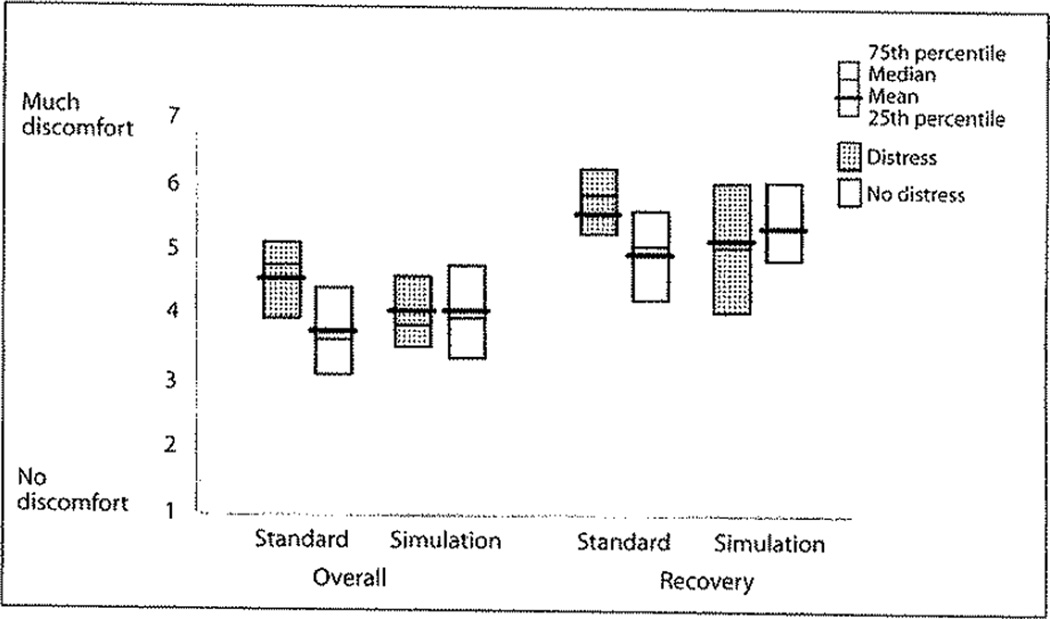
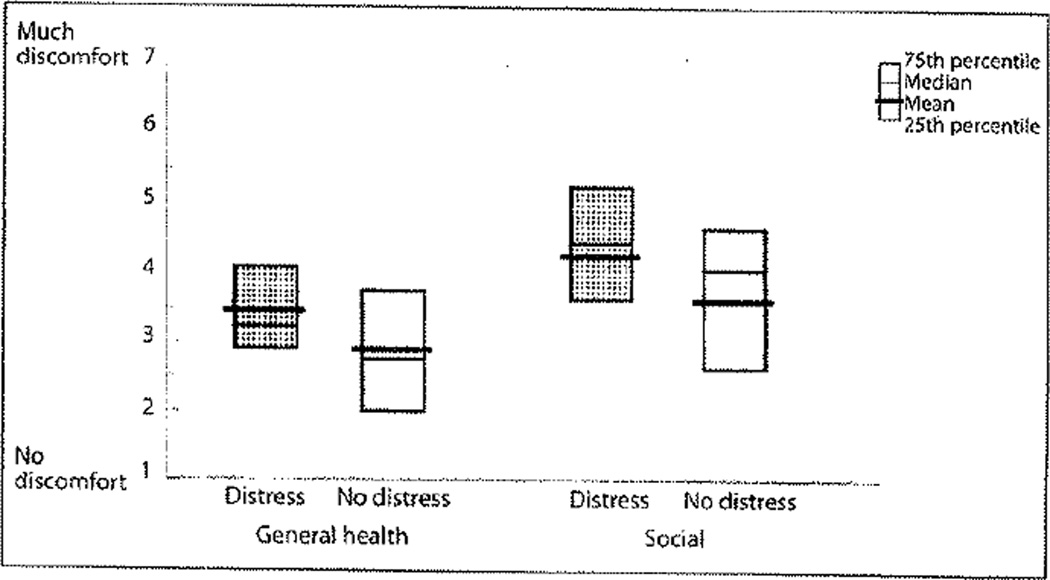
Effect of preparation strategy on expectations
Preparation strategy did not have a significant effect on the anticipation of social/interpersonal or general health problems in the first month after surgery. These 2 areas of concern were significantly related to psychological well-being (Table 6, Fig 3). Regardless of the preparation strategy used, distressed patients expected significantly more problems in social/interpersonal relations and in general health during the first month after surgery (Fig 2).
Table 6.
Analysis of variance for short-term expectations (n = 146)
| Total | Postsurgical discomfort |
Social concerns | General health | |||||
|---|---|---|---|---|---|---|---|---|
| MS | P value | MS | P value | MS | P value | MS | P value | |
| Interaction* | ||||||||
| Preparation strategy × psychological distress | 3.84 | .05 | 5.41 | .02 | — | — | — | — |
| Main effects | ||||||||
| Center | 3.32 | .07 | .63 | .42 | 1.57 | .21 | 2.44 | .12 |
| Gender | 2.83 | .09 | 5.75 | .02 | .8 | .37 | 1.67 | .20 |
| Psychological distress | 5.61 | .02 | 1.26 | .26 | 7.27 | .01 | 9.31 | .003 |
| Preparation strategy | 0.41 | .52 | 0.02 | .82 | 0.24 | .63 | 0.04 | .85 |
The interaction between preparation strategy and psychological distress was the only statistically significant pairwise interaction and only in the ANOVA models for overall and postsurgery short-term expectations for discomfort.
Results form the reduced models are presented in this table.
Fig 3.
Effect of preparation strategy and psychological distress on the level of discomfort expected overall and in recovery symptoms in the first month after surgery. When given a standard presurgical consultation, patients who reported clinically elevated psychological distress anticipated on average more problems overall (P < .0005) and in symptom recovery (P < .005) than those who were not distressed. When a treatment simulation presentation was included in the consultation, the average level of overall (P = .12) and symptom recovery problems (P = .13) expected were not significantly different for distressed and not distressed patients.
Fig 2.
Effect of psychological distress on the level of discomfort expected in general health and social interactions in the first month after surgery. Psychologically distressed patients anticipated, on average, more discomfort of problems with general health (P = .003) and social well-being (P = .01) than patients who were not distressed.
Viewing a treatment simulation did affect patients’ overall expectations about problems and symptom recovery in the first month after surgery. However, the impact of the presentation was related to the patient’s psychological well-being (Table 6, Fig 3). For patients given a standard presurgical consultation, those with elevated psychological distress had significantly higher average levels of overall concerns (P = .0005, x̄ = 4.48) and recovery concerns (P = .0005, x̄ = 5.55) than those who did not report elevated distress (x̄ = 3.72 and 4.92, respectively). However, the average levels of overall and recovery concern were not statistically different (P = .12 and .13, respectively) for distressed and non-distressed patients when shown a treatment simulation (distressed patients: x̄total = 4,02, x̄recovery = 5.08; non-distressed patients: x̄total = 3.95 and x̄recovery = 5.31). For both measures, the mean level of concern was higher in the treatment simulation group than in the standard group for those patients who did not report distress. For those who did report distress, the mean score was lower in the simulation group (Fig 3) for both measures.
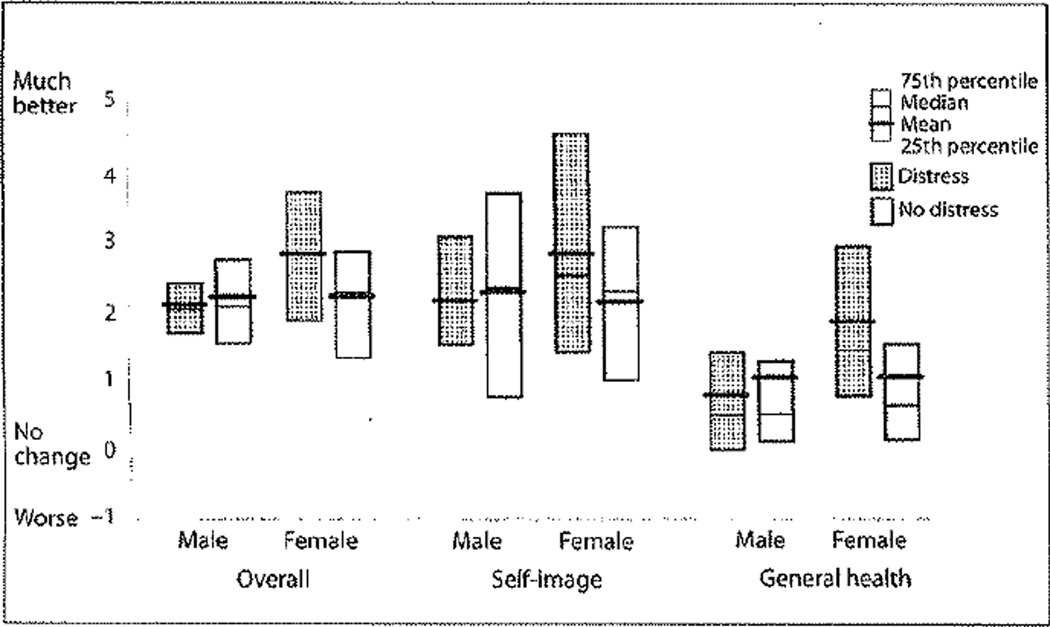
Preparation strategy did not affect long-term expectations for improvement after treatment (Table 7). The expectation of improvement was related to gender and to psychological well-being (Fig 4). Men tended, on average, to have similar expectations about treatment outcomes, regardless of their psychological status. In contrast, women who were distressed anticipated significantly more improvement overall (P = .003), in self-image (P = .006), and in general health (P = .003) after treatment than women who were not distressed. In general, patients at UNC tended on average to have significantly higher expectations of improvement than the patients in Seattle (Table 7).
Table 7.
Analysis of variance models for long-term expectations (n = 146)
| Total | Social/self | Function | General health | |||||
|---|---|---|---|---|---|---|---|---|
| MS | P value | MS | P value | MS | P value | MS | P value | |
| Interaction* | ||||||||
| Gender × psychological distress | 4.13 | .04 | 3.90 | .05 | — | — | 4.49 | .04 |
| Gender × center | — | — | — | — | 4.13 | .04 | — | — |
| Main effects | ||||||||
| Center | 5.61 | .02 | 14.3 | .0002 | 1.74 | .17 | 0.69 | .41 |
| Gender | 3.41 | .07 | .98 | .32 | 1.16 | .28 | 5.2 | .02 |
| Psychological distress | 1.96 | .16 | 1.41 | .24 | .90 | .35 | 1.53 | .22 |
| Preparation strategy | 0.59 | .44 | 0.51 | .48 | 0.59 | .44 | 0.01 | .90 |
No other pairwise interaction terms were statistically significant.
Results from the reduced models are presented in this table.
Fig 4.
Expected improvement at the end of treatment overall, in self-image, and in general health for men and women who did and did not report psychological distress. Women who reported clinically elevated psychological distress tended on average to expect more improvement after treatment overall, in self-image, and in general health than men (regardless of their distress level) and women who were not distressed.
Discussion
The patients randomly assigned to the 2 surgical preparation strategies were similar in age and demographic characteristics to those studied in larger groups of orthognathic surgery patients.25,26 Randomization did not create equivalent groups with regard to psychological distress and race. Although it is the most effective method for achieving equivalence across treatment groups for both known and unknown prognostic characteristics, randomization does not guarantee a balance of characteristics, such as race and psychological distress, that are not included in the design.27 The patients enrolled at the 2 centers were similar in demographic characteristics, except that the patients at the academic care center tended to be younger than those in the community-based practice.
The impact on short-term expectations of viewing a treatment simulation in conjunction with a standard presurgical consultation is moderated by the patient’s psychological distress. It appears that viewing a treatment simulation tends to increase concern about the problems that might be experienced for those individuals with low psychological distress and decrease concern in those with higher levels of distress. This may be quite a beneficial impact, since the goal of a preparation strategy should be to provide patients with an appropriate level of concern that is neither too low nor too high. If concerns about the immediate postoperative period are too low, then the experienced level may exceed what was expected. This type of discrepancy has been shown to cause dissatisfaction and increased awareness of symptoms.4–6 If expectations about problems are too high, then the expectations may cause unwarranted presurgical anxiety and stress that, given the effect of stress on the immune system, may slow postsurgical recovery.9,10
The type of preparation a patient received had no direct effect on long-term expectations. This differs from an earlier report on the effect of treatment simulation, in which the long-term expectation of improvement in self-image was higher in the treatment simulation group.13 The difference in the timing of the presentation in these 2 clinical trials may explain this discrepancy. In the first trial, the treatment simulation was shown as a part of the case presentation 2 to 4 weeks after the initial consultation. Patients had not yet made a treatment decision, and many were still in the process of deciding on the relative risks and benefits of treatment. In that trial, patients considered the treatment simulation to be the most helpful of the physical records with regard to treatment decision and understanding what to expect from treatment. Patients in the current trial were already well vested in the treatment process by the time of the treatment simulation presentation 1 to 2 months before surgery. It may be that, in terms of long-term expectations, the presentation of a treatment simulation is more effective as a cognitive strategy at the pretreatment consultation.
The percentage of patients in this sample of presurgery patients with a positive diagnosis for current psychological distress levels was even higher than the prevalence of distress reported previously for skeletal disharmony patients who presented for a pretreatment consultation. Approximately one third of the patients in the community practice and in the academic center endorsed items suggestive of clinically elevated psychological distress. This finding suggests that the level of distress reported earlier21,22 is not reflective only of patients who seek treatment at an academic center.
Recent findings indicate that presurgical psychological distress in orthognathic surgery patients has a negative impact on postsurgical outcomes28 and on the perception of oral health before and after surgery.29 Results from the current study indicate that psychological distress is associated with a higher expectation of problems after surgery and with an increased expected benefit after treatment. The relationship between psychological distress and expectations, although not previously reported in the orthognathic surgery literature, is well substantiated in the medical literature.2,3 These findings illustrate the importance of clinicians providing appropriate presurgical information, including simulated images of treatment outcomes, as well as emotional support and referral to a mental health professional if necessary.
Generally, patients are willing to complete an instrument such as the SCL-90-R when the patient understands that (1) the clinician is interested in the patient’s overall well-being, not just the appearance of the teeth and/or face; and (2) the information is confidential and is meant to assist the clinician in supporting the patient during the treatment process. Psychological distress, as indicated on a measure such as the SCL-90-R, may prompt the orthodontist and/or surgeon to explore those areas that may complicate or interfere with a patient’s treatment and recovery from surgery. If appropriate, patients with clinically elevated scores can be referred to a mental health specialist for evaluation and counseling. Counseling, if viewed by the clinician as a constructive option for addressing life problems, can be recommended without offending the patient, particularly when the recommendation is presented as the clinician’s concern regarding the additional stress of surgery and recovery.
Conclusions
Presentation of a treatment simulation 1 to 2 months before surgery does not affect patients’ long-term expectations of the benefit of treatment.
Psychological distress moderates the effect of the treatment simulation on short-term expectations of problems after surgery.
Patients who reported no clinically elevated psychological distress expected more postsurgical problems after viewing the treatment simulation than those who received the standard presurgical consultation only.
Patients with clinically elevated psychological distress expected fewer postsurgical problems after viewing the treatment simulation than those who received the standard presurgical consultation only.
Acknowledgments
This project was supported by NIH grants DE10028 and DE05215. The authors wish to thank Debora Price, Teresa Hagan, Will Harvey, Steve Dickens, Lawrence Patrick, and Carol Dean for their assistance with data collection and processing.
Contributor Information
Ceib Phillips, Department of Orthodontics, University of North Carolina, Chapel Hill, North Carolina.
L’Tanya Bailey, Department of Orthodontics, University of North Carolina, Chapel Hill, North Carolina.
H. Asuman Kiyak, Department of Oral and Maxillofacial Surgery, University of Washington, Seattle, Washington.
Dale Bloomquist, Private Practice in Oral and Maxillofacial Surgery, Seattle, Washington.
References
- 1.Brody H. Placebos and the Philosophy of Medicine. Chicago: University of Chicago Press; 1977. [Google Scholar]
- 2.Flood AB, Lorence DP, Ding J, McPherson K, Black NA. The role of expectations in patients’ report of post-operative outcomes and improvement following therapy. Med Care. 1993;31(11):1043–1056. doi: 10.1097/00005650-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kravitz RL. Patients’ expectations for medical care: An expanded formulation based on review of the literature. Med Care Res Rev. 1996;53(1):3–27. doi: 10.1177/107755879605300101. [DOI] [PubMed] [Google Scholar]
- 4.Kiyak HA, McNeill RW, West RA, Hohl T, Bucher F, Sherrick P. Predicting psychologic responses to orthognathic surgery. J Oral Maxillofac Surg. 1982;40(3):150–155. doi: 10.1016/0278-2391(82)90046-5. [DOI] [PubMed] [Google Scholar]
- 5.Kiyak HA, Vitaliano PP, Crinean J. Patients’ expectations as predictors of orthognathic surgery outcomes. Health Psychol. 1988;7(3):251–268. doi: 10.1037//0278-6133.7.3.251. [DOI] [PubMed] [Google Scholar]
- 6.Ostler S, Kiyak HA. Treatment expections versus outcomes among orthognathic surgery patients. Int J Adult Orthod Orthognath Surg. 1991;6(4):247–255. [PubMed] [Google Scholar]
- 7.Garvill J, Garvill H, Kahnberg KE, Lundgren S. Psychological factors in orthognathic surgery. J Craniomaxillofac Surg. 1992;20(1):28–33. doi: 10.1016/s1010-5182(05)80193-3. [DOI] [PubMed] [Google Scholar]
- 8.Phillips C. Patient-centered outcomes: Impact on clinical practice and research. Semin Orthod. 1999;5:223–231. doi: 10.1016/s1073-8746(99)80016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson M. Pre-operative emotional states and post-operative recovery. Adv Psychosom Med. 1986;15:1–22. doi: 10.1159/000411845. [DOI] [PubMed] [Google Scholar]
- 10.Linn BS, Linn MW, Klimas NG. Effects of psychophysical stress on surgical outcome. Psychosomat Med. 1988;50:230–244. doi: 10.1097/00006842-198805000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Grubb JE, Smith T, Sinclair P. Clinical and scientific applications/advances in video imaging. Angle Orthod. 1996;66:407–416. doi: 10.1043/0003-3219(1996)066<0407:CASAAI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan B, Lundsgaarde HP. Toward an evaluation of an integrated clinical imaging system; Identifying clinical benefits. Methods Inform Med. 1996;35:221–229. [PubMed] [Google Scholar]
- 13.Sarver DM. Video imaging and treatment presentation: Medicolegal-legal implications and patient perception. Am J Orthod Dentofac Orthop. 1998;112:360–363. doi: 10.1016/s0889-5406(98)70154-4. [DOI] [PubMed] [Google Scholar]
- 14.Chavez AK, Dagum P, Koch RJ, Newman JP. Legal issues of computer imaging in plastic surgery: A primer. Plast Reconstr Surg. 1997;100:1601–1608. doi: 10.1097/00006534-199711000-00040. [DOI] [PubMed] [Google Scholar]
- 15.Phillips C, Hill BJ, Cannac C. The influence of video imaging on patients’ perceptions and expectations. Angle Orthod. 1995;65(4):263–270. doi: 10.1043/0003-3219(1995)065<0263:TIOVIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Ackerman JL, Proffit WR. Communication in orthodontic treatment planning: Bioethical and informed consent issues. Angle Orthod. 1995;65:253–262. doi: 10.1043/0003-3219(1995)065<0253:CIOTPB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Sarver DM, Johnston MJ, Matukas VJ. Video imaging for planning and counseling for orthognathic surgery. J Oral Maxillofac Surg. 1988;46:939–945. doi: 10.1016/0278-2391(88)90330-8. [DOI] [PubMed] [Google Scholar]
- 18.Griffiths RDP, Gillingham P. The influence of videotape feedback on the self-assessments of psychiatric patients. Br J Psychiatry. 1978;183:156–161. doi: 10.1192/bjp.133.2.156. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths RDP, Hinkson J. The effect of videotape feedback on the self-assessments of psychiatric patients. Br J Psychiatry. 1973;123(573):223–224. doi: 10.1192/bjp.123.2.223. [DOI] [PubMed] [Google Scholar]
- 20.Biggs SJ, Rosen B, Summerfield AB. Video-feedback and personal attribution in anorexic, depressed and normal viewers. Br J Med Psychol. 1980;33:249–254. doi: 10.1111/j.2044-8341.1980.tb02548.x. [DOI] [PubMed] [Google Scholar]
- 21.Phillips C, Bennett ME, Broader HL. Dentofacial disharmony: Psychological status of patients seeking treatment consultation. Angle Orthod. 1998;68(6):547–556. doi: 10.1043/0003-3219(1998)068<0547:DDPSOP>2.3.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Phillips C, Bennett ME, Kiyak HA. Psychological distress in orthognathic surgery patients. J Dent Res. 1998;77:219. [abstract #911]. [Google Scholar]
- 23.Derogatis LR. The SCL-90 Administration, Scoring and Procedures Manual. Baltimore: Johns Hopkins University Press; 1977. [Google Scholar]
- 24.Hatcher L. A Step-By-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling. Cary, NC: SAS institute; 1994. pp. 57–127. [Google Scholar]
- 25.Proffitt WR, Phillips C, Dann C., IV Who seeks surgical-orthodontic treatment? The characteristics of patients evaluated in the UNC Dentofacial Clinic. Int J Adult Orthod Orthognath Surg. 1990;5:153–160. [PubMed] [Google Scholar]
- 26.Barber HD, Wilmot JJ, Scott RF, Fonseca RJ, Vig KWL. The Dentofacial Deformity Program of the University of Michigan: Organization, analysis of data, and benefits of the program. Int J Adult Orthod Orthognath Surg. 1992;7:119–128. [PubMed] [Google Scholar]
- 27.Therneau TM. How many stratification factors are “too many” to use in a randomization plan? Control Clin Trials. 1993;14:98–108. doi: 10.1016/0197-2456(93)90013-4. [DOI] [PubMed] [Google Scholar]
- 28.Scott AA, Hatch JP, Rivera SM, et al. Psychosocial predictors of high-risk patients undergoing orthognathic surgery. Int J Adult Orthod Orthognath Surg. 2000;15:7–15. [PubMed] [Google Scholar]
- 29.Hatch JP, Rugh JD, Clark GM, Keeling SD, Tiner BD, Bays RA. Health-related quality of life following orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1998;13:67–77. [PubMed] [Google Scholar]