Abstract
The purpose of this study was to examine the relationships between acculturation level and perceptions of health access, Chinese health beliefs, Chinese health practices, and knowledge of breast cancer risk. This descriptive, correlational cross-sectional study used a survey approach. The sample included 135 Chinese women from the New York City metropolitan area. Data were analyzed using correlational techniques and polytomous regression. There were no significant relationships between acculturation and health access, Chinese health beliefs, Chinese health practices, and breast cancer risk knowledge. Only “years of education,” “marital status,” and “household income” significantly predicted breast cancer risk knowledge level. The data indicate that women with a better knowledge of breast cancer risk are twice as likely to have higher income and have more education. The most knowledgeable women are less likely to be married and less likely to have partners compared to least knowledgeable group. Providers need to promote health knowledge and provide information about as well as access to preventive health practices to the immigrant population, given that acculturation to the new dominant society is inevitable.
Keywords: Acculturation, Breast cancer, Chinese medicine, Immigrants, Knowledge
The United States continues to be a destination for a large number of immigrants and refugees.1 In the United States, immigrants face a complex healthcare system in which the modes of communication and expectations of both clients and providers differ from those in their home countries. With immigration, they may lose their former social support system, experience a decrease in socioeconomic status, and in their new land, be exposed to pathogens and disease risk factors never encountered before.2–4 The risk factors might present as food-consumption changes, stress-level increases, or polluted environments. The purpose of this study was to examine the relationships between acculturation level and perceptions of health access, Chinese health beliefs, Chinese health practices, and knowledge of breast cancer risk in a sample of female Chinese immigrants in the New York City metropolitan area.
According to the US census of the year 2000, there are 11.9 million Chinese immigrants in the United States, a 72.2% increase since 1990.5 The Asian population, considered as a group, increased from 3.8% to 5.5% of the total population of New York County (Manhattan), increasing from 689,303 to 1,044,976.5 In Queens County, there was a 14.2% increase in the Asian population over the decade 1990–2000 from 1,951,598 to 2,229,379.5
Among all women, including Chinese women, breast cancer is the most commonly diagnosed cancer.6 Chinese women in the United States have a lower incidence of breast cancer (54.0 per 100,000) than do Caucasian women (86.5 per 100,000),7 but survival rates as long as 5 years are less frequent for Chinese women (64%) than for Caucasian women (71%).7 A late stage of diagnosis, because of cultural and institutional barriers, increases cancer mortality among Chinese women.4,8–12
The incidence of breast cancer among Chinese women in the United States is substantially higher than that of Chinese women in Asia.13 The latter ranges from 6.1 per 100,000 in Taipei to 18.2 per 100,000 in Singapore and 21.5 per 100,000 in Hong Kong.14 Factors thought to increase the cancer risk of Chinese women in the United States (both immigrant and American-born) include the westernization of the diet (less fiber, more fat), earlier age of menarche, later age of bearing a first child, fewer children, and less breast-feeding.15–18
Conceptual Framework
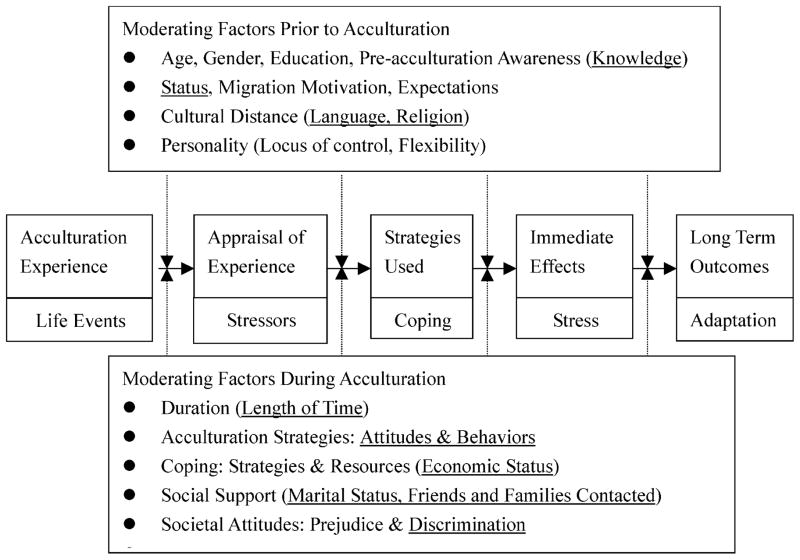
The theoretical framework of acculturation utilized in this study has been partially adapted from Berry’s model19 (see Fig 1). The World Health Organization’s conceptualization of health is “a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity.”20 Most acculturative studies focus on measuring mental health outcomes.21–24 Two important issues can be noted from these research studies. First, patterns of physical illness among immigrants tend to resemble those found in nonimmigrants (eg, hypertension and cancer). Second, some physical health problems increase because of exposure to new sources of diseases as well as to increased stress (which leads to increased susceptibility).24
Figure 1.
Acculturation model. The underlined text indicates study variables. Model partially adapted with permission from Berry.19
The effect of acculturation on health is characteristically seen as a negative linear process that results from increasing “acculturative stresses” as immigrants come into conflict with new values and customs in their host country.25 For recent female immigrants to this country, the stressors include changes in environment and culture, which are often experienced as internalized fears or anticipatory concerns.26 Among the most frequent stressors are external events relating to her partner (eg, marital discord), monetary issues, language, customs, and work or education issues.27
In Berry’s model, there is no specific stage related to knowledge level and health access. However, there are many related factors (variables) prior to and during acculturation, for example, life events such as taking children to have immunization shots or personal illness would influence her knowledge of disease prevention. In the case of breast cancer knowledge, women might or might not encounter prevention of breast cancer in their hometown, since the breast cancer rate is low in women in Asia. The study variables used in this study predicting breast cancer knowledge were underlined in this framework. Acculturation is an important factor in whether Chinese women gain more knowledge of cancer prevention and know where to seek for medical attention after they come to the United States.
Methods
Study Design
This descriptive correlational cross-sectional study used a self-administered survey approach. Participation in the study was limited to Chinese immigrant women, aged 18 and older. Chinese literacy was an inclusion criterion because the questionnaire used in the survey was written in Chinese. Three research questions were addressed.
Are acculturation level and perceptions of health access significantly related?
Are acculturation level, Chinese health beliefs, and traditional Chinese health practices significantly related?
Do demographic variables and acculturation level significantly predict breast cancer risk knowledge?
Study Instruments
The instrument for this study was partially adapted from Lee’s California Pathway cancer prevention survey of a Chinese population in California.10 Psychometric characteristics were reported in a series of studies in California.10,28–33 The questionnaire consists of 6 major categories of questions: (1) demographics, (2) acculturation, (3) access to medical care, (4) attitudes toward healthcare and cancer, (5) breast-screening practices, and (6) barriers to cancer-screening practices.10 Because of cultural differences between the Chinese populations of New York and California, 23 questions were added to target New York City Chinese, resulting in a total of 80 questions in the survey instrument for this study.
A pilot study was conducted to assess reliability of the revised instrument. Using a sample of 35 participants, the sub-scale reliabilities ranged from 0.72 to 0.96. A summary of variables and related questions are shown in Table 1.
Table 1.
Study Measures
| Variables | Number of Items | Item Content |
|---|---|---|
| Acculturation | 9 | Language, identity, social preferences, behaviors, and attitudes |
| General health concepts | Transportation difficulty, waiting time, child-care issues, cost, regular checkup concept, traditional Chinese health practice | |
| •Healthcare access | 14 | |
| •Traditional Chinese medicine | 6 | |
| Knowledge of breast cancer risk | 10 | Questions related to breast cancer risk |
| Demographic data | 19 | Insurance, support system, length of stay in the United States, educational level, working hours, number of children, original country, religion, annual income |
Procedures
Columbia Presbyterian Medical Center (CPMC) Institutional Review Board approved the study in 2001. All study participants were recruited from various public arenas in the New York City metropolitan area: 2 churches, 1 temple, 2 childbirth classes, and 4 American Cancer Society activities. The investigator approached potential subjects and offered an invitation in Chinese for participation in the study. After securing the participant’s permission, a written questionnaire was administered. Each participant was asked to complete it independently. The data collection period was approximately 4 months from July to November 2001. Approximately 210 Chinese women were approached, 195 questionnaires were distributed, and 135 were returned for a return rate of 70%.
Data Analysis
Analyses were conducted using Statistical Package of Social Science (SPSS) Version 9.0. Polytomous logistic regression was used to determine the significant predictors of knowledge of breast cancer risk: insurance status, age, marital status, length of stay in New York, employment status, legal status, household income, and acculturation level. Other research questions were examined using Pearson γ to examine the relationships among research variables.
Results
Demographics
The mean for number of years of education was 10.23; most participants only finished junior high school (56%). The average years of living in the United States is 11 years; however, most of the women live in the States for only 2 years. The participants reported an average of 4 close friends and relatives all over the world and 4 people living with them in the same home. The majority (74%) were married with 1 or 2 children. Most participants immigrated from Hong Kong, Taiwan, and China, with 67% holding legal immigrant status in the United States (Green Card residence and/or citizenship). Most were Buddhists. Slightly more than a quarter of the participants smoked or lived with someone who smoked. About one half of the participants were employed and almost 57% of the study sample reported their yearly household income to be less than $20,000. Nineteen percent of the women reported incomes of $50,001 or greater. Approximately 29% of the participants reported that they had no health insurance.
Most of the women recruited from the childbirth classes were from China. They were younger in age (Mean = 36.6 years) than those recruited from the other locations (Mean = 47.7 years). Also, most of the women recruited from childbirth classes were undocumented aliens. Ninety percent of the undocumented women in the study were from China; others were from other countries, eg, Malaysia and/or Vietnam.
Healthcare Access
Acculturation level and perceptions of health access were not significantly related (r = −0.061 P = .11). However, descriptive statistics indicated that these women experienced several issues with accessing healthcare services. More than half of the women had problems securing transportation to see the doctor. Nearly three quarters were concerned about medical costs. More than half had communication problems with providers. A small proportion (9%) of the participants felt that medical professionals treated them differently because of their ethnicity and communicating ability. The vast majority (93%) of the women reported that they waited a long time to see doctors and usually, when they made appointments, there were no slots for them to see the doctor sooner.
Chinese Health Beliefs
There were no relationships between acculturation level and Chinese health beliefs (r = −0.11, P = .14) and traditional Chinese health practices (r = −0.153, P = .9). Chinese health beliefs and Chinese health practices were significantly correlated (r = 0.24 and P <.05). Descriptive statistics showed that a distinct majority (82%) of the Chinese women believed that most diseases are caused by the imbalance of ying and yang; however, 47% of them did not know which diseases were caused by the imbalance. About one quarter of the women (26%) believed that discomfort in the digestive system is the major cause of the “hot” and “cold” imbalance. The vast majority (87%) of the participants reported that they would use combined (Western and Eastern medicine) methods for cancer treatment.
Knowledge of Breast Cancer Risk
Knowledge scores ranged from 0 to 8 out of 10. For the regressions, knowledge scores were categorized as high (4–8, n = 19), moderate (2–3, n = 39), and low (0–1, n = 57). Results of the polytomous regressions are shown in Table 2. Women who acculturated more to the dominant society were one-and-a-half times more likely to have more knowledge of breast cancer risks than their less acculturated peers; however, the relationship was not statistically significant (OR = 1.63, P = .091). Controlling for marital status, education, and acculturation level, women with a high level of knowledge of breast cancer risk were twice as likely to have higher income (OR = 2.12, P = .014) and more education (OR = 2.327, P = .009) than those with a low level of knowledge. The most knowledgeable women were less likely to be married and less likely to have partners compared to the least knowledgeable group. Women who were in the moderate knowledge of breast cancer risk group were most likely to have a higher educational level (OR = 1.708, P = .024) compared to the group in the low knowledge level group, controlling for income, marital status, and acculturation level.
Table 2.
Knowledge of Breast Cancer Risk With Significant Predictors
| Knowledge Scores | Log (OR) | Standard Error | P | OR | 95% CI for OR
|
|
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| 4–8 | ||||||
| Intercept | −1.297 | 0.351 | .000 | |||
| Income | 0.752 | 0.307 | .014* | 2.120 | 1.161 | 3.873 |
| Marital status | −0.620 | 0.296 | .037* | 0.538 | 0.301 | 0.962 |
| Education | 0.845 | 0.324 | .009* | 2.327 | 1.233 | 4.393 |
| Acculturation | 0.485 | 0.287 | .091 | 1.625 | 0.926 | 2.849 |
| 2–3 | ||||||
| Intercept | −0.248 | 0.230 | .281 | |||
| Income | 0.06 | 0.235 | .798 | 1.062 | 0.670 | 1.682 |
| Marital status | −0.155 | 0.246 | .527 | 0.856 | 0.529 | 1.386 |
| Education | 0.535 | 0.237 | .024* | 1.708 | 1.073 | 2.719 |
| Acculturation | 0.276 | 0.230 | .231 | 1.317 | 0.839 | 2.067 |
Indicates significance at the .05 level (2-tailed test).
Discussion
Overall, the Chinese women in the dataset were not well acculturated: 75 of the 135 participants indicated that they still live more in the “Chinese” way instead of assimilating into the American culture. The results indicate that those Chinese women who evidenced greater acculturation into the American society had fewer healthcare access problems when seeking medical care. The relationship between acculturation level and knowledge of breast cancer risk was nonsignificant (P = .09). Among this first generation immigrant population, lack of acculturation also may pose an important barrier to medical care access and to undergoing cancer-screening tests. However, it is easy for Chinese in the New York City metropolitan area to continue to live in the “Chinese” way. All their daily activities can be undertaken within Chinatown. Within Chinatown, they can buy their Chinese foods, speak their language, and take shuttle buses to Brooklyn, Flushing, and other parts of Manhattan.
Health access and acculturation were also not significantly related, but the data did show that Chinese women who were more acculturated into the society tend to have fewer health-care access problems when they need medical attention. It is unsurprising that women who are more knowledgeable about the functioning of the healthcare system can access help from resources in their society more easily. For example, the more acculturated might have fewer communication problems with healthcare providers and might be more adept at making an appointment to see a doctor, thus cutting down on the waiting time.
Acculturation and general health practices were not significantly related in this sample of Chinese women. In addition, the level of acculturation was not significantly related to Chinese health practices and health beliefs. In other words, no matter how well they spoke English and regardless of the number of American friends they had, the Chinese women in this sample still tended to believe in Chinese medicine to some degree.
In this study, Chinese women sought traditional Chinese medicine no matter how acculturated they were to the society in the United States, suggesting that Chinese women who strongly believe in Chinese medicine tend to seek Chinese alternative medicine for treatment if they have healthcare needs. The results did show a high degree of correlation between Chinese health beliefs and Chinese health practices. For example, women who believe that acupuncture can cure their back pain will seek a traditional acupuncturist to take away the discomfort by placing fine needles in different “body channels.”
Polytomous logistic regression showed that income, marital status, and education significantly predicted knowledge of breast cancer risk (OR = 2.12, 0.59, and 2.33, respectively). Unexpectedly, length of stay in New York and insurance status did not influence the women’s knowledge of breast cancer risk. Thus, it would seem that the critical factor in gaining knowledge might be access to information about breast cancer prevention. It appears that Chinese women tend to rely on the physician’s suggestion to have the test but that they might not understand why they need to have the test.
Women who are married have less knowledge of breast cancer risk compared to women who are single. After marriage, Chinese women shift their focus from themselves to their family members. It is not surprising, therefore, that the married participants do not have much knowledge of breast cancer risk. Women, who have a higher educational level, have higher income, and are more acculturated into America society, tended to have a higher level of knowledge of breast cancer risks. The legal status and age did not have a significant relationship to breast cancer risk knowledge level.
Given the small sample size and a potential participant bias, the findings of this study involving Chinese women in New York City should be viewed as preliminary. These findings, therefore, may not be generalizable to the broader population of Chinese women in the United States. Although the sampling frame was designed to capture urban New York where there is a high density of Chinese, it is notable that previous research on Asian women in other US cities produced relatively similar results.2,4,8,9,11,12,17,18,34 This suggests that the findings of the study may be indicative of characteristics and relationships in Chinese communities elsewhere in the United States. The results suggest communities need to assess health-care resources to ascertain whether there are adequate numbers of Chinese-speaking providers and whether there are adequate numbers of female practitioners to support women as they try to access the use of Western medicine. There is a need to design more cost-effective programs by incorporating increased cross-cultural knowledge and expertise to tailor programs to specific populations and individualized care. Acknowledging cultural differences, paying attention to them, and tailoring care accordingly will increase nurses’ ability to be more critical in their assessments of the patients’ population to develop more accurate nursing care plans, and to increase the likelihood that appropriate outcomes will be used to evaluate care. With greater cultural competence, the specificity of care, and thereby the effectiveness, efficiency, and success in providing acceptable and optimal patient care, will increase. The results of this study can be used to guide the development of more appropriate and efficient care for Chinese women in the area of breast healthcare.
Acknowledgments
The study was supported by Foundation of The New York State Nurse Association, Center for Nursing Research, and 2001 Rita C. Kopf Memorial Research Grant. The preparation of the manuscript was partially supported by NIH-NINR T32-NR0708 (Holzemer, Project Director) and Center for Evidence-based Practice in the Underserved (NIH-NINR P20NR07799, S. Bakken, Principal Investigator).
References
- 1.Immigration Review. 5 million illegal immigrants. Immigration Rev. 1997;28:1–4. [Google Scholar]
- 2.Kagawa-Singer M. Socioeconomic and cultural influences on cancer care of women. Semin Oncol Nurs. 1995;11(2):109–119. doi: 10.1016/s0749-2081(05)80018-x. [DOI] [PubMed] [Google Scholar]
- 3.Kagawa-Singer M. Addressing issues for early detection and screening in ethnic populations. Oncol Nurs Forum. 1997;24(10):1705–1711. [PubMed] [Google Scholar]
- 4.McPhee SJ, Bird JA, Davis T, Ha NT, Jenkins CN, Le B. Barriers to breast and cervical cancer screening among Vietnamese–American women. Am J Prev Med. 1997;13(3):205–213. [PubMed] [Google Scholar]
- 5.US Census Bureau. Census 2000 redistricting data. U.S. Census Bureau; [Accessed March 21, 2001.]. Available at: http://www.census.gov/Press-Release/www/2001/tables/NewYork.xls. [Google Scholar]
- 6.Miller BA, Kolonel LN, Bernstein L, et al. Racial/Ethnic Patterns of Cancer in the United States 1988–1992. Bethesda, Md: National Cancer Institute; 1996. [Google Scholar]
- 7.National Cancer Institute. Knowledge, Attitudes, and Behavior of Immigrant Asian American Women Ages 40 and Older Regarding Breast Cancer and Mammography Screening. Bethesda, Md: National Cancer Institute; 1999. [Google Scholar]
- 8.Lee MM, Lee F, Stewart S, McPhee S. Cancer screening practices among primary care physicians serving Chinese Americans in San Francisco. West J Med. 1999;170(3):148–155. [PMC free article] [PubMed] [Google Scholar]
- 9.Lee MM, Lin SS, Wrensch MR, Adler SR, Eisenberg D. Alternative therapies used by women with breast cancer in four ethnic populations. J Nat Cancer Inst. 2000;92(1):42–47. doi: 10.1093/jnci/92.1.42. [DOI] [PubMed] [Google Scholar]
- 10.Lee M, Lee F, Stewart S. Pathways to early breast and cervical detection for Chinese American women. Health Educ Q. 1996;23(suppl):S76–S88. [Google Scholar]
- 11.McPhee SJ, Bird JA, Ha N-T, Jenkins CNH, Fordham D, Le B. Pathways to early cancer detection for Vietnamese women: Suc Khoe La Vang! (Health is gold) Health Educ Q. 1996;23(suppl):S60–S75. [Google Scholar]
- 12.McPhee SJ, Stewart S, Brock KC, Bird JA, Jenkins CN, Pham GQ. Factors associated with breast and cervical cancer screening practices among Vietnamese American women. Cancer Detect Prev. 1997;21(6):510–521. [PubMed] [Google Scholar]
- 13.Yu H, Harris RE, Gao YT, Gao R, Wynder EL. Comparative epidemiology of cancers of the colon, rectum, prostate and breast in Shanghai, China versus the United States. Int J Epidemiol. 1991;20(1):76–81. doi: 10.1093/ije/20.1.76. [DOI] [PubMed] [Google Scholar]
- 14.Mo B. Modesty, sexuality, and breast health in Chinese-American women. West J Med. 1992;157(3):260–264. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S. Fat, fatigue and the feminine: the changing cultural experience of women in Hong Kong. Cult Med Psychiatry. 1999;23(1):51–73. doi: 10.1023/a:1005451614729. [DOI] [PubMed] [Google Scholar]
- 16.Johnson BE. Women’s Health Care Handbook. 2. Philadelphia: Hanley & Belfus; 2000. [Google Scholar]
- 17.Kagawa-Singer M, Wellisch DK, Durvasula R. Impact of breast cancer on Asian American and Anglo American women. Cult, Med Psychiatry. 1997;21(4):449–480. doi: 10.1023/a:1005314602587. [DOI] [PubMed] [Google Scholar]
- 18.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer. 2000;89(3):696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 19.Berry JW. Immigration, acculturation, and adaptation. Appl Psychol Int Rev. 1997;46(1):5–68. [Google Scholar]
- 20.World Health Organization. Social Dimensions of Mental Health. Geneva: World Health Organization; 1981. [Google Scholar]
- 21.Svebak S, Apter MJ. Stress & Health: A Reversal Theory Perspective. Washington, DC: Taylor & Francis; 1997. [Google Scholar]
- 22.Tsunoda T, Parrish KM, Higuchi S, et al. The effect of acculturation on drinking attitudes among Japanese in Japan and Japanese Americans in Hawaii and California. J Stud Alcohol. 1992;53(4):369–377. doi: 10.15288/jsa.1992.53.369. [DOI] [PubMed] [Google Scholar]
- 23.Takenaka K, Zaichkowsky LD. Physiological reactivity in acculturation: a study of female Japanese students. Issues Ment Health Nurs. 1990;70(2):503–513. doi: 10.2466/pms.1990.70.2.503. [DOI] [PubMed] [Google Scholar]
- 24.Williams CL, Berry JW. Primary prevention of acculturative stress among refugees. Application of psychological theory and practice. Am Psychol. 1991;46(6):632–641. doi: 10.1037//0003-066x.46.6.632. [DOI] [PubMed] [Google Scholar]
- 25.English PB, Kharrazi M, Guendelman S. Pregnancy outcomes and risk factors in Mexican Americans: the effect of language use and mother’s birthplace. Ethn Dis. 1997;7(3):229–240. [PubMed] [Google Scholar]
- 26.Hattar-Pollara M, Meleis AI. The stress of immigration and the daily lived experiences of Jordanian immigrant women in the United States. West J Nurs Res. 1995;17(5):521–539. doi: 10.1177/019394599501700505. [DOI] [PubMed] [Google Scholar]
- 27.Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4(4):101–107. discussion 108–110. [PubMed] [Google Scholar]
- 28.Perez-Stable EJ, Otero-Sabogal R, Sabogal F, Napoles-Springer A. Pathways to early cancer detection for Latinas: En Accion Contra El Cancer. Health Educ Q. 1996;23(suppl):S41–S59. [Google Scholar]
- 29.Pasick RJ, Sabogal F, Bird JA, et al. Problems and progress in translation of health survey questions: the pathways experience. Health Educ Q. 1996;23(suppl):S28–S40. [Google Scholar]
- 30.Pasick RJ, D’Onofrio CN, Otero-Sabogal R. Similarities and difference across cultures: questions to inform a third generation for health promotion research. Health Educ Q. 1996;23(suppl):S142–S161. [Google Scholar]
- 31.Sabogal F, Otero-Sabogal R, Pasick RJ, Jenkins CNH, Perez-Stable EJ. Printed health education materials for diverse communities: suggestions learned from the field. Health Educ Q. 1996;23(suppl):S123–S141. [Google Scholar]
- 32.Bird JA, Otero-Sabogal R, Ha N-T, McPhee SJ. Tailoring lay health worker interventions for diverse cultures: lessons learned from Vietnamese and Latina communities. Health Educ Q. 1996;23(suppl):S105–S122. [Google Scholar]
- 33.Engelstad L, Bedeian K, Schorr K, Stewart S. Pathways to early detection of cervical cancer for a multiethnic, indigent, emergency department population. Health Edu Q. 1996;23(suppl):S89–S104. [Google Scholar]
- 34.Yi JK. Are Asian/Pacific Islander American women represented in women’s health research? [letter] Womens Health Issues. 1996;6(4):237–238. doi: 10.1016/1049-3867(96)00013-8. [DOI] [PubMed] [Google Scholar]