Abstract
High blood pressure disproportionately affects African American adults and is a leading cause of stroke and heart attack. Engaging in recommended levels of physical activity reduces blood pressure, and social and physical environmental supports for physical activity may increase engagement in physical activity. Based on social cognitive theory within a bioecological framework, the present study tested hypotheses that perceived peer social support for physical activity and neighborhood walkability would be positively associated with physical activity, and that physical activity would mediate their relation with blood pressure. Baseline data were collected with 434 African American adults in underserved communities (low income, high crime) participating in the Positive Action for Today's Health (PATH) trial. Perceived peer social support for physical activity and neighborhood walkability were measured with validated surveys. Physical activity was assessed with 7-day accelerometry (moderate-to-vigorous physical activity, min/day) and with a 4-week recall of walking. Three blood pressure assessments were taken by trained staff using standard protocols, with values from the second and third assessments averaged. The sample was predominantly female (63%), overweight (mean body mass index=30.9, SD=8.4), and had slightly elevated blood pressure with a mean systolic blood pressure of 132.4 (SD=17.9) and a mean diastolic blood pressure of 81.4 (SD=11.0). Results demonstrated that peer social support for physical activity (B=2.43, p=.02) and neighborhood walkability (B=2.40, p=.046) were significantly related to average daily moderate-to-vigorous physical activity. Neighborhood walkability was also significantly associated with self-reported average daily walking (B=8.86, p=.02). Physical activity did not mediate their relation with blood pressure and no significant direct effects of these variables on blood pressure were found. The positive influence of social and physical environmental supports on physical activity in underserved African American communities may guide intervention efforts and contribute to our understanding of physical activity and related health outcomes.
Keywords: physical activity, social support, neighborhood walkability, blood pressure, African American
Introduction
African Americans are disproportionately affected by cardiovascular disease, with low levels of physical activity (PA) and high rates of hypertension linked to this disparity (Roger et al., 2012). Social and physical environmental factors may impact PA and indirectly influence blood pressure (BP) and cardiovascular health (Geronimus, 2000; Thorpe, Brandon, & LaVeist, 2008). Additionally, these factors may be particularly important in underserved African American communities which historically experience greater or more complex environmental barriers to PA and related increased risk of cardiovascular health problems (Cutts, Darby, Boone, & Brewis, 2009; Eugeni, Baxter, Mama, & Lee, 2011; Minor, Wofford, & Jones, 2008; Ofili, 2001). A better understanding of links among relevant environmental factors, PA, and BP may therefore inform public health efforts to support positive health behaviors such as PA, and to reduce CVD health disparity experienced by African Americans.
Ecological theory presents a multilevel conceptual framework through which complex, interactive processes among social and physical environmental factors and health behaviors affect health outcomes (Tudge, Mokrova, Hatfield, & Karnik, 2009), and a growing body of literature asserts that its application is necessary to advance the study of PA and fully understand its effects on outcomes like BP (King et al., 2006; Stokols, 1996; Tu & Ko, 2008). Additionally, it has been noted that neighborhood features and the built environment should be considered in the study of environmental justice issues and their impact on health in minority communities, which historically have had to cope with numerous environmental injustices (Cutter, 1995; Greenberg & Renne, 2005; Scott & Wilson, 2011). While ecological theory is comprehensive and broadly applicable, it does not necessarily inform directionality of relations between the environment, health behaviors, and health outcomes, and thus social cognitive theory (SCT) may be integrated to inform hypotheses. SCT assumes that individual behaviors influence health outcomes and are critically affected by the social and physical environmental contexts which they are exposed to, indicating a potential causal pathway for understanding environmental influences on health (Bandura, 2004).
Two key social and physical environmental factors have been consistently linked to PA both generally and in African American adults: 1) social support for PA, and 2) neighborhood walkability (Eyler et al., 2002; Fleury & Lee, 2006; Owen, Humpel, Leslie, Bauman, & Sallis, 2004; Wendel-Vos, Droomers, Kremers, Brug, & van Lenthe, 2007). Social support for PA characterizes the extent to which peers provide companionship, encouragement, and/or functional supports for PA (Cohen & Wills, 1985). Higher levels of general social support for PA, as well as specific instrumental/tangible, informational, emotional, and appraisal supports, have been linked to increased PA, and these associations are present across varied types of PA (e.g. sport, leisure) and in some studies of African American women (Ainsworth, Wilcox, Thompson, Richter, & Henderson, 2003; Eyler et al., 1999; Kanu, Baker, & Brownson, 2008; Sharma, Sargent, & Stacy, 2005; Wilbur, Chandler, Dancy, & Lee, 2003). In the present study, peer support for PA was targeted because a number of studies have found peer support to be more influential than family support (Hemmingsson, Hellenius, Ekelund, Bergstrom, & Rossner, 2008; Sharma, et al., 2005; Wilbur, et al., 2003), more stable over time (Resnick, Orwig, Magaziner, & Wynne, 2002), and potentially more relevant in female populations (Hovell et al., 1989). It is noteworthy that these relations remain unclear in African American men residing in underserved communities, likely due in part to the noted difficulties of engaging men in health-related research (Patsdaughter, Christensen, Kelley, Masters, & Ndiwane, 2001).
Neighborhood walkability refers to access to physical spaces and neighborhood features (e.g. the presence of adequate sidewalks), which are conducive to engaging in PA and walking. Studies of neighborhood walkability demonstrate that positive safety, traffic, and neighborhood aesthetic environments are consistently associated with higher levels of PA (Duncan, Spence, & Mummery, 2005; Pikora et al., 2006; Sallis, King, Sirard, & Albright, 2007; Van Dyck et al., 2010; Wilcox, Bopp, Oberrecht, Kammermann, & McElmurray, 2003), both globally (Sallis et al., 2009) and in studies of multiethnic samples (Addy et al., 2004; Ainsworth, et al., 2003; Wilson, Kirtland, Ainsworth, & Addy, 2004). Because social support for PA and neighborhood walkability have been consistently linked to PA, they were targeted in the present study.
Social and physical environmental factors influence PA, and may therefore indirectly influence BP as part of a potential etiologic pathway, consistent with an ecological framework and SCT. Indeed the link between PA and BP is well established, with increased PA linked to decreased casual BP. Estimates of this effect indicate that engaging in PA can reduce systolic and diastolic BP in the general population by 4.2 mmHg and 2.9 mmHg, respectively, and that African Americans may experience even greater PA-related reductions of 6.2 mmHg systolic BP and 11.0 mmHg diastolic BP (He & Whelton, 1999; Whelton, Chin, Xin, & He, 2002). Evidence for a strong beneficial effect of PA on BP warrants the investigation of direct and indirect effects which may link environmental supports through statistical mediation (Baranowski, Anderson, & Carmack, 1998; Bauman, Sallis, Dzewaltowski, & Owen, 2002; MacKinnon & Luecken, 2008). While a few studies have investigated PA as a mediator linking environmental factors and BP or related health outcomes (Chaix et al., 2010; Fischer Aggarwal, Liao, & Mosca, 2008; Mowen, Orsega-Smith, Payne, Ainsworth, & Godbey, 2007), the literature is limited and findings have been mixed.
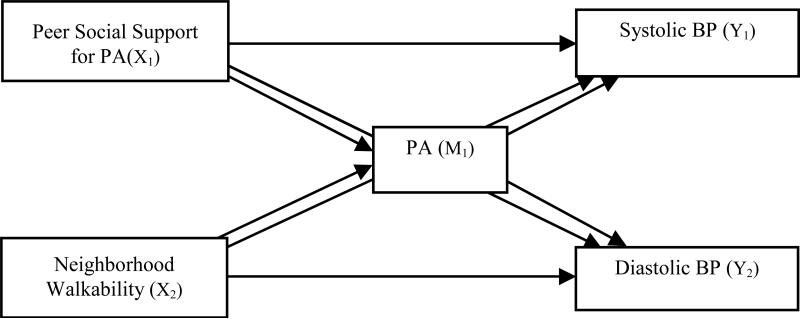
The primary aim of this study was to examine whether peer social support for PA and neighborhood walkability were related to accelerometry-estimated MVPA and BP within African American communities, as part of the Positive Action for Today's Health (PATH) randomized trial. PA was also investigated as a mediator to explore indirect pathways through which the environmental supports might influence BP, with accelerometry used to provide an accurate assessment of general PA (Esliger & Tremblay, 2006). A secondary aim was to examine these relations with participants’ self-reported walking and exercise PA over four weeks; accelerometry-estimated PA quantifies only total minutes of PA, and does not quantify PA by type (e.g. walking, exercising). Based on an ecological framework and SCT, it was hypothesized that peer support for PA and neighborhood walkability would be positively associated with MVPA and reported walking, and inversely associated with BP (Figure). It was also hypothesized that PA would be inversely associated with BP and would mediate an indirect relation of peer support for PA and neighborhood walkability, with BP.
Figure.
Theoretical model.
Methods
Participants
Data were collected from 434 African American adults residing in three low-income communities located in the southeastern U.S. Communities were participating in the Positive Action for Today's Health (PATH) and were matched demographically using census data (e.g. poverty, ethnicity). Two recruitment strategies were used within each community, with participants initially recruited from a random list of households in specified census tracts in each targeted community, each receiving letters and follow-up phone calls. Of the 1986 households called, 770 did not answer. Of the 1216 persons reached, 581 declined participation and 734 individuals were invited to participate. Participants were also recruited through volunteer advertisements and by word of mouth. Approximately 54% of the final sample was recruited from the random list of households and 46% through volunteer advertisements and word of mouth. Individuals were included in the PATH sample if they met the following criteria: 1) African-American (three of four grandparents of African heritage), 2) ≥ 18 years of age, 3) no plans to move within two years as part of the larger intervention trial, 4) no medical condition that would limit participation in moderate intensity PA, including life-threatening illness (e.g., immobile, severely disabled, bedridden), 5) residing in specified census areas within one of three targeted communities, and 6) with controlled blood pressure (<180 mmHg systolic / <110 mmHg diastolic) and blood sugar levels (< 300 mg/dL non-fasting, ≤250 mg/dL fasting), as measured using a glucometer and Dinamap blood pressure apparatus with exclusionary criteria based on national recommendations for seeking emergency care (Chobanian et al., 2003; Franz et al., 2002). Participants were also excluded if they answered affirmatively to any item on the Physical Activity and Readiness Questionnaire (Thomas, Reading, & Shephard, 1992), indicating that they were could not safely participate in moderate PA. Participants signed informed consent and were compensated monetarily for their time, and the study was approved by the Institutional Review Board at the University of South Carolina.
Study Design and Procedures
The PATH randomized trial is described in detail elsewhere (Coulon et al., 2012; Wilson et al., 2010). Assessments were conducted in each of the three communities at baseline, 6, 12-, 18-, and 24-months between the years 2008 and 2010. Though the trial was a 2-year intervention, only data gathered during baseline assessments were included in this cross-sectional study.
During baseline assessments participants attended a 2-hour health screening during which BP, height, weight, waist circumference, and physical activity were measured by research staff. Survey assessment of psychosocial variables such as perceived peer social support for PA and neighborhood walkability was completed, and participants then received a monetary incentive. BP was measured by a registered nurse trained in the research protocol using a Dinamap BP apparatus (model 8100; Critikon Inc., Tampa, FL), as outlined by National High Blood Pressure Education Program Working Group on Hypertension Control (Pickering et al., 2005). Demographic information including age, sex, annual income, education status, occupation status, and marital status was collected.
Measures
Peer Social Support for PA
Items from the peer subscale of the Social Support for Exercise Habits Scale elicited responses to five items on a 5-point Likert scale. The subscale has an internal consistency of α=0.84 and criterion validity established as it correlates with self-reported PA (Sallis, Grossman, Pinski, Patterson, & Nader, 1987), and it has been used in African American samples (Resnick, et al., 2002).
Neighborhood Walkability
The Walking and Cycling subscale of the Neighborhood Environment Walkability Survey (NEWS) elicited responses to five items on a 4-point Likert scale. The subscale has an internal consistency of α=.79 and factorial and criterion validity has been established (Cerin, Conway, Saelens, Frank, & Sallis, 2009; Saelens, Sallis, Black, & Chen, 2002), and also validated against geographic information systems (GIS) measures (Adams et al., 2009).
Accelerometery-estimated MVPA
Accelerometry assessments of PA over 7 consecutive days were collected using Actical devices (Mini-Mitter, Bend, OR). Accelerometers are small electronic devices that measure intensity and frequency of movement (i.e. PA) by detecting accelerations within spatial planes (Esliger & Tremblay, 2006). Activity was categorized as MVPA if counts per minute were greater than or equal to 1075, based on data from a calibration study conducted within a sample matched to the PATH sample (Trumpeter et al., 2012). The final MVPA variable was quantified as minutes per day.
Four-Week History PA Questionnaire (FWH)
The FWH is a one-time self-report of PA that measures frequency and duration of specific types of PA over the previous four weeks, rather than measuring general PA. Walking and exercise activity variables were investigated and quantified as minutes per day spent walking or exercising. Previous research has demonstrated the reliability and validity of this measure in national studies (Ainsworth, Leon Richardson, Jacobs & Paffenbarger, 1993). Test-retest reliability has been high (r = .60), with correlations for moderate intensity activities consistent with reliability studies of other PA questionnaires (Ainsworth, Leon, Richardson, Jacobs, & Paffenbarger, 1993; Pereira et al., 1997).
Blood Pressure
BP was measured by a registered nurse trained using a Dinamap BP apparatus (model 8100; Critikon Inc., Tampa, FL). Participants were seated in a relaxed position with legs uncrossed, and the appropriately-sized cuff was placed on the left arm. Participants had a 5-minute resting period and then three BP readings were taken with one minute passing between each. The average of the second and third readings was used for analyses given evidence that the initial BP reading is often elevated due to reactivity or a “white coat effect” (Pickering, et al., 2005). Blood pressure medication status was quantified by indexing whether participants had been prescribed medication and whether they were taking it as directed by their physicians.
Analytic Plan
Direct and indirect effects of peer social support for PA and neighborhood walkability were tested within a mediation framework. Accelerometry-estimated MVPA and reported FWH PA data were positively skewed and were log-transformed. Both transformed and untransformed MVPA were tested in the models, and given the benefits of retaining original metrics, analytic results obtained using untransformed data were reported since they did not differ from results based on transformed data. Models were also tested with outliers, influential cases, and participants with less than one half of a day of accelerometry data excluded; these cases did not affect results and were therefore included in final analyses. Variables not of theoretical interest but that demonstrated large correlations (r ≥ 0.37; Cohen, 1988) with targeted variables were entered as control variables, including age, sex, BP medication status, and BMI. Given the nested design of the study within three communities, community was also entered as a control variable; statistical approaches which rely on multi-level modeling or the estimation of cluster-robust standard errors to handle nested data are reliable only with cluster-level samples of N≥50 (Kezdi, 2003; Maas & Hox, 2004; Nichols & Schaffer, 2007). Communities were also matched demographically, and low intraclass correlation coefficients (e.g. 0.007 - 0.030) have been found in previous studies for which PA and BP were outcomes (Gulliford, Ukoumunne, & Chinn, 1999; Hannan, Murray, Jacobs, & McGovern, 1994).
The product of coefficients method for testing statistical mediation was applied using MPlus Version 5.2 (Muthén & Muthén, Los Angeles, LA), with percentile bootstrapping implemented to adjust asymmetric confidence limits and address biased standard errors (Fairchild, Mackinnon, Taborga, & Taylor, 2009; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). This method provides a balance of power and Type I error and supports the use of mediation when there may not be strong predictor-outcome associations, whereas the causal steps and difference in coefficients methods are less advisable for relatively smaller samples, and are more susceptible to Type II errors (Fairchild & MacKinnon, 2009; Fritz & MacKinnon, 2007; MacKinnon, et al., 2002). The product of coefficients method involves regression of outcomes on the mediator and predictors, and regression of the mediator on the predictors, yielding two coefficients that link predictors to the mediator and the mediator to the outcome, with the product of these coefficients providing an estimate of the mediated indirect effect (αβ). Thus, PA (M1) was regressed on peer social support for PA (X1), neighborhood walkability (X2), and control variables, and SBP (Y1) and DBP (Y2) were regressed on PA (M1), peer social support for PA (X1), neighborhood walkability (X2), and control variables, as in the Figure and equations:
| Equation 1 |
| Equation 2 |
The mediated indirect effect (αβ) was then divided by bootstrapped standard errors to test for statistical significance and direct effects (τ’) were also computed. The approach was powered at 1-β>.80 with α=.05, and the r2 measure of the mediated effect was used to indicate the variance accounted for by the mediator (MacKinnon & Luecken, 2008). Missing data were addressed using full information maximum likelihood estimation (FIML), which provides more accurate type 1 error rates than listwise or pairwise deletion and results in a response pattern most similar to multiple imputation (Acock, 2005; Enders & Bandalos, 2001).
Results
Sample Characteristics
Demographic data are reported in Table 1. The sample was predominantly female (63%) with a substantial representation of males (37%), was overweight (MBMI30.88, SD=8.43), and had a mean age of 51 years (SD=16). Communities differed slightly by age and education status (Wilson, et al., 2010). Twelve participants, or 3% of the sample, were excluded from primary analyses due to missing data for predictor variables in the models, resulting in a final sample of N=422.
Table 1.
Sample Characteristics with N(%) in Total and by Community.
| Community A | Community B | Community C | Total | |
|---|---|---|---|---|
| N (%) | 133 (28) | 164 (38) | 137 (32) | 434 |
| Gender | ||||
| Male | 44 (33) | 57 (35) | 61 (44) | 162 (37) |
| Female | 89 (67) | 107 (65) | 76 (56) | 272 (63) |
| Agea | ||||
| Mean (SD) | 54.18 (15.58) | 48.14 (15.64) | 51.85 (15.39) | 51.19 (15.68) |
| 18-24 | 8 (6) | 15 (9) | 10 (7) | 33 (8) |
| 25-44 | 22 (17) | 52 (32) | 28 (20) | 102 (24) |
| 45-64 | 67 (50) | 70 (42) | 70 (51) | 207 (48) |
| 65+ | 36 (27) | 27 (17) | 29 (21) | 92 (21) |
| Employmenta | ||||
| Working | 38 (29) | 71 (43) | 60 (44) | 169 (39) |
| Unemployed | 29 (22) | 32 (20) | 24 (18) | 85 (20) |
| Retired | 39 (29) | 26 (16) | 29 (21) | 94 (22) |
| Disabled | 7 (5) | 19 (12) | 9 (7) | 36 (8) |
| Other | 19 (14) | 16 (10) | 14 (10) | 49 (11) |
| No Response | 1 (.5) | 0 ( 0) | 1 (.5) | 2 (1) |
| Marital Status | ||||
| Married | 36 (27) | 32 (20) | 32 (23) | 100 (23) |
| Separated | 18 (14) | 20 (12) | 21 (15) | 59 (14) |
| Divorced | 16 (12) | 18 (11) | 15 (11) | 49 (11) |
| Widowed | 30 (23) | 27 (17) | 24 (18) | 81 (19) |
| Never Married | 23 (17) | 54 (33) | 34 (25) | 111 (26) |
| Unmarried Couple | 9 (7) | 13 (8) | 9 (7) | 31 (7) |
| No Response | 1 (1) | 0 (0) | 2 (1) | 3 (1) |
| Education | ||||
| <High School Degree | 36 (27) | 43 (26) | 39 (29) | 118 (27) |
| High School Degree/GED | 49 (37) | 76 (46) | 49 (36) | 174 (40) |
| >High School Degree | 45 (34) | 43 (26) | 44 (32) | 132 (30) |
| No Response | 3 (2) | 2 (1) | 5 (4) | 10 (2) |
| Income | ||||
| <$10 K | 42 (32) | 42 (26) | 41 (30) | 125 (29) |
| $10-24 K | 43 (32) | 61 (37) | 41 (30) | 145 (33) |
| $25-39 K | 24 (18) | 24 (15) | 29 (21) | 77 (18) |
| ≥$40 K | 20 (15) | 27 (17) | 16 (12) | 63 (15) |
| No Response | 4(3) | 10 (6) | 10 (7) | 24 (6) |
| Health Factors | ||||
| BMI | ||||
| Mean (SD) | 31.05 (7.93) | 30.26 (8.34) | 31.40 (9.03) | 30.88 (8.43) |
| < 25 | 30 (23) | 49 (30) | 33 (24) | 112 (26) |
| 25-30 | 34 (26) | 40 (24) | 31 (23) | 105 (24) |
| >30 | 67 (50) | 73 (45) | 71 (52) | 211 (49) |
| Waist Circumference | ||||
| Mean (SD) | 97.24 (16.15) | 95.47 (18.91) | 98.28 (18.59) | 96.78 (18.16) |
| Men, > 102 cm | 17 (39) | 16 (28) | 21 (34) | 54 (12) |
| Women, > 88 cm\ | 60 (67) | 74 (69) | 61 (80) | 195 (45) |
| Blood Pressure | ||||
| Medication Statusa | ||||
| Not medicated | 63 (47) | 96 (59) | 67 (49) | 226 (52) |
| Meds adherent | 33 (25) | 22 (13) | 39 (28) | 94 (22) |
| Meds nonadherent | 0 (0) | 0 (0) | 1 (1) | 1 (0) |
| No data | 37 (28) | 46 (28) | 30 (22) | 113 (26) |
Note: Demographics reported as number (percentage), with age and health factors reported as mean (standard deviation).
Significant differences (p<.05) between community demographics were found for age, employment status, and blood pressure medication status.
Descriptive data for the predictors, mediators, and outcomes of substantive interest are presented in Table 2. On average, participants engaged in approximately 21 minutes of MVPA each day (SD=26.3), though data were positively skewed, and median MVPA was 13 minutes daily. Participants reported engaging in an average of 37 minutes of walking and 19 minutes of exercise daily through FWH measures. Participants had elevated blood pressure values (MSBP=132.37, SD=17.89; MDBP=81.39, SD=10.96), and mean scores for social and environmental measures typically fell within the mid-range of the 4- or 5-point response scales, with slight indication of more positive perceptions of neighborhood environmental supports. MVPA, reported walking, and reported exercise differed significantly by community (p≤.01), with Community B differing from the other two communities (Table 2).
Table 2.
Descriptive Statistics with Mean (SD) in Total and by Community for Model Variables.
| Community A | Community B | Community C | Total | |
|---|---|---|---|---|
| Friend Social Support | 2.35 (.96) | 2.52 (1.03) | 2.61 (1.06) | 2.50 (1.03) |
| Walkability | 2.31 (.34) | 2.33 (.80) | 2.35 (.86) | 2.33 (.84) |
| MVPA/Day | 19.67 (30.36) | 23.01 (31.77) | 19.73 (22.58) | 21.42 (26.29) |
| Reported Walking/Daya | 32.94 (41.41) | 28.37 (57.13) | 49.02 (71.55) | 36.96 (58.25) |
| Reported Exercise/Daya | 18.17 (29.88) | 15.81 (27.30) | 20.19 (38.90) | 19.03 (32.38) |
| SBP | 131.14 (17.15) | 131.05 (18.90) | 134.96 (16.98) | 132.37 (17.89) |
| DBP | 80.11 (10.77) | 80.62 (11.22) | 83.67 (10.49) | 81.39 (10.96) |
Denotes significant differences by community at p≤ .01.
Analyses
Correlations were significant and in the expected directions linking neighborhood walkability with MVPA and peer social support for PA. MVPA was also linked inversely with SBP and positively with younger age, being male, having a lower BMI, and not being medicated for BP. Higher SBP was associated with older age, higher BMI, and not taking BP medications, while higher DBP was only associated with being male. Results indicated that the primary model accounted for 35% of the variance in MVPA (r2=.35), and 12% and 2% of the variance in SBP (r2=.12) and DBP (r2=.02), respectively.
Direct Effects
MVPA was associated with social support for PA (B=2.40, p=.02) and neighborhood walkability (B=2.43, p=.046), with a 1-unit increase in peer social support for PA and neighborhood walkability related to a 2-minute increase in daily MVPA (Table 3). Reported walking was associated with neighborhood walkability (B=8.86, p=.02), with a 1-unit increase in neighborhood walkability related to a 9-minute increase in reported daily walking. Social support for PA, neighborhood walkability, MVPA, and reported walking did not predict SBP or DBP.
Table 3.
Results of Primary Analyses for MVPA as a Mediator Relating Peer Social Support for PA and Neighborhood Walkability with SBP and DBP (N = 434).
| Variable | B | SE | t | p | LCL | UCL | R 2 |
|---|---|---|---|---|---|---|---|
| MVPA (M1) on Peer Support and Walkability with Control Variables | |||||||
| Intercept (I1) | 54.81 | 8.88 | 6.17 | .00 | 37.19 | 72.19 | |
| Age (C1) | -.37 | .10 | -3.88 | .00 | -.55 | -.18 | |
| Sex (C2) | -19.32 | 2.99 | -6.47 | .00 | -25.14 | -13.54 | |
| BP Med Status (C3) | -3.03 | 2.65 | -1.14 | .25 | -8.17 | 2.24 | .350 |
| BMI (C4) | -.54 | .12 | -4.45 | .00 | -.78 | -.31 | |
| Community (C5) | 1.68 | 1.52 | 1.11 | .27 | -1.16 | 4.76 | |
| Peer Support (X1) | 2.40 | 1.06 | 2.26 | .02 | .22 | 4.47 | |
| Walkability (X2) | 2.43 | 1.22 | 1.99 | .05 | .02 | 4.79 | |
|
SBP (Y1) on PA, Peer Support and Walkability with Control Variables | |||||||
| Intercept (I1) | 113.55 | 6.53 | 17.39 | .00 | 100.93 | 126.91 | |
| Age (C1) | .28 | .07 | 4.24 | .00 | .14 | .40 | |
| Sex (C2) | -4.31 | 2.02 | -2.13 | .03 | -8.41 | -.50 | |
| BP Med Status (C3) | 3.30 | 2.31 | 1.43 | .15 | -1.20 | 7.93 | |
| BMI (C4) | .28 | .11 | 2.49 | .01 | .07 | .51 | .122 |
| Community (C5) | -.53 | 1.09 | -.49 | .62 | -2.60 | 1.65 | |
| PA (M1) | -.03 | .04 | -.68 | .49 | -.11 | .05 | |
| Peer Support (X1) | -.33 | .81 | -.40 | .69 | -1.91 | 1.23 | |
| Walkability (X2) | -.14 | .98 | -.15 | .88 | -2.05 | 1.81 | |
|
DBP on PA, Peer Support and Walkability with Control Variables | |||||||
| Intercept (I1) | 83.08 | 3.83 | 21.70 | .00 | 75.48 | 90.37 | |
| Age (C1) | .02 | .04 | .37 | .71 | -.07 | .10 | |
| Sex (C2) | -2.40 | 1.34 | -1.80 | .07 | -5.09 | .31 | |
| BP Med Status (C3) | .70 | 1.45 | .48 | .63 | -2.09 | 3.47 | |
| BMI (C4) | .04 | .07 | .52 | .61 | -.09 | .17 | .022 |
| Community (C5) | -1.27 | .68 | -1.86 | .06 | -2.56 | .17 | |
| PA (M1) | -.01 | .03 | -.33 | .74 | -.07 | .05 | |
| Peer Support (X1) | -.06 | .53 | -.12 | .91 | -1.14 | .98 | |
| Walkability (X2) | .18 | .64 | .28 | .78 | -1.05 | 1.41 | |
Note: MVPA= accelerometry-estimated physical activity; SBP=systolic blood pressure; DBP=diastolic blood pressure; BMI=body mass index; SE=standard error; DF=degrees of freedom; LCL=lower confidence limit; UCL=upper confidence limit; Mediated indirect (αβ) and direct (τ’) effects not shown; all effects were non-significant with r2<.001.
* = p < .05, ** = p < .01
aValues of r2 are based on semi-partial correlations and thus represent the amount of variance in an outcome accounted for by a predictor, exclusive of overlap with other predictors.
Indirect Effects
The mediated effects of MVPA and reported walking (αβ) were not statistically significant, with r2 values for mediated effects indicating that PA accounted for 0% of variance among supports for PA and BP.
Discussion
Social and physical environmental perceptions of peer social support for PA and neighborhood walkability were related to greater MVPA measured via accelerometry, in a sample of African American adults residing in underserved communities. Neighborhood walkability was also linked to reported walking, supporting previous evidence of the consistent relation of neighborhood walkability with PA behaviors. Neither environmental supports nor PA were associated with BP, and PA therefore did not mediate an indirect relation of peer social support for PA and neighborhood walkability with BP.
While findings that peer social support for PA and neighborhood walkability significantly influence PA are consistent with previous studies, this is the first to examine these effects in African American adults residing in underserved communities, using two distinct measures of PA. Though the magnitudes of the effects of peer social support for PA and neighborhood walkability on PA were not large (increases of 2-9 minutes of daily MVPA or reported walking), the potential public health impact should not be understated, as small effects can result in clinically meaningful improvements in population estimates of health. For example, meeting daily PA recommendations has been linked to an average decrease of 10.96 mm Hg in African American adults, independent of weight loss (Whelton, et al., 2002). Additionally, previous studies have often examined whether PA is increased by the presence of environmental supports (e.g. by investigating the likelihood that individuals will exercise or meet PA recommendations), and thus, these findings present supplemental data that indicate to what extent PA might be increased (e.g. 2-9 minutes of daily MVPA).
These findings are consistent with similar mediation models that have produced mixed results (Baruth et al., 2010; Chaix, et al., 2010; Fischer Aggarwal, et al., 2008; Mowen, et al., 2007). Additionally, it is not surprising that the PA mediator accounted for 0% of the variance among PA supports and BP since no covariation was found between these variables. It should be noted however that small correlations between supports for PA and PA, and between PA and SBP, do provide some support for the indirect pathways hypothesized.
Also consistent with the previous research (Ham & Ainsworth, 2010), reported walking was higher than MVPA measured via accelerometry, with results positively skewed, and lower levels of MVPA may have resulted in a lack of variability or intensity needed to detect relations among PA and BP. Future studies might increase power to detect effects by investigating relations only among participants engaging in substantial amounts of PA or in exercise bouts of PA, a strategy which this study was not statistically powered to implement.
Investigation of such pathways is important given the high prevalence of CVD and related mortality, and that minority health disparities may be driven in part by issues of environmental injustice (Gadegbeku, Lea, & Jamerson, 2005). It has been theorized that socioeconomically disadvantaged persons experience chronic environmental stress, increased barriers to engaging in positive health behaviors (e.g. PA), adverse physiologic functioning, cardiovascular “wear and tear”, and ultimately high BP and CV (Anderson, 1998; Matthews & Gallo, 2011; Steptoe & Marmot, 2002). Furthermore, estimated health care costs due to physical inactivity can greatly outweigh the costs of creating walkable neighborhoods (Wang et al., 2004), and African American communities have reported that they would be more active if their neighborhoods were more walkable (Greenberg & Renne, 2005; Griffin, Wilson, Wilcox, Buck, & Ainsworth, 2008; Wilson, et al., 2004). Additionally, achievement of national health equity and reducing health disparities is a top priority for the Healthy People 2020 initiative (Koh, 2010; U.S. Department of Health and Human Services, 2011), and calls for a comprehensive approach to understanding and addressing community-wide health risk (Gibbons, 2008). Thus, continued investigation of the impact of environmental factors on PA and BP is recommended to develop efficacious strategies to prevent high BP and CVD, and to reduce minority health disparities.
Limitations of the study should be considered. The nested, cross-sectional design does not afford causal inference and it cannot be assumed that findings were entirely unaffected by community-level differences among model variables; under certain circumstances this can result in biased parameter estimates and standard errors within a mediation framework. Additionally, effects found in this cross-sectional study could be bidirectional, such that more physically active individuals are more likely to choose more walkable neighborhoods to reside in. It should be noted however that all available methodological and statistical controls for such threats were applied. Additionally, while medication status was assessed and the final variable included information on adherence, few individuals reported nonadherence to their medication regimen. Given the difficulties of measuring the influence of medication, it is possible that relations between blood pressure and physical activity and social environmental factors, which may be small in magnitude, were confounded. Finally, it should be noted that there may be limitations to the generalizability of these findings given that 46% of the sample was comprised of volunteers, and that the sample was nested within three communities, with the design not affording a multilevel model to examine community-level variation.
This study has a number of important strengths. The sample of African American adults recruited from underserved communities was large, diverse in age, included a relatively high proportion of males, and represents a population that experiences considerable barriers to PA and CVD health disparity. As noted previously, African American men often comprise small proportions of research samples, and studies investigating the effects of social support for PA and neighborhood walkability on PA and health outcomes have often focused on women. These findings therefore provide novel evidence that these environmental effects are present for men as well. This study was also theory-based, and adds to the literature by presenting and testing a comprehensive model for understanding one pathway by which the environment may ultimately influence health. Finally, this study included two measures of PA, one objective (accelerometry), and the effects of neighborhood walkability were consistent across both.
Future investigations of potential pathways among environmental factors, health behaviors, and cardiovascular health outcomes may include longitudinal designs and additional measures of the environment (e.g. GIS, access to places and services to walk to) and health outcomes (e.g. BMI, cardiometabolic risk). Given evidence that environmental stressors such as exposure to crime are relevant to health behaviors, health outcomes, and issues of environmental justice (Ford, Kim, & Dancy, 2009; Foster, Giles-Corti, & Knuiman, 2010; Kamphuis et al., 2010), testing interactions among such environmental supports and stressors may be important and would be consistent with classic psychosocial theories of health (Cohen, 1988). It is also interesting to note that despite thorough strategies for matching the three communities on demographic- and health-related characteristics, one community differed by average blood pressure and reported physical activity. Future investigations that include more communities and robust measures as those noted above may lend insight into why such differences might occur, and their implications for intervention effectiveness.
In summary, the results of this study present the role of social and physical environmental factors, specifically peer social support and neighborhood walkability, in influencing PA. This study also represents one of the first attempts to investigate such relations as they influence BP within a mediation design. Future investigations may build on these findings to better understand the potential etiology of chronic diseases such as high BP in African American adults, and to reduce CVD health disparities experienced by underserved communities.
Research Highlights.
We report associations among environmental supports, physical activity, and blood pressure in African American adults
Neighborhood walkability and social support for physical activity were linked to 2-9 more minutes of daily activity
Neither environmental supports nor physical activity were related to blood pressure as part of a mediation pathway
Findings contribute to a greater understanding of health behaviors and potential etiologic pathways for high blood pressure
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67(4):1012–1028. [Google Scholar]
- Adams MA, Ryan S, Kerr J, Sallis JF, Patrick K, Frank LD, et al. Validation of the Neighborhood Environment Walkability Scale (NEWS) items using geographic information systems. J Phys Act Health. 2009;6(Suppl 1):S113–123. doi: 10.1123/jpah.6.s1.s113. [DOI] [PubMed] [Google Scholar]
- Addy CL, Wilson DK, Kirtland KA, Ainsworth BE, Sharpe P, Kimsey D. Associations of perceived social and physical environmental supports with physical activity and walking behavior. Am J Public Health. 2004;94(3):440–443. doi: 10.2105/ajph.94.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth BE, Leon AS, Richardson MT, Jacobs DR, Paffenbarger RS. Accuracy of the college alumnus physical activity questionnaire. Journal of Clinical Epidemiology. 1993;46(12):1403–1411. doi: 10.1016/0895-4356(93)90140-v. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Wilcox S, Thompson WW, Richter DL, Henderson KA. Personal, social, and physical environmental correlates of physical activity in African-American women in South Carolina. Am J Prev Med. 2003;25(3 Suppl 1):23–29. doi: 10.1016/s0749-3797(03)00161-2. [DOI] [PubMed] [Google Scholar]
- Anderson NB. Levels of analysis in health science. A framework for integrating sociobehavioral and biomedical research. Ann N Y Acad Sci. 1998;840:563–576. doi: 10.1111/j.1749-6632.1998.tb09595.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;15(4):266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- Baruth M, Wilcox S, Blair S, Hooker S, Hussey J, Saunders R. Psychosocial mediators of a faith-based physical activity intervention: implications and lessons learned from null findings. Health Educ Res. 2010;25(4):645–655. doi: 10.1093/her/cyq007. [DOI] [PubMed] [Google Scholar]
- Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(2 Suppl):5–14. doi: 10.1016/s0749-3797(02)00469-5. [DOI] [PubMed] [Google Scholar]
- Cerin E, Conway TL, Saelens BE, Frank LD, Sallis JF. Cross-validation of the factorial structure of the Neighborhood Environment Walkability Scale (NEWS) and its abbreviated form (NEWS-A). Int J Behav Nutr Phys Act. 2009;6:32. doi: 10.1186/1479-5868-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B, Bean K, Leal C, Thomas F, Havard S, Evans D, et al. Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: which risk factors explain the associations? Hypertension. 2010;55(3):769–775. doi: 10.1161/HYPERTENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- Chobanian A, Bakris G, Black H, Cushman W, Green L, Izzo J, Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Coulon SM, Wilson DK, Griffin S, St George SM, Alia KA, Trumpeter NN, et al. Formative Process Evaluation for Implementing a Social Marketing Intervention to Increase Walking Among African Americans in the Positive Action for Today's Health Trial. Am J Public Health. 2012;102(12):2315–2321. doi: 10.2105/AJPH.2012.300758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutter SL. Race, class and environmental justice. Progress in Human Geography. 1995;19:111–111. [Google Scholar]
- Cutts BB, Darby KJ, Boone CG, Brewis A. City structure, obesity, and environmental justice: an integrated analysis of physical and social barriers to walkable streets and park access. Soc Sci Med. 2009;69(9):1314–1322. doi: 10.1016/j.socscimed.2009.08.020. [DOI] [PubMed] [Google Scholar]
- Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: a meta-analysis of selected environmental characteristics. Int J Behav Nutr Phys Act. 2005;2:11. doi: 10.1186/1479-5868-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. [Google Scholar]
- Esliger DW, Tremblay MS. Technical reliability assessment of three accelerometer models in a mechanical setup. Medicine & Science in Sports & Exercise. 2006;38(12):2173. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- Eugeni ML, Baxter M, Mama SK, Lee RE. Disconnections of African American public housing residents: connections to physical activity, dietary habits and obesity. Am J Community Psychol. 2011;47(3-4):264–276. doi: 10.1007/s10464-010-9402-1. [DOI] [PubMed] [Google Scholar]
- Eyler A, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999;49(6):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- Eyler A, Wilcox S, Matson-Koffman D, Evenson KR, Sanderson B, Thompson J, et al. Correlates of physical activity among women from diverse racial/ethnic groups. J Womens Health Gend Based Med. 2002;11(3):239–253. doi: 10.1089/152460902753668448. [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prev Sci. 2009;10(2):87–99. doi: 10.1007/s11121-008-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild AJ, Mackinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behav Res Methods. 2009;41(2):486–498. doi: 10.3758/BRM.41.2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer Aggarwal BA, Liao M, Mosca L. Physical activity as a potential mechanism through which social support may reduce cardiovascular disease risk. J Cardiovasc Nurs. 2008;23(2):90–96. doi: 10.1097/01.JCN.0000305074.43775.d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleury J, Lee SM. The social ecological model and physical activity in African American women. Am J Community Psychol. 2006;37(1-2):129–140. doi: 10.1007/s10464-005-9002-7. [DOI] [PubMed] [Google Scholar]
- Ford CD, Kim MJ, Dancy BL. Perceptions of hypertension and contributing personal and environmental factors among rural Southern African American women. Ethn Dis. 2009;19(4):407–413. [PMC free article] [PubMed] [Google Scholar]
- Foster S, Giles-Corti B, Knuiman M. Neighbourhood design and fear of crime: a social-ecological examination of the correlates of residents’ fear in new suburban housing developments. Health Place. 2010;16(6):1156–1165. doi: 10.1016/j.healthplace.2010.07.007. [DOI] [PubMed] [Google Scholar]
- Franz MJ, Bantle JM, Beebe CA, Brunzell JD, Chiasson JL, Garg A, et al. American Diabetes Association Position Statement: Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Journal of the American Dietetic Association. 2002;102(1):109–118. doi: 10.1016/s0002-8223(02)90031-3. [DOI] [PubMed] [Google Scholar]
- Fritz M, MacKinnon D. Required sample size to detect the mediated effect. Psychological Science. 2007;18(3):233. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadegbeku C, Lea J, Jamerson K. Update on disparities in the pathophysiology and management of hypertension: focus on African Americans. The Medical clinics of North America. 2005;89(5) doi: 10.1016/j.mcna.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Geronimus AT. To mitigate, resist, or undo: addressing structural influences on the health of urban populations. Am J Public Health. 2000;90(6):867–872. doi: 10.2105/ajph.90.6.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons MC. Populomics. Stud Health Technol Inform. 2008;137:265–268. [PubMed] [Google Scholar]
- Greenberg MR, Renne J. Where does walkability matter the most? An environmental justice interpretation of New Jersey data. J Urban Health. 2005;82(1):90–100. doi: 10.1093/jurban/jti011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SF, Wilson DK, Wilcox S, Buck J, Ainsworth BE. Physical activity influences in a disadvantaged African American community and the communities’ proposed solutions. Health Promot Pract. 2008;9(2):180–190. doi: 10.1177/1524839906296011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies: data from the Health Survey for England 1994. Am J Epidemiol. 1999;149(9):876–883. doi: 10.1093/oxfordjournals.aje.a009904. [DOI] [PubMed] [Google Scholar]
- Ham SA, Ainsworth BE. Disparities in data on Healthy People 2010 physical activity objectives collected by accelerometry and self-report. Am J Public Health. 2010;100(Suppl 1):S263–268. doi: 10.2105/AJPH.2009.180075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan PJ, Murray DM, Jacobs DR, Jr., McGovern PG. Parameters to aid in the design and analysis of community trials: intraclass correlations from the Minnesota Heart Health Program. Epidemiology. 1994;5(1):88–95. doi: 10.1097/00001648-199401000-00013. [DOI] [PubMed] [Google Scholar]
- He J, Whelton PK. Elevated systolic blood pressure and risk of cardiovascular and renal disease: overview of evidence from observational epidemiologic studies and randomized controlled trials. Am Heart J. 1999;138(3 Pt 2):211–219. doi: 10.1016/s0002-8703(99)70312-1. [DOI] [PubMed] [Google Scholar]
- Heil DP. Predicting activity energy expenditure using the Actical activity monitor. Res Q Exerc Sport. 2006;77(1):64–80. doi: 10.1080/02701367.2006.10599333. [DOI] [PubMed] [Google Scholar]
- Hemmingsson E, Hellenius ML, Ekelund U, Bergstrom J, Rossner S. Impact of social support intensity on walking in the severely obese: a randomized clinical trial. Obesity (Silver Spring) 2008;16(6):1308–1313. doi: 10.1038/oby.2008.204. [DOI] [PubMed] [Google Scholar]
- Hovell MF, Sallis JF, Hofstetter CR, Spry VM, Faucher P, Caspersen CJ. Identifying correlates of walking for exercise: an epidemiologic prerequisite for physical activity promotion. Prev Med. 1989;18(6):856–866. doi: 10.1016/0091-7435(89)90021-2. [DOI] [PubMed] [Google Scholar]
- Kamphuis CB, Mackenbach JP, Giskes K, Huisman M, Brug J, van Lenthe FJ. Why do poor people perceive poor neighbourhoods? The role of objective neighbourhood features and psychosocial factors. Health Place. 2010;16(4):744–754. doi: 10.1016/j.healthplace.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Kanu M, Baker E, Brownson R. Exploring associations between church-based social support and physical activity. Journal of physical activity & health. 2008;5(4):504. doi: 10.1123/jpah.5.4.504. [DOI] [PubMed] [Google Scholar]
- Kezdi G. Robust standard error estimation in fixed-effects panel models. 2003. Available at SSRN 596988.
- King AC, Toobert D, Ahn D, Resnicow K, Coday M, Riebe D, et al. Perceived environments as physical activity correlates and moderators of intervention in five studies. Am J Health Promot. 2006;21(1):24–35. doi: 10.1177/089011710602100106. [DOI] [PubMed] [Google Scholar]
- Koh HK. A 2020 vision for healthy people. N Engl J Med. 2010;362(18):1653–1656. doi: 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- Maas CJ, Hox JJ. Robustness issues in multilevel regression analysis. Statistica Neerlandica. 2004;58(2):127–137. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychol. 2008;27(2 Suppl):S99–S100. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011;62:501–530. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minor D, Wofford M, Jones D. Racial and ethnic differences in hypertension. Current atherosclerosis reports. 2008;10(2):121–127. doi: 10.1007/s11883-008-0018-y. [DOI] [PubMed] [Google Scholar]
- Mowen A, Orsega-Smith E, Payne L, Ainsworth BE, Godbey G. The role of park proximity and social support in shaping park visitation, physical activity, and perceived health among older adults. J Phys Act Health. 2007;4(2):167–179. doi: 10.1123/jpah.4.2.167. [DOI] [PubMed] [Google Scholar]
- Nichols A, Schaffer M. Clustered errors in Stata; Paper presented at the United Kingdom Stata Users’ Group Meeting.2007. [Google Scholar]
- Ofili E. Ethnic disparities in cardiovascular health. Ethn Dis. 2001;11(4):838–840. [PubMed] [Google Scholar]
- Owen N, Humpel N, Leslie E, Bauman A, Sallis JF. Understanding environmental influences on walking; Review and research agenda. Am J Prev Med. 2004;27(1):67–76. doi: 10.1016/j.amepre.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Patsdaughter CA, Christensen MH, Kelley BR, Masters JA, Ndiwane AN. Meeting folks where they are: collecting data from ethnic groups in the community. J Cult Divers. 2001;8(4):122–127. [PubMed] [Google Scholar]
- Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves JW, Hill MN, et al. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich) 2005;7(2):102–109. doi: 10.1111/j.1524-6175.2005.04377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikora TJ, Giles-Corti B, Knuiman MW, Bull FC, Jamrozik K, Donovan RJ. Neighborhood environmental factors correlated with walking near home: Using SPACES. Med Sci Sports Exerc. 2006;38(4):708–714. doi: 10.1249/01.mss.0000210189.64458.f3. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Magaziner J, Wynne C. The effect of social support on exercise behavior in older adults. Clin Nurs Res. 2002;11(1):52–70. doi: 10.1177/105477380201100105. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive Summary: Heart Disease and Stroke Statistics--2012 Update: A Report From the American Heart Association. Circulation. 2012;125(1):188. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- Saelens B, Sallis J, Black J, Chen D. Measuring perceived neighborhood environment factors related to walking/cycling. Annals of Behavioral Medicine. 2002;24:S139. [Google Scholar]
- Sallis JF, Bowles HR, Bauman A, Ainsworth BE, Bull FC, Craig CL, et al. Neighborhood environments and physical activity among adults in 11 countries. Am J Prev Med. 2009;36(6):484–490. doi: 10.1016/j.amepre.2009.01.031. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Sallis JF, King AC, Sirard JR, Albright CL. Perceived environmental predictors of physical activity over 6 months in adults: activity counseling trial. Health Psychol. 2007;26(6):701–709. doi: 10.1037/0278-6133.26.6.701. [DOI] [PubMed] [Google Scholar]
- Scott AJ, Wilson RF. Social determinants of health among African Americans in a rural community in the Deep South: an ecological exploration. Rural Remote Health. 2011;11(1):1634. [PubMed] [Google Scholar]
- Sharma M, Sargent L, Stacy R. Predictors of leisure-time physical activity among African American women. American Journal of Health Behavior. 2005;29(4):352–359. doi: 10.5993/ajhb.29.4.7. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Marmot M. The role of psychobiological pathways in socio-economic inequalities in cardiovascular disease risk. Eur Heart J. 2002;23(1):13–25. doi: 10.1053/euhj.2001.2611. [DOI] [PubMed] [Google Scholar]
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Canadian Journal of Sport Sciences. 1992 [PubMed] [Google Scholar]
- Thorpe RJ, Jr., Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study. Soc Sci Med. 2008;67(10):1604–1611. doi: 10.1016/j.socscimed.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trumpeter NN, Lawman HG, Wilson DK, Pate RR, Van Horn ML, Tate AK. Accelerometry cut points for physical activity in underserved African Americans. Int J Behav Nutr Phys Act. 2012;9:73. doi: 10.1186/1479-5868-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu JV, Ko DT. Ecological studies and cardiovascular outcomes research. Circulation. 2008;118(24):2588–2593. doi: 10.1161/CIRCULATIONAHA.107.729806. [DOI] [PubMed] [Google Scholar]
- Tudge JRH, Mokrova I, Hatfield BE, Karnik RB. Uses and misuses of Bronfenbrenner's bioecological theory of human development. Journal of Family Theory & Review. 2009;1(4):198–210. [Google Scholar]
- U.S. Department of Health and Human Services [August 9, 2011];About Healthy People. 2011 from http://www.healthypeople.gov/2020/about/default.aspx.
- Van Dyck D, Cardon G, Deforche B, Sallis JF, Owen N, De Bourdeaudhuij I. Neighborhood SES and walkability are related to physical activity behavior in Belgian adults. Prev Med. 2010;50(Suppl 1):S74–79. doi: 10.1016/j.ypmed.2009.07.027. [DOI] [PubMed] [Google Scholar]
- Wang G, Macera CA, Scudder-Soucie B, Schmid T, Pratt M, Buchner D, et al. Cost analysis of the built environment: the case of bike and pedestrian trials in Lincoln, Neb. Am J Public Health. 2004;94(4):549–553. doi: 10.2105/ajph.94.4.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendel-Vos W, Droomers M, Kremers S, Brug J, van Lenthe F. Potential environmental determinants of physical activity in adults: a systematic review. Obes Rev. 2007;8(5):425–440. doi: 10.1111/j.1467-789X.2007.00370.x. [DOI] [PubMed] [Google Scholar]
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- Wilbur JE, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern African-American women. American journal of preventive medicine. 2003;25(3):45–52. doi: 10.1016/s0749-3797(03)00164-8. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Bopp M, Oberrecht L, Kammermann SK, McElmurray CT. Psychosocial and perceived environmental correlates of physical activity in rural and older african american and white women. J Gerontol B Psychol Sci Soc Sci. 2003;58(6):P329–337. doi: 10.1093/geronb/58.6.p329. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Kirtland KA, Ainsworth BE, Addy CL. Socioeconomic status and perceptions of access and safety for physical activity. Ann Behav Med. 2004;28(1):20–28. doi: 10.1207/s15324796abm2801_4. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Trumpeter NN, St George SM, Coulon SM, Griffin S, Lee Van Horn M, et al. An overview of the “Positive Action for Today's Health” (PATH) trial for increasing walking in low income, ethnic minority communities. Contemp Clin Trials. 2010;31(6):624–633. doi: 10.1016/j.cct.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]