Abstract
Introduction:
Neuropsychiatry has generally been regarded as a hybrid discipline that lies in the borderland between the disciplines of psychiatry and neurology. There is much debate on its current and future identity and status as a discipline.
Materials and Methods:
Taking a historical perspective, the future of neuropsychiatry is placed within the context of recent developments in clinical neuroscience.
Results:
The authors argue that with the maturation of the discipline, it must define its own identity that is not dependent entirely upon the parent disciplines. The requirements for this are the claiming of neuropsychiatric territory, a strong training agenda, an emphasis on treatments that are uniquely neuropsychiatric, and a bold embrace of new developments in clinical neuroscience.
Conclusion:
The exponential growth in neuroscientific knowledge places neuropsychiatry in an excellent position to carve out a strong identity. It is imperative that the leaders of the discipline seize the moment.
Keywords: Behavioural neurology, Brain stimulation, Neuropsychiatry, Neurorehabilitation, Psychiatry, Research agenda, Specialty, Training
Introduction
Debate on the role and future of neuropsychiatry as a discipline has been a common theme of editorial comment and scholarly discussion in the last decade (Coffey et al., 2004[2]; Hurwitz, 2004[11]. Sachdev, 2005a[22]; Nierenberg, 2009[20]; Mendez and Manes, 2011[19]). These authors highlight the difficult task of defining neuropsychiatry, and thereby delineating its scope. The definition put forth by the International Neuropsychiatric Association probably best captures the zeitgeist of the discipline (Sachdev, 2005b[23]). It defines neuropsychiatry as “a field of scientific medicine that concerns itself with the complex relationship between human behaviour and brain function, and endeavours to understand abnormal behaviour and behavioural disorders on the basis of an interaction of neurobiological and psychological–social factors”.
Implicit in this definition is the primacy of neuroscience and neurobiology in the practice of neuropsychiatry, and its essence as an academic discipline. It is important to note that neuropsychiatry rejects the Cartesian posit of dualism of mind and brain, choosing instead to adopt an integrative approach to neuropsychiatric disorders. Neuropsychiatry regards the mind as an emergent property of the brain and considers all mental disorders as brain disorders as well, although accepting that mental phenomena can frequently not be reduced to neural phenomena. Neuropsychiatrists are comfortable in conceptualising and relating psychological and neural processes. Their training therefore demands proficiency in psychiatry, neuroscience and, to some extent, general medicine in order to deal with the complexity of the patient population they encounter. They also bear the onus of staying abreast of neuroscientific discoveries and novel and experimental therapies.
It is useful to digress briefly to the history of neuropsychiatry, one that can be traced back to the mid nineteenth century, or even as early as the seventeenth century. The conceptual foundations of neuropsychiatry have been particularly vulnerable to the socio-political contexts of the time. One could argue that this chameleon-like need to shift and adapt its territorial boundaries and identity continues to influence attempts at standardisation of the discipline internationally. The boundary fences have had to shift to accommodate the prevailing knowledgebase and injunctions of medical practice. A core pursuit has been to link psychopathology to demonstrable brain deficits, an endeavour that relies heavily on the technology available to “visualise” the brain and alterations in brain functioning in vivo. Viewed from this perspective, it is inevitable that neuropsychiatric formulations will evolve as technologies develop. In the last two decades, we have seen an onslaught of neuroimaging technologies, in particular the various modalities of magnetic resonance imaging (MRI) and positron emission tomography (PET), but the emphasis is now shifting to the “omics,” with rapid advances in genomics, proteomics, metabolomics, lipidomics, epigenomics, transcriptomics and neuronomics, to name only a few (Filiou and Turck, 2011[7]). These developments suggest that the disorders neuropsychiatry considers as its core business are on a list that the quill of neuroscientific discovery will rewrite and reorder from time to time. Patients with tertiary syphilis and epilepsy that filled the psychiatric hospitals in the early 19th century are ready examples of this phenomenon.
The relationship of neuropsychiatry to its “parent” disciplines of psychiatry and neurology requires consideration. As has been previously argued (Sachdev, 2005a[22]), to consider neuropsychiatry as an amalgam of these two arguably better-established disciplines is over-simplistic. The discipline has, in the throes of its re-emergence in the last two decades, reflexively placed itself in the borderland between neurology and psychiatry. This move has in hindsight been misguided as the “borderland” is forever changing, depending on the fortunes of the combatants on either side. Twenty-first century commentators are calling for an integration of neurology, psychiatry, and the neurosciences, providing a new backdrop for the debate on the future of neuropsychiatry (Martin, 2002[17]; Hobson, 2003[9]). It is in this context that many commentators have questioned whether there will be a need for neuropsychiatry and, if so, whether there will be a future for neurology and psychiatry as distinct disciplines. Territorial claims are dynamic processes that are resolved by historical developments and shifts in thinking. The “biologisation” of psychiatry is inevitable. Neurologists on the other hand find themselves confronted with a “softer” view of the brain, in which it is seen as a plastic organ shaped by the environment and forever changing and adapting (May, 2011[18]). In the midst of these shifting paradigms, the future of neuropsychiatry lies in claiming and consolidating its territory, developing a training manifesto, delivering effective treatments, and advancing a research agenda that reflects its multidisciplinary and bridging perspectives.
Defining its territory
The need for neuropsychiatry to have a “secure base” of clinical disorders has been outlined in a previous editorial (Sachdev, 2005a[22]). This “base” cannot comprise exclusively of disorders that neither neurology nor psychiatry feels comfortable with. The latter approach is particularly susceptible to changes in thinking, models of service delivery, and the inexorable march of scientific discovery. Historically, the fences around neuropsychiatric territory have needed to be permeable, allowing the bidirectional diffusion of ideas, information, philosophies, and therapies. This is in fact one of the specialty's greatest strengths and has shaped a neuropsychiatrist's view of his or her work.
A few examples may serve to illustrate these developments. There has been a resurgence of interest in the putative role of autoimmune disorders in the pathophysiology of neuropsychiatric symptoms in the last 6 years or so (Davison, 2012[6]). The description of encephalitis associated with autoantibodies to the NMDA receptor (Tüzün and Dalmau, 2007[25]) in light of growing evidence for the role of NMDA receptor hypofunction in schizophrenia (Labrie and Roder, 2010[12]) has focussed the attention of the psychiatric community on the link between psychosis and disorders of the immune system, with autoimmune screening being proposed for individuals with first episode psychosis (Lennox et al., 2012[13]). However, the variability of presenting symptoms in such disorders has made it extremely difficult to present accurate clinico-pathological correlations and speculate about causal associations. What is clear, however, is that a proportion of these patients have prominent psychiatric symptoms at the outset and may present to psychiatric services at initial contact (Dalmau et al., 2011[5]). A skilled neuropsychiatrist, with knowledge of neuroanatomy, neurophysiology, and neuropsychology, would be well placed to provide tertiary-level care for such patients. The prominence of persistent executive deficits in some of these patients has led to speculation about the involvement of fronto-subcortical circuits. This is material that has been the subject of neuropsychiatric scrutiny for some time, even if the answers are likely to be more complicated.
As another example, the management of Tourette syndrome requires familiarity with movement disorders as well as obsessive-compulsive disorder, attention deficit disorder, conduct disorder, mood disorders, specific developmental disabilities, and sleep disorder, and requires skills in pharmacotherapy, behaviour therapy, family therapy, genetic counselling, and rehabilitation. Here too, a neuropsychiatrist brings a more integrative approach to bear upon the problems, far better than a combination of clinicians from different disciplines.
What characterises neuropsychiatry is the skill of its proponents in a variety of methods and techniques rather than a monopoly over any one particular technique. There are many disorders that currently fit the bill of being “neuropsychiatric”. The diagnoses that come to mind are neurocognitive disorders, drug-induced movement disorders, Tourette syndrome, psychiatric disorders associated with other movement disorders such as Parkinson's disease and dystonia, psychiatric disorders associated with epilepsy, cerebrovascular disease and head injury, chronic fatigue syndrome and other psychoneuroimmunological disorders, attention deficit hyperactivity disorder, and other conditions in which cognitive, behavioural, or affective disturbance results directly from brain insult. The neurocognitive disorders are another large and important group of disorders currently managed by neurologists, geropsychiatrists, or geriatricians, each bringing a particular bias to their management. The neuropsychiatrist is well placed to bring multiple skills to bear upon the effective management of these disorders. In particular, the assessment and management of young onset dementia is an orphan territory that neuropsychiatry could easily claim.
In the final analysis, neuropsychiatry is what a neuropsychiatrist does. The International Neuropsychiatric Association was acutely aware of this when it formulated its curriculum, as the knowledge and skills objectives of training will define the field for the future (Sachdev, 2010[21]).
Developing a training manifesto
The future and security of a discipline lies in its ability to attract and retain motivated, inquisitive, and committed trainees. This in turn requires the development and delivery of high-quality training to its newest members. Most of the current generation of neuropsychiatrists around the world is self-trained, but this situation cannot lead to a secure professional status for the future. Therefore, neuropsychiatry must foster a strong training agenda. Training requirements and opportunities have regional disparities and are subject to the vagaries of local funding infrastructures. Nevertheless, a core curriculum, such as the one proposed by the International Neuropsychiatric Association (Sachdev, 2010[21]), would have wide application. This curriculum has well-delineated objectives in relation to the knowledge and skills base as well as the attitudes to the profession. It comprises core competencies as well as skills and knowledge pertaining to specific disorders such as neurocognitive disorders, seizure disorders, movement disorders, traumatic brain injury, secondary psychiatric disorders, substance-induced disorders, attentional disorders, neurodevelopmental disorders, and sleep disorders. In addition, it refers to neuropsychiatric rehabilitation and forensic neuropsychiatry.
Some jurisdictions already have well-established neuropsychiatry training programmes. The United Council for Neurological Subspecialties (UCNS) in the United States of America oversees the accreditation of 19 Fellowship programmes in behavioural neurology and neuropsychiatry, certifying diplomates in Behavioural Neurology and Neuropsychiatry (BN and NP) on completion of a prescribed curriculum and a certification examination (Silver JM, 2006[24]). The UCNS was incorporated in March 2003. The situation remains less structured in other parts of the world, where training in neuropsychiatry can depend heavily on access to local tertiary services and adoption of modified versions of existing curricula. In the Indian context, exposure to Neuropsychiatry training follows a similar model, with larger, tertiary, university-affiliated centres offering more structured training while others offer a more eclectic mix often through cross-placement of post graduate trainees in neurology and psychiatry for limited periods of time. Nonetheless, the finer details of the composition of training and decisions around the requisite skill levels in neuroimaging, clinical neurophysiology, and neuropsychological expertise have been made clear (Sachdev, 2010[21]). It is imperative that national associations of neuropsychiatry place the discipline firmly on their agenda, develop comprehensive training programmes, and resource them through various funding bodies. The involvement of psychiatry and neurology in this would be paramount, not only for the intellectual and clinical input but also because neuropsychiatry trainees are at an advanced level with basic training in one of the parent disciplines. Neuropsychiatry thus positions itself to benefit from both the objectivity and the empiricism of the neurologist as well as the psychotherapeutic expertise of the psychiatrist applying this potent mix of clinical skills to the evaluation of complex disease and dysfunction in a quintessentially human context.
The pace of progress in neuroscientific knowledge will continue to challenge clinicians’ ability to maintain the skill and knowledge basis of their discipline, such that a neurologist, no matter how well trained, will find it impossible to acquire sufficient psychiatric skills to achieve competence in this field and vice versa. Continuing in this vein, it is reasonable to assert that the skills that define a neuropsychiatrist require a period of specialised advanced training irrespective of the trainee's basic skills. Both psychiatry and neurology appear comfortable with this premise, and the nature of referrals to neuropsychiatry from these disciplines bears testament to this. A contemporary example from neuropsychiatry is Alzheimer's disease. Rapid advances have occurred in the last 15 years; however, much of the tertiary management of this disorder in many countries is in the domain of neuropsychiatry and psychogeriatrics rather than neurology, which will more than likely continue. The expanding panel of biomarkers and their incorporation into diagnostic criteria, including in the forthcoming DSM-5, suggests a move towards earlier diagnosis and the clinical research focus on early intervention and disease modification strategies. A rapprochement does not entail an amalgamation. Psychiatry and neurology can therefore be rest assured that their respective futures as individual disciplines are secure. Neuropsychiatric training entails the acquisition of knowledge, some of which has a significant overlap with neurology and psychiatry. It is however in the integration and application of this knowledge that the neuropsychiatrists differentiate themselves from their counterparts in these disciplines.
Developing a strong treatment agenda
Most treatment strategies in neuropsychiatry are shared with psychiatry and neurology, with the contribution of neuropsychiatry being that the practitioner is equally comfortable with certain therapies used in either discipline. A neuropsychiatrist managing psychosis associated with epilepsy is expected to be comfortable in the usage of both antipsychotic and antiepileptic treatments. In the management of dementia, he or she has good knowledge of the specific treatments of cognitive disorders as well as the psychiatric manifestations of these disorders. Neuropsychiatric recovery and rehabilitation in this context are essentially multidisciplinary endeavours, requiring the expert contributions of a variety of health professionals, including social workers, occupational therapists, speech and language therapists, physiotherapists, and others. The neuropsychiatrist must learn to function within such a team and form part of a system that delivers competent, consistent, collaborative, and individualised care.
There are some treatment modalities that the neuropsychiatrist may stake a primary claim on. In particular, these are the developing techniques of neuromodulation and neurostimulation, and the exciting developments in neuropsychiatric rehabilitation, including measures to enhance neuroplasticity.
Neurostimulation treatments have a long history in neuropsychiatry and neuropsychiatric training is uniquely placed to provide the theoretical basis and skills for such interventions. Electroconvulsive therapy (ECT) retains its place as one of the most effective and reliable treatments for refractory depression (Lisanby, 2007[14]). Research in the field has continued to march on, with resulting refinements in technique and stimulus parameters. The use of brief pulse and, increasingly, ultra-brief pulse stimuli in clinical practice are making the treatment more tolerable from a cognitive point of view, hitherto the Achilles heel of ECT. Vagus nerve stimulation (VNS), transcranial direct current stimulation (tDCS), and transcranial magnetic stimulation (TMS) have shown modest efficacy as treatments in medication-resistant depression (Malhi et al., 2006[16]). Deep brain stimulation (DBS) for neuropsychiatric disorders, particularly Tourette's syndrome, OCD, and depression, has arrived on the scene, bringing with it the long-awaited data from naturalistic studies as well as controlled trials in the last few years (Holtzheimer et al., 2012[10]), suggesting a potentially effective treatment for the most perniciously ill patients in these groups. The march of such treatments is inexorable, and neuropsychiatry is well positioned to take advantage of these developments.
Neuropsychiatric rehabilitation is an emerging field that has moved from its focus on traumatic brain injury to include a range of disorders, including neurocognitive disorders and the cognitive syndromes associated with schizophrenia, substance abuse, and even normal ageing. The discovery of neurogenesis in the adult brain has spawned a paradigm shift in the neuroscientific community's perception of the adult brain, viewing it now as a dynamic and plastic structure capable of remodelling itself in response to external and internal drivers. The processes involved in this include neurogenesis and changes in functional connectivity through synaptic formation and pruning, dendritic outgrowth and de-branching, and axonal spouting and pruning (Curtis et al., 2011[4]). Research efforts are beginning to focus on the translation of neuroplasticity into effective clinical strategies for use in patient populations such as those with neuropsychiatric disorders. Non-invasive brain stimulation techniques such as ECT, TMS, and tDCS have been speculated to modulate brain function in the cortical and subcortical regions through neuroplastic processes. ECT (or electro-convulsive shock or ECS) has been studied more extensively in animal models, including non-human primates, where it has been shown to increase hippocampal BDNF and synaptic density and promote neurogenesis. It has been suggested that these processes mediate behavioural recovery in depression. DBS has been proposed to induce neuroplastic changes that mediate the more gradual effects of chronic stimulation (Cramer et al., 2011[3]).
Another exciting recent development has been in cognitive stimulation treatments that lie within the domain of neuropsychiatry. This could be in the form of cognitive training, compensatory cognitive rehabilitation, or general cognitive stimulation. Cognitive training provides structured practice of complex mental activity in order to enhance cognitive function (Belleville, 2008[1]), and has attracted intense public, commercial, and scientific interest. Cognitive stimulation has been used to refer to interventions ranging from generic topical discussions, executive exercises, and memory strategy training (Wenisch et al., 2007[26]). As the focus on cognitive ageing and the prevention of dementia increases, these techniques will gain further prominence, and neuropsychiatry is well placed to adopt them.
Embracing and contributing to new research
The strong academic track of neuropsychiatry can only be maintained if the discipline not only embraces new research and technology but also contributes actively to its development. Every neuropsychiatrist must also, therefore, be an active researcher. In the academic sense, this broadens the scope of neuropsychiatry considerably. While clinical training in neuropsychiatry requires initial specialisation in either psychiatry or neurology, research in this field is open to a wide range of neuroscientists whose ranks include, in addition to basic neuroscientists, developmental paediatricians, neuroradiologists, neuropsychologists, geropsychiatrists, and others. This discipline is intellectually young and must maintain its vigour. Remarkable advances are occurring in neuropsychiatric disorders and their treatment. The neuromodulation techniques mentioned above are still at an early stage of development, and many refinements are necessary. The field of neurorehabilitation and means to exploit neuroplasticity are undergoing rapid advancement.
Another area of great excitement is in the discovery of biomarkers. It is important to recognise that the establishment of biomarkers for psychiatric disorders will place them firmly in neuropsychiatric territory (Macaluso and Preskorn, 2012[15]). So far, much of the advances have been in the field of dementia (Hampel et al., 2011[8]), but primary psychiatric disorders are showing promise. Neuropsychiatrists of the future will need to do more than remain passive observers of these developments. Engagement in the process of discovery is essential, and underscores the positioning of neuropsychiatry as a “frontier discipline”.
Concluding Remarks [See also Figure 1: Flowchart of paper]
Figure 1.
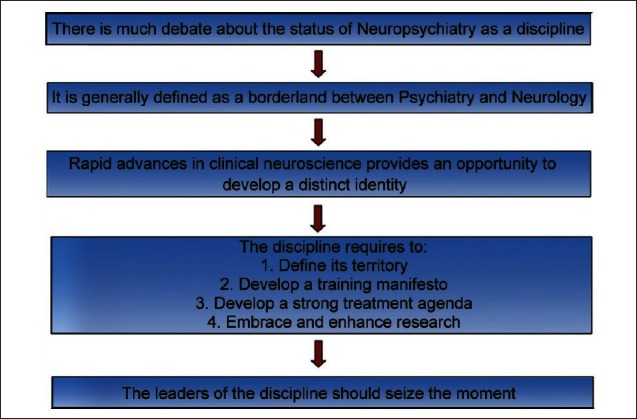
Flowchart of the paper
The discipline of neuropsychiatry has arrived, and the status of knowledge in neuroscience and clinical practice is ripe for exploitation to advance it further. It is important that the practitioners of the discipline recognise their moment in the sun and grasp it with both hands. For this, they will need to be clear about their objectives and will need to define their territory in practice and research. They will have to be clinician scientists, with a strong imperative for research and the advancement of knowledge. They will need to train the next generation of neuropsychiatrists with determination and courage, and have an important agenda for therapeutics such that they can engage the community. If they are able to do so, there is no reason why the future should not belong to neuropsychiatry.
Take home message
Neuropsychiatry has better defined itself in the current clinical context, both in its scope as well as in its relationship to the disciplines of psychiatry and neurology. The pressing need now is for training programmes internationally to develop and deliver advanced training in the field such that future neuropsychiatrists can be comfortable with the skill set that they acquire, the knowledge base that they must continue to expand, and the service that they deliver, both to their patients and to the medical community at large. Neuroscience demands that these neuropsychiatrists have a research agenda as well.
Questions that this Paper Raises
How do developments in functional neuroimaging and the “omics” influence the clinical and scientific agenda of neuropsychiatry?
How does a potential neuropsychiatrist keep abreast of the rapidly expanding literature in neurostimulation, neuromodulation, and neuroplasticity and find ways to translate research into clinical practice?
What are the pathways by which standardised training programmes can seek sustainable funding?
What is the therapeutic agenda that neuropsychiatry must develop as being distinctive from psychiatry and neurology?
About the Author

Perminder Sachdev AM MBBS MD FRANZCP PhD MFPOA is Scientia Professor of Neuropsychiatry, Co-Director of the Centre for Healthy Brain Ageing (CHeBA), in the School of Psychiatry, University of New South Wales in Sydney, Australia, and Clinical Director of the Neuropsychiatric Institute (NPI) at the Prince of Wales Hospital, Sydney. He is a former President of the International Neuropsychiatric Association and President-elect of the International College of Geriatric Psychoneuropharmacology. He has broad research interests, with a major focus on dementia and cognitive ageing, drug-induced movement disorders, neuroimaging, and brain stimulation. He has published over 350 peer-reviewed journal papers and five books, including one for lay readers (The Yipping Tiger and other tales from the neuropsychiatric clinic). In 2011, he was appointed Member of the Order of Australia (AM) for service to medical research in the field of neuropsychiatry and to professional associations at a national and international level.
About the Author

Adith Mohan MRCPsych, FRANZCP, is currently a consultant neuropsychiatrist at the Neuropsychiatric Institute, Sydney, and an early career researcher with the Centre for Healthy Brain Ageing (CHeBA), School of Psychiatry, UNSW Medicine, University of New South Wales, Australia. He completed his postgraduate training in psychiatry in the UK and moved to Australia to pursue a career in neuropsychiatry. His primary research interest is in cognitive disorders and newer brain stimulation techniques and their application in psychiatric disorders.
Acknowledgement
This study has been supported by the National Health and Medical Research Council of Australia Program Grant (ID 350833) and Capacity Building Grant (ID568940).
Footnotes
Conflict of interest: None declared
Declaration
This is the authors’ original unpublished work, and has not been submitted elsewhere for publication.
CITATION: Sachdev PS, Mohan A. Neuropsychiatry: Where Are We And Where Do We Go From Here? Mens Sana Monogr 2013;11:4-15.
Peer Reviewers for this paper: 1. Moises Gaviria MD; 2. Ennapadam S Krishnamoorthy MD, PhD; 3. Subbulakshmy Natarajan MBBS, DCN, PhD
References
- 1.Belleville S. Cognitive training for persons with mild cognitive impairment. Int Psychogeriatr. 2008;20:57–66. doi: 10.1017/S104161020700631X. [DOI] [PubMed] [Google Scholar]
- 2.Coffey CE, Silver J, McAllister T, Restak R. An update of the strategic plan for neuropsychiatry. J Neuropsychiatry Clin Neurosci. 2004;16:133–4. doi: 10.1176/jnp.16.2.133. [DOI] [PubMed] [Google Scholar]
- 3.Cramer SC, Sur M, Dobkin BH, O’Brien C, Sanger TD, et al. Harnessing neuroplasticity for clinical applications. Brain. 2011;134:1591–609. doi: 10.1093/brain/awr039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curtis MA, Kam M, Faull RL. Neurogenesis in humans. Eur J Neurosci. 2011;33:1170–4. doi: 10.1111/j.1460-9568.2011.07616.x. [DOI] [PubMed] [Google Scholar]
- 5.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74. doi: 10.1016/S1474-4422(10)70253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davison K. Autoimmunity in psychiatry. Br J Psychiatry. 2012;200:353–5. doi: 10.1192/bjp.bp.111.104471. [DOI] [PubMed] [Google Scholar]
- 7.Filiou MD, Turck CW. General overview: Biomarkers in neuroscience research. Int Rev Neurobiol. 2011;101:1–17. doi: 10.1016/B978-0-12-387718-5.00001-8. [DOI] [PubMed] [Google Scholar]
- 8.Hampel H, Prvulovic D, Teipel S, Jessen F, Luckhaus C, Frölich L, et al. The future of Alzheimer's disease: The next 10 years. Prog Neurobiol. 2011;95:718–28. doi: 10.1016/j.pneurobio.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Hobson JA. Neurology, Psychiatry, and Neuroscience. Am J Psychiatry. 2003;160:1013–4. doi: 10.1176/appi.ajp.160.5.1013-a. [DOI] [PubMed] [Google Scholar]
- 10.Holtzheimer PE 3rd, Kosel M, Schlaepfer T. Brain stimulation therapies for neuropsychiatric disease. Handb Clin Neurol. 2012;106:681–95. doi: 10.1016/B978-0-444-52002-9.00041-3. [DOI] [PubMed] [Google Scholar]
- 11.Hurwitz TA. Neuropsychiatry: Grasping the body-mind and mind-body problems. Can J Psychiatry. 2004;49:155–6. doi: 10.1177/070674370404900301. [DOI] [PubMed] [Google Scholar]
- 12.Labrie V, Roder JC. The involvement of the NMDA receptor D-serine/glycine site in the pathophysiology and treatment of schizophrenia. Neurosci Biobehav Rev. 2010;34:351–72. doi: 10.1016/j.neubiorev.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Lennox BR, Coles AJ, Vincent A. Antibody-mediated encephalitis: A treatable cause of schizophrenia. Br J Psychiatry. 2012;200:92–94. doi: 10.1192/bjp.bp.111.095042. [DOI] [PubMed] [Google Scholar]
- 14.Lisanby SH. Electroconvulsive therapy for depression. N Engl J Med. 2007;357:1939–45. doi: 10.1056/NEJMct075234. [DOI] [PubMed] [Google Scholar]
- 15.Macaluso M, Preskorn SH. How biomarkers will change psychiatry: from clinical trials to practice. Part I: Introduction. J Psychiatr Pract. 2012;18:118–21. doi: 10.1097/01.pra.0000413277.11091.25. [DOI] [PubMed] [Google Scholar]
- 16.Malhi GS, Loo C, Cahill CM, Lagopoulos J, Mitchell P, Sachdev P. “Getting physical”: The management of neuropsychiatric disorders using novel physical treatments. Neuropsychiatr Dis Treat. 2006;2:165–79. doi: 10.2147/nedt.2006.2.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin JB. The integration of neurology, psychiatry, and neuroscience in the 21st century. Am J Psychiatry. 2002;159:695–704. doi: 10.1176/appi.ajp.159.5.695. [DOI] [PubMed] [Google Scholar]
- 18.May A. Experience-dependent structural plasticity in the adult human brain. Trends Cogn Sci. 2011;15:475–82. doi: 10.1016/j.tics.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Mendez MF, Manes F. The emerging impact of social neuroscience on neuropsychiatry and clinical neuroscience. Soc Neurosci. 2011;6:415–19. doi: 10.1080/17470919.2011.624806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nierenberg AA. Psychiatry and neuropsychiatry as a craft. CNS Spectr. 2009;14:408–9. doi: 10.1017/s1092852900020356. [DOI] [PubMed] [Google Scholar]
- 21.Sachdev P. The Curriculum Committee of the INA. Core curriculum in Neuropsychiatry of the International Neuropsychiatric Association. In: Miyoshi K, Morimura Y, Maeda K, editors. Neuropsychiatric Disorders. Tokyo: Springer; 2010. pp. 317–46. [Google Scholar]
- 22.Sachdev P. International Neuropsychiatric Association (Guest Editorial) Neuropsychiatr Dis Treat. 2005;1:191–2. [PMC free article] [PubMed] [Google Scholar]
- 23.Sachdev PS. Whither neuropsychiatry? J Neuropsychiatry Clin Neurosci. 2005;17:140–4. doi: 10.1176/jnp.17.2.140. [DOI] [PubMed] [Google Scholar]
- 24.Silver JM. Behavioural neurology and neuropsychiatry is a subspecialty. J Neuropsychiatry Clin Neurosci. 2006;18:146–8. doi: 10.1176/jnp.2006.18.2.146. [DOI] [PubMed] [Google Scholar]
- 25.Tüzün E, Dalmau J. Limbic encephalitis and variants: Classification, diagnosis and treatment. Neurologist. 2007;13:261–71. doi: 10.1097/NRL.0b013e31813e34a5. [DOI] [PubMed] [Google Scholar]
- 26.Wenisch E, Cantegreil-Kallen I, De Rotrou J, Garrigue P, Moulin F, Batouche F, et al. Cognitive stimulation intervention for elders with mild cognitive impairment compared with normal aged subjects: Preliminary results. Aging Clin Exp Res. 2007;19:316–22. doi: 10.1007/BF03324708. [DOI] [PubMed] [Google Scholar]