Abstract
Objective
Vibratory perception threshold (VPT) assesses a distinct yet related sensory pathway that has been associated with neuropathic arthropathy but has not been assessed in knee osteoarthritis (OA). The purpose of this study was to evaluate VPT in subjects with knee OA to determine whether the lower extremity afferent deficits observed in knee OA involve more than just proprioception.
Methods
Twenty-seven individuals with symptomatic and radiographic knee OA were compared with 14 age-matched normal subjects. VPT was assessed using a biothesiometer. Five sites of the lower extremity were evaluated. VPT of OA subjects was compared with VPT of normal subjects.
Results
VPT of the OA subjects was significantly reduced at all 5 testing sites compared with normal subjects (P < 0.05 at all sites). VPT scores (mean ± SEM volts) for OA subjects and normal subjects were as follows: first metatarsophalangeal joint (15.0 ± 1.9 versus 6.4 ± 0.9), medial malleolus (22.0 ± 2.2 versus 12.3 ± 1.4), lateral malleolus (22.3 ± 2.0 versus 10.4 ± 0.8), medial femoral condyle (25.8 ± 1.8 versus 15.9 ± 1.9), and lateral femoral condyle (27 ± 1.9 versus 18.9 ± 2.4).
Conclusion
This was the first study to evaluate VPT in OA and demonstrate that VPT is reduced at the lower extremity of subjects with knee OA. The noted deficits in VPT may have significant implications in the neuromechanical pathophysiology of OA. VPT is a simple and reliable technique to measure sensory deficits in subjects with OA of the knee.
INTRODUCTION
Patients with osteoarthritis (OA) of the knee have been shown to have proprioceptive sensory deficits in the lower extremities (1– 4), and it has been hypothesized that this reduced sense of position in space may be pathophysiologically related to the onset or progression of knee OA (4,5). To date, observations concerning lower extremity sensory deficits in persons with OA have been restricted to proprioceptive loss. However, the methods used to assess proprioceptive acuity through measurements of balance, joint position sense, and/or kinesthesia testing at the knee (1–3) have been criticized for their poor reliability and variability in results, particularly because they may be confounded by factors such as patient memory, reaction time, and concentration, as well as joint pain during testing (6). Furthermore, there appears to be poor correlation between these sensory testing modalities (2,7).
It remains unclear whether the sensory deficits in knee OA are restricted purely to proprioception or whether they involve other afferent pathways as well. For example, vibratory perception travels through similar neurologic pathways to proprioception, therefore vibratory sense may also be decreased in knee OA (8). Vibratory perception threshold (VPT) is a sensory measure that is commonly used to evaluate diabetic neuropathy (9,10) and that has been associated with neuropathic arthropathy (11,12), but has not previously been assessed in persons with knee OA. The purpose of this study was to evaluate VPT in subjects with OA of the knee, and to test the hypothesis that lower extremity afferent deficits observed in knee OA involve more than only proprioception, and therefore that these subjects would exhibit reduced vibratory acuity (increased VPT) compared with normal subjects without OA.
SUBJECTS AND METHODS
Subjects
This research was in compliance with the Declaration of Helsinki. The study was approved by the institution’s review board for studies involving human subjects and informed consent was obtained from all subjects. We conducted a cross-sectional study comparing sensory testing data from 2 groups of subjects: subjects with knee OA and healthy age-matched controls. Subjects were recruited through ongoing studies and the clinical population of the Section of Rheumatology at Rush University Medical Center. Inclusion criteria for the knee OA group included the presence of symptomatic OA of the knee, which was defined by the American College of Rheumatology clinical criteria for the classification and reporting of knee OA (13) and by a walking pain score of least 20 mm on a 100-mm scale (corresponding to question 1 of the visual analog format of the knee-directed Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC]) (14), and radiographic OA of the symptomatic knee documented within the preceding 6 months with a Kellgren/Lawrence (K/L) grade of 2 or higher out of a maximum of 4 (15,16). For the normal comparator group, healthy age-matched subjects were recruited and were excluded if they had pain or symptoms of arthritis in either lower extremity (site-directed WOMAC visual analog scale ≥ 10 mm) or definite evidence of radiographic knee OA (K/L grade >1). The exclusion criteria for all subjects were the presence of systemic inflammatory arthropathy, any history of knee or hip replacement, the presence of diabetes mellitus for >10 years, or evidence by history or physical examination of neurologic disease.
Testing procedures
All subjects underwent clinical evaluation, weight-bearing bilateral anteroposterior knee radiography, and testing for VPT using a biothesiometer (Bio-Medical Instrument, Newberry, OH) (Figure 1) according to previously published methods (17). The biothesiometer has a vibrating tip that oscillates at a constant frequency of 120 Hz. A manual dial on the instrument is used to adjust the voltage; the amplitude of the vibration from the tip is proportional to the square of the applied voltage. The tip was applied with uniform pressure to the bony prominences at 5 sites: first metatarsophalangeal (MTP) joint, medial malleolus, lateral malleolus, medial femoral condyle, and lateral femoral condyle. Uniform pressure was achieved by using the weight of the testing device itself as the sole source of pressure of the biothesiometer tip against the skin. This was accomplished by holding the applicator at its proximal end where it attaches to the power cord (Figure 1) with the subjects in a dependent position during testing. For example, for testing the MTP joint, the plantar aspect of the subjects’ feet was flat against the examining table. Likewise, for testing the left medial malleolus and left medial femoral condyle, subjects laid on their left side and for the lateral malleolus and lateral femoral condyle, on their right side. A single investigator (AA) tested all subjects. Prior to testing, patients were given a demonstration of the effect of the biothesiometer on their hand, with an initial demonstration of pressure from the weight of the machine only with the voltage set at zero, and then a demonstration of the sensation of vibration with the voltage increased from zero to moderate and then high levels.
Figure 1.
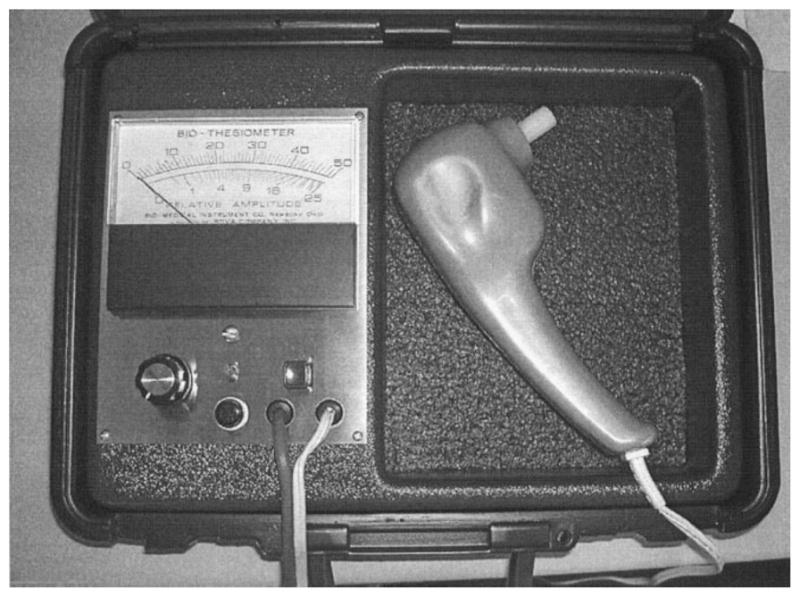
The biothesiometer (Bio-Medical Instrument, Newberry, OH) consists of a handheld applicator with a vibrating tip (right). The voltage intensity of the instrument is adjusted with a manual dial (lower left) and can be visualized on the meter dial (upper left).
At each of the 5 testing sites in the lower extremity, the voltage on the biothesiometer was initially set at zero, and then the voltage was increased by 1 volt per second. Subjects remained supine and did not move the extremity during the testing procedure. Subjects were instructed to comment on their first sensation of vibration, and this was noted as the VPT. A higher VPT threshold represents a greater sensory deficit. The VPT measurement was then obtained a second time by resetting the voltage to zero and again increasing the voltage by one volt per second. The correlations between the first and second readings in this group were high (r = 0.93– 0.99, P < 0.001) and the second VPT measurement was averaged with the first VPT reading at each site to give the final VPT measurement reading. Of note, at each site the biothesiometer tip was not moved from the surface of the skin between the first and second trials. This was done to increase reliability of testing by reducing the chance that replacement of the tip over a slightly different site relative to the first testing site would result in different measurements. The intraclass correlation coefficient was 0.96 – 0.99 between initial and repeat testing on separate days. Previous studies using the biothesiometer to evaluate VPT have similarly demonstrated high reproducibility and reliability (9,17,18).
Statistical analysis
Statistical analysis was performed using SPSS software (SPSS, Chicago, IL). An independent samples t-test was used to compare VPT of OA subjects with normal controls. Prior to testing a power analysis was performed to determine sample sizes. A sample size of 30 OA subjects and 15 normal subjects provided >90% power to detect differences (at a P value less than 0.05) in vibratory sensation, even after considering that the difference in vibratory threshold in our population of subjects may be half the difference between diabetic subjects and normal subjects in previous studies (9,10,18). Linear regression was used to evaluate the effects of age, body mass index (BMI), and sex on the results.
RESULTS
Twenty-seven OA subjects and 14 normal controls completed the study. In the OA group there were 22 women (81.5%) and 5 men (18.5%), and in the normal group there were 9 women (64.3%) and 5 men (35.7%). The mean ± SD ages of the OA and normal subjects were not significantly different (54 ± 12 years and 47 ± 14 years, respectively; P = 0.106). BMI was significantly higher in the OA group compared with the normal group (mean ± SD 37.8 ± 8.6 kg/m2 and 29.8 ± 5.6 kg/m2, respectively; P = 0.001). The OA subjects included 17 patients with K/L grade 2 radiographic OA, 8 patients with K/L grade 3, and 2 patients with K/L grade 4. WOMAC pain scores, based on the summed scores of pain questions 1–5 of the knee-directed WOMAC, ranged from 114 to 483 (out of a maximum of 500) in the knee OA group, with a mean ± SD score of 308 ± 94.
VPT testing revealed that within each of the 2 groups, there was a normal physiologic increase in VPT from distal testing sites to more proximal sites (8,19). VPT was significantly increased at all 5 testing sites of the OA subjects compared with normal controls (Table 1).
Table 1.
Comparison of VPT values between OA subjects and normal subjects*
| OA | Control | P | |
|---|---|---|---|
| First MTP | 15.0 ± 9.9 | 6.4 ± 3.3 | <0.001 |
| Medial malleolus | 22.0 ± 11.7 | 12.3 ± 5.2 | 0.001 |
| Lateral malleolus | 22.3 ± 10.5 | 10.4 ± 3.2 | <0.001 |
| Medial femoral condyle | 25.8 ± 9.3 | 15.9 ± 7.0 | 0.001 |
| Lateral femoral condyle | 27.0 ± 9.7 | 18.9 ± 9.1 | 0.014 |
Values are the mean ± SD volts unless otherwise indicated. VPT = vibratory perception threshold (volts); OA = osteoarthritis; MTP = metatarsophalangeal joint.
A subgroup analysis eliminating age outliers was performed to more closely match the ages between the groups and thus to exclude any confounding influence of age on the results. The subgroup was created by excluding the older OA subjects and the younger normal subjects. The subgroup had 23 subjects in the OA group and 11 subjects in the normal group. The mean ± SD ages of the OA and normal subjects in the subgroup were 50.6 ± 9.0 years and 51.8 ± 10.8 years, respectively (P = 0.76). The mean VPT score at all 5 testing sites remained significantly different between the groups (P < 0.05).
Secondary analyses using linear regression were also performed to evaluate the effects of BMI and sex on the results. At all sites, OA subjects had significantly reduced vibration sense compared with normal subjects, adjusting for differences in BMI (β = −1.0 to −0.16, P = 0.09 – 0.81) and sex (β = −0.63 to 0.31, P = 0.34 – 0.99). Furthermore, there was not a significant relationship between BMI and vibratory sense in the group as a whole (β = −0.30 to 0.1, P = 0.08 – 0.95). Regarding sex in the group overall, men had significantly increased vibration at the medial knee (r2 = 0.24, P = 0.02) and lateral knee (r2 = 0.21, P = 0.03) compared with women. However, there was no significant impact of sex at the other sites or on the differences in vibration between the OA and normal groups.
Although subjects with diabetes of >10 years’ duration or history of neuropathy were excluded, 3 subjects with diabetes were included in the OA group. There were no subjects with diabetes in the control group. The results did not change after excluding the 3 diabetic subjects from the analysis.
DISCUSSION
This study demonstrated significant deficits in vibratory sensation at the lower extremity in subjects with OA of the knee compared with normal age-matched healthy subjects. These deficits in VPT may have significant implications both for the assessment of sensory deficits in subjects with OA and regarding the neuromechanical pathophysiology of knee OA.
Previous studies have demonstrated that proprioceptive acuity in the lower extremities is diminished with normal aging, and that there are significant proprioceptive deficits in knee OA independent of aging (1–3). Proprioceptive sense is believed to propagate from peripheral mechano-receptors through large-fiber (specifically, Aαβ) afferent nerves to the dorsal root ganglia of the dorsal columns of the spinal cord (8). Proprioception usually refers to postural, positional, or kinetic information provided to the central nervous system by peripheral mechanoreceptors (8). Thus, proprioception has been measured in previous studies as balance (3), joint position sense (ability to reproduce a specified flexion angle at the knee) (2,3), and kinesthesia (ability to detect subtle flexion or extension at the knee) (1,2). Because these methods require movement of a diseased and potentially unstable joint, they may be affected by disease severity and pain, independent of any true lower extremity sensory deficits. Results from these methods may be further confounded by the fact that they require a fair degree of comprehension, concentration ability, and memory, and may be influenced by patients’ reaction time. Thus, the reliability of these procedures in most instances is not ideal (6). Furthermore, most of the testing procedures for proprioception evaluation are moderately lengthy and require specialized equipment that is not readily available.
Vibratory sense has also been shown to decrease with age (17) and this study has now demonstrated a further significant reduction in vibratory sense in knee OA. In addition to age, some studies have previously suggested a possible effect of sex on VPT, in which men generally have higher VPT values than women (17). In the present investigation, neither age nor sex had a significant influence on the primary results. Furthermore, on the basis of previous data (17), it would have been expected that the increased proportion of men in the control group would have, if anything, underestimated the difference in VPT between the groups.
Vibratory sense is believed to travel through the same type of large afferent nerve fibers (Aαβ) as proprioception sense (8). The assessment of vibratory sense is both technically easier and objectively less influenced by confounding factors than proprioception testing. Subjects are supine during the procedure and are not required to move the extremity when obtaining the VPT, thus pain severity and coordination ability do not influence the VPT. Similarly, memory is not a confounder because subjects are not required to remember a particular position. And although subjects do have to indicate the moment at which they initially feel a vibration, this is done verbally and does not require the push of a button; therefore, reaction time is less of an issue. This study, similar to previous studies using VPT (9,17,18), demonstrated high reliability and reproducibility with the procedure. The equipment required for testing VPT is simple, portable, and inexpensive and the time requirement for testing is significantly shorter than that required for proprioception. In this study, 5 sites of the lower extremity were tested and the average total testing time was approximately 10 minutes. Because this was the first investigation of VPT in subjects with OA, the pattern of any sensory deficits had not yet been elucidated; therefore, multiple sites of the lower extremity were evaluated. In contrast to diabetes, which is the most common indication for vibratory testing, OA is generally considered to be a localized disease. In diabetes, the first MTP has been the site tested most often because of the strong association between distal neuropathy and foot ulcerations. Here, a physiologic increase in VPTs was observed in both the OA group and normal group from distal to proximal sites. This may be related to differences in proximal soft tissue density or the density of afferent sensory fibers, and has been reported previously (8,19). Nevertheless, because the subjects with OA had significantly different VPTs from the normal controls at each testing site, it is possible that evaluation of a single site, for example, the first MTP, may be sufficient for evaluation in OA as well in diabetes.
Most previous studies of VPT have been performed on subjects with diabetes mellitus. Most studies in subjects with diabetes have evaluated the first MTP only. Although values of VPT vary between studies depending the age of the study group, severity of neuropathy, or specific testing procedure and site, most subjects with diabetes have 33–50% greater absolute VPT values at the first MTP than OA subjects in the current study (17,19). Future studies should look more closely at whether vibratory loss in diabetes may increase the incidence of OA in this group.
Because proprioception and vibratory sensation represent similar sensory modalities, the hypotheses for the role of these deficits in the pathophysiology of knee OA would be similar. Current hypotheses suggest that diminished sensory input may interfere with or diminish protective muscular reflexes around the joint, leading to increased mechanical load on the joint and subsequent damage to cartilage (4,5).
It should be recognized that neither this study nor previous studies have established a causal relationship between the sensory deficits and the development of OA of the knee. Therefore, it is not clear whether these deficits precede or follow the development of knee OA. Furthermore, it is not known whether sensory deficits are focal and limited to the lower extremity or more diffuse abnormalities in these subjects. In addition, although proprioception and vibration sense travel through similar neurologic pathways, future studies should evaluate correlations between these sensory modalities.
To our knowledge, this is the first study to evaluate VPT in OA and to demonstrate that VPT is increased at the lower extremity of subjects with OA of the knee. As a single testing technique, VPT evaluation may be the simplest and most reliable technique for identifying sensory loss in these subjects.
Acknowledgments
Supported by the NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases (grants K23-AR-049748 and P50-AR-048941) and the Schweppe Foundation.
Footnotes
AUTHOR CONTRIBUTIONS
Dr. Shakoor had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Shakoor, Agrawal, Block.
Acquisition of data. Agrawal.
Analysis and interpretation of data. Shakoor, Agrawal, Block.
Manuscript preparation. Shakoor, Agrawal, Block.
Statistical analysis. Shakoor, Agrawal.
References
- 1.Pai YC, Rymer WZ, Chang RW, Sharma L. Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum. 1997;40:2260–5. doi: 10.1002/art.1780401223. [DOI] [PubMed] [Google Scholar]
- 2.Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73:53– 6. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- 3.Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis. 1997;56:641– 8. doi: 10.1136/ard.56.11.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma L. Proprioceptive impairment in knee osteoarthritis. Rheum Dis Clin North Am. 1999;25:299–314. doi: 10.1016/s0889-857x(05)70069-7. [DOI] [PubMed] [Google Scholar]
- 5.Shakoor N, Moisio K. A biomechanical approach to musculoskeletal disease. Best Pract Res Clin Rheumatol. 2004;18:173–86. doi: 10.1016/j.berh.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Lephart SM. Proprioception and neuromuscular control in joint stability. Champaign (IL): Human Kinetics; 2000. [Google Scholar]
- 7.Grob KR, Kuster MS, Higgins SA, Lloyd DG, Yata H. Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br. 2002;84:614– 8. doi: 10.1302/0301-620x.84b4.11241. [DOI] [PubMed] [Google Scholar]
- 8.Goetz CG. Textbook of clinical neurology. 3. Philadelphia: WB Saunders; 2007. [Google Scholar]
- 9.Davis EA, Jones TW, Walsh P, Byrne GC. The use of biothesiometry to detect neuropathy in children and adolescents with IDDM. Diabetes Care. 1997;20:1448–53. doi: 10.2337/diacare.20.9.1448. [DOI] [PubMed] [Google Scholar]
- 10.Olsen BS, Nir M, Kjaer I, Volund A, Mortensen HB. Elevated vibration perception threshold in young patients with type 1 diabetes in comparison to non-diabetic children and adolescents. Diabet Med. 1994;11:888–92. doi: 10.1111/j.1464-5491.1994.tb00374.x. [DOI] [PubMed] [Google Scholar]
- 11.Foltz KD, Fallat LM, Schwartz S. Usefulness of a brief assessment battery for early detection of Charcot foot deformity in patients with diabetes. J Foot Ankle Surg. 2004;43:87–92. doi: 10.1053/j.jfas.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Rajbhandari SM, Jenkins RC, Davies C, Tesfaye S. Charcot neuroarthropathy in diabetes mellitus. Diabetologia. 2002;45:1085–96. doi: 10.1007/s00125-002-0885-7. [DOI] [PubMed] [Google Scholar]
- 13.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29:1039– 49. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 14.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833– 40. [PubMed] [Google Scholar]
- 15.Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman BN, Aliabadi P, et al. The incidence and natural history of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1995;38:1500–5. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frenette B, Mergler D, Ferraris J. Measurement precision of a portable instrument to assess vibrotactile perception threshold. Euro J App Physiol Occup Physiol. 1990;61:386–91. doi: 10.1007/BF00236057. [DOI] [PubMed] [Google Scholar]
- 18.Van Deursen RW, Sanchez MM, Derr JA, Becker MB, Ulbrecht JS, Cavanagh PR. Vibration perception threshold testing in patients with diabetic neuropathy: ceiling effects and reliability. Diabet Med. 2001;18:469–75. doi: 10.1046/j.1464-5491.2001.00503.x. [DOI] [PubMed] [Google Scholar]
- 19.Armstrong DG, Hussain SK, Middleton J, Peters EJ, Wunderlich RP, Lavery LA. Vibration perception threshold: are multiple sites of testing superior to single site testing on diabetic foot examination? Ostomy Wound Manage. 1976;44:70– 4. [PubMed] [Google Scholar]


