Abstract
Implant-associated infection is becoming more and more challenging to the healthcare industry worldwide due to increasing antibiotic resistance, transmission of antibiotic resistant bacteria between animals and humans, and the high cost of treating infections.
In this study, we disclose a new strategy that may be effective in preventing implant-associated infection based on the potential antimicrobial properties of platelet-rich plasma (PRP). Due to its well-studied properties for promoting healing, PRP (a biological product) has been increasingly used for clinical applications including orthopaedic surgeries, periodontal and oral surgeries, maxillofacial surgeries, plastic surgeries, sports medicine, etc.
PRP could be an advanced alternative to conventional antibiotic treatments in preventing implant-associated infections. The use of PRP may be advantageous compared to conventional antibiotic treatments since PRP is less likely to induce antibiotic resistance and PRP's antimicrobial and healing-promoting properties may have a synergistic effect on infection prevention. It is well known that pathogens and human cells are racing for implant surfaces, and PRP's properties of promoting healing could improve human cell attachment thereby reducing the odds for infection. In addition, PRP is inherently biocompatible, and safe and free from the risk of transmissible diseases.
For our study, we have selected several clinical bacterial strains that are commonly found in orthopaedic infections and examined whether PRP has in vitro antimicrobial properties against these bacteria. We have prepared PRP using a twice centrifugation approach which allows the same platelet concentration to be obtained for all samples. We have achieved consistent antimicrobial findings and found that PRP has strong in vitro antimicrobial properties against bacteria like methicillin-sensitive and methicillin-resistant Staphylococcus aureus, Group A Streptococcus, and Neisseria gonorrhoeae. Therefore, the use of PRP may have the potential to prevent infection and to reduce the need for costly post-operative treatment of implant-associated infections.
Keywords: Infection, Issue 74, Infectious Diseases, Immunology, Microbiology, Medicine, Cellular Biology, Molecular Biology, Bacterial Infections and Mycoses, Musculoskeletal Diseases, Biological Factors, Platelet-rich plasma, bacterial infection, antimicrobial, kill curve assay, Staphylococcus aureus, clinical isolate, blood, cells, clinical techniques
Introduction
Implant-associated infection is a significant clinical complication. Staphylococcus aureus (S. aureus) is one of the most common microorganisms isolated from implant-associated infections. It is capable of producing a biofilm that covers the surfaces of implants and may lead to antibiotic-resistant infection 1,2. Treatment of implant-associated infection frequently requires long-term hospitalization for repeated debridements and prolonged parenteral antibiotic therapy. In antibiotic resistant cases, removal of the implant may be necessary. The rising resistance of bacteria to antibiotics has also been referred to by the Centers for Disease Control and Prevention (CDC) as "one of the world's most pressing health problems." In time, without the development of new and effective antimicrobial treatments, it is possible that multi-drug resistant pathogens will be untreatable with conventional antibiotics. Prevention of implant-associated infection is therefore important and novel prophylactic agents or approaches are needed for preventing such infections.
Platelet-rich plasma (PRP) is a concentration of autologous blood that contains over 30 growth factors which can help with bone and bone graft healing 3-5. The application of PRP to enhance bone regeneration and soft tissue maturation has been increasingly reported in clinics because of its high concentration of various growth factors released by platelets.
Several characteristics of PRP indicate that PRP may also have antimicrobial properties 6-9. PRP contains a large number of platelets, a high concentration of leukocytes (which may possess host-defense actions against bacteria and fungi), and multiple antimicrobial peptides 7,8,10. In a recent study of a large cohort of cardiac surgical patients, it was revealed that the intraoperative use of PRP-gel during wound closure significantly decreased the incidence of superficial and deep sternum infection 11. For these reasons and observations, we hypothesized that PRP, besides its well-studied healing-promoting properties, has antimicrobial properties. The potential advantages of using PRP to prevent infection may include: (i) PRP is less likely to induce resistance compared to conventional antibiotic treatments. (ii) PRP also has properties that promote healing which may have a synergistic effect on infection prevention; PRP's healing-promoting properties could provide a seal to prevent bacterial attachment thereby reducing the odds for infection as pathogens and human cells are racing for implant surfaces 12,13. (iii) PRP is inherently biocompatible, and safe and free from the risk of transmissible diseases.
Our long-term goal is to use PRP as a new approach to prevent implant-associated infections. The aim of this study was to prepare PRP using a twice centrifugation approach, to examine PRP's in vitro antimicrobial properties, and to describe the protocols for evaluating such antimicrobial properties.
Protocol
1. Preparation and Activation of PRP
1.1 Blood draw
Anesthetize rabbit by inhalation of isoflurane (2% in O2 for induction and 1% for maintenance).
Draw 2 ml 0.129 M tri-sodium citrate (an anticoagulent solution) into a 20 ml syringe. The tri-sodium citrate solution is prepared by dissolving 1.897 g tri-sodium citrate in 50 ml distilled H2O and filtering with a 0.22 μm sterile filter.
Sterilize the rabbit ear using 70% ethanol.
Draw blood (e.g. 5 ml) from the rabbit ear vein via a butterfly needle (25 G) connected to the syringe.
Mix the blood with the tri-sodium citrate solution by gentle agitation. The volume ratio of blood and tri-sodium citrate solution is 9:1.
1.2 PRP preparation (Figure 1)
Transfer the anticoagulated blood to a 50 ml plastic centrifuge tube. Take an aliquot of 10 μl blood to determine the baseline platelet count using hemocytometry.
Centrifuge the blood at 300 x g for 10 min at room temperature (RT) in a centrifuge with a swing-out rotor. Set the acceleration and brake velocity to low (Figure 1).
After centrifugation, the blood is separated into three layers. The bottom layer is mainly red blood cells, the middle layer (commonly referred to as the "buffy coat") is composed of concentrated platelets and leukocytes, and the top layer is mainly plasma, which is the liquid component of blood, and platelets (Figure 1). Carefully transport the centrifuge tube to a cell culture hood; do not disturb the layers. Transfer all of the plasma, buffy coat, and 2-3 mm thick red blood cell layer into a 15 ml plastic tube using a 1 ml plastic pipettor.
Centrifuge the transferred sample a second time at 3,000 x g for 15 min at RT. The top layer (supernatant) is considered platelet poor plasma (PPP) and is transferred to a new tube.
Obtain PRP by adjusting the platelet concentration in the remaining blood sample using PPP to obtain 2.0 x 106 platelets/μl (determined by hemocytometry).
1.3 PRP activation
Prepare PRP activation solution by dissolving 5,000 IU bovine thrombin with 5 ml 10% calcium chloride to the working concentration of 1,000 IU/ml.
Add the activation solution to PRP and PPP, and mix the solution by repeatedly pipetting to form PRP- and PPP-gels. The volume ratio of the activation solution to PRP or PPP is 1:4.
2. In vitro Antimicrobial Test of PRP Using Kill Curve Assay (Figure 2)
Using a sterile inoculating loop, add several colonies of S. aureus from its overnight plate culture into 5 ml of Mueller Hinton broth (MHB) in a plastic tube. Vortex briefly and then incubate the sample for 2 hr at 37 °C. Next, the optical density of the bacterial media was determined using a spectrophotometer and adjusted to an optical density equal to ~1 x 108 CFU/ml based on the pre-determined standard curve.
Make a 100x dilution using PBS to obtain 1 x 106 CFU/ml and place the inoculums on ice.
Set up and label sterile, disposable 5 ml round-bottom polystyrene tubes, and prepare the following sample groups as indicated in Table 1 for a final volume of 2 ml in each tube.
Add PRP, PPP, or PBS first to the polystyrene tubes, followed by the thrombin solution for activation (gel formation). Next, add MHB and then the S. aureus inoculums (1 x 106 CFU/ml) to obtain the final concentration of 1 x 105 CFU/ml.
Incubate the tubes at 37 °C with orbital agitation at 150 rpm.
At pre-determined time points (e.g. 0, 1, and 2 hr), mix the solutions in each tube via repeat pipetting (this step is important since bacteria may be trapped inside the PRP gel). Take 10 μl of sample, dilute serially with sterile 0.9% saline, and pipette a 100 μl aliquot of each dilution onto a Tryptic soy agar (TSA, with 5% sheep blood) plate for CFU counting.
Culture the agar plates overnight at 37 °C, then count and record the plate colonies. Plot data on a logarithimic scale with time (hr) on the x-axis and CFU/ml on the y-axis.
Representative Results
PRP is reproducibly prepared using a twice centrifugation approach (Figure 1). PRP is found to present strong (up to 100-fold reduction in CFUs) in vitro antimicrobial properties against methicillin resistant S. aureus (MRSA) (Figure 3), which is commonly found in hospitals worldwide 14. Similarly, PRP has strong antimicrobial properties against methicillin sensitive S. aureus (MSSA), Group A Streptococcus, and Neisseria gonorrhoeae.
The twice centrifugation approach allows acquisition of PRP with the same platelet concentration (i.e. 2.0 x 106 platelets/μl) but concentrated (~10 times above the baseline in blood; Figure 4) and allows us to obtain consistent antimicrobial findings; no significant differences in CFU findings among PRPs from different individual animals (i.e. rabbits) have been observed.
| Groups | PRP/PPP/PBS | MHB | MRSA inoculum |
| Control | None | 1,800 μl | 200 μl |
| Control | None | 2,000 μl | None |
| Control | PBS + thrombin (200 μl) | 1,600 μl | 200 μl |
| PPP | PPP + thrombin (200 μl) | 1,600 μl | 200 μl |
| PRP | PRP + thrombin (200 μl) | 1,600 μl | 200 μl |
Table 1. Experimental samples for antimicrobial assessment of PRP.
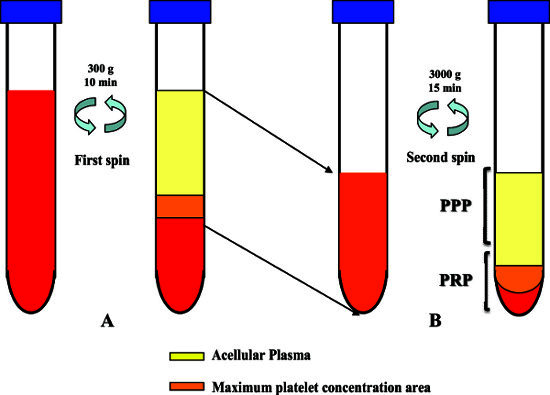 Figure 1. PRP preparation using a twice centrifugation procedure. (A) First centrifugation. After the first centrifugation, three layers are formed, and the top two layers (i.e. plasma and buffy coat layers) and 2-3 mm of the bottom layer (i.e. red blood cell layer) are transferred to a second sterile centrifuge tube. (B) Second centrifugation. After the second centrifugation, the top layer is transferred to a new sterile tube and designated as PPP. The remaining is adjusted with PPP to a platelet concentration of 2.0 x 106 platelets/μl and designated as PRP.
Figure 1. PRP preparation using a twice centrifugation procedure. (A) First centrifugation. After the first centrifugation, three layers are formed, and the top two layers (i.e. plasma and buffy coat layers) and 2-3 mm of the bottom layer (i.e. red blood cell layer) are transferred to a second sterile centrifuge tube. (B) Second centrifugation. After the second centrifugation, the top layer is transferred to a new sterile tube and designated as PPP. The remaining is adjusted with PPP to a platelet concentration of 2.0 x 106 platelets/μl and designated as PRP.
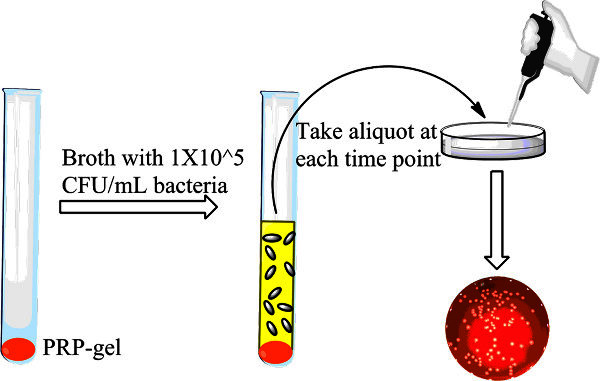 Figure 2. Experimental set-up for assessing the antimicrobial properties of PRP using the kill curve assay. First, PRP or PPP is added to the test tubes, and immediately activated with thrombin solution. Next, MHB is added followed by bacterial inoculums. Aliquots of samples are taken at different time points and plated for CFU counts.
Figure 2. Experimental set-up for assessing the antimicrobial properties of PRP using the kill curve assay. First, PRP or PPP is added to the test tubes, and immediately activated with thrombin solution. Next, MHB is added followed by bacterial inoculums. Aliquots of samples are taken at different time points and plated for CFU counts.
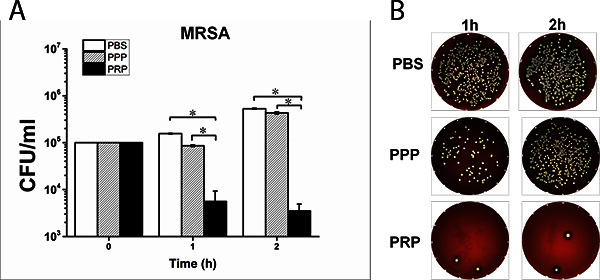 Figure 3. PRP, PPP, or PBS are placed in a sterile 5 ml polystyrene tube along with thrombin, MHB broth, and MRSA inoculum and then incubated at 37 °C with orbital agitation at 150 rpm. At pre-determined time points (i.e. 1 and 2 hr), aliquots of samples are taken and plated for CFU counts. (A) CFU data and (B) representative plate images at 10-2 dilution. Significant reduction (~100-fold at 2 hr) of MRSA growth is obtained using PRP compared to PPP and PBS controls. This is true for bacteria like MSSA, Group A Streptococcus, and Neisseria gonorrhoeae as well.
Figure 3. PRP, PPP, or PBS are placed in a sterile 5 ml polystyrene tube along with thrombin, MHB broth, and MRSA inoculum and then incubated at 37 °C with orbital agitation at 150 rpm. At pre-determined time points (i.e. 1 and 2 hr), aliquots of samples are taken and plated for CFU counts. (A) CFU data and (B) representative plate images at 10-2 dilution. Significant reduction (~100-fold at 2 hr) of MRSA growth is obtained using PRP compared to PPP and PBS controls. This is true for bacteria like MSSA, Group A Streptococcus, and Neisseria gonorrhoeae as well.
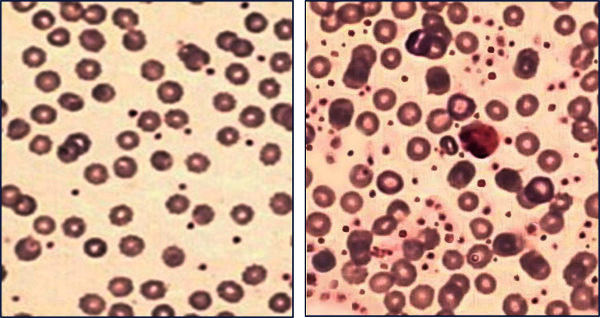 Figure 4. Blood smears of whole blood (left) and PRP (right). PRP prepared from the twice centrifugation approach has ~10 times the number of platelets compared to whole blood.
Figure 4. Blood smears of whole blood (left) and PRP (right). PRP prepared from the twice centrifugation approach has ~10 times the number of platelets compared to whole blood.
Discussion
Platelet-rich plasma has been increasingly used for clinical applications due to its healing-promoting properties 15-17. In the present study, PRP was presented as a new approach for infection prevention. PRP was found to have strong antimicrobial properties against MRSA, MSSA, Group A Streptococcus, and Neisseria gonorrhoeae. The major advantages of PRP, compared to conventional antibiotic treatments, for infection prevention include: (1) Current antibiotic therapies are facing challenges including increasingly reported antibiotic resistance 14,18-20. PRP could be an advanced alternative because (i) PRP's platelet microbicidal proteins may possess chemotactic properties for immune cells such as neutrophils, monocytes and T cells which play important roles in defending against pathogen invasion 21, and (ii) compared to conventional antibiotics, platelet microbicidal proteins are less prone to inducing bacterial resistance due to the difficulty in changing bacterial membrane structures 22. (2) PRP not only reduces infections but also promotes wound healing; both are costly in terms of trauma, time, and money.
PRP has recently attracted increased interest. However, there are numerous complex variations among PRP preparation protocols including the starting number of platelets, the use of anticoagulants, the inclusion of leukocytes, and the use of activators 23-27. The variation in PRP preparation contributes in part to the controversial outcomes both in animal and clinical studies 28. As a result, a big issue for PRP studies is to control the variation. In the current study, a twice centrifugation approach was performed, and the platelet concentration of PRP was fixed at 2 x 106 platelets/μl (~10 times above the baseline in blood) to standardize the PRP preparation protocol and to limit the variability in PRP preparation. The twice centrifugation approach presented is simple, can be easily applied for isolation of PRP from blood of other animals and human beings, and has led to consistent in vitro antimicrobial properties of rabbit PRP in the present study. However, differences may still exist since the growth factors and other chemicals within or released from platelets may vary among individual cells and animals; some cell populations (e.g. leukocyte) were not controlled. Note that leukocyte-rich PRP was prepared and used in this study, since leukocytes are involved in direct bacterial killing and antigen-specific immune response. The protocols could be further modified to obtain leukocyte-poor PRP by carrying out a second centrifugation of only the top layer (i.e. plasma and platelet portion) after the first centrifugation (Figure 1).
In this study, 50 ml whole blood was used to obtain approximately 5 ml PRP. If blood volume is a concern, pooled blood from multiple animals may be used to prepare PRP. If clots form during blood draw and/or centrifugation, most likely some platelets are activated which will result in low platelet yield. Therefore, sufficient anticoagulants and gentle but thorough mixing are important steps for successful PRP isolation.
PRP was activated using thrombin in the present study. Other approaches including calcium chloride, exogenous or autologous thrombin with or without calcium chloride, mechanical stress (additional high speed centrifugation), and batroxobin can also be applied for PRP activation 29-32. Note that platelets activated by thrombin may likely release their granule contents much faster than platelets activated by other chemicals. The cause is that, besides its capability to convert factor XI to XIa, VIII to VIIIa, V to Va, and fibrinogen to fibrin, thrombin can promote platelet activation and aggregation via activation of protease-activated receptors on platelet cell membranes 33-35.
The kill curve assay was presented to assess the in vitro antimicrobial activity of PRP. Unlike the agar disk diffusion assay, the kill curve assay allows quantitative assessment of the rate of bactericidal activity over time. One critical step to properly disperse bacteria when counting CFUs is to mix the whole culture thoroughly by vigorous pipetting before the sample is drawn and vortexed for serial dilutions, as PRP gel may confound one's ability to properly disperse bacteria.
Overall, platelet-rich plasma has strong antimicrobial properties against bacteria such as S. aureus, Group A Streptococcus, and Neisseria gonorrhoeae. Besides its well-studied healing-promoting properties, PRP may serve as a new approach to prevent implant-associated infections. The mechanism of PRP's antimicrobial properties is still unknown and further investigations in this area are needed.
The limitations of this study include that PRP did not fully eliminate the bacteria under our experimental conditions (1 x 105 CFU/ml). This may be due to the high virulence of our clinical bacterial strains that were used; 1 x 102 CFU (0.1 ml) of S. aureus induced severe infections in vivo 36-38. Alternatively, the amount of PRP may be increased to achieve better bacterial elimination, or PRP can be used together with systemic or local administration of conventional antibiotics for infection prevention; the dual effects (i.e. antimicrobial and healing-promoting properties) of PRP may be advantageous in promoting healing while preventing infection. Another limitation is that PRP should not be used for patients who have already been systemically infected (e.g. sepsis patients). This is because bacteria in the blood may be passed on from PRP to the application site unless appropriate sterilization techniques are applied. We recommend careful examination of possible bacterial contaminations of PRP before its usage.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
The authors thank Therwa Hamza, John E. Tidwell, Nina Clovis, and Suzanne Smith for experimental assistance and Suzanne Smith for proofreading. The authors also thank John Thomas, PhD for providing the bacterial clinical isolates and John B. Barnett, PhD for his support and the use of the biological safety lab at the Department of Microbiology, Immunology and Cell Biology at West Virginia University. The authors acknowledge financial support from the Osteosynthesis and Trauma Care Foundation and National Science Foundation (#1003907). Microscope experiments and image analysis were also performed in the West Virginia University Imaging Facility, which is supported in part by the Mary Babb Randolph Cancer Center and NIH grant P20 RR016440.
Animal use for blood draws were approved by the West Virginia University Institutional Animal Care and Use Committee. All experiments were executed in compliance with all relevant guidelines, regulations, and regulatory agencies.
References
- Gristina AG. Biomaterial-centered infection: microbial adhesion versus tissue integration. Science. 1987;237:1588–1595. doi: 10.1126/science.3629258. [DOI] [PubMed] [Google Scholar]
- Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J. Bone Joint Surg. Am. 1985;67:264–273. [PubMed] [Google Scholar]
- Everts PA, et al. Reviewing the structural features of autologous platelet-leukocyte gel and suggestions for use in surgery. Eur. Surg. Res. 2007;39:199–207. doi: 10.1159/000101743. [DOI] [PubMed] [Google Scholar]
- Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP. Implant. Dent. 2001;10:225–228. doi: 10.1097/00008505-200110000-00002. [DOI] [PubMed] [Google Scholar]
- Toscano N, Holtzclaw D. Surgical considerations in the use of platelet-rich plasma. Compend. Contin. Educ. Dent. 2008;29:182–185. [PubMed] [Google Scholar]
- Cieslik-Bielecka A, Gazdzik TS, Bielecki TM, Cieslik T. Why the platelet-rich gel has antimicrobial activity? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007;103:303–306. doi: 10.1016/j.tripleo.2006.08.034. [DOI] [PubMed] [Google Scholar]
- Yeaman MR. The role of platelets in antimicrobial host defense. Clin. Infect. Dis. 1997;25:951–970. doi: 10.1086/516120. [DOI] [PubMed] [Google Scholar]
- Tang YQ, Yeaman MR, Selsted ME. Antimicrobial peptides from human platelets. Infect Immun. 2002;70:6524–6533. doi: 10.1128/IAI.70.12.6524-6533.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sharkawy H, et al. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. J. Periodontol. 2007;78:661–669. doi: 10.1902/jop.2007.060302. [DOI] [PubMed] [Google Scholar]
- Krijgsveld J, et al. Thrombocidins, microbicidal proteins from human blood platelets, are C-terminal deletion products of CXC chemokines. J. Biol. Chem. 2000;275:20374–20381. doi: 10.1074/jbc.275.27.20374. [DOI] [PubMed] [Google Scholar]
- Trowbridge CC, et al. Use of platelet gel and its effects on infection in cardiac surgery. J. Extra Corpor. Technol. 2005;37:381–386. [PMC free article] [PubMed] [Google Scholar]
- Gristina AG, Naylor P, Myrvik Q. Infections from biomaterials and implants: a race for the surface. Med. Prog. Technol. 1988;14:205–224. [PubMed] [Google Scholar]
- Subbiahdoss G, Kuijer R, Grijpma DW, vander Mei HC, Busscher HJ. Microbial biofilm growth vs. tissue integration: "the race for the surface" experimentally studied. Acta Biomater. 2009;5:1399–1404. doi: 10.1016/j.actbio.2008.12.011. [DOI] [PubMed] [Google Scholar]
- Klevens RM, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am. J. Sports Med. 2009;37:2259–2272. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- Carlson NE, Roach RB. Platelet-rich plasma: clinical applications in dentistry. J. Am. Dent. Assoc. 2002;133:1383–1386. doi: 10.14219/jada.archive.2002.0054. [DOI] [PubMed] [Google Scholar]
- Man D, Plosker H, Winland-Brown JE. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast. Reconstr. Surg. 2001;107:229–237. doi: 10.1097/00006534-200101000-00037. [DOI] [PubMed] [Google Scholar]
- Fridkin SK, et al. Epidemiological and microbiological characterization of infections caused by Staphylococcus aureus with reduced susceptibility to vancomycin, United States, 1997-2001. Clin. Infect. Dis. 1997;36:429–439. doi: 10.1086/346207. [DOI] [PubMed] [Google Scholar]
- Jackson CR, Fedorka-Cray PJ, Davis JA, Barrett JB, Frye JG. Prevalence, species distribution and antimicrobial resistance of enterococci isolated from dogs and cats in the United States. J. Appl. Microbiol. 2009;107:1269–1278. doi: 10.1111/j.1365-2672.2009.04310.x. [DOI] [PubMed] [Google Scholar]
- Murray CK, et al. Recovery of multidrug-resistant bacteria from combat personnel evacuated from Iraq and Afghanistan at a single military treatment facility. Mil. Med. 2009;174:598–604. doi: 10.7205/milmed-d-03-8008. [DOI] [PubMed] [Google Scholar]
- Durr M, Peschel A. Chemokines meet defensins: the merging concepts of chemoattractants and antimicrobial peptides in host defense. Infect Immun. 2002;70:6515–6517. doi: 10.1128/IAI.70.12.6515-6517.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock RE. Peptide antibiotics. Lancet. 1997;349:418–422. doi: 10.1016/S0140-6736(97)80051-7. [DOI] [PubMed] [Google Scholar]
- Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF) Trends Biotechnol. 2009;27:158–167. doi: 10.1016/j.tibtech.2008.11.009. [DOI] [PubMed] [Google Scholar]
- Kalen A, Wahlstrom O, Linder CH, Magnusson P. The content of bone morphogenetic proteins in platelets varies greatly between different platelet donors. Biochem. Biophys. Res. Commun. 2008;375:261–264. doi: 10.1016/j.bbrc.2008.08.014. [DOI] [PubMed] [Google Scholar]
- Weibrich G, Kleis WK, Hafner G, Hitzler WE. Growth factor levels in platelet-rich plasma and correlations with donor age, sex, and platelet count. J. Craniomaxillofac. Surg. 2002;30:97–102. doi: 10.1054/jcms.2002.0285. [DOI] [PubMed] [Google Scholar]
- Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal. Evaluation of growth factor availability for tissues through four PRP-gel preparations: Fibrinet, RegenPRP-Kit, Plateltex and one manual procedure. Vox Sang. 2009;97:110–118. doi: 10.1111/j.1423-0410.2009.01188.x. [DOI] [PubMed] [Google Scholar]
- Lei H, Gui L, Xiao R. The effect of anticoagulants on the quality and biological efficacy of platelet-rich plasma. Clin. Biochem. 2009;42:1452–1460. doi: 10.1016/j.clinbiochem.2009.06.012. [DOI] [PubMed] [Google Scholar]
- Redler LH, Thompson SA, Hsu SH, Ahmad CS, Levine WN. Platelet-rich plasma therapy: a systematic literature review and evidence for clinical use. Phys. Sportsmed. 2011;39:42–51. doi: 10.3810/psm.2011.02.1861. [DOI] [PubMed] [Google Scholar]
- Whitman DH, Berry RL, Green DM. Platelet gel: an autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 1997;55:1294–1299. doi: 10.1016/s0278-2391(97)90187-7. [DOI] [PubMed] [Google Scholar]
- Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int. J. Oral Maxillofac. Implants. 1999;14:529–535. [PubMed] [Google Scholar]
- Whitman DH, Berry RL. A technique for improving the handling of particulate cancellous bone and marrow grafts using platelet gel. J. Oral. Maxillofac. Surg. 1998;56:1217–1218. doi: 10.1016/s0278-2391(98)90776-5. [DOI] [PubMed] [Google Scholar]
- Currie LJ, Sharpe JR, Martin R. The use of fibrin glue in skin grafts and tissue-engineered skin replacements: a review. Plast. Reconstr. Surg. 2001;108:1713–1726. doi: 10.1097/00006534-200111000-00045. [DOI] [PubMed] [Google Scholar]
- Nikulin AA. Effect of calcium, thrombin and nucleotides (ADP, cAMP, cGMP) on blood platelet glycolysis and energy metabolism. Farmakol. Toksikol. 1980;43:585–590. [PubMed] [Google Scholar]
- Hantgan RR, Taylor RG, Lewis JC. Platelets interact with fibrin only after activation. Blood. 1985;65:1299–1311. [PubMed] [Google Scholar]
- Hantgan R, Fowler W, Erickson H, Hermans J. Fibrin assembly: a comparison of electron microscopic and light scattering results. Thromb. Haemost. 1980;44:119–124. [PubMed] [Google Scholar]
- Li B, Jiang B, Boyce BM, Lindsey BA. Multilayer polypeptide nanoscale coatings incorporating IL-12 for the prevention of biomedical device-associated infections. Biomaterials. 2009;30:2552–2558. doi: 10.1016/j.biomaterials.2009.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B, Jiang B, Dietz MJ, Smith ES, Clovis NB, Rao KMK. Evaluation of local MCP-1 and IL-12 nanocoatings for infection prevention in open fractures. J. Orthop. Res. 2010;28:48–54. doi: 10.1002/jor.20939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce BM, Lindsey BA, Clovis NB, Smith ES, Hobbs GR, Hubbard DF, Emery SE, Barnett JB, Li B. Additive effects of exogenous IL-12 supplementation and antibiotic treatment in infection prophylaxis. J. Orthop. Res. 2012;30(2):196–202. doi: 10.1002/jor.21520. [DOI] [PMC free article] [PubMed] [Google Scholar]


