Abstract
This study examined sex differences in alcohol-associated smoking urge and smoking patterns to elucidate factors contributing to the co-use of alcohol and cigarettes. Participants were 39 (22M, 17F) binge-drinking tobacco chippers. Although men and women showed similar alcohol-smoking patterns and similar alcohol-induced smoking urges, a positive association between these factors was observed only in men. The lack of relationship in women suggests that co-use of these substances may be due to exteroceptive factors beyond the pharmacological effects of alcohol potentiating smoking urge.
INTRODUCTION
There is a strong positive association between cigarette smoking and alcohol use. In human laboratory studies, acute alcohol consumption (compared with placebo) has been shown to increase cigarette smoking behavior.1–7 Alcohol has also been shown to increase smoking urge in the context of cues or cigarette smoking6,8–10 as well as in the absence of smoking cues or cigarette availability.11,12 Alcohol-related increases in smoking urge have been found to be partially mediated by the positive stimulating effects that are prominent just after alcohol consumption,11 as alcohol may enhance the rewarding effects of nicotine.13
Tobacco and alcohol consumption may carry serious health risks for women.14,15 However, whereas some lab studies have included mixed subject samples of men and women,8,10,12 very few have examined potential sex differences in alcohol-related smoking urges and behaviors. Only one study has specifically examined alcohol-induced smoking behaviors in women, and no studies to date have examined women’s alcohol-induced smoking urges under controlled conditions. Mello and colleagues5 found that when female heavy smokers had access to both cigarettes and alcohol in a lab setting, they showed increases in smoking behavior. These results support alcohol-cigarette use interactions similar to that previously observed in men.1,2,4,6 However, laboratory studies have found inconsistent results regarding sex differences in nicotine-alcohol interactions. In one study, the combination of nicotine via nasal spray and alcohol produced heightened subjective effects (both positive and negative) in women but not in men.16 In another investigation examining the converse relationship (i.e. nicotine’s effects on alcohol response), increasing doses of nicotine patch augmented the number of alcoholic drinks chosen in men but not in women.17 Therefore, it is unclear if women are more or less sensitive to alcohol-smoking effects compared with men.
Perkins18 has postulated that women’s smoking may relate more to exteroceptive features (handling, social, context, emotional, and situational aspects), whereas men’s smoking may relate more to direct CNS-mediated effects of nicotine. Evidence for this hypothesis derives from studies indicating that female smokers are less successful in discriminating nicotine via nasal spray18 and less confident in their discrimination responses compared with male smokers.19 Further, the positive rewarding effects of women’s smoking response may vary based on instructional set (revealing the nicotine content of cigarettes), whereas such information has no effect on subjective smoking responses in men.20 Although there is still debate,21 in general, women show worse smoking cessation outcomes than men, especially with nicotine replacement or minimal intervention counseling.22 Taken together, these laboratory and clinical findings indicate that there may be factors beyond the pharmacological effects of nicotine that play an important role in sustaining women’s smoking behavior. It remains to be determined whether sex differences in smoking response may extend to alcohol’s effects on smoking response in persons who habitually co-use these substances.
The majority of human laboratory studies on alcohol-nicotine interactions have focused on smokers who are regular habitual users. Therefore, less is known about these interactions in nondependent smokers or “tobacco chippers,” despite findings that alcohol is the most common environmental cue for smoking in tobacco chippers.23 Tobacco chippers are persons who smoke on occasion or at low levels without developing physical dependence or other signs of addiction, such as withdrawal symptoms.24–27 Light, occasional smoking patterns are more prevalent among younger than older smokers and appear to occur equally in men and women.28,29 It is unclear whether alcohol’s potentiation of smoking in chippers is the result of a paired behavior (i.e. due to situational and social cues30) or a direct neurobiological mechanism, or both.
The goals of this study were to compare men and women non-alcohol-dependent tobacco chippers on daily alcohol and smoking patterns, alcohol’s effects on smoking urges in the laboratory, and the relationship between these variables. Given the greater preponderance of binge drinking in young men than women,31 male heavy social drinkers may be more frequently exposed to the pairing of alcohol and nicotine. Therefore, it was hypothesized that men, compared with women, would report more frequent excessive drinking and concomitant drinking-smoking episodes and would have a stronger relationship between alcohol-related smoking behavior and urges.
METHODS
Participants
The sample included 39 heavy social drinkers with concomitant light, non-dependent smoking patterns. These participants were enrolled in the larger Chicago Social Drinking Project, which examined subjective, objective, and physiological responses to alcohol in a range of social drinkers. The majority of participants have been described in recent papers from this project.11,32,33
Study candidates were recruited using the Internet, flyers, and word-of-mouth referrals, with the goal of enrolling an equal proportion of men and women for the purpose of examining sex differences. Inclusion criteria included age between 21–35, body mass index between 19–30, and no major current medical or psychiatric conditions. In addition, candidates must have met criteria for heavy social binge drinking consistent with our past studies34 with weekly alcohol consumption of 10–45 alcohol drinks per week and regular weekly binge episodes (i.e. 5+ drinks/occasion for men; 4+ drinks/occasion for women) one to five times per week for at least the last two years. To meet criteria as a tobacco chipper, candidates must have smoked an average of 1 to 5 cigarettes at least two days per week for a minimum of one year. Up to 15 cigarettes were allowed during binge drinking occasions, consistent with our prior studies.11,12
After telephone screening, candidates underwent an in-laboratory screening, where they signed informed consent and underwent a physical examination, blood and urine tests, a diagnostic interview, and several psychosocial and health history questionnaires. Participants were excluded if they were taking any psychotropic medications, had a major medical or psychiatric condition (including past or current alcohol or substance dependence), or had a positive urine toxicology screen (morphine, cocaine, methamphetamine, barbiturates, or benzodiazepines). Persons with alcohol and/or nicotine dependence were excluded to avoid potential withdrawal during the sessions. Women were excluded if they were pregnant or breastfeeding.
PROCEDURE
Each participant arrived between 3 pm and 5 pm for their three laboratory sessions. Sessions were conducted in comfortable, living room-like testing rooms in the Clinical Addictions Research Laboratory. In random session order, the participant consumed a beverage containing either high dose alcohol (0.8 g/kg; 16% volume alcohol), low dose alcohol (0.4 g/kg; 8% volume alcohol), or placebo (1% volume ethanol as a taste mask). To reduce alcohol expectancies,35 the participant was informed that the beverages might contain a stimulant, sedative, alcohol, placebo, or a combination of two substances. The drinks were prepared with Kool-Aid, water, Splenda®, and the appropriate dose of 190-proof ethanol based on body weight. Adjustments were made for women to receive an approximate 85 percent dose as compared with men due to potential differences in total body water affecting blood alcohol concentrations.36,37 Sessions were separated by at least 48 hours.
Each participant was asked to abstain from alcohol and recreational drugs 48 hours before each session, as well as caffeine, food, and cigarettes three hours before each session. Upon arrival, to assess compliance with these restrictions, participants were interviewed and provided objective verification via breath tests for carbon monoxide (Smokerlyzer®, Bedfont Scientific, Medford, New Jersey, USA) and breath alcohol content (BAC; Alco-Sensor III, Intoximeter, St. Louis, Missouri, USA), as well as a random urine toxicology screen. This was followed by consumption of a low-fat snack (20% daily calories) to help reduce the potential for alcohol-induced nausea and avoid hunger effects on mood state. Thirty minutes post-arrival, the participant completed baseline questionnaires, and then was instructed to consume the allocated beverage over a 15-minute interval in the presence of the research assistant. The beverages were served in plastic cups with a lid and straw in order to help conceal the scent and identification of the alcohol content. At set intervals after the completion of the drink (15, 45, 105, and 165 minutes), the participant completed study measures and breathalyzer readings. The second and third sessions were identical to the first session with the exception of beverage alcohol content. At the end of each session, a questionnaire was administered to ask the participant if s/he believed the beverage contained alcohol, a stimulant, a sedative, or a placebo. This was followed by transportation to home provided by a livery service. At the end of the study, each participant was debriefed and compensated $200. The study was fully approved by the University of Chicago Institutional Review Board.
MEASURES
Participants’ daily pattern of alcohol and smoking behavior was assessed at screening using a Timeline Follow-Back interview (TLFB38,39). The TLFB is a reliable and valid calendar interview method of obtaining daily estimates of alcohol and smoking patterns over the previous 28-day period. The dependent measures from TLFB included the daily number of reported cigarettes and alcoholic drinks consumed (one drink = 12 oz. beer, 5 oz. wine, or 1.5 oz. liquor). For statistical analyses, to control for sex differences in body water that may impact BAC, each subject’s daily number of drinks was divided by their estimated body water, based on the formula by Watson, Watson, and Batt.40 Because these behaviors were anticipated to fluctuate from weekdays to weekends, only data from the four full weeks (Monday to Sunday) prior to screening were used for analyses. Change scores were also computed to determine alcohol-related cigarette use patterns by subtracting the average number of cigarettes smoked on all non-drinking days from the average number of cigarettes smoked on all heavy drinking days (5+ drinks/day; 4+ for women).
Smoking in urges the laboratory sessions were assessed by the Brief Questionnaire of Smoking Urges (BQSU), a reliable and valid measure of urge to smoke and especially suited for short-term laboratory assessment.41 The BQSU consists of 10 smoking-urge related statements scored on a Likert scale from 1 (strongly disagree) to 7 (strongly agree), with higher scores indicating stronger smoking urges. The BQSU includes two sub factors. Factor 1, which measures urge to smoke for pleasure and stimulation, was the primary outcome measure, and Factor 2, which measures urge to smoke to relieve negative affect and withdrawal, was the secondary measure. This was based on our prior research showing marked increases in Factor 1 scores in chippers after alcohol drinking but only modest increases in Factor 2.12 Change scores were computed by subtracting the baseline value from each time point. A summary measure of alcohol’s increase in smoking urge was also computed: the change score at 45 minutes in the placebo session was subtracted from the change score at 45 minutes in the high alcohol dose session.
BACs during the experimental procedure were measured by the Alco-Sensor IV breathalyzer (Intoximeter, St. Louis, Missouri, USA). The device’s monitor was blinded to read 0.000 throughout the session, with actual values downloaded later.
Statistical Analyses for Primary Measures
Men and women were compared on background characteristics via t-tests and chi-square tests, where appropriate, and on BACs via a repeated measures analysis of variance (ANOVA). The TLFB data was analyzed for cigarette consumption by a two-way ANOVA with sex as the between-subjects factor and drinking day type (no, light, or heavy drinking) as the within-subjects factor. The TLFB data was further examined with a mixed linear model, with daily cigarette use as the outcome, and daily alcohol use, sex, week number, day of the week, and related interactions as the independent variables. As this initial analysis showed no difference in alcohol and smoking patterns by week (i.e. no main effect of week and no interactions with other variables), the mixed linear model was simplified, combining the days in the week to create average consumption scores for each day. A first-order autoregressive correlation structure was used to account for correlations among these measures over time. Smoking urges after alcohol consumption in the laboratory were analyzed by a three-way repeated measures analysis of variance (ANOVA) with sex as the between-subjects variable and dose and time as the within subjects variables. The p values of repeated factors (dose and time) were adjusted by the Greenhouse-Geisser method. A moderation analysis42 examined the role of sex in the relationship between alcohol-associated smoking behaviors from the TLFB and alcohol-induced smoking urge in the lab (using the summary change scores for both measures). A robust standard error estimation method was used in the moderation analysis to relax the homogeneity of variance assumption in linear regression.
RESULTS
Participant Characteristics
Forty-one subjects were initially enrolled. However, two subjects failed to complete all sessions due to positive random urine drug test results prior to a laboratory session (i.e. a protocol violation). Therefore, the final sample size was made up of 17 women and 22 men. The sexes were similar on general characteristics (except for weight and body water), as well as on their background smoking and drinking histories (see Table 1).
TABLE 1.
Background characteristics in women and men
| Women | Men | |
|---|---|---|
| General characteristics | (n = 17) | (n = 22) |
| Age (years) | 25.1 (0.7) | 24.8 (0.7) |
| Education (years) | 15.8 (0.2) | 15.8 (0.4) |
| Race (% Caucasian) | 14/17 (82.4%) | 18/22 (81.8%) |
| Weight (pounds) | 142.2 (5.2) | 186.4 (3.8)* |
| BMI (kg/m2) | 23.4 (0.7) | 25.9 (0.5)† |
| Body water estimates | 31.6 (0.6) | 47.9 (0.6)* |
| Smoking behavior | ||
| Smoking days/week | 3.4 (0.4) | 3.7 (0.5) |
| Average number of cigarettes/day |
5.4 (0.6) | 4.8 (0.6) |
| Total cigarettes/week | 22.6 (4.3) | 22.0 (4.0) |
| Smoking duration (years) | 7.0 (0.8) | 5.9 (0.8) |
| FTND score (0–10 range) | 0.2 (0.1) | 0.6 (0.2) |
| Drinking behavior§ | ||
| Drinking days/week | 3.0 (0.3) | 3.6 (0.2) |
| Average number of alcohol drinks/occasion |
5.3 (0.5) | 6.2 (0.7) |
| Total drinks/week | 16.2 (2.0) | 22.1 (2.5) |
| Average number of binges∥ per month |
10.1 (1.2) | 9.9 (0.9) |
| Lifetime alcohol abuse | 8/17 (47.1%) | 10/22 (45.4%) |
Note. Data are mean (±SEM) or ratio (%).
p < .001
p = .05. Body water estimates based on Watson et al. (1980)40: [male body water = 2.447 – 0.09516 (age years) + 0.1074 (height cm) +0.3362 (weight kg); female body water = −2.097 + 0.1069 (height cm) +0.2466 (weight kg)]
Data presented are raw data obtained from a TLFB interview; analyses covaried for body water.
Binge = 5+ drinks/occasion for men, 4+ for women.
TLFB
Table 2 depicts the average number of cigarettes consumed by drinking day type. Cigarette smoking was significantly greater on binge drinking days compared with both light- and non-alcohol drinking days [F(2,74) = 45.77, p < 0.0001; Tukey’s HSD: binge > light = non drinking day]. Confirming that drinking behaviors varied by these drinking day types, the average number of drinks consumed on light drinking days was 2.4 ± 0.2 and for binge drinking days 7.0 ± 0.3. Taking into account body water differences, men and women were similar on these patterns. In terms of use patterns over time from the TLFB, daily fluctuations in alcohol drinking were significantly correlated with daily fluctuations in cigarette smoking [F(1, 208) = 103.9, p < 0.001; see Figure 1], and both were consumed at significantly higher levels on weekends (Friday and Saturday) compared with other days of the week (Sunday, Monday, Tuesday, Wednesday) [cigarettes: F(6, 266) = 10.91, p < 0.001, Tukey’s HSD: (Fri = Sat) > (all other days); alcohol: F(6, 266) = 33.99, p < 0.001, Tukey’s HSD: (Friday = Saturday) > Thursday > (Sunday = Monday = Tuesday = Wednesday)]. Average and daily fluctuations in smoking and drinking behaviors did not differ between the sexes (main effect of sex, p = 0.13, sex × drinking, p = 0.45, sex × drinking × day, p = .37; see Figure 1).
TABLE 2.
TLFB summary by drinking day type and smoking urge in laboratory
| Smoking behavior (TLFB): | Women | Men |
|---|---|---|
| Average number of Cigarettes | (n = 17) | (n = 22) |
| No alcohol drinking day | 0.78 (0.37) | 1.71 (0.52) |
| Light drinking day | 2.39 (0.68) | 2.20 (0.48) |
| Binge drinking day | 6.19 (0.87) | 5.68 (0.91) |
| Smoking urge (BQSU): | ||
| Factor 1 scores Baseline |
9.82 (1.33) | 13.11 (1.76) |
| Placebo | ||
| +15 min. | 10.47 (1.84) | 13.55 (1.97) |
| +45 min. | 10.41 (1.71) | 13.59 (1.88) |
| +105 min. | 10.24 (1.69) | 13.55 (1.92) |
| +165 min. | 11.00 (1.89) | 14.73 (2.09) |
| Low alcohol dose | ||
| +15 min. | 15.00 (1.96) | 17.55 (2.33) |
| +45 min. | 14.12 (2.04) | 17.41 (2.27) |
| +105 min. | 12.29 (1.75) | 17.00 (2.32) |
| +165 min. | 11.94 (1.89) | 16.59 (2.42) |
| High alcohol dose | ||
| +15 min. | 19.35 (2.17) | 21.64 (2.43) |
| +45 min. | 19.53 (2.13) | 21.27 (2.69) |
| +105 min. | 16.71 (2.04) | 19.23 (2.49) |
| +165 min. | 15.88 (1.71) | 18.05 (2.47) |
Note. Data are mean (±SEM).
Smoking behavior: No alcohol drinking day = days in which no alcohol consumption reported; light drinking day = days in which 1–4 drinks reported for men, 1–3 for women; binge drinking day = days in which five or more drinks reported for men, four or more for women.
Smoking urge: Baseline = average value for all three laboratory baseline sessions; BQSU scores depicted are for Factor 1 only for ease of presentation. +15, +45, +105, +165 min. = time since completion of the respective beverage.
FIGURE 1.
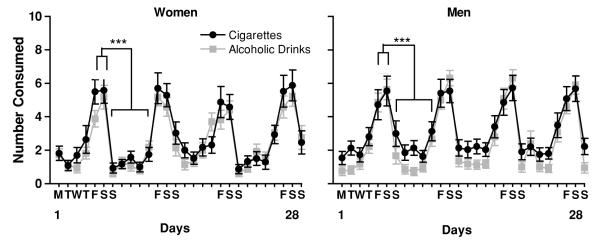
Timeline Follow-Back derived daily patterns for alcohol and cigarette use over the last month in women and men. MTWTFSS = Monday though Sunday; for ease of presentation, only the label FSS (i.e. Friday, Saturday, and Sunday) is repeated for the second, third, and fourth weeks, with tick marks included to represent the other days. ***p < .001, for cigarettes: Friday and Saturday > other days of the week; for alcohol: Friday and Saturday > Thursday > other days of the week.
Blood Alcohol Concentrations
After alcohol consumption, as expected, BAC levels increased sharply during the first 45 minutes to peak, and then slowly decreased over time during the alcohol elimination phase [dose × time: F(4, 337) = 6.21, p = 0.001). Men and women did not differ on BAC levels at either dose or across time (ps > 0.38). Across post-drinking time points (i.e. 15, 45, 105, and 165 minutes after beverage completion), average BACs during the low dose session were 0.040, 0.036, 0.019, and 0.004, and during the high dose session were 0.083, 0.092, 0.074, and 0.057, respectively. There was a dose-dependent relationship in terms of beverage content estimates: at the end of the placebo beverage session, 5% of subjects believed they received alcohol and 31% believed they received either a sedative or stimulant; at low dose alcohol, 46% believed they received alcohol and 15% believed they received either a sedative or stimulant; and at high dose alcohol, 82% believed they received alcohol and 18% believed they received either a sedative or stimulant. Men and women did not differ in their estimations of beverage content.
Brief Questionnaire of Smoking Urges
Alcohol dose-dependently increased BQSU Factor 1 scores, and these increases in smoking urges were most pronounced during the first 45 min after alcohol consumption of the BAC [dose × time: F(6,407) = 2.39, p < 0.05; see Table 2]. Men and women did not differ on baseline BQSU Factor 1 scores [t(37) = 0.98, p ≥ .06]. The main effect of sex and interactions of both sex × dose and sex × dose × time were all non significant, indicating that the sexes did not differ on reported smoking urges in the laboratory after alcohol consumption. Separate analyses for BQSU Factor 2 also showed a similar pattern of alcohol-induced increases in smoking urge, with no sex differences across dose or time.
Relationship between Alcohol-Induced Smoking Behaviors and Urges
A moderation analysis with robust standard error estimation indicated that the relationship between alcohol-associated smoking behavior from the TLFB and alcohol-induced smoking urges from the laboratory differed between sexes [sex × smoking response: beta(se) = 1.66(0.51), p = 0.002, see Figure 2]. For men, there was a positive relationship between alcohol-associated smoking behavior and alcohol’s increases in smoking urge (BQSU Factor 1), whereas there was no association between these measures in women. A secondary analysis examining BQSU Factor 2 showed a similar moderation effect of sex [sex × smoking response: beta(se) = 1.19(0.42), p = 0.008], with a positive alcohol-related smoking behavior and urge relationship in men but not in women.
FIGURE 2.
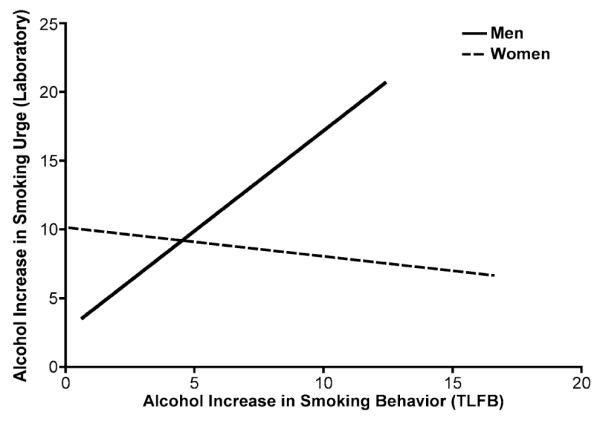
The fitted regression lines between alcohol-associated increases in smoking behavior (TLFB) and alcohol increases in smoking urge (BQSU Factor 1) for men and women. Sex moderated the relationship between alcohol induced smoking behavior and alcohol induced urge (p = 0.002). Result for BQSU Factor 2 was similar (not depicted for ease of presentation).
DISCUSSION
The results of the current study indicate that men and women nondependent drinker-smokers reported similar weekly fluctuations in alcohol drinking and cigarette smoking. The lowest frequency for both sexes occurred on Mondays, Tuesdays, and Wednesdays, and the highest frequency occurred on Fridays and Saturdays, with Thursdays intermediate for alcohol drinking. Further, in the laboratory portion of the study, alcohol consumption increased smoking urges similarly in men and women. Smoking urge increases after drinking were especially pronounced for both sexes during the rising limb of the BAC. Interestingly, when alcohol-related smoking behaviors in the natural setting were linked to alcohol-induced smoking urges in the laboratory, a positive relationship was found only in men, and not in women.
Despite decades of lower smoking prevalence in women compared with men, statistics show that over the last twenty years this difference between the sexes may be closing, particularly in young samples.43 Similarly, whereas binge drinking rates in men have remained relatively constant over the past few decades, rates in women have been increasing, although they still remain at a lower rate than men (i.e., 49% in men versus 41% in women).31 Contrary to our prediction that men would show more frequent pairings of heavy drinking and smoking, these patterns were similar between the sexes. This may be due to several factors, including recruiting a homogenous sample of nondependent heavy alcohol drinking tobacco chippers, as well as controlling for body water differences between the sexes, which may affect blood alcohol concentrations (i.e. at the same dose of alcohol, women have greater blood alcohol concentrations than men). While general population statistics show that men binge drink more than women and are at higher risk for the development of alcohol dependence, in the current sample of social drinker-smokers, use patterns for these substances were markedly similar throughout the week for both men and women. Studies examining future patterns of alcohol and cigarette behaviors over time in identified early nondependent users may further elucidate the effect of sex on cessation, continued habitual use, or exacerbations and development of dependence on one or both substances.
Further, in the well-controlled laboratory environment where many exteroceptive factors are ostensibly minimized (social setting, affective cues, etc.), men and women exhibited similar alcohol-induced increases in smoking urge. This result indicates that for both sexes, there may be robust pharmacological effects of alcohol that increase smoking urge, potentially due to alcohol interacting with brain nicotinic receptors,44 and ultimate activation of brain reward pathways and dopamine release.45 Because the lab environment did not allow for cigarette smoking, it is unclear whether the reported increases in smoking urge would have resulted in differential smoking behaviors between the sexes; such studies are currently underway in our laboratory.46
Supporting our hypothesis, in men compared with women, there was a stronger link between alcohol-smoking behavior from TLFB and alcohol-induced smoking urges in the laboratory. This finding supports and extends prior research showing that men (versus women) may smoke primarily due to the direct effects of nicotine,47 show better smoking cessation outcomes with nicotine replacement,48–52 and increase their alcohol choice behavior after nicotine administration.17 We may speculate that, in women, alcohol potentiation of cigarette smoking may be due to the combined influence of direct nicotine effects and associated features of smoking (smoking cues, environment, emotions, appearance, etc.). Although a direct test of such hypotheses is beyond the scope of this pilot study, future research is warranted to further clarify women’s and men’s co-occurring alcohol and smoking behaviors.
While there were several strengths in the current study, including an a priori design of examining sex differences and employing well-controlled measures, there are a few caveats worth mentioning. First, the study examined only non-nicotine dependent smokers, and it remains to be determined whether the sex differences observed in this study extend to heavier smokers. It is possible that nicotine-dependent women may exhibit different alcohol-smoking interactions than less-smoking women. Second, the study examined smoking behavior and urges using two different modalities: the TLFB, through which the reciprocal relationship between alcohol and cigarette consumption cannot be observed in real-time, and the BQSU, which was obtained during a laboratory assessment. Whereas incorporating measurement of both smoking behaviors and urges within the same modality would be highly desirable, it would also be complicated by the fact that acute cigarette smoking decreases smoking urge,53 which would confound assessment in the naturalistic setting. Third, in terms of methodology, while an advantage of the laboratory setting is the minimization of potential extraneous cues, one disadvantage is that the data may not generalize to a naturalistic drinking-smoking episode that likely consists of alcohol consumption over a longer duration with likely fluctuations in smoking urges and cigarette use, partially dependent on availability, monetary issues, and social setting factors
In sum, the results show that nondependent drinker-smoker men and women report similar fluctuations in drinking and smoking and exhibit similar alcohol-induced increases in smoking urge (in the absence of smoking). For men, alcohol’s potentiation of cigarette smoking may be more directly related to increases in smoking urges, but for women, more complex factors may be involved. Future studies are underway in our group to examine the sexes on the effects of alcohol versus placebo on smoking behaviors for nicotine versus non-nicotine factors to further elucidate aspects underlying concomitant use of these substances in young persons.
Acknowledgments
This research was supported by grants #F31-AA15017 (Dr. Epstein); and #R01-AA013746 and #R03-AA015337 (Dr. King) from the National Institute on Alcohol Abuse and Alcoholism, Bethesda, Md.; by a Cancer Center Grant #P30-CA14599 (Dr. King), Chicago, Ill.; and by a General Clinical Research Center Grant #M01-RR00055 (Dr. King), Chicago, Ill.
The authors would like to thank Dr. Royce Lee for performing medical screenings and for medical oversight of the study. The experiments in this study comply with the current U.S. laws and were in compliance with the Declaration of Helsinki for human subjects.
Footnotes
Work was performed at the Clinical Addictions Research Laboratory, University of Chicago.
REFERENCES
- 1.Griffiths RR, Bigelow GE, Liebson I. Facilitation of human tobacco self-administration by ethanol: A behavioral analysis. J Exp Anal Behav. 1976;25:279–292. doi: 10.1901/jeab.1976.25-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henningfield JE, Chait LD, Griffiths RR. Cigarette smoking and subjective response in alcoholics: Effects of pentobarbital. Clin Pharmacol Ther. 1983;33:806–812. doi: 10.1038/clpt.1983.110. [DOI] [PubMed] [Google Scholar]
- 3.Henningfield JE, Chait LD, Griffiths RR. Effects of ethanol on cigarette smoking by volunteers without histories of alcoholism. Psychopharmacology. 1984;82:1–5. doi: 10.1007/BF00426371. [DOI] [PubMed] [Google Scholar]
- 4.Mello NK, Mendelson JH, Sellers ML, Kuehnle JC. Effects of alcohol and marihuana on tobacco smoking. Clin Pharmacol Ther. 1980;27:202–209. doi: 10.1038/clpt.1980.32. [DOI] [PubMed] [Google Scholar]
- 5.Mello NK, Mendelson JH, Palmieri SL. Cigarette smoking by women: Interactions with alcohol use. Psychopharmacology. 1987;93:8–15. doi: 10.1007/BF02439579. [DOI] [PubMed] [Google Scholar]
- 6.Mintz J, Boyd G, Rose JE, Charuvastra VC, Jarvik ME. Alcohol increases cigarette smoking: A laboratory demonstration. Addict Behav. 1985;10:203–207. doi: 10.1016/0306-4603(85)90001-2. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell SH, de Wit H, Zacny JP. Effects of varying ethanol dose on cigarette consumption in healthy normal volunteers. Behav Pharmacol. 1995;6:359–365. [PubMed] [Google Scholar]
- 8.Burton SM, Tiffany ST. The effect of alcohol consumption on craving to smoke. Addiction. 1997;92:15–26. [PubMed] [Google Scholar]
- 9.Glautier S, Clements K, White JAW, Taylor C, Stolerman IP. Alcohol and the reward value of cigarette smoking. Behav Pharmacol. 1996;7:144–154. [PubMed] [Google Scholar]
- 10.Sayette MA, Martin CS, Wertz JM, Perrott MA, Peters AR. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychol Addict Behav. 2005;19:263–270. doi: 10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein AM, Sher TG, Young MA, King AC. Tobacco chippers show robust increases in smoking urge after alcohol consumption. Psychopharmacology. 2007;190:321–329. doi: 10.1007/s00213-006-0438-8. [DOI] [PubMed] [Google Scholar]
- 12.King AC, Epstein AM. Alcohol dose-dependent increases in smoking urge in light smokers. Alcohol Clin Exp Res. 2005;29:547–552. doi: 10.1097/01.alc.0000158839.65251.fe. [DOI] [PubMed] [Google Scholar]
- 13.Rose JE, Brauer LH, Behm FM, Cramblett M, Calkins K, Lawhon D. Psychopharmacological interactions between nicotine and ethanol. Nicotine Tob Res. 2004;6:133–144. doi: 10.1080/14622200310001656957. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention [Retrieved 7 September 2007];Fact Sheet: Women and Tobacco (updated November 2006) Available from: http://www.cdc.gov/tobacco/data_statistics/Factsheets/women_tobacco.htm.
- 15.U.S. Department of Health and Human Services . A Report of the Surgeon General. Government Printing Office; Washington, DC: 2001. Women and Smoking. 2001. [Google Scholar]
- 16.Perkins KA, Sexton JE, DiMarco A, Grobe J, Scierka A, Stiller RL. Subjective and cardiovascular responses to nicotine combined with alcohol in male and female smokers. Psychopharmacology. 1995;119:205–212. doi: 10.1007/BF02246162. [DOI] [PubMed] [Google Scholar]
- 17.Acheson A, Mahler SV, Chi H, de Wit H. Differential effects of nicotine on alcohol consumption in men and women. Psychopharmacology. 2006;186:54–63. doi: 10.1007/s00213-006-0338-y. [DOI] [PubMed] [Google Scholar]
- 18.Perkins KA. Individual variability in response to nicotine. Behav Genet. 1995;25:119–132. doi: 10.1007/BF02196922. [DOI] [PubMed] [Google Scholar]
- 19.Perkins KA, Sanders M, D’Amico D, Wilson A. Nicotine discrimination and self-administration as a function of smoking status. Psychopharmacology. 1997;131:361–370. doi: 10.1007/s002130050304. [DOI] [PubMed] [Google Scholar]
- 20.Perkins KA, Doyle T, Ciccocioppo M, Conklin C, Sayette M, Caggiula A. Sex differences in the influence of nicotine dose instructions on the reinforcing and self-reported rewarding effects of smoking. Psychopharmacology. 2006;184:600–607. doi: 10.1007/s00213-005-0103-7. [DOI] [PubMed] [Google Scholar]
- 21.Killen JD, Fortmann SP, Varady A, Kraemer HC. Do men outperform women in smoking cessation trials? Maybe, but not by much. Exp Clin Psychopharmacol. 2002;10:295–301. doi: 10.1037//1064-1297.10.3.295. [DOI] [PubMed] [Google Scholar]
- 22.Perkins KA. Smoking cessation in women: special considerations. CNS Drugs. 2001;15:391–411. doi: 10.2165/00023210-200115050-00005. [DOI] [PubMed] [Google Scholar]
- 23.Shiffman S, Fischer LA, Paty JA, Gnys M, Hickcox M, Kassel JD. Drinking and smoking: A field study of their association. Ann Behav Med. 1994;16:203–209. [Google Scholar]
- 24.Shiffman S. Tobacco “chippers”—individual differences in tobacco dependence. Psychopharmacology. 1989;97:539–547. doi: 10.1007/BF00439561. [DOI] [PubMed] [Google Scholar]
- 25.Shiffman S, Paty JA, Gnys M, Kassel JD, Elash C. Nicotine withdrawal in chippers and regular smokers: Subjective and cognitive effects. Health Psychol. 1995;14:301–309. doi: 10.1037//0278-6133.14.4.301. [DOI] [PubMed] [Google Scholar]
- 26.Shiffman S, Paty JA, Kassel JD, Gnys M, Zettler-Segal M. Smoking behavior and smoking history of tobacco chippers. Exp Clin Psychopharmacol. 1994;2:126–142. [Google Scholar]
- 27.Shiffman S, Zettler-Segal M, Kassal JD, Paty JA, Benowitz NL, O’Brien G. Nicotine elimination and tolerance in non-dependent cigarette smokers. Psychopharmacology. 1992;109:449–456. doi: 10.1007/BF02247722. [DOI] [PubMed] [Google Scholar]
- 28.Pleis JR, Lethbridge-Çejku M. Summary of health statistics for U.S. adults: National Health Interview Survey, 2005. National Center for Health Statistics; Atlanta, Ga: 2006. Vital Health Stat Series No. 10(232) [PubMed] [Google Scholar]
- 29.Wortley PM, Husten CG, Trosclair A, Chrismon J, Pederson LL. Nondaily smokers: A descriptive analysis. Nicotine Tob Res. 2003;5:755–759. doi: 10.1080/1462220031000158753. [DOI] [PubMed] [Google Scholar]
- 30.Shiffman S, Paty J. Smoking patterns and dependence: Contrasting chippers and heavy smokers. J Abnorm Psychol. 2006;115:509–523. doi: 10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- 31.Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. J Am Coll Health. 2004;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- 32.Brumback T, Cao D, King A. Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug Alcohol Depend. 2007;91:10–17. doi: 10.1016/j.drugalcdep.2007.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.King AC, Munisamy G, de Wit H, Lin S. Attenuated cortisol response to alcohol in heavy social drinkers. Int J Psychophysiol. 2006;59:203–209. doi: 10.1016/j.ijpsycho.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 34.King AC, Houle T, de Wit H, Holdstock L, Schuster A. Biphasic alcohol response differs in heavy versus light drinkers. Alcohol Clin Exp Res. 2002;26:827–835. [PubMed] [Google Scholar]
- 35.Martin CS, Sayette MA. Experimental design in alcohol administration research: Limitations and alternatives in the manipulation of dosage-set. J Stud Alcohol. 1993;54:750–761. doi: 10.15288/jsa.1993.54.750. [DOI] [PubMed] [Google Scholar]
- 36.Frezza M, di Padova C, Pozzato G, Terpin M, Baraona E, Lieber CS. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322:95–99. doi: 10.1056/NEJM199001113220205. [DOI] [PubMed] [Google Scholar]
- 37.Sutker PB, Tabakoff B, Goist KC, Randall CL. Acute alcohol intoxication, mood states and alcohol metabolism in women and men. Pharmacol Biochem Behavior. 1983;18(Suppl):349–354. doi: 10.1016/0091-3057(83)90198-3. [DOI] [PubMed] [Google Scholar]
- 38.Sobell LC, Sobell MB. Alcohol Timeline Follow-Back Users’ Manual. Addiction Research Foundation; Toronto, Canada: 1995. [Google Scholar]
- 39.Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behav Res Ther. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- 40.Watson PE, Watson ID, Batt RD. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am J Clin Med. 1980;33:27–39. doi: 10.1093/ajcn/33.1.27. [DOI] [PubMed] [Google Scholar]
- 41.Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine Tob Res. 2001;3:7–16. doi: 10.1080/14622200020032051. [DOI] [PubMed] [Google Scholar]
- 42.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 43.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Decline in daily smoking by younger teens has ended. University of Michigan News and Information Services; Ann Arbor, Mich.: [Accessed November 19, 2007]. Dec 21, 2006. Available at: http://www.monitoringthefuture.org.pressreleases/06cigpr.pdf. [Google Scholar]
- 44.Collins AC, Burch JB, de Fiebre CM, Marks MJ. Tolerance to and cross tolerance between ethanol and nicotine. Pharmacol Biochem Behav. 1988;29:365–373. doi: 10.1016/0091-3057(88)90170-0. [DOI] [PubMed] [Google Scholar]
- 45.Balogh SA, Owens JC, Butt CM, Wehner JM, Collins AC. Animal models as a tool for studying mechanisms of co-abuse of alcohol and tobacco. Alcohol Clin Exp Res. 2002;26:1911–1914. doi: 10.1097/01.ALC.0000040847.98115.6D. [DOI] [PubMed] [Google Scholar]
- 46.McNamara PJ, Conrad MF, Cao D, King AC. Sex differences in alcohol-induced increases in smoking topography for nicotinized and denicotinized cigarettes. Paper presented at: the Annual Scientific Sessions of the Society for Research on Nicotine and Tobacco; Portland, Oregon. Feb, 2008. [Google Scholar]
- 47.Perkins KA. Sex differences in nicotine versus nonnicotine reinforcement as determinants of tobacco smoking. Exp Clin Psychopharmacol. 1996;4:166–177. [Google Scholar]
- 48.Davis LJ, Hurt RD, Offord KP, Lauger GG, Morse RM, Bruce BK. Self-administered nicotine-dependence scale (SANDS): Item selection, reliability estimation, and initial validation. J Clin Psychol. 1994;50:918–930. doi: 10.1002/1097-4679(199411)50:6<918::aid-jclp2270500617>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 49.Killen JD, Fortmann SP, Newman B, Varady A. Evaluation of a treatment approach combining nicotine gum with self-guided behavioral treatments for smoking relapse prevention. J Consult Clin Psychol. 1990;58:85–92. doi: 10.1037//0022-006x.58.1.85. [DOI] [PubMed] [Google Scholar]
- 50.King AC, de Wit H, Riley RC, Cao D, Niaura R, Hatsukami D. Efficacy of naltrexone in smoking cessation: A preliminary study and an examination of sex differences. Nicotine Tob Res. 2006;8:671–682. doi: 10.1080/14622200600789767. [DOI] [PubMed] [Google Scholar]
- 51.Nides MA, Rakos RF, Gonzales D, et al. Predictors of initial smoking cessation and relapse through the first two years of the Lung Health Study. J Consult Clin Psychol. 1995;63:60–69. doi: 10.1037//0022-006x.63.1.60. [DOI] [PubMed] [Google Scholar]
- 52.Swan GE, Jack LM, Ward MM. Subgroups of smoker with different success rates after use of transdermal nicotine. Addiction. 1997;92:207–217. [PubMed] [Google Scholar]
- 53.King AC, Meyer PJ. Naltrexone alteration of acute smoking response in nicotine-dependent subjects. Pharmacol Biochem Behav. 2000;66:563–572. doi: 10.1016/s0091-3057(00)00258-6. [DOI] [PubMed] [Google Scholar]


