Abstract
It is suggested that the internal thoracic artery (ITA) harvesting technique influences the incidence of sternal wound infection (SWI) after coronary artery bypass graft (CABG). To determine if there is any real difference between skeletonized vs pedicled ITA, we performed a meta-analysis to determine if there is any real difference between these two established techniques in terms of SWI. We performed a systematic review using MEDLINE, EMBASE, CENTRAL/CCTR, SciELO, LILACS, Google Scholar and reference lists of relevant articles to search for studies that compared the incidence of SWI after CABG between skeletonized vs pedicled ITA until June 2012. The principal summary measures were odds ratio (OR) with 95% confidence interval (CI) and P values (statistically significant when <0.05). The ORs were combined across studies using the weighted DerSimonian–Laird random effects model and weighted Mantel–Haenszel fixed effects. Meta-analysis, sensitivity analysis and meta-regression were completed using the software Comprehensive Meta-Analysis version 2 (Biostat, Inc., Englewood, NJ, USA). Twenty-two studies involving 4817 patients (2424 skeletonized; 2393 pedicled) met the eligibility criteria. There was no evidence for important heterogeneity of effects among the studies. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.443, 95% CI 0.323–0.608, P < 0.001; random effect model: OR 0.443, 95% CI 0.323–0.608, P < 0.001). In the sensitivity analysis, the difference in favour of skeletonized ITA was also observed in subgroups such as diabetic, bilateral ITA and diabetic with bilateral ITA; we also observed that there was a difference in the type of study, since non-randomized studies together demonstrated the benefit of skeletonized ITA in comparison with pedicled ITA, but the randomized studies together did not show this difference (although close to statistical significance and with the tendency to favour the skeletonized group). In meta-regression, we observed a statistically significant coefficient for SWI and proportion of diabetic patients (coefficient −0.02, 95% CI −0.03 to −0.01, P = 0.016). In conclusion, skeletonized ITA appears to reduce the incidence of postoperative SWI in comparison with pedicled ITA after CABG, with this effect being modulated by the presence of diabetes.
Keywords: Meta-analysis, Coronary artery bypass, Mammary arteries, Surgical wound infection
INTRODUCTION
Rationale
Sternal wound infection (SWI) is a recognized and important complication of coronary artery bypass graft (CABG) surgery [1]. The most serious manifestation of an SWI is mediastinitis, which extends the previous anatomical classification to the risk of sepsis. It is well known that an infection of the mediastinum can be severe and potentially lethal [2].
It is suggested that the method of internal thoracic artery (ITA) harvesting influences the incidence of postoperative SWI [3–5]. There are two established harvesting techniques: pedicled and skeletonized ITAs. Whereas the pedicled technique dissects the artery away from the sternum with its accompanying veins, fascia, adipose tissue and lymphatics, generating a pedicled graft, skeletonization requires the ITA to be dissected free of all surrounding tissue, solely yielding the artery [3].
Our meta-analysis attempts to determine if there is any real difference between skeletonized and pedicled ITA in terms of SWI.
Objectives
We performed a meta-analysis and meta-regression of studies to compare skeletonized vs pedicled ITA during CABG, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [6].
METHODS
Eligibility criteria
Using the PICOS (Population, Intervention, Comparison, Outcome, Study design) strategy, studies were considered if: (i) the population comprised patients undergoing CABG; (ii) they compared outcomes between skeletonized vs pedicled ITA; (iii) outcomes studied included any situations considered as SWI—superficial, deep and/or mediastinitis; (iv) they were prospective or retrospective or non-randomized studies or randomized controlled trials.
Information sources
The following databases were used (until June 2012): MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL/CCTR), ClinicalTrials.gov, Scientific Electronic Library Online (SciELO), Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS)—The Latin American and Caribbean Health Sciences), Google Scholar and reference lists of relevant articles.
Search
We conducted the search using Medical Subject Heading (MeSH) terms (‘skeletonized’ OR ‘skeletonization’) AND (‘pedicled’ OR ‘pedunculated’ OR ‘in situ’) AND (‘arteries, mammary’ OR ‘artery, mammary’ OR ‘mammary artery’ OR ‘internal mammary artery’ OR ‘arteries, internal mammary’ OR ‘artery, internal mammary’ OR ‘internal mammary arteries’ OR ‘mammary arteries’ OR ‘mammary arteries, internal’ OR ‘mammary artery, internal’ OR ‘internal thoracic artery’ OR ‘arteries, internal thoracic’ OR ‘artery, internal thoracic’ OR ‘internal thoracic arteries’ OR ‘thoracic arteries, internal’ OR ‘thoracic artery, internal’) AND (‘coronary artery bypass graft’ OR ‘coronary artery bypass grafting’ OR ‘coronary artery bypass surgery’ OR ‘coronary bypass surgery’ OR ‘coronary artery bypass graft surgery’ OR ‘coronary artery bypass’ OR ‘coronary bypass’).
Study selection
The following steps were done: (i) identification of titles of records through searching of databases; (ii) removal of duplicates; (iii) screening and selection of abstracts; (iv) assessment for eligibility through full-text articles and (v) final inclusion in the study.
One reviewer followed steps 1–3. Two independent reviewers followed step 4 and selected studies. Inclusion or exclusion of studies was decided unanimously. When there was disagreement, a third reviewer took the final decision.
Data items
The endpoints were odds ratio (OR) for SWI after CABG using skeletonized vs pedicled ITA.
Data collection process
Two independent reviewers extracted the data. When there was disagreement about data, a third reviewer (the first author) checked the data and took the final decision about it. From each study, we extracted patient characteristics, study design and outcomes (number of events and number of total groups).
Risk of bias in individual studies
Included studies were assessed for the following characteristics: (i) sequence generation; (ii) allocation concealment; (iii) blinding; (iv) incomplete outcome data; (v) selective outcome reporting and (6) other sources of bias. Taking these characteristics into account, the papers were classified into A (low risk of bias), B (moderate risk of bias) or C (high risk of bias).
Two independent reviewers assessed risk of bias. Agreement between the 2 reviewers was assessed using kappa statistics for full-text screening, and rating of relevance and risk of bias. When there was a disagreement about risk of bias, a third reviewer (the first author) checked the data and took the final decision on it.
Summary measures
The principal summary measures were ORs with 95% confidence interval (CI) and P values (considered statistically significant when <0.05). The meta-analysis was completed using the software Comprehensive Meta-Analysis version 2 (Biostat, Inc., Englewood, NJ, USA).
Synthesis of results
Forest plots were generated for graphical presentations for clinical outcomes, and we performed the I2 test and χ2 test for the assessment of heterogeneity across the studies [7]. Each study was summarized by the OR for skeletonized ITA compared with pedicled ITA. The ORs were combined across studies using weighted DerSimonian–Laird random effects model [8] and weighted fixed effects model using the Mantel–Haenszel model [9]. The models were weighted by the number of events in each study to show how much each study contributed in the analysis.
Risk of bias across studies
To assess publication bias, a funnel plot was generated, which was statistically assessed by Begg and Mazumdar's test [10] and Egger's test [11].
Sensitivity analysis
Since the medical literature demonstrates that the use of BITA grafts has been shown to have the potential to increase the incidence of SWI, and this effect is believed to be amplified in diabetic patients [12, 13], we performed subgroup analysis involving patients presenting diabetes or use of bilateral ITA or both. We also performed a subgroup analysis taking into consideration the type of study (randomized or non-randomized).
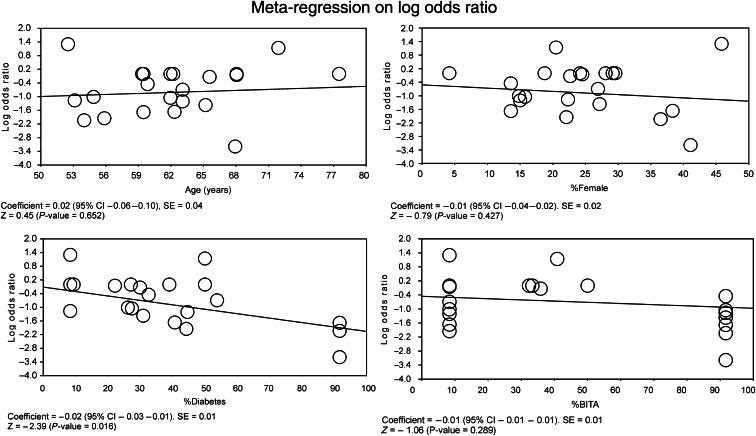
Meta-regression analysis
Meta-regression analyses were performed to determine whether the effects of skeletonized ITA were modulated by prespecified factors. Meta-regression graphs describe the effect of skeletonized ITA on the outcome (plotted as a log OR on the y-axis) as a function of a given factor (plotted as a mean or proportion of that factor on the x-axis). Meta-regression coefficients show the estimated increase in log OR per unit increase in the covariate. Since log OR > 0 corresponds to OR > 1 and log OR < 0 corresponds to OR < 1, a negative coefficient would indicate that as a given factor increases, the OR decreases.
The predetermined modulating factors to be examined were: sex, age, diabetes and use of bilateral ITA. Sex was represented as the proportion of females in the study. Age was represented as the mean age of the patients participating in the study. Diabetes was represented as the proportion of diabetics (insulin dependent or non-insulin dependent) in the study. Bilateral ITA was represented as the proportion of patients that used left and right ITA during CABG.
RESULTS
Study selection
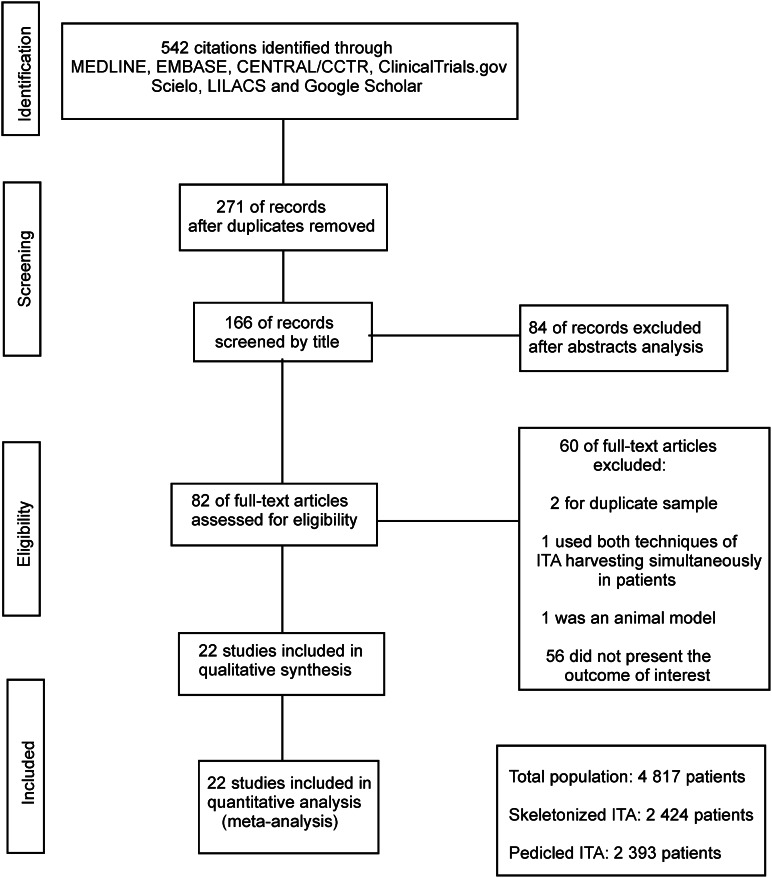
A total of 542 citations were identified, of which 82 studies were potentially relevant and retrieved as full text. Twenty-two [3, 12–32] publications fulfilled our eligibility criteria. Interobserver reliability of study relevance was excellent (κ = 0.85). Agreement for decisions related to study validity was very good (κ = 0.81). The search strategy can be seen in Fig. 1.
Figure 1:
Flow diagram of studies included in data search.
Study characteristics
The characteristics of each study are shown in Table 1. A total of 4817 patients were studied, with 2424 using skeletonized ITA and 2393 using pedicled ITA, including the years 1999–2011; 13 were prospective (59.1%), 8 randomized (36.4%), and 2 multicenter (9.1%). Most studies (77.3%) used a multivariable adjustment for possible confounders. Information not shown in Table 1, but noteworthy, is that most studies consisted of patients whose mean age was around the sixth decade of life, mostly male, and more than half of the studies with more than one third of the population consisted of diabetic patients. The overall internal validity was considered to be a moderate risk of bias.
Table 1:
Study characteristics and risk of bias (internal validity)
| Study | Total incidence of SWI (%) | SKT/PED (n) | Study design | Selection bias | Performance bias | Attrition bias | Detection bias | Multivariable adjustment for possible confounders |
|---|---|---|---|---|---|---|---|---|
| Sá et al. [3] | 5.0 | 186/226 | NP, NR, NM | B | B | A | B | Probably adequate |
| Nishi et al. [12] | 2.2 | 23/23 | P, NR, M | B | B | A | B | Probably adequate |
| Mannacio et al. [13] | 1.0 | 100/100 | P, R, NM | A | B | A | B | Probably adequate |
| Markman et al. [14] | 4.9 | 21/20 | P, R, NM | A | B | A | A | Probably adequate |
| Kamiya et al. [15] | 8.3 | 12/12 | P, R, NM | A | B | A | B | Probably adequate |
| Milani et al. [16] | 4.3 | 35/35 | NP, NR, NM | C | B | C | C | Probably inadequate |
| Gideon et al. [17] | 5.0 | 68/68 | NP, NR, NM | B | B | A | B | Probably adequate |
| Kai et al. [18] | 2.2 | 162/23 | NP, NR, NM | B | B | A | B | Probably adequate |
| Belov et al. [19] | 2.6 | 69/82 | NP, NR, NM | B | B | A | B | Probably adequate |
| De Paulis et al. [20] | 14.9 | 150/300 | P, NR, NM | B | B | A | B | Probably adequate |
| Castro et al. [21] | 4.0 | 25/25 | P, R, NM | A | B | A | B | Probably adequate |
| Hirose et al. [22] | 9.3 | 115/99 | P, NR, M | B | B | A | B | Probably adequate |
| Peterson et al. [23] | 10.4 | 79/36 | P, NR, NM | B | B | A | B | Probable adequate |
| Takami and Ina [24] | 1.5 | 45/20 | P, R, NM | C | B | B | C | Probably inadequate |
| Cartier et al. [25] | 1.1 | 200/440 | NP, NR, NM | B | B | A | B | Probably inadequate |
| Lorberboym et al. [26] | 13.0 | 11/12 | P, R, NM | B | B | A | B | Probably adequate |
| Bonnachi et al. [27] | 4.2 | 110/179 | P, R, NM | B | B | A | B | Probably adequate |
| Huang et al. [28] | 2.0 | 50/50 | NP, NR, NM | B | B | A | B | Probably adequate |
| Cohen et al. [29] | 17.4 | 11/12 | P, R, NM | B | B | A | B | Probably adequate |
| Calafiore et al. [30] | 2.4 | 842/304 | NP, NR, NM | B | B | A | B | Probably adequate |
| Wendler et al. [31] | 2.5 | 40/40 | NP, NR, NM | C | B | C | B | Probably inadequate |
| Deja et al. [32] | 1.4 | 70/287 | P, NR, NM | C | B | C | B | Probably inadequate |
This was performed by 2 independent reviewers. The overall bias of the combined studies was considered moderate.
A: risk of bias is low; B: risk of bias is moderate; C: risk of bias is high; D: incomplete reporting; P: prospective; NP: non-prospective; R: randomized; NR: non-randomized; M: multicenter; NM: non-multicenter; SKT/PED: skeletonized grafts/pedicled grafts.
Synthesis of results
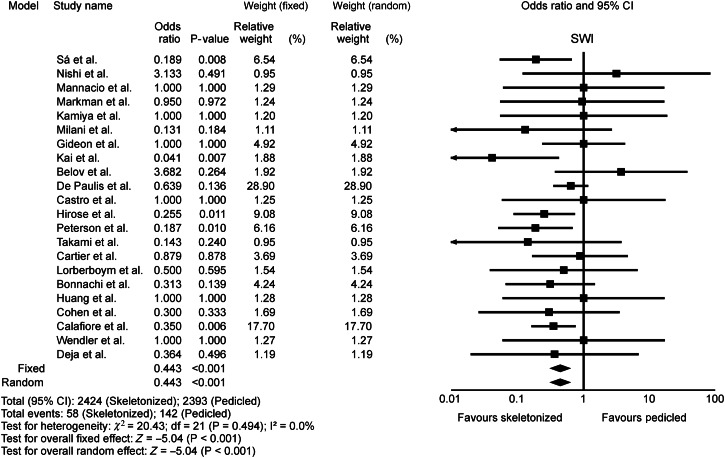
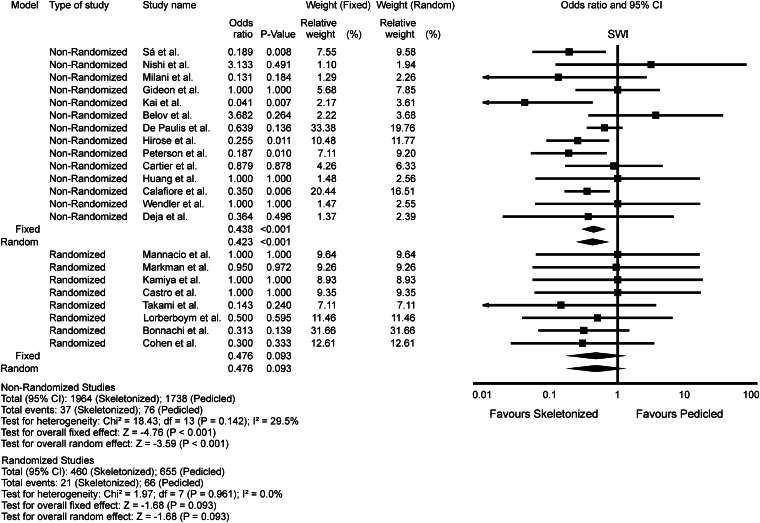
The OR of SWI in the skeletonized ITA group compared with the pedicled ITA group in each study is reported in Fig. 2. There was no evidence for important heterogeneity of treatment effect among the studies for SWI. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.443, 95% CI 0.323–0.608, P < 0.001; random effect model: OR 0.443, 95% CI 0.323–0.608, P < 0.001).
Figure 2:
Odds ratio and conclusions plot of sternal wound infection associated with skeletonized versus pedicled internal thoracic artery.
Risk of bias across studies
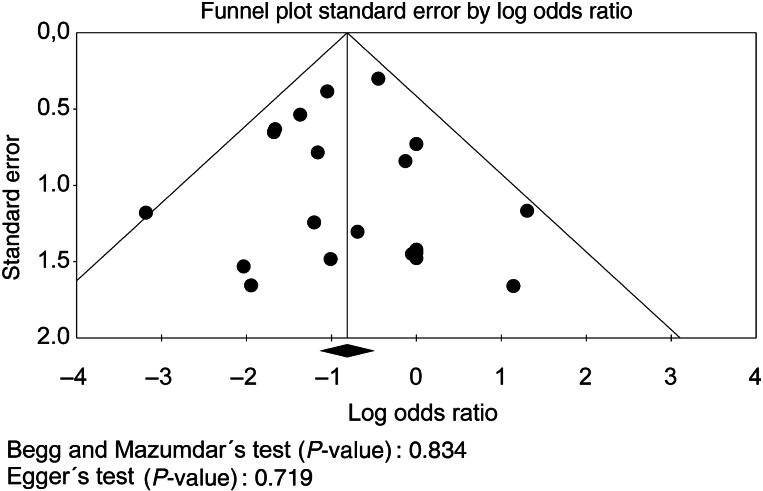
Funnel plot analysis (Fig. 3) disclosed symmetry around the axis for the treatment effect in the SWI outcome, which means we probably do not have a publication bias related to this endpoint.
Figure 3:
Publication bias analysis by funnel plot graphic for sternal wound infection.
Sensitivity analysis
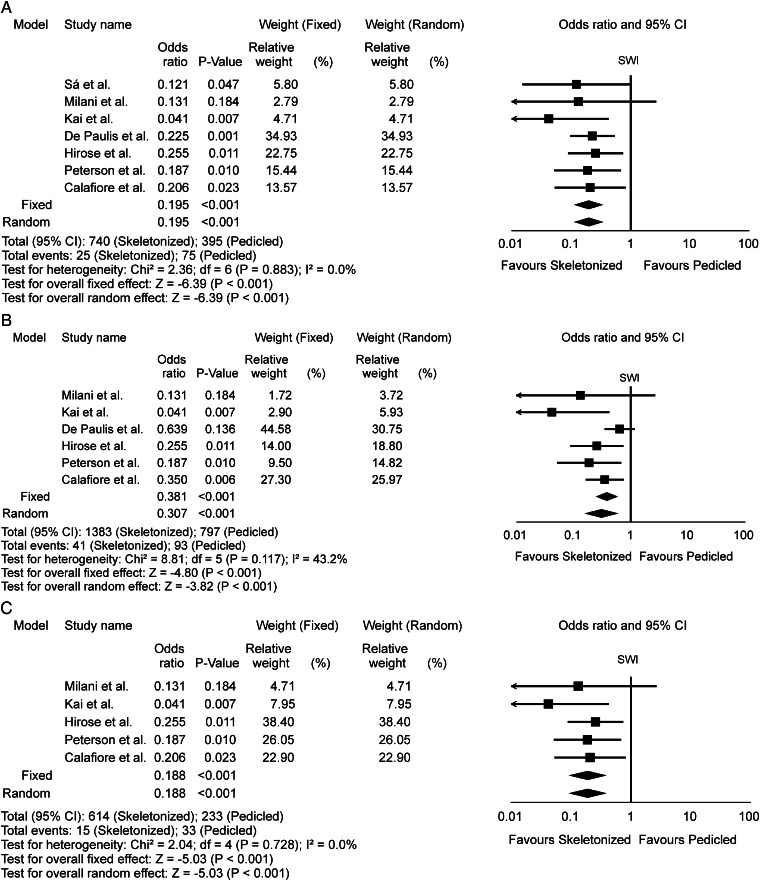
The OR of SWI for diabetic patients in the skeletonized ITA group compared with the pedicled ITA group in each study is reported in Fig. 4A. There was no evidence for important heterogeneity of treatment effect among the studies for SWI in this subgroup. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.195, 95% CI 0.118–0.322, P < 0.001; random effect model: OR 0.195, 95% CI 0.118–0.322, P < 0.001).
Figure 4:
Odds ratio and conclusions plot of sternal wound infection associated with skeletonized vs pedicled internal thoracic artery in sensitivity analysis. (A) Diabetic; (B) Bilateral ITA; (C) Diabetic with bilateral internal thoracic artery harvesting.
The OR of SWI for patients submitted to bilateral ITA harvesting in the skeletonized ITA group compared with the pedicled ITA group in each study is reported in Fig. 4B. There was evidence for important heterogeneity of treatment effect among the studies for SWI in this subgroup. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.381, 95% CI 0.257–0.565, P < 0.001; random effect model: OR 0.307, 95% CI 0.168–0.563, P < 0.001).
The OR of SWI for diabetic patients submitted to bilateral ITA harvesting in the skeletonized ITA group compared with the pedicled ITA group in each study is reported in Fig. 4C. There was no evidence for important heterogeneity of treatment effect among the studies for SWI in this subgroup. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.188, 95% CI 0.098–0.360, P < 0.001; random effect model: OR 0.188, 95% CI 0.098–0.360, P < 0.001).
The OR of SWI in the skeletonized ITA group compared with the pedicled ITA group in non-randomized studies is reported in Fig. 5. There was evidence for moderate heterogeneity of treatment effect among the non-randomized studies for SWI. The overall OR (95% CI) of SWI showed a statistically significant difference in favour of skeletonized ITA (fixed effect model: OR 0.438, 95% CI 0.312–0.616, P < 0.001; random effect model: OR 0.423, 95% CI 0.265–0.677, P < 0.001).
Figure 5:
Odds ratio and conclusions plot of sternal wound infection associated with skeletonized vs pedicled internal thoracic artery in sensitivity analysis (non-randomized vs randomized studies).
The OR of SWI in the skeletonized ITA group compared with the pedicled ITA group in randomized studies is reported in Fig. 5. There was no evidence for heterogeneity of treatment effect among the randomized studies for SWI. The overall OR (95% CI) of SWI showed no statistically significant difference (fixed effect model: OR 0.476, 95% CI 0.201–1.131, P = 0.093; random effect model: OR 0.476, 95% CI 0.201–1.131, P = 0.093).
Meta-regression analysis
Meta-regression coefficients were not statistically significant for SWI and proportion of females, proportion of use of bilateral ITA and mean age, which means that they do not modulate the effect of skeletonized ITA. However, we observed a statistically significant coefficient for SWI and proportion of diabetic patients (coefficient −0.02, 95% CI −0.03 to −0.01, P = 0.016), which means that the greater the proportion of diabetic patients in a population undergoing CABG, the lower the OR for SWI in the skeletonized ITA group, i.e. the greater the protective effect of skeletonized ITA for diabetic patients in relation to the incidence of SWI, (Fig. 6).
Figure 6:
Meta-regression analysis by representative plots.
DISCUSSION
Summary of evidence
The results of this meta-analysis demonstrate that there was a statistically significant difference in favour of skeletonized ITA compared with pedicled ITA in the risk for SWI, the summary measures being free from the influence of heterogeneity of the effects (except for bilateral ITA subgroup) or publication bias. In the sensitivity analysis, the difference in favour of skeletonized ITA was also observed in subgroups such as diabetic, bilateral ITA and diabetic with bilateral ITA. Also, in the sensitivity analysis, we observed that there was a difference in the type of study, since non-randomized studies together demonstrated the benefit of skeletonized ITA in comparison with pedicled ITA, but the randomized studies together did not show this difference. Meta-regression did not demonstrate any influence of female gender, age or use of bilateral ITA on SWI, but showed a modulation influence of diabetes.
Considerations about this meta-analysis
To our knowledge, this is the largest meta-analysis of studies performed to date, providing incremental value by demonstrating that skeleletonized ITA reduces the incidence of SWI compared with pedicled ITA. These results were found probably as a result of better sternal perfusion after ITA skeletonization compared with the pedicled ITA [15, 33]. Kamiya et al. [15] showed that the oxygen saturation and blood flow in the microcirculation of the sternum tissue were better when using the skeletonized ITA compared with pedicled ITA. Boodhwani et al. [33] conducted a study with 48 patients, in which each individual was subjected to CABG using bilateral ITA, and all ITAs were dissected skeletonized on the left side and pedicled on the right side (this study was not included in our meta-analysis since all patients were submitted to both harvesting techniques, making comparison non-feasible). Patients were then evaluated for sternal perfusion through scintigraphy (radionuclear image). The authors found that sternal perfusion was increased in the skeletonized side compared with the pedicle side (increase of 17.6%, P = 0.03).
According to some authors [34, 35], females, the elderly and patients submitted to bilateral ITA harvesting are thought to face higher risks associated with pedicled ITA and therefore benefit more from skeletonized ITA. The meta-regression analysis in this study refutes the hypothesis that differences related to gender, age or use of bilateral ITA in the study population are responsible for the treatment effects observed across studies. Interestingly, we observed a modulation of the effect of the skeletonized ITA by the variable diabetes. The negative coefficient observed indicates that there is an inverse relationship in modulation, i.e. the more diabetic patients we have in a study group, the smaller is the OR of SWI risk in the group treated with skeletonized ITA. This demonstrates that skeletonization is beneficial in general, and even more so in the diabetic group—something confirmed by analysis of the subgroup of diabetics.
We also observed a difference in summary results depending on the type of study analyzed. As we demonstrated, non-randomized studies support the idea of the benefit of skeletonized ITA in comparison with pedicled ITA, while randomized studies have failed to show this difference (although the result was close to statistical significance and with the tendency to favour the skeletonized group). The main explanation for this phenomenon lies in the sample size for each type of study. While non-randomized studies have a total population of 4102 patients, randomized studies have only 715 patients. Considering that SWI is a complication with low incidence, a larger sample is needed to demonstrate a statistically significant difference between the two types of intervention for a particular outcome, and obviously the randomized studies totalled a small sample for this purpose. We argue that the maximum incidence of SWI in CABG surgery should be no larger than 5.0%. Among the studies included in our meta-analysis, six studies exceeded this cut-off [15, 20, 22, 23, 26, 29]. Of these, three studies had a very small sample size [15, 26, 29], <25 patients, which makes few events in this population simulate a high incidence (a merely aesthetic statistical effect), so that their incidences do not reflect the context of CABG in the general population. The other 3 studies [20, 22, 23] dealt with a special risk group—in this case, diabetic patients, exclusively—in which we would have expected a higher incidence of SWI, but being risk groups, these studies also do not reflect the context of CABG in the general population. Considering all the other 16 studies, which had larger sample sizes and dealt with populations that included all types of patients, we have established our argument, since none exceeded the cut-off of 5.0%. We simulated a calculation of the minimum sample size required to obtain a probabilistic sample for conducting a randomized study, considering a 95% CI, power of 80%, a proportion of 1 patient in the skeletonized group for each patient in the pedicled group, the maximum acceptable incidence for postoperative SWI reported in the literature being 5%, and we obtained a minimum total sample of 1526 individuals (763 patients in each arm). This could explain why the non-randomized studies have demonstrated a statistical difference (because they reached the minimum sample) while randomized trials have failed (because they did not reach the minimum sample.) This fact points to the need for a randomized study with a larger sample to confirm or refute the hypothesis of the benefit of skeletonized ITA in comparison with pedicled ITA.
What is different from the largest previous meta-analysis?
Although another meta-analysis from Saso et al. [36] has been published in this field, this analysis is important for certain reasons.
Our pooled sample size was 31.5% larger than the largest previously published meta-analysis [36]. This larger sample size translated into greater statistical power and precision, reducing the amount of uncertainty surrounding treatment effects. Nine published studies had not been included in the largest prior meta-analysis and were included in our analysis (contributing 1154 out of the 4817 patients).
Saso et al. [36] performed a publication bias analysis without the application of statistical analysis for this specific study. We performed a publication bias analysis applying two statistical tests for each analysis.
We also conducted an analysis of risk of bias of individual studies, something not done by our predecessor. They also showed no heterogeneity of effects in bilateral ITA subgroup analysis, but we claim this is not true, considering that we used the same studies and the same sample size for this subgroup analysis, and we identified an important heterogeneity of the effect of skeletonized ITA in this specific group.
All these characteristics may give readers a more detailed view and a better critical analysis of the medical literature on this issue. Our meta-analysis summarized the results of studies on medical literature regarding SWI outcomes, strengthening the concept of ITA skeletonization for CABG. Furthermore, the meta-regression enhances the consistency of pooled results and reveals the importance of skeletonization for diabetic patients.
Risk of bias and limitations
This meta-analysis included data from non-randomized and/or observational studies, which reflects the real world, but they are limited by treatment bias, confounders and a tendency to overestimate treatment effects. Patient selection alters outcome and thus makes non-randomized studies obviously less robust.
Although important statistical heterogeneity among studies was not observed (except when we analysed bilateral ITA subgroup), the differences in terms of operative technique and volume may have led to an influence of clinical heterogeneity not picked up by the meta-analysis. Other factors that would have influenced the results but were not well reported and thus not taken into consideration were the prevalence of obesity, chronic pulmonary obstructive disease, excessive use of bone wax or diathermy, quality of operative antisepsis prophylaxis, multiple transfusions, glycemic control in diabetics and the way the patient is prepared for surgery (shaving, cleaning and timing of both before the operation), bacterial flora of each centre, etc.
There are inherent limitations with meta-analyses, including the use of cumulative data from summary estimates. Patient data were gathered from published data, not from individual patient follow-up. Access to individual patient data would have enabled us to conduct further subgroup analysis and propensity analysis to account for differences between the treatment groups.
Future perspectives
Because the findings support a potential benefit from a specific harvesting method and as part of the regular curriculum in cardiovascular surgery, we recommend that the skeletonization technique should become a mandatory part of the training of cardiovascular surgery residents. The results of this study suggest the need for large-scale (with a calculated probabilistic sample size), multicentre, prospective, randomized trials of skeletonized vs pedicled ITA grafts to verify that there is indeed a difference in the incidence of postoperative SWI.
Conclusions
Skeletonized ITA appears to reduce the incidence of postoperative SWI in comparison with pedicled ITA after CABG, with this effect being modulated by the presence of diabetes.
Conflict of interest: none declared.
REFERENCES
- 1.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care: associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. doi: 10.1016/j.ajic.2008.03.002. doi:10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Sá MP, Silva DO, Lima EN, Lima RC, Silva FP, Rueda FG, et al. Postoperative mediastinitis in cardiovascular surgery. Analysis of 1038 consecutive surgeries. Rev Bras Cir Cardiovasc. 2010;25:19–24. doi:10.1590/S0102-76382010000100008. [PubMed] [Google Scholar]
- 3.Sá MP, Soares EF, Santos CA, Figueiredo OJ, Lima RO, Escobar RR, et al. Risk factors for mediastinitis after coronary artery bypass grafting surgery. Rev Bras Cir Cardiovasc. 2011;26:27–35. doi: 10.1590/s0102-76382011000100008. doi:10.1590/S0102-76382011000100008. [DOI] [PubMed] [Google Scholar]
- 4.Sá MP, Soares EF, Santos CA, Figueiredo OJ, Lima RO, Escobar RR, et al. Skeletonized left internal thoracic artery is associated with lower rates of mediastinitis in diabetic patients. Rev Bras Cir Cardiovasc. 2011;26:183–9. doi: 10.1590/s0102-76382011000200007. doi:10.1590/S0102-76382011000200007. [DOI] [PubMed] [Google Scholar]
- 5.Sá MP, Santos CA, Figueiredo OJ, Lima RO, Ferraz PE, Soares AM, et al. Skeletonized left internal thoracic artery is associated with lower rates of mediastinitis in elderly patients. Rev Bras Cir Cardiovasc. 2011;26:617–23. doi: 10.1590/s0102-76382011000200007. doi:10.5935/1678-9741.20110053. [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 7.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. doi:10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–14. doi: 10.1016/j.cct.2006.04.004. doi:10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–6. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. doi:10.2307/2533446. [PubMed] [Google Scholar]
- 11.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. doi:10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nishi H, Mitsuno M, Tanaka H, Ryomoto M, Fukui S, Miyamoto Y. Decreasing sternum microcirculation after harvesting the internal thoracic artery. Eur J Cardiothorac Surg. 2011;40:240–4. doi: 10.1016/j.ejcts.2010.10.027. doi:10.1016/j.ejcts.2010.10.027. [DOI] [PubMed] [Google Scholar]
- 13.Mannacio V, Tommaso L, Amicis V, Stassano P, Vosa C. Randomized flow capacity comparison of skeletonized and pedicled left internal mammary artery. Ann Thorac Surg. 2011;91:24–30. doi: 10.1016/j.athoracsur.2010.06.131. doi:10.1016/j.athoracsur.2010.06.131. [DOI] [PubMed] [Google Scholar]
- 14.Markman PL, Rowland MA, Leong JY, van der Merwe J, Storey E, Marasco S, et al. Skeletonized internal thoracic artery harvesting reduces chest wall dysesthesia after coronary bypass surgery. J Thorac Cardiovasc Surg. 2010;139:674–9. doi: 10.1016/j.jtcvs.2009.03.066. doi:10.1016/j.jtcvs.2009.03.066. [DOI] [PubMed] [Google Scholar]
- 15.Kamiya H, Akhyari P, Martens A, Karck M, Haverich A, Lichtenberg A. Sternal microcirculation after skeletonized versus pedicled harvesting of the internal thoracic artery: a randomized study. J Thorac Cardiovasc Surg. 2008;135:32–7. doi: 10.1016/j.jtcvs.2007.09.004. doi:10.1016/j.jtcvs.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Milani R, Brofman PR, Guimaraes M, Barboza L, Tchaick RM, Meister Filho H, et al. Double skeletonized internal thoracic artery vs. double conventional internal thoracic artery in diabetic patients submitted to OPCAB. Rev Bras Cir Cardiovasc. 2008;23:351–7. doi: 10.1590/s0102-76382008000300011. doi:10.1590/S0102-76382008000300011. [DOI] [PubMed] [Google Scholar]
- 17.Gideon S, Meir A, Battler A, Shapira Y, Vidne BA, Ben-Dor I. Bilateral skeletonized internal mammary versus single-pedicled internal mammary grafting in the elderly. Isr Med Assoc J. 2007;9:294–8. [PubMed] [Google Scholar]
- 18.Kai M, Hanyu M, Soga Y, Nomoto T, Nakano J, Matsuo T, et al. Off-pump coronary artery bypass grafting with skeletonized bilateral internal thoracic arteries in insulin-dependent diabetics. Ann Thorac Surg. 2007;84:32–6. doi: 10.1016/j.athoracsur.2007.02.095. doi:10.1016/j.athoracsur.2007.02.095. [DOI] [PubMed] [Google Scholar]
- 19.Belov IUV, Bazylev VV, Sanai EB. Comparative assessment of the use of skeletonized and un-skeletonized internal thoracic artery for myocardial revascularization. Kardiologiia. 2005;45:50–4. [PubMed] [Google Scholar]
- 20.De Paulis R, de Notaris S, Scaffa R, Nardella S, Zeitani J, Del Giudice C, et al. The effect of bilateral internal thoracic artery harvesting on superficial and deep sternal infection: the role of skeletonization. J Thorac Cardiovasc Surg. 2005;129:536–43. doi: 10.1016/j.jtcvs.2004.07.059. doi:10.1016/j.jtcvs.2004.07.059. [DOI] [PubMed] [Google Scholar]
- 21.Castro GP, Dussin LH, Wender OB, Barbosa GV, Saadi EK. Comparative analysis of the flows of left internal thoracic artery grafts dissected in the pedicled versus skeletonized manner for myocardial revascularization surgery. Arq Bras Cardiol. 2005;84:261–6. doi: 10.1590/s0066-782x2005000300013. doi:10.1590/S0066-782X2005000300013. [DOI] [PubMed] [Google Scholar]
- 22.Hirose H, Amano A, Takanashi S, Takahashi A. Skeletonized bilateral internal mammary artery grafting for patients with diabetes. Interact CardioVasc Thorac Surg. 2003;2:287–92. doi: 10.1016/S1569-9293(03)00046-X. doi:10.1016/S1569-9293(03)00046-X. [DOI] [PubMed] [Google Scholar]
- 23.Peterson MD, Borger MA, Rao V, Peniston CM, Feindel CM. Skeletonization of bilateral internal thoracic artery grafts lowers the risk of sternal infection in patients with diabetes. J Thorac Cardiovasc Surg. 2003;126:1314–9. doi: 10.1016/s0022-5223(03)00808-0. doi:10.1016/S0022-5223(03)00808-0. [DOI] [PubMed] [Google Scholar]
- 24.Takami Y, Ina H. Effects of skeletonization on intraoperative flow and anastomosis diameter of internal thoracic arteries in coronary artery bypass grafting. Ann Thorac Surg. 2002;73:1441–5. doi: 10.1016/s0003-4975(02)03501-4. doi:10.1016/S0003-4975(02)03501-4. [DOI] [PubMed] [Google Scholar]
- 25.Cartier R, Leacche M, Couture P. Changing pattern in beating heart operations: use of skeletonized internal thoracic artery. Ann Thorac Surg. 2002;74:1548–52. doi: 10.1016/s0003-4975(02)04015-8. doi:10.1016/S0003-4975(02)04015-8. [DOI] [PubMed] [Google Scholar]
- 26.Lorberboym M, Medalion B, Bder O, Lockman J, Cohen N, Schachner N, et al. 99mTc-MDP bone SPECT for the evaluation of sternal ischaemia following internal mammary artery dissection. Nucl Med Commun. 2002;23:47–52. doi: 10.1097/00006231-200201000-00008. doi:10.1097/00006231-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Bonacchi M, Prifti E, Giunti G, Salica A, Frati G, Sani G. Respiratory dysfunction after coronary artery bypass grafting employing bilateral internal mammary arteries: the influence of intact pleura. Eur J Cardiothorac Surg. 2001;19:827–33. doi: 10.1016/s1010-7940(01)00695-9. doi:10.1016/S1010-7940(01)00695-9. [DOI] [PubMed] [Google Scholar]
- 28.Huang Q, Wendler O, Langer F, Tscholl D, Schaefers HJ. Effects of skeletonized versus pedicled internal thoracic artery grafts on free flow capacity during bypass. J Tongji Med Univ. 2000;20:308–10. doi: 10.1007/BF02888187. doi:10.1007/BF02888187. [DOI] [PubMed] [Google Scholar]
- 29.Cohen AJ, Lockman J, Lorberboym M, Bder O, Cohen N, Medalion B, et al. Assessment of sternal vascularity with single photon emission computed tomography after harvesting of the internal thoracic artery. J Thorac Cardiovasc Surg. 1999;118:496–502. doi: 10.1016/s0022-5223(99)70188-1. doi:10.1016/S0022-5223(99)70188-1. [DOI] [PubMed] [Google Scholar]
- 30.Calafiore AM, Vitolla G, Iaco AL, Fino C, Di Giammarco G, Marchesani F, et al. Bilateral internal mammary artery grafting: midterm results of pedicled versus skeletonized conduits. Ann Thorac Surg. 1999;67:1637–42. doi: 10.1016/s0003-4975(99)00282-9. doi:10.1016/S0003-4975(99)00282-9. [DOI] [PubMed] [Google Scholar]
- 31.Wendler O, Tscholl D, Huang Q, Schafers HJ. Free flow capacity of skeletonized versus pedicled internal thoracic artery grafts in coronary artery bypass grafts. Eur J Cardiothorac Surg. 1999;15:247–50. doi: 10.1016/s1010-7940(99)00012-3. doi:10.1016/S1010-7940(99)00012-3. [DOI] [PubMed] [Google Scholar]
- 32.Deja MA, Wos S, Golba KS, Zurek P, Domaradzki W, Bachowski R, et al. Intraoperative and laboratory evaluation of skeletonized versus pedicled internal thoracic artery. Ann Thorac Surg. 1999;68:2164–8. doi: 10.1016/s0003-4975(99)00820-6. doi:10.1016/S0003-4975(99)00820-6. [DOI] [PubMed] [Google Scholar]
- 33.Boodhwani M, Lam BK, Nathan HJ, Mesana TG, Ruel M, Zeng W, et al. Skeletonized internal thoracic artery harvest reduces pain and dysesthesia and improves sternal perfusion after coronary artery bypass surgery: a randomized, doubleblind, within-patient comparison. Circulation. 2006;114:766–73. doi: 10.1161/CIRCULATIONAHA.106.615427. doi:10.1161/CIRCULATIONAHA.106.615427. [DOI] [PubMed] [Google Scholar]
- 34.Bellchambers J, Harris JM, Cullinan P, Gaya H, Pepper JR. A prospective study of wound infection in coronary artery surgery. Eur J Cardiothorac Surg. 1999;15:45–50. doi: 10.1016/s1010-7940(98)00255-3. doi:10.1016/S1010-7940(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 35.Toumpoulis IK, Theakos N, Dunning J. Does bilateral internal thoracic artery harvest increase the risk of mediastinitis? Interact CardioVasc Thorac Surg. 2007;6:787–91. doi: 10.1510/icvts.2007.164343. doi:10.1510/icvts.2007.164343. [DOI] [PubMed] [Google Scholar]
- 36.Saso S, James D, Vecht JA, Kidher E, Kokotsakis J, Malinovski V, et al. Effect of skeletonization of the internal thoracic artery for coronary revascularization on the incidence of sternal wound infection. Ann Thorac Surg. 2010;89:661–70. doi: 10.1016/j.athoracsur.2009.08.018. doi:10.1016/j.athoracsur.2009.08.018. [DOI] [PubMed] [Google Scholar]