Abstract
Pneumopericardium is rare and has been reported secondary to chest trauma. We report a case of tension pneumopericardium occurring during double-lung transplantation, where intraoperative transoesophageal echocardiography first showed a hypokinetic left ventricle and a few minutes later a compression of its anterolateral portion due to pneumopericardium. Although the pericardium was opened, left ventricular function remained depressed, necessitating extracorporeal membrane oxygenation, which was withdrawn after 48 h of assistance when left ventricular function had recovered. The patient was extubated on the seventh postoperative day but died of multiorgan failure on the 64th postoperative day.
Keywords: Lung transplantation, Pneumopericardium, Transoesophageal echocardiography
INTRODUCTION
Few observations of pneumopericardium have been published following lung transplantation [1–3]. We report the first case of tension pneumopericardium occurring intraoperatively during double-lung transplantation and leading to haemodynamic failure.
CASE REPORT
A 46-year old woman with emphysema had been registered on the lung transplantation list for 7 days. Right lung perfusion was 75% of total. Preoperative echocardiography showed normal right and left ventricular ejection fractions (LVEF). Right cardiac cavities were of normal size. Pulmonary systolic pressure was ascertained to be 40 mmHg. Coronary arteries appeared normal on coronary angiography.
Intraoperative monitoring included continuous systemic and right heart pressure measurements, continuous cardiac output and mixed venous oxygen saturation monitoring, and transoesophageal echocardiography (Cardiac Ultrasound System Vivid 7 and multiplane 6.2/5.0-MHz probe; GE Healthcare, Fairfield, CT, USA). The Oto score of the donor lungs was 0.
Induction of anaesthesia was without any significant haemodynamic event; femoral artery pressure was 145/82 mmHg, pulmonary artery pressure was 40/22 mmHg and venous oxygen saturation was 65%. Transoesophageal echocardiography showed a LVEF of 50% with no valvular lesions, and a patent foramen ovale was ruled out.
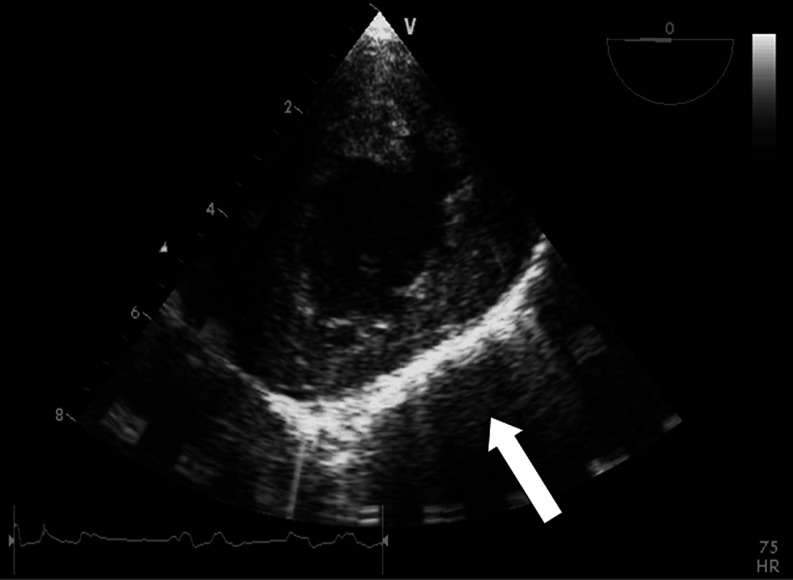
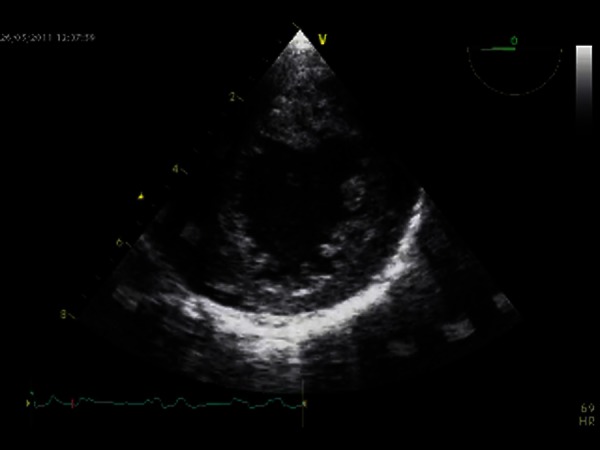
Surgery began with a left anterolateral thoracotomy, and selective right lung ventilation was used to facilitate the dissection of pleural adhesions. Acute haemodynamic deterioration occurred during the intrapericardial dissection of the left superior pulmonary vein. The femoral artery pressure decreased abruptly to 55/35 mmHg and pulmonary artery pressure increased to 68/40 mmHg at that time, while mixed venous oxygen blood saturation decreased to 45%. Transoesophageal echocardiography showed a decrease in LVEF to 40% and the left ventricle was globally hypokinetic, but no air emboli were visible at this stage of the transplant surgery (Video 1). Ten minutes later, severe posteroseptal hypokinesis appeared, while contractility of the right ventricle seemed normal. Epinephrine was started at 0.5 mg/h and increased to 2 mg/h, but we did not observe any improvement of LVEF. A few minutes later, transoesophageal echocardiography showed a compression of the anterolateral portion of the left ventricle that appeared unexpectedly, given that there was no surgical dissection manoeuvre in the same area (Fig. 1; Video 2). The surgeon immediately performed a short right anterolateral thoracotomy to eliminate a possible right compressive pneumothorax, which was not found. Given that the increase in epinephrine dose rate had not improved the situation, extracorporeal membrane oxygenation (ECMO) was quickly initiated via the femoral artery and vein to improve the haemodynamic state. A 3 l/min flow provided satisfactory pressure to permit surgery to continue. At this point, no explanation for the acute occurrence of left ventricular hypokinesis and haemodynamic failure had been found. Only when the surgeon returned to the left side of the thorax did he discover a dilated pericardium filled with air. The pericardium was opened, liberating air under pressure. Despite this manoeuvre, left ventricular function failed to improve; the LVEF remained at approximately 40% despite an infusion of 1–1.8 mg/h epinephrine and an ECMO assistance flow of 1 l/min. The double-lung transplantation was completed uneventfully under ECMO assistance, which could not be weaned at the end of the procedure. The double-lumen tube was replaced with a standard tracheal tube and during this exchange procedure the airways were examined fiberoptically by a pneumologist, who found no airway lesion that could explain the occurrence of this pneumopericardium.
Video 1:

Global left ventricular hypokinesis (0° transgastric view).
Figure 1:
Anterolateral compression of the left ventricle (arrow) on a 0° transgastric view.
Video 2:
Severe left ventricular inferoseptal hypokinesis and anterolateral compression of the left ventricle (0° transgastric view).
The patient was transferred to the intensive care unit, where left ventricular function recovered after 48 h of assistance, allowing cessation of ECMO. The epinephrine infusion was stopped on the third postoperative day. The patient was extubated on the seventh postoperative day, but died of multiorgan failure secondary to sepsis on the 64th postoperative day.
DISCUSSION
Long ago, Macklin [4] described three possible mechanisms for the development of a pneumopericardium: direct communication between the airways and the pericardium, pleuropericardial communication associated with a pneumothorax, or a migration of air due to alveolar rupture from the interstitial tissue along the pulmonary perivascular sheaths to the pericardium.
Bronchial suture dehiscence, barotraumas and air leaks have been proposed as the possible aetiologies of the cases of pneumopericardium that have occurred during the postoperative course of lung transplantations. These cases can be explained by the first two mechanisms mentioned by Macklin [4], namely direct communication between the airways and the pericardium or pleuropericardial communication associated with a pneumothorax, because they occurred in the postoperative period and because the pericardium is opened during lung transplantation.
In our patient, a bronchial aetiology is unlikely because pneumopericardium occurred early, before surgery on the bronchial area, and postoperative fibreoptic bronchoscopy did not show any sign of a bronchial tear, which could have resulted from insertion of the double-lumen tube. A contralateral pneumothorax was ruled out intraoperatively. Macklin's third pathophysiological mechanism of air migration along the perivascular sheaths to the pericardium might be the only one to fit our case report to some degree. Thus, a possible hypothesis, even if it is difficult to admit, may be the occurrence of an air trap. Some degree of alveolar rupture and air leakage may have occurred during dissection on the left side. Air could have migrated to the pericardium, which was opened on the left side during dissection, followed the vascular sheaths and remained trapped on the anterolateral side of the pericardium, thus compressing the left ventricle. Once this air was inside the pericardium on the right side of the thorax, it probably could not exit the pericardial sac because the emphysematous right lung occupied the whole hemithorax and acted as a one-way valve.
In our case, it was surprising to observe acute and severe left ventricular failure without echographic signs that could help to enable a diagnosis to be reached. No specific echographic signs of pneumopericardium have been described, but it may be suggestive when the pericardial space appears hyperechogenic. Thus, transoesophageal echocardiography did not establish a clear diagnosis, but at least allowed us to rule out potential causes of haemodynamic failure.
The second striking fact in our case is the prolonged left ventricular dysfunction despite the fact that compression of the heart lasted less than 30 min. Generally, pneumopericardium diminishes the cardiac output because of impaired cardiac diastolic filling and not because of decreased LVEF. Our case corresponds to a stunned myocardium, which was defined by Braunwald et al. [5] as prolonged, yet reversible postischaemic ventricular dysfunction, usually without tissue necrosis. A stunned myocardium can be observed in critically ill patients without ischaemic heart disease, after transient myocardial ischaemia, successful defibrillation, central nervous system injury and various aetiologies all characterized by normal coronary arteries, as in our case. A particular type of stunned myocardium is Tako-tsubo cardiomyopathy, which is characterized by transient abnormalities of wall motion involving the left ventricular apex and mid-ventricle, but echocardiographic imaging in our case did not reveal this.
In conclusion, this case shows that tension pneumopericardium may appear intraoperatively during lung transplantation and can lead to prolonged left ventricular dysfunction. The severity of left ventricular dysfunction and an image of compression were established by transoesophageal echocardiography, but the diagnosis of pneumopericardium was not clear on transoesophageal echocardiography.
Funding
This work was supported by institutional funding.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
References
- 1.Taccone FS, Marechal R, Appoloni O. Pneumopericardium after bilateral lung transplantation. Heart. 2006;92:1326. doi: 10.1136/hrt.2005.082370. doi:10.1136/hrt.2005.082370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lasocki S, Castier Y, Geffroy A, Mal H, Brugière O, Lesèche G, et al. Early cardiac tamponade due to tension pneumopericardium after bilateral lung transplantation. J Heart Lung Transplant. 2007;26:1069–71. doi: 10.1016/j.healun.2007.07.014. doi:10.1016/j.healun.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Navas B, Cobos MJ, Vaquero JM, Santos F, Cosano A. Cardiac tamponade secondary to pneumopericardium after lung transplantation: a case report. Transplant Proc. 2008;40:3123–5. doi: 10.1016/j.transproceed.2008.09.026. doi:10.1016/j.transproceed.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 4.Macklin C. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med. 1939;64:913–26. doi:10.1001/archinte.1939.00190050019003. [Google Scholar]
- 5.Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation. 1982;66:1146–9. doi: 10.1161/01.cir.66.6.1146. doi:10.1161/01.CIR.66.6.1146. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.