Abstract
Sternal clefts are rare congenital malformations of the chest wall. Immediate correction in neonates or in infancy is beneficial in terms of providing skeletal cover with little or no need for any prosthetic material for reconstruction. In the absence of internal midline defects, one should aim to provide complete correction when the chest wall is still compliant, and cardiorespiratory compromise is expected to be least after correction. We report on 2 children who underwent primary sternal-cleft repair using a periosteal advancement flap along with mobilization of lateral sternal bars after sliding osteotomy of corresponding ribs.
Keywords: Sternal cleft, Primary repair
INTRODUCTION
A sternal cleft is an extremely rare condition resulting from a failure of the fusion of the sternal bars. This can be classified as complete or incomplete, where there is either an inferior or superior attachment. Sternal clefts can be associated with other defects, particularly intracardiac, diaphragmatic or intra-abdominal midline defects. When associated conditions are extensive, the prognosis is generally very poor, but isolated sternal clefts are usually associated with good recovery and survival. The use of prosthetic material on top of the periosteal flap is known and is common, particularly when primary repair is delayed beyond neonates. We report on the technical feasibility of sliding osteochondroplasty combined with a periosteal flap to treat this cleft in 2 infants without the need for any prosthetic material.
CASE REPORTS
Two neonates were referred for evaluation of chest wall defects by the postnatal team. Both neonates had uneventful antenatal histories and normal scans before birth. Delivery was uneventful, but soon after birth, the chest wall defect was noticed by the paediatric team while assessing the newborn. There was no respiratory distress and no need for any intervention at that stage.
A detailed echocardiography was organized in both of them to rule out intracardiac defects. One neonate had an aortic arch extending to the thoracic inlet and also had a cutaneous haemangioma. There was a suspicion of Phaces syndrome in that neonate, though it could not be proven at that stage. There were no cardiac defects otherwise in both of them. Abdominal evaluation was normal. Sternal examination consisted of initial video examination soon after birth, which showed features of a near-total sternal cleft with attachment at the inferior edge. Subsequently, a thorough clinical assessment was carried out by the specialist team, confirming the nature of defect and its attachment at the lower edge.
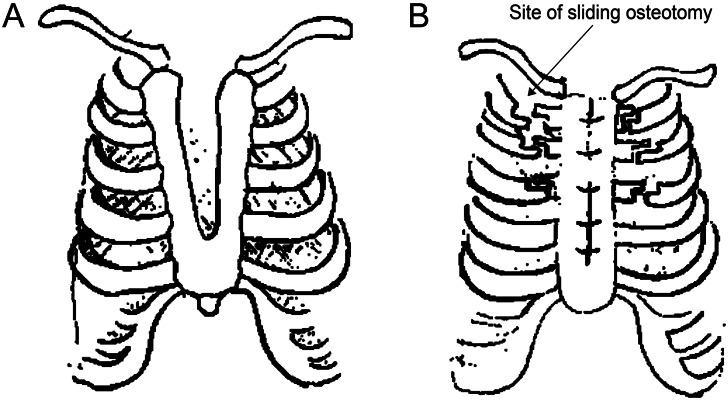
Imaging consisted of magnetic resonance imaging (MRI) in both infants. This confirmed the presence of a sternal cleft and a bar inferiorly (Fig. 1). In view of the extent of the cleft, repair was planned soon and was performed at 2 and 3 months of age in both infants.
Figure 1:
(A) Images of MRI showing the edges of lateral sternal bars (arrow). (B) Intraoperative photograph showing the lateral sternal bars and an inferior sternal attachment.
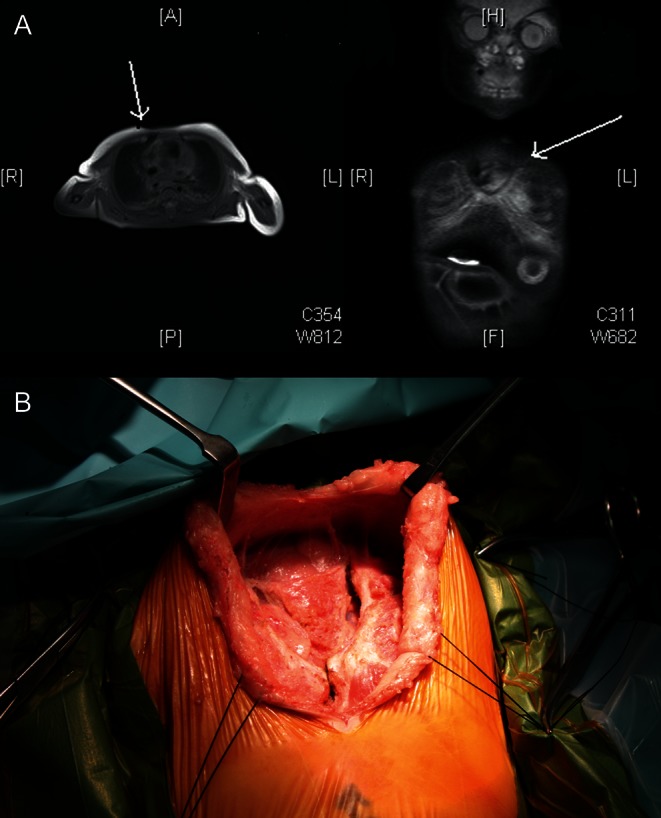
Surgery was done through a vertical midline incision, and the sternal edges were defined (Fig. 2). The inferior sternal bar was divided and further mobilization was carried out to isolate the sternal edges from both sides. The thymus was removed in total. There was an anterior pericardial defect in 1 infant that was left untreated, though an external inspection of the heart was carried out further in that infant and confirmed as a normal external anatomy of the heart. There was also a defect noted in the anterior portion of the diaphragm just behind the sternal bar (Morgagni type hernia without any contents), which was closed with a polytetrafluoroethylene patch.
Figure 2:
(A) Line diagram showing the nature of upper sternal cleft and the inferior sternal bar; (B) line diagram showing the site of sliding osteotomy on either side starting from the second rib downwards. The muscle flap involving pectoralis major is reattached at the end, providing a muscle cover to the repair site.
The periosteum was incised on the opposing edge of the sternum on both sides to create both raw surfaces for union, and a periosteal flap. A sliding cartilage flap was created between the second and fourth costal cartilages, and the sternal bars from both sides were advanced to meet in the midline. The posterior periosteal flat was initially sutured followed by sternal approximation with vicryl sutures (Polyglactin 910, Ethicon, Inc., USA). The detached pectoralis major muscle was sutured back on the area of the costal slide to close the dead space on the cartilages on both sides. There was no loss of tidal volume on ventilation. A single mediastinal drain was left in situ, and a further suction drain was left in the subcutaneous plane for further wound closure.
Recovery in both infants was uncomplicated, and they were discharged home between 4 and 6 days. Review at 2 and 4 months showed complete wound healing, and a well-united sternum and no evidence of any instability. Both remain asymptomatic on follow-up.
DISCUSSION
Sternal clefts are rare congenital anomalies and are either upper- or lower-type defects. A lower-type defect is usually associated with other congenital defects such as exomphalos or abdominal wall defects, diaphragmatic hernia and intracardiac defects and can be part of Pentrology of Cantrell. Upper defects are equally rare, but have the uniting bar at the lower end, and are more commonly seen in isolation [1].
They usually result from the primary failure of sternal edges at the time of migration of the lateral plate of the mesoderm at the 10th week of gestation [2]. They may either fail to migrate at this stage, which may lead to a complete sternal cleft or an incomplete migration or separation due to rupture of the chorion or yolk sac resulting from a cardiac descent causing a cleft [3]. Upper clefts are more common than a lower cleft. There may occasionally be a primary absence of the cephalic single element, called presternum.
A similar early disturbance of the midline mesodermal structures at this stage along with the cutaneous tissue has also been thought to be the cause of the association of sternal malformations with vascular dysplasias such as haemangiomas [3].
An antenatal diagnosis is likely, particularly when the clefts are extensive, and associated with other conditions such as diaphragmatic hernia, abdominal wall defects or ectopia cordis. Quite often, the diagnosis is obvious at the time of delivery, in both isolated clefts and in extensive variants.
Diagnostic work-ups include computed tomography scans or MRI evaluation of the chest and abdomen, focusing on those rare but complex associated anomalies. They are quite helpful in prognosticating the extent of the lesion, and directing the appropriate surgical therapy.
Surgery is the treatment of choice, is performed usually soon after diagnosis and is rarely effective when performed beyond 3 months, if one were to avoid the use of any prosthetic material [4]. A simple advancement of lateral sternal bars is ineffective, as a loss of tidal volume or restriction of thoracic contents can negate the surgical effectiveness [4]. A lateral release is usually necessary and our technique of sliding chondroplasty is effective in achieving the release of sternal bars well enough to avoid the associated restrictive effect. Sometimes, the hypoplastic nature of the sternal edges may preclude primary approximation and may even necessitate the use of either autologous grafts such as cartilages or bone grafts and at times synthetic substances like acrylic or silicone elastomer [5].
In conclusion, a primary repair early in life with advancement of lateral sternal bars provides a good cosmetic and physiological result in this rare but difficult group of chest wall defects.
ACKNOWLEDGEMENT
The author acknowledges M. Kanani for his kind help in preparing the line diagrams used to sketch the nature of the defect and its repair, which were used in this manuscript.
Conflict of interest: none declared.
REFERENCES
- 1.Yavuzer S, Kara M. Primary repair of a sternal cleft in an infant with autogenous tissues. Interact CardioVasc Thorac Surg. 2003;2:541–3. doi: 10.1016/S1569-9293(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 2.Amato JJ, Douglas WI, Desai U, Burke S. Ectopia cordis. Chest Surg Clin North Am. 2000;10:297–316. doi:10.1161/CIRCULATIONAHA.106.176158. [PubMed] [Google Scholar]
- 3.Kaplan LC, Matsuoka R, Gilbert EF, Opitz JM, Kumit DM. Ectopia cordis and cleft sternum: evidence for mechanical teratogenesis following rupture of the chorion or yolk sac. Am J Med Genet. 1985;21:187–99. doi: 10.1002/ajmg.1320210128. doi:10.3945/ajcn.2009.27725. [DOI] [PubMed] [Google Scholar]
- 4.Campos JM, Das-Neves-Pereira JC, Velhote MCP, Jatene FB. Twenty seven-year experience with sternal cleft repair. Eur J Cardiothorac Surg. 2009;35:539–41. doi: 10.1016/j.ejcts.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Snyder BJ, Robbins RC, Ramos D. Primary repair of complete sternal cleft with pectoralis major muscle flaps. Ann Thorac Surg. 1996;61:983–4. doi: 10.1016/0003-4975(95)00786-5. doi:10.3945/ajcn.2009.29146. [DOI] [PubMed] [Google Scholar]