Abstract
Children spend a considerable amount of time in preschools and child care centers. As a result, these settings may have an influence on their diet, weight, and food security, and are potentially important contexts for interventions to address nutritional health. The Child and Adult Care Food Program (CACFP) is one such intervention. No national study has compared nutrition-related outcomes of children in CACFP-participating centers to those of similar children in non-participating centers. We use a sample of four-year old children drawn from the Early Childhood Longitudinal Study, Birth Cohort to obtain estimates of associations between CACFP program participation and consumption of milk, fruits, vegetables, fast food, and sweets, and indicators of overweight, underweight status and food insecurity. We find that, among low-income children, CACFP participation moderately increases consumption of milk and vegetables, and may also reduce the prevalence of overweight and underweight. Effects on other outcomes are generally small and not statistically significant.
Keywords: child nutrition, early childhood programs, public assistance, program evaluation
The incidence of overweight among preschoolers (children aged two to five) increased from 7.2% to 13.9% between the late 1970s and the early 2000s and has been particularly elevated for low-income children (Wang & Beydoun, 2007). For example, in the early 2000s, 17.4% of low-SES children aged two to nine were overweight, as compared to 9.7% of same-aged high-SES children (Wang & Beydoun, 2007). The amount of time young children spend in non-parental care has also increased; for example, the fraction of three- to four-year-olds enrolled in preschools doubled between 1970 to 1993, and increased another nine percentage points between 1994 and 2002, reaching more than 56% in 2002, before falling to about 52% in the recent economic recession (Aud et al., 2011). Increasing overweight and time in child care have led policymakers and others to focus on preschools, child care centers, and homes as important access points for nutritional programs for young children, especially poor children; some have argued that efforts to improve nutrition and influence the dietary habits in child care settings may be particularly effective (American Dietetic Association, 2005; Briley & McAllaster, 2011; Story, Kaphingst, & French, 2006).
The federal Child and Adult Care Food Program (CACFP) or its predecessors has been serving children in child care since the late 1960s. As of 2008, the CACFP spends about $2.4 billion annually to reimburse child care providers for meals and snacks served to children in their care. The size of the program in terms of expenditures is similar to the USDA's School Breakfast Program. The CACFP reimburses participating centers according to a child's family income, similar to the USDA's School Lunch Program. In addition, Head Start program rules require participation in CACFP. Nonetheless, CACFP fails to reach many children, including many poor children, because of program rules that prevent some child care providers from participating and because of provider non-participation, even though almost all providers are eligible for some level of subsidy (Gordon, Kaestner, Korenman, & Abner, 2011).
Despite the size and potential importance of the program, few studies have examined the effects of CACFP on children, and to our knowledge, only one study of two centers (Bruening, Gilbride, Passannante, & McClowry, 1999, reviewed below) has compared children in CACFP-participating settings to similar children in non-participating settings. This gap in research and in knowledge about a program of this size has been noted in prior reviews of social welfare programs. Glantz (2004, p. 326) summarized his review of CACFP research as follows: “Some studies have assessed the nutrient contribution of CACFP meals and snacks to participants' overall diets. However, there has been no research on the impact of the program on participants' nutrition and health status, relative to nonparticipants.” And, in a comprehensive review of federal nutrition programs, Currie (2006, p. 86) concluded:
One of the most important [of the smaller food programs] is the Child and Adult Care Food Program, which operates somewhat like the school meals programs, but serves approximately 1.7 million low-income children in daycare centers. There has been little investigation of the benefits of participation in these programs.
We use the Early Childhood Longitudinal Survey-Birth Cohort (ECLS-B; Snow et al., 2007) to obtain estimates of associations between CACFP participation and children's food consumption, weight (e.g., obesity), and family food security. The ECLS-B is a household survey that includes direct child assessments, as well as on-site visits and observations of child care providers and interviews with center directors and home care providers. The linked household-provider design is critical to this study because participation in CACFP is determined by providers, and families may not be aware that their provider receives reimbursements from the CACFP. Ours is the first large-scale study to examine the potential benefits of participation in CACFP, especially for low-income children, the target beneficiaries of CACFP.
Program Description
The CACFP reimburses caregivers for meals and snacks served to children in child care centers, preschools, day care homes, after-school programs, and homeless shelters. As noted above, CACFP serves approximately two million children and had expenditures of $2.4 billion in 2008.
CACFP Eligibility and Reimbursement Rates
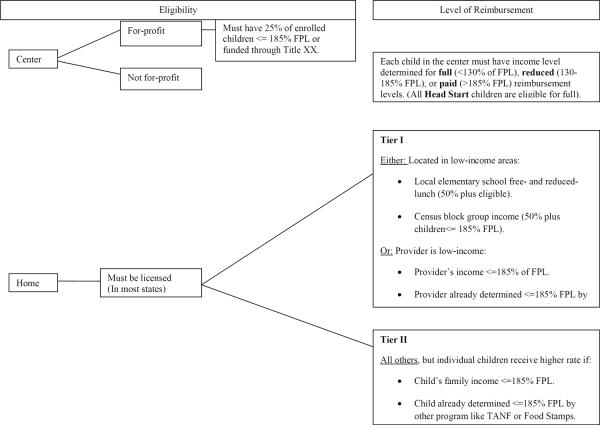
Four criteria determine eligibility and reimbursement levels: type of care (center vs. home, for-profit vs. non-profit, licensed vs. unlicensed), neighborhood income, provider income, and/or family income of children. Figure 1 (from Gordon et al., 2011) describes these criteria for the period corresponding to our study, 2001–2005. As we discuss below, we focus our analysis on 4-year-old children in centers or preschools. Our program description, therefore, pertains to these ages and settings.
Figure 1.
Eligibility and reimbursement rules for child care providers participating in the Child and Adult Care Food Program (CACFP).
Note. FPL=federal poverty level
CACFP reimburses centers on a per-meal, per-child basis. All centers are eligible to receive some level of reimbursement from CACFP except for-profit providers that serve few low-income children. The child's family income determines the reimbursement level: full (for incomes below 130% of the federal poverty line), reduced (for incomes between 130% and 185% of poverty), or paid (for incomes above 185% of poverty). In 2004–05, full reimbursement rates were $1.23 for breakfast, $2.24 for lunch, and $0.61 for snacks; reduced rates were $0.93, $1.84 and $0.30, respectively; and paid rates equaled $0.23, $0.21, and $0.05, respectively (U.S. Department of Agriculture, n.d.). Program rules make children who participate in Temporary Assistance for Needy Families (TANF), Food Stamps (now the Supplemental Nutrition Assistance Program, or SNAP), or Head Start categorically eligible for full reimbursement. For-profit centers are ineligible if fewer than 25% of enrolled children are either categorically eligible, income-eligible (less than 185% of poverty) or receive subsidies for care through Title XX (Social Services Block Grant funds; U.S. Department of Agriculture, 2008). Federal regulations require that centers “be licensed, or otherwise have approval, by the appropriate Federal, State, or local licensing authority” (Richard B. Russell National School Lunch Act, 2010, p. 73). States typically do not require centers and preschool programs overseen by organizations such as schools, churches, or local governments to obtain licenses (National Child Care Information Center and the National Association for Regulatory Administration, 2009).
Potential Mechanisms Linking CACFP to Children's Nutritional Outcomes
There is considerable scope for CACFP to influence nutritional outcomes because children in full-time care typically consume half to two-thirds of their daily meals and snacks at child care on days when they are in care (Ziegler, Briefel, Ponza, Novak, & Hendricks, 2006). The CACFP may influence children's nutritional health directly or indirectly, through several pathways. Consider, for example, the possible causal pathways from CACFP participation to children's overweight status. CACFP could directly reduce the chance that a child is overweight by improving dietary quality in the child care setting. CACFP seeks to improve dietary quality though three primary mechanisms: resources (reimbursements for meals), information (such as nutritional guidelines), and monitoring (of menus). Monitoring and resources (reimbursements) should increase providers' adherence to the dietary guidelines. In principle, the CACFP could operate through indirect mechanisms; for example, promoting healthy eating in the child care setting could carry over into the home, as children may develop healthier eating habits.
CACFP-participating providers receive information about federal nutritional guidelines, although providers retain discretion in menu planning (Fleischhacker, Cason, & Achterberg, 2006; Oakley, Bomba, Knight, & Byrd, 1995). For children aged three to five, CACFP meal patterns recommend that, for breakfast, children have three-fourths cup of milk, one-half cup of a fruit or vegetable, and one-half slice or one-half serving of a grain. For lunch or supper, three-to-five-year olds should consume three-fourths cup milk, two half-cup servings of a fruit or vegetable, one serving of a grain or bread, and one serving of meat or meat alternate. A lunch-time serving of meat for a three-to-five year-old is 1.5 ounces, although meal patterns include a variety of alternates such as a six ounce serving of yogurt. Snacks must include two of the following four components: one-half cup of milk, one fruit or vegetable, one grain or bread, or one meat or meat alternative (U.S. Department of Agriculture, 2009).
Thus, information provided in the CACFP guidelines has the potential to improve dietary quality by increasing children's consumption of milk, fruits, vegetables, and grains and by reducing their consumption of less nutritious foods such as sweet snacks, sodas, or fruit-flavored drinks. Moreover, periodic monitoring provides incentives to adhere to the guidelines so as not to risk losing funding. Providers must keep daily documentation of planned menus and any deviations from plans including a record of the foods and drinks served for meals and snacks each day. They must also record program enrollment, attendance, and the number of meals served. Upon request, providers must produce these records for review.
Reimbursements for meals also increases resources available to CACFP-participating providers and may allow providers to increase the quantity or quality of food provided relative to non-participating settings. If the quantity of food is increased, then some low-income children will meet calorie needs and be less likely to be underweight when care occurs in a participating setting rather than a non-participating setting. However, whether and how changes in diet affect weight is uncertain because weight is determined by net caloric intake; and, whereas some CACFP-recommended foods such as vegetables have few calories, other nutritious foods, such as whole milk and fruit juice, do not. The potentially greater quantity and quality of food consumed at CACFP-participating settings should also improve children's food security unless parents alter the food served to children at home to offset the food their children eat in child care, which seems unlikely (Nord, 2009).
On the other hand, providers have latitude in food menus and monitoring of meals is imperfect. Further, children may not eat the food that is served. Thus, CACFP participation may have little effect on food intake. Evidence on provider adherence to menu requirements is mixed. Some studies find relatively good adherence. For example, Crepinsek, Burstein, Lee, Kennedy, and Hamilton (2002) found that, in home care settings, over 90% of breakfasts, lunches, and snacks met the meal pattern requirements. In addition, the Feeding Infants and Toddlers Study (FITS) showed that children consumed more milk, fruits and vegetables during lunches served at child care than during lunches served at home, though it did not identify which child care providers participated in CACFP (Ziegler et al., 2006). However, other studies observed deviations from meal patterns, unrecorded substitutions from planned menus or unconsumed food in CACFP-participating settings. For example, a study of participating homes and centers in Texas found that no provider always adhered to the CACFP meal patterns, and the only meal components served 100% of the time were milk at breakfast and meat at lunch (Kuratko, Martin, Lan, Chappell, & Ahmad, 2000). In a study of Head Start centers, only four of 269 meals perfectly matched menu descriptions (Fleischhacker et al., 2006). A recent study of 40 centers in New York City, 38 of which participated in CACFP, also observed disparities between national dietary guidelines, foods served, and children's dietary intake (Erinosho, Dixon, Young, Brottman, & Hayman, 2011).
While it is useful to compare actual practices against standards, as several studies have done, ultimately, the effect of CACFP on children can only be determined by comparing children who participate in CACFP to similar children who do not participate. Bruening, Gilbride, Passannante and McClowry (1999) conducted the only study of this type of which we are aware. They compared outcomes for 20 children in an urban day care center that participated in the CACFP to 20 children cared for in a nearby non-participating center where children brought meals from home. Dietary quality was determined for a 14-day period from both observations of foods consumed at the centers and parental reports of children's food intake outside the centers. Bruening et al. (1999) reported that, on average, children at the CACFP-participating center had higher intake of vitamin A, riboflavin, and calcium, increased consumption of milk and vegetables, and reduced consumption of sweets/fats compared to children at the non-participating center. CACFP participation was not statistically significantly associated with a child's weight or dental health, but was significantly associated with fewer missed days of care due to illness.
The strength of the Bruening et al. (1999) study is the depth and quality of outcome measures, particularly measures based on dental exams and direct observation of dietary intake. The two major weaknesses are external validity because of the limited sample size and context (40 children in two centers) and threats to internal validity because of the lack of adjustment for potentially confounding factors such as participation in other nutrition assistance programs (85% of children cared for in the CACFP-participating center also received other Federal food assistance whereas only 20% of children in the non-participating center received such support).
The size and potential impact of the program and the virtual absence of previous study of the nutritional impacts of CACFP underscores the importance of our study. Our study is national in scope, giving it wide external validity. While it is a non-experimental study, we exploit access to an extensive set of measured characteristics that, along with an appropriate research design and statistical methods, addresses many potential threats to internal validity. In sum, our study fills a gap in knowledge about the potential effects of CACFP on child nutritional outcomes and it represents the first, large-scale study of the issue. While we cannot claim that estimates of CACFP impacts from our study are causal, they are obtained after adjusting for many potential confounding influences and are arguably the best and most informative estimates available.
Research Questions
In this article, we compare the food intake, food security, and weight-for-height of preschoolers who attend CACFP-participating child care centers to preschoolers who attend non-participating centers. We take advantage of the nationally-representative ECLS-B to examine the following research questions:
Research question 1
How do food consumption, weight, and food insecurity of preschoolers who attend CACFP-participating centers compare to preschoolers who attend non-participating centers, among all children, and among low-income children? Among low-income children participating in CACFP, how do those who attend Head Start differ from those who do not? We use extensive descriptive statistics to answer this question.
Research question 2
What are the associations between attending a CACFP-participating center and children's food intake (diet), weight, and food security, adjusting for covariates, among all children and among low-income children? Among low income children, how do these associations differ for children who do not attend Head Start? We use propensity-weighted multivariable logistic regression to answer this question. This approach yields estimates of associations between attending a CACFP-participating center and children's food intake (diet), weight, and food security, adjusted for covariates.
Method
Estimating CACFP Effects
Our objective was to estimate associations between CACFP participation and food consumption, weight-for-height (e.g., overweight status), and food security, with a focus on low-income children. Ideally, we would obtain estimates that could be interpreted as causal. However, given the observational nature of our data, achieving this goal was made difficult by two problems: non-random participation in CACFP and mandatory participation of Head Start centers in CACFP. The first of these is common to non-experimental evaluations of program impact, whereas the second is more specific to the CACFP.
Non-Random CACFP Participation
CACFP participation was not randomly assigned. As descriptive statistics (presented shortly) clearly showed, family and provider characteristics of children whose providers received CACFP benefits differ from those of children whose providers did not receive benefits. Differences in these characteristics are likely to affect children's nutritional outcomes. Indeed, in prior research, we found that children are more likely to attend CACFP-participating centers when they live in a higher-poverty ZIP code and when their family is poor (Gordon et al., 2011). Lower income has also been associated with overweight status and food insecurity (Nord, Andrews, & Carlson, 2009; Wang & Beydoun, 2007).
Other characteristics of the child, family, community, and child care provider may also be correlated with both CACFP participation and children's food intake, weight status, and food insecurity. The reasons that a family uses a particular child care center may be either positively or negatively correlated with children's health (Gordon et al., 2011). Some parents may seek out a center with ample, high-quality food because they lack food at home. Other parents may seek out a provider who offers nutritious food because they prioritize nutrition, and also provide healthy meals and snacks at home. At the community level, some poor neighborhoods have been called `food deserts' and may have more children participating in CACFP at the same time that healthy foods may be less available or more expensive than in higher-income neighborhoods (Beaulac, Kristjansson, & Cummins, 2009). At the center level, directors with more experience may be more likely to seek reimbursements from CACFP and also deliver effective care in other ways, such as through better health practices.
In sum, family, organizational and environmental factors are likely to influence both CACFP participation and children's food consumption, weight, and food insecurity. Fortunately, the ECLS-B measured many such variables. In addition, the longitudinal nature of the data allowed us to include children's prior outcomes (food consumption, BMI, and food insecurity) as covariates, which is a powerful method for addressing the non-random selection associated with CACFP participation (NICHD Early Child Care Research Network & Duncan 2003).
Analytically, we addressed the issue of selection on observed characteristics (including prior outcomes) by using propensity-score, weighted regression, an approach that is becoming more widely used in non-experimental evaluation (see Imbens & Wooldridge, 2009 for a detailed review of recent developments in techniques for program evaluation; Williamson, Morley, Lucas, & Carpenter, 2012 for an excellent non-technical discussion of propensity score methods; and Ferguson & Ready, 2011, and Ryan, Johnson, Rigby, & Brooks-Gunn, 2011 for recent applications in early childhood research).
For this approach, we first estimated the child's propensity to participate in (receive benefits from) CACFP using a logistic regression. We then used the regression results to calculate each child's predicted probability of participating in CACFP. Since all of the outcomes we studied are dichotomous (e.g., the child consumed two or more servings of vegetables per day or not), we estimated a logistic regression to model the impact of CACFP participation on each nutrition-related outcome. For the second logistic regression, we used the predicted probability of participating in CACFP – referred to as the propensity score – as a weight for children who did not participate in CACFP. Because we were interested in the effect of participating in CACFP on children who participated (referred to as the “effect of the treatment on the treated” in the program evaluation literature), propensity weights were computed as follows. Observations for participants were given a weight of one, and those for non-participants were given a weight of , where, for each non-participant , is the predicted probability of participation computed from the logistic regression (Imbens & Wooldridge, 2009; for an application, see Hirano & Imbens, 2002). Non-participant weights were re-scaled (normed) so the weighted sample size equaled the unweighted sample count for non-participants. We used the same set of covariates (other than CACFP participation) in these outcome regressions as in the participation regressions used to estimate propensity weights.
Propensity-score, weighted regression has several advantages over standard multiple regression for program evaluation foremost of which is better “matching” (i.e., balance of covariates) between the children who did and did not participate in CACFP. Unlike standard multiple regression (e.g., OLS, logit, probit), propensity-score weighting ensures that covariates are balanced—children who do and do not participate in CACFP have a similar distribution of covariates. Propensity score weighting also addresses in a parsimonious way the problem of choosing the correct model specification, for example, whether to include non-linear terms and interactions between variables. Unlike ordinary regression, estimate from propensity-weighted regressions are “doubly robust,” meaning they are consistent even if the outcome equation or the participation equation is mis-specified, as long as there are no unmeasured confounders (Busso, DiNardo, & McCrary, 2009; Imbens & Wooldridge, 2009). Propensity weighting also has some advantages over a closely related technique: propensity matching. Although a variety of propensity matching techniques have been employed, most match each program participant to one or a few “nearest neighbors” (i.e., observations with a similar propensity to participate) in the non-participant group. Nearest neighbor matching requires researchers to choose a standard of closeness for matches as well as the number of matches if there is to be more than one. Propensity-weighted regression requires no such decision or criteria as it merely down-weights observations among the control group with lower propensities to participate. As for statistical efficiency, Busso et al. (2009) report that “…the large sample literature has established two results that are relevant here. First, a suitable reweighting estimator is asymptotically efficient…Second, pair matching is asymptotically inefficient” (p. 1). Furthermore, Busso et al. (2009) conduct simulation studies for finite samples that indicate that, for applications such as the one under study here, propensity-weighted regression estimators are likely to have lower variances than similar propensity-matching estimators.
Since we used propensity score weights, we used a model-based approach to account for the complex sampling design of the ECLS-B, rather than a design-based approach to applying sampling weights. Specifically, we included design variables (low birth weight and race/ethnicity) and the sampling weight as controls in our regression models (Korn & Graubard, 1995a, 1995b; Potter, Grau, Williams, Diaz-Tena, & Carlson, 2006). We also calculated robust standard errors that allow for clustering on the ZIP code of residence (Rogers, 1993; Wooldridge, 2002, 2006).
We note that we did not use another widely used method for non-experimental evaluation–person fixed effects (within-case design also known as first differences) – because of limitations of our data. Fixed-effects methods require exact repeated measures for predictors and outcomes across waves, which we did not have. We also had a wide interval of two years between waves; and, we anticipate that the subsample of children in centers likely differs between age two and age four (due to the well-established increase in center use for preschoolers versus toddlers); and, because we expect that the association between CACFP participation and child outcomes might vary for two- and four-year-olds, due to developmental differences at these ages. We did, however, include lagged measures of food intake, BMI, and food security in our propensity-score-weighted regressions, using the most comparable measures from the two-year-old wave. This approach will adjust for health characteristics of children that are stable across time (Johnson, 2005).
In reporting regression results, we indicate significance at the p<.05 or p<.10 level based on two-sided tests. We discuss results that are significant at the p<0.10 level if they are in the expected direction (i.e., if participation in CACFP is beneficial for children's nutritional outcomes).
Mandatory Participation of Head Start Centers in CACFP
Although children at all income levels may derive some benefits from the CACFP program, our primary interest is in estimating effects of CACFP participation on outcomes for low-income children. Therefore, for some analyses, we restricted the sample to low-income children (those with family incomes below 185% of the federal poverty line or who recently participated in TANF or SNAP). The co-occurrence of Head Start and CACFP presented an analytical challenge for this purpose, beyond the issue of non-random participation just discussed. All Head Start centers are required to participate in CACFP and, thus, there was no comparison group of low-income children who attended a Head Start setting but did not receive CACFP. Some studies have found evidence that participating in Head Start is associated with children's weight status, a finding that may or may not be due to aspects of Head Start beyond CACFP participation (see, for example, Frisvold & Lumeng, 2011). If Head Start improves nutritional outcomes, then we may erroneously attribute some of those benefits to the CACFP program. Therefore, we tested the sensitivity of CACFP estimates to the inclusion or exclusion of Head Start children from the subsample of low-income children. Specifically, we estimated separate CACFP participation equations and outcome equations for each of three subsamples: all children, low-income children, and low-income children who did not participate in Head Start.
Data and Sample
We used data from the restricted-use files of the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), a study of a nationally representative sample of children followed from birth. We rounded sample sizes to the nearest 50 as required by the data-sharing agreement that governs the use of the restricted ECLS-B data.
Children in the ECLS-B were born in 2001 in 46 states. At the initial nine-month interview, the sample size was 10,700, resulting from a response rate of 74%. At the two-year and four-year follow up interviews, sample sizes were 9,850 and 8,950, respectively. The ECLS-B oversampled twins, children born at low birth weight, and American Indian and Asian children. (We retained only the “focal” twin of each twin pair.) At age two, 43% of children in the sample were non-Hispanic White, 16% non-Hispanic Black, 20% non-Hispanic other, and 21% were Hispanic. At the two- and four-year follow-ups, the child's primary non-parental care provider—the person who cared for the child for the most hours per week—was contacted for an interview. The weighted response rate in the four-year follow-up was approximately 90% for center-based and Head Start providers (Snow et al., 2007). Sampling weights were created to adjust for the initial sampling design, initial nonresponse, and differential nonresponse over time (Snow et al., 2007). We used these weights for descriptive statistics and included the sample weight and design variables as controls in regression models.
We restricted our regression analyses to four-year-olds who were cared for in centers (we use the term “center” and “preschool” interchangeably). We focused on centers (including preschools) because our goal was to compare participating and non-participating children in comparable child care settings. License-exempt homes are ineligible for CACFP in most states, and, in our sample, only a tiny fraction participated in CACFP. In addition, only a small percentage of four-year-olds, and a small number of children in our sample, were in licensed homes, as centers were the primary settings for non-parental care for three-quarters of low-income four-year-olds in our sample (Gordon et al., 2011). We studied outcomes for four-year-olds rather than two-year-olds because few children were in centers at earlier ages and because several outcomes (e.g., detailed food intake) were not available for two-year-olds. For some models, we restricted the sample to low-income children because of the increased likelihood of poor nutritional outcomes for this group and because the CACFP rules and reimbursement rates have increasingly targeted benefits to this group (Glantz, 2004).
Restricting to the subpopulation of children in center care retained 4,250 of the 8,950 four-year-olds in the study; requiring non-missing information on CACFP participation and nutritional outcomes reduced the sample size to 4,050, of which 1,850 participated in the CACFP program. We imputed data for item non-response for covariates other than CACFP participation using Stata's multiple imputation routines “ice” and “mim” (Royston, 2005). We included all variables (other than CACFP participation) listed in Tables 1 and 2 in the imputation models, including outcomes, though for each regression we discarded cases with an imputed outcome value (von Hippel, 2007). We completed 10 imputations (Graham, Olchowski, & Gilreath, 2007).
Table 1.
Means, 4-Year-Olds in Child Care Centers
| Full Sample | Low- Income Familiesa | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| CACFP Participation | CACFP Participation | Among CACFP Participants: HS Participation | ||||
|
|
||||||
| No (1) | Yes (2) | No (3) | Yes (4) | No (5) | Yes (6) | |
| 1. Outcomes | ||||||
| Child's healthy food intake | ||||||
| Milk, 2+ cups/day | 0.70 | 0.73* | 0.66 | 0.75* | 0.74 | 0.75 |
| Fruit or Juice, 3+ servings/day | 0.48 | 0.54* | 0.54 | 0.57 | 0.53 | 0.61* |
| Vegetables, 2+ servings/day | 0.32 | 0.40* | 0.38 | 0.41 | 0.37 | 0.45* |
| Child's avoidance of less-healthy foods | ||||||
| Salty Snacks, <= 1 – 3 servings/week | 0.61 | 0.59 | 0.55 | 0.60 | 0.60 | 0.60 |
| Fast Food < = 1 – 3 servings/week | 0.91 | 0.87* | 0.90 | 0.86* | 0.88 | 0.84 |
| Sweet Snacks, < = 1 – 3 servings/week | 0.34 | 0.42* | 0.41 | 0.44 | 0.45 | 0.46 |
| Sodas <= to 1 – 3 servings/week | 0.74 | 0.57* | 0.61 | 0.56* | 0.56 | 0.56 |
| Child's weight-for-height (measured) | ||||||
| Underweight | 0.03 | 0.02 | 0.03 | 0.02 | 0.02 | 0.02 |
| Overweight | 0.15 | 0.19* | 0.23 | 0.20 | 0.18 | 0.21 |
| Overweight or at-risk of overweight | 0.32 | 0.39* | 0.37 | 0.39 | 0.39 | 0.39 |
| Child and household food insecurity | ||||||
| Household is food insecure | 0.08 | 0.32* | 0.34 | 0.45* | 0.41 | 0.49* |
| Children are food insecure | 0.05 | 0.20* | 0.19 | 0.28* | 0.25 | 0.31* |
| 2. Child characteristics | ||||||
| Race/ethnicity | ||||||
| Hispanic | 0.13 | 0.30* | 0.25 | 0.33* | 0.33 | 0.34 |
| Non-Hispanic, White | 0.73 | 0.39* | 0.51 | 0.33* | 0.34 | 0.30 |
| Non-Hispanic, Black | 0.07 | 0.25* | 0.17 | 0.28* | 0.27 | 0.30 |
| Non-Hispanic, Other | 0.07 | 0.06 | 0.06 | 0.06 | 0.06 | 0.06 |
| Child was born low birth weight | 0.05 | 0.09* | 0.07 | 0.09 | 0.09 | 0.09 |
| Mother ever breast fed child | 0.78 | 0.61* | 0.65 | 0.58* | 0.61 | 0.55* |
| Child had < 2 check-upsd in last 2 years | 0.16 | 0.17 | 0.18 | 0.17 | 0.20 | 0.13* |
| 3. Family income and neighborhood poverty | ||||||
| Family Income-to-Needs Ratioe | 4.36 | 1.83* | 1.19 | 1.00* | 1.09 | 0.91* |
| Since last interview, family Food Stamps use | 0.09 | 0.42* | 0.42 | 0.58* | 0.52 | 0.65* |
| Since last interview, family TANF use | 0.03 | 0.14* | 0.12 | 0.20* | 0.18 | 0.22* |
| Since last interview, child WIC use | 0.13 | 0.54* | 0.49 | 0.68* | 0.65 | 0.73* |
| Young child poverty rate in ZIP code | 12.2 | 22.7* | 19.6 | 25.4* | 25.5 | 25.5 |
| 4. Mother characteristics | ||||||
| Mother's age | 34.5 | 30.7* | 30.8 | 29.7* | 29.7 | 29.8 |
| Mother's education | ||||||
| Less than high school | 0.11 | 0.32* | 0.34 | 0.40* | 0.38 | 0.44* |
| High school graduate | 0.10 | 0.25* | 0.18 | 0.28* | 0.26 | 0.29 |
| Some college | 0.30 | 0.31 | 0.35 | 0.28* | 0.31 | 0.26 |
| Bachelor's degree or higher | 0.49 | 0.12* | 0.13 | 0.04* | 0.06 | 0.02* |
| Mother married | 0.84 | 0.53* | 0.51 | 0.44* | 0.46 | 0.45 |
| Mother's employment status | ||||||
| Not employed | 0.38 | 0.39 | 0.39 | 0.46* | 0.41 | 0.54* |
| Full-time | 0.39 | 0.43* | 0.39 | 0.35 | 0.38 | 0.30* |
| Part-time | 0.23 | 0.18* | 0.22 | 0.18 | 0.20 | 0.16* |
| No English at home or mother not born in US | 0.15 | 0.27* | 0.21 | 0.30* | 0.29 | 0.31 |
| Household has rules about food | 0.87 | 0.69* | 0.74 | 0.65* | 0.68 | 0.62* |
| 5. Center characteristics | ||||||
| Head Start (HS) | 0.00 | 0.35* | 0.00 | 0.44* | 0.00 | 1.00* |
| Non-HSb center, refers to or from HS | 0.21 | 0.37* | 0.36 | 0.34 | 0.62 | 0.00* |
| Not Head Start | 0.79 | 0.28* | 0.64 | 0.22* | 0.38 | 0.00* |
| Director experience at center, years | 7.88 | 7.30* | 7.39 | 7.42 | 6.95 | 8.0*7 |
| Sponsorship and Accreditation | ||||||
| Center for-profit | 0.33 | 0.14* | 0.29 | 0.12* | 0.16 | 0.05* |
| Center not sponsored, non-profit | 0.28 | 0.31* | 0.26 | 0.31* | 0.20 | 0.46* |
| Center sponsored, non-profit | 0.38 | 0.55* | 0.40 | 0.57* | 0.63 | 0.49* |
| Center accredited | 0.40 | 0.58* | 0.41 | 0.59* | 0.61 | 0.58 |
| Licensure and Size | ||||||
| Center Licensed | 0.74 | 0.86* | 0.73 | 0.85* | 0.80 | 0.92* |
| Center Licensed to Care Size | 79.4 | 122.4* | 74.0 | 121.8* | 128.5 | 108.3* |
| 6. Lagged child outcomes (age 2) | ||||||
| Food Insecurity at Age 2 | ||||||
| Not food insecure | 0.92 | 0.76* | 0.77 | 0.71* | 0.71 | 0.68 |
| Household food insecure only | 0.04 | 0.11* | 0.11 | 0.13 | 0.13 | 0.15 |
| Household and children food insecure | 0.04 | 0.13* | 0.11 | 0.16* | 0.16 | 0.17 |
| Child milk consumption at age 2 | ||||||
| No milk consumption | 0.21 | 0.26* | 0.27 | 0.27 | 0.25 | 0.29 |
| Drinks milk with meals only | 0.29 | 0.25* | 0.25 | 0.25 | 0.24 | 0.24 |
| Drinks milk with snacks only | 0.18 | 0.23* | 0.24 | 0.23 | 0.24 | 0.22 |
| Drinks milk with snacks and meals | 0.32 | 0.25* | 0.24 | 0.26 | 0.26 | 0.25 |
| Child BMI at age 2 | 17.3 | 17.7* | 17.3 | 17.8* | 17.8 | 17.7 |
| Unweighted sample sizec | 2200 | 1850 | 500 | 1300 | 750 | 600 |
Note. HS = Head Start; TANF = Temporary Assistance for Needy Families; WIC = Supplemental Feeding Program for Women, Infants and Children; CACFP = Child and Adult Care Food Program; BMI = Body Mass Index; HH=Household.
Family incomes less than 185% of federal poverty line or participates in TANF or Food Stamps.
Refers to or from Head Start or Early Head Start.
Sample size rounded to the nearest 50 per ECLS-B license agreement.
Check-ups for well-child care only.
Family income divided by the federal poverty threshold specific to the family size and age composition (number of adults and number of children).
p<0.05, for test of equal means (or proportion) in the corresponding “yes” and “no” column.
Table 2.
Effects of CACFP on Nutrition-Related Outcomes: Propensity Score Weighted Logistic Regressions 4-Year-Olds in Centers Odds Ratio (95% CI) [Difference in Predicted Probabilitya]
| Mean of Outcome, Low-Income Non-Participants (1) | Sample |
|||
|---|---|---|---|---|
| Outcome | All Incomes (2) | Low-Incomeb (3) | Low-Income Not in Head Startb (4) | |
| Healthy food intake | ||||
| Milk, 2+ cup/day | 0.66 | 1.23+ (0.97, 1.57) [0.04] | 1.39* (1.03, 1.89) [0.06] | 1.41+ (0.99, 2.01) [0.07] |
| Fruits or juice, 3+ servings/day | 0.54 | 1.18 (0.95, 1.48) [0.04] | 1.20 (0.90, 1.60) [0.04] | 1.08 (0.78, 1.49) [0.02] |
| Vegetables, 2+ servings/day | 0.38 | 1.60* (1.27, 2.02) [0.11] | 1.58* (1.15, 2.14) [0.11] | 1.48* (1.04, 2.11) [0.09] |
| Avoidance of less healthy foods | ||||
| Salty snacks, <= 1–3 servings/wk | 0.55 | 1.11 (0.88, 1.40) [0.03] | 1.16 (0.85, 1.58) [0.04] | 1.29 (0.92, 1.81) [0.06] |
| Fast food, <= 1–3 servings/wk | 0.90 | 1.00 (0.73, 1.37) [−0.00] | 0.92 (0.63, 1.35) [−0.01] | 1.04 (0.67, 1.63) [0.00] |
| Sweet snacks, <= 1–3 servings/wk | 0.41 | 0.90 (0.71, 1.14) [−0.03] | 0.96 (0.70, 1.32) [−0.01] | 0.96 (0.68, 1.34) [−0.01] |
| Soda, <= 1-3 servings/wk | 0.61 | 0.78+ (0.61, 1.00) [−0.05] | 0.77+ (0.56, 1.05) [−0.06] | 0.85 (0.59, 1.22) [−0.04] |
| Weight-for-height | ||||
| Underweight | 0.03 | 0.51* (0.26, 0.97) [−0.003] | 0.54 (0.24, 1.21) [−0.002] | 0.41+ (0.15, 1.11) [−0.003] |
| Overweight | 0.23 | 0.83 (0.60, 1.15) [−0.02] | 0.79 (0.54, 1.17) [−0.03] | 0.64+ (0.41, 1.00) [−0.06] |
| Overweight/at-risk of overweight | 0.37 | 1.08 (0.82, 1.43) [0.02] | 1.03 (0.73, 1.46) [0.01] | 1.01 (0.69, 1.48) [0.00] |
| Food insecure | ||||
| Household | 0.34 | 0.95 (0.70, 1.30) [−0.00] | 0.85 (0.62, 1.16) [−0.04] | 0.84 (0.58, 1.21) [−0.04] |
| Children | 0.19 | 1.02 (0.73, 1.43) [0.00] | 0.98 (0.70, 1.36) [−0.00] | 1.02 (0.68, 1.51) [0.00] |
| Unweighted sample sizec | 500 | 4050 | 1750 | 1200 |
p < 0.05; + 0.05< p <0.10 from two-sided tests.
HS = Head Start.
Probabilities predicted at covariate means.
Low-income is family income <185% of the federal poverty line or family participates in Food Stamps/SNAP or TANF.
Rounded to the nearest 50 per the ECLS-B license agreement, after imputation of missing data for covariates. See text for details of multiple imputation procedures.
Controls: In addition to those listed in Table 1, covariates include child's age (in months), gender, presence of other children in the household (dummy variables for presence of other children under age 6 and other children aged 6–18), region of residence, and parent sampling weight. For the sample that does not include Head Start centers (Column 4) only, we also include a control for whether the center had a referral relationship with Head Start.
Low-income children were defined to correspond to income and categorical eligibility for full meal reimbursement from CACFP as those (1) who had family incomes less than 185% of the federal poverty line (for a family of their size) or (2) whose family had participated in the federal TANF or Food Stamps/SNAP program since the previous interview. The low-income sample consisted of 1,800 of the 4,050 observations.
Measures
The ECLS-B collected information through interviews with parents and caregivers and through direct assessments of children.
Dependent variables
We examined three categories of outcomes: food intake; weight-for-height; and food insecurity.
Food intake
At the four-year follow-up, the mother reported the frequency with which the child consumed specified foods over the seven days prior to the interview. The child's mother was instructed to think about all the meals and snacks the child had from the time she got up until the time she went to bed. Specifically, mothers were asked: “During the past seven days, how many times did your child drink (or eat) [item]?” Possible responses are: one time per day, two times per day, three times per day, four to six times per day, one to three times during the past seven days, four to six times during the past seven days, or the child did not drink (or eat) [item] during the past seven days. Mothers were further asked to “be sure to include food {CHILD} ate at home, preschool, restaurants, play dates, anywhere else, and over the weekend.” Limitations on a parent's ability to know what the child ate when not in her presence or to recall a child's food and beverage consumption over a seven-day period are a weakness of the present study.
We created dichotomous indicators of the child's intake of several types of food using cutoffs that correspond roughly to the CACFP meal guidelines and other nutritional guidelines (American Heart Association, n.d.). (We present the full distributions across response categories in supplementary tables available on-line.) The indicators were the following: drinking two or more cups of milk per day; having: two or more servings of vegetables per day; three or more servings per day of fruits or of 100% fruit juice; one to three or fewer servings per week of salty snacks; one to three or fewer servings per week of sweet snacks; one to three or fewer servings per week of soda; and one to three or fewer servings per week of fast food. The questions related to juice consumption instructed mothers to include 100% fruit juice, and to not include “punch, Sunny Delight, Kool-Aid, sport drinks or other fruit-flavored drinks.” Instead, mothers were asked to include these fruit-flavored drinks with their reports about the child drinking soda. For vegetables, the mother was asked to exclude French fries and other fried potatoes, but to “include vegetables like those served in a stir-fry, soup, or stew.” Food frequency questions have been used in numerous studies to compare dietary intake of individuals, including in longitudinal studies (such as the ECLS-B), where, due to low respondent burden, they are the “dietary assessment method of first choice” (Boushey, 2006, p. 53). Reliability studies have found substantial measurement error in all dietary assessment methods, including assessments of young children in low-income populations based on maternal responses to food frequency questions (Boushey, 2006; Klohe et al., 2005). Because the ECLS-B does not have alternative measures of food intake, we could not directly assess the reliability of the mother reports in our data; we must assume that reporting errors are not correlated with CACFP participation.
Weight-for-height
Children's heights and weights were measured by interviewers with a stadiometer and digital bathroom scale. ECLS-B data collectors were trained in the appropriate use of these instruments, and the recorded height and weight is the average of two measures Snow et al., 2007). Specifically, a trainer demonstrated how to use each measurement tool and how to record measurements. Trainees received video instruction and two hours of hands-on practice.
We computed the child's body mass index (BMI) and then classified the child as underweight (less than the 5th percentile), overweight (greater than or equal to the 95th percentile) and overweight or at risk of overweight (85th percentile or above) based on CDC Growth Charts appropriate for the child's age (Center for Disease Control and Prevention, 2000).
Food insecurity
Parents reported food insecurity for the family as a whole and specific to children using the 18-item Current Population Survey-Food Security Scale (CPS-FSS; Nord et al. 2009). Because few mothers endorsed any specific aspect of food insecurity (e.g., whether children's meals were reduced in size, children skipped a meal or went hungry, or did not eat a balanced meal), we created a dichotomous indicator for whether the mother endorsed any of the eight food insecurity items about the children in the household or eighteen items for the entire household (the eight child items and 10 additional items such as whether adults cut the size of meals or skipped meals, or the household could not afford to eat balanced meals).
CACFP and Head Start participation
CACFP participation was constructed from the center director's response to the question: Do you currently receive reimbursement from the United States Department of Agriculture (USDA) for meals or snacks served to children in your {center/program}? We coded the small fraction (under five percent) of centers that did not serve meals or snacks as nonparticipants in CACFP. We classified centers as Head Start centers if the director responded affirmatively to the question: Is your center a Head Start center?
Control variables
We controlled for numerous child, family, and center characteristics that might be associated both with CACFP participation and child outcomes. All of the time-varying characteristics were measured at the 4-year interview except for lagged child outcomes.
Child characteristics
Child characteristics included gender, race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic other and non-Hispanic White), whether the child was born low birth weight, whether the child was ever breast fed, the number of well-child doctor visits (zero or one versus two or more) since the two-year-old interview, whether the family had rules about food the child may eat, as well as the child's age in months (ranging from 45 to 64 months).
Family demographics
Characteristics of the mother included her age in years, education (less than high school graduate; high school graduate, no college; some college, but no four-year degree, and college graduate or higher), employment status (full-time, part-time, or not employed), whether the home language is English and whether the mother was born outside of the U.S., presence of other children in the household (under age six and aged six to 18), and poverty rate among young children (under age six) in the child's ZIP code of residence, family income (the “income/needs ratio,” defined as family income divided by the poverty threshold specific to the family's size and age composition). We also adjusted for the ECLS-B sampling weight from the four-year follow up and included dummy indicators for region of residence (Northeast, Midwest, West, or South).
Center characteristics
Center controls included accreditation status, whether or not the center is sponsored (by a church, school or some other organization), licensed status, and if licensed, licensed capacity, the director's years of experience at the center, and whether the center accepts children from or refers children to Head Start or Early Head Start.
Lagged child outcomes
At age two, the mother report of food intake did not include all of the food categories reported at age four; thus, we dummy-coded whether the mother reported that the two-year-old child drank milk at: both meals and snacks, meals only, snacks only, or neither. We used the child's measured height and weight to calculate the child's Body Mass Index (BMI) at age two. And, we included measures of household and child food insecurity when the child was two-years-old, based on the same scale as used at the four-year follow up, with two dummy variables: any food insecurity for both the household and the children, and any food insecurity for the household but not the children, versus the reference category of no food insecurity.
Results
Descriptive Analysis
We calculated means and proportions for our outcomes, key predictors, and control variables within six subgroups of four-year-old children in centers: (1) full sample, attending a non-CACFP center, (2) full sample, attending a CACFP center, (3) low-income subsample, attending a non-CACFP center, (4) low-income subsample, attending a CACFP center, (5) low-income CACFP subsample, attending a non-Head Start center, and (6) low-income CACFP subsample, attending a Head Start center. We conducted chi-square tests (for categorical variables) or t-tests (for continuous variables) to compare CACFP participants and nonparticipants in the full sample (the first versus the second group) and the low-income subsample (the third versus the fourth group), and to compare Head Start participants and nonparticipants among low-income CACFP participants (the fifth versus the sixth group). We weighted all of these descriptive statistics and bivariate hypothesis tests by the ECLS-B sampling weights.
Table 1 presents these descriptive statistics, with the six columns corresponding to the six groups just described. An asterisk attached to an entry in the “yes” column indicates a statistically significant difference from the entry in the corresponding “no” column (column 2 versus column 1; column 4 versus column 3; column 6 versus column 5). We have grouped the variables into six panels for ease of reference and presentation. The first panel presents means of children's nutrition-related outcomes at age 4. The second through sixth panels correspond, respectively, to five groupings of covariates: child characteristics, family income and neighborhood poverty, mother characteristics, center characteristics, and “lagged” child outcomes measured at age two.
We focus first on the results for the full sample (columns 1 and 2). The simple descriptive statistics for the outcomes (unadjusted for covariates) presented in the first panel indicate that nonparticipants in CACFP have generally, but not uniformly, better nutrition-related outcomes than participants. Without adjusting for measured characteristics, CACFP participants are less likely than nonparticipants to limit consumption of sodas and fast food, though they are more likely to consume the recommended number of servings of milk, fruit or juices and vegetables, and more likely to limit consumption of sweet snacks. CACFP participants are also four to six percentage points more likely to be overweight or at-risk of overweight than nonparticipants. Participants and their families are much more likely to be food insecure than nonparticipants: for example, children are food insecure in 20% of participant households versus 4% of nonparticipant households.
These nutrition-related disadvantages reflect, at least in part, participants' substantial socioeconomic disadvantages. In fact, differences in nutrition-related outcomes were already evident at age two, before most children have entered center care (see the sixth panel at the bottom of Table 1). Compared to nonparticipants at age four, children who participated in CACFP at age four were more likely at age two to have lived in a household in which children were food insecure (13% versus 4%), and they also had higher BMIs on average (17.7 versus 17.3).
CACFP participants' socioeconomic disadvantages are also evident from figures presented in the second and third panels of Table 1. Participating children are more likely to be racially identified as Hispanic or non-Hispanic Black, to have been born low birth weight, and less likely to have been breastfed. They have much lower incomes on average than nonparticipants (an income-to-needs ratio of 1.83 versus 4.36), and to have recently participated in other means-tested assistance programs such as TANF, Food Stamps/SNAP, or WIC (third panel). They also live in much poorer neighborhoods; the average poverty rate for young children under five in their ZIP codes of residence is 22.7 percent compared to 12.2 percent among CACFP nonparticipants. And, as is evident from figures presented in the fourth panel of Table 1, mothers of participating children are younger, less educated, and less likely to be married than mothers of non-participating children. Participants' mothers are also more likely to work full-time, which has been associated with overweight among children (Anderson & Butcher, 2006).
CACFP participants and nonparticipants are cared for in centers with markedly different characteristics (fifth panel). Participants' centers are more likely to be Head Start programs, which is not surprising given the requirement to participate in CACFP for Head Start centers. Participants' centers are more likely to be sponsored by a church, school, or other organization, and to be accredited, licensed, and licensed to care for a large number of children: an average licensed size of 122 at centers attended by participating children, compared to just 79 among those attended by non-participating children.
A simple strategy to increase the comparability of participants and nonparticipants is to focus on low-income children (those with family incomes below 185% of the federal poverty line or who recently participated in TANF or SNAP), which we do in the third and fourth columns of the table. Although limiting the sample to low-income children narrows differences in socioeconomic status between CACFP participants and nonparticipants, even among low-income children, participants (column 4) are disadvantaged relative to nonparticipants (column 3). For example, low-income participants are more likely than nonparticipants to be Hispanic or Black, less likely to have been breastfed, and they have lower family incomes (income-to-needs ratio of 1.00 on average versus 1.19 among nonparticipants), live in poorer neighborhoods, and are more likely to participate in other public assistance programs. Among low-income families, mothers of CACFP-participating children are less educated and less likely to be married, although differences between participants and nonparticipants are considerably smaller in the low-income sample than in the full sample.
Given the sizable remaining disadvantages in the background of CACFP participants, it is perhaps surprising that simple differences in outcomes between low-income participants and nonparticipants are modest and sometimes favor participants (first panel of Table 1). As in the full sample, low-income participants are more likely than low-income nonparticipants to consume the recommended servings of milk, but four to five percentage points less likely to limit fast food or soda consumption and more likely to be food insecure. Low-income CACFP participants are no more likely to be overweight than low-income nonparticipants, in contrast to the full sample results, where participants were four percentage points more likely to be overweight than non-participants.
Our final comparison is between low-income CACFP participants who do and do not participate in Head Start (the sixth and fifth columns, respectively). This comparison helps us to judge the likely influence of combining Head Start participants with other CACFP participants in estimating the impact of CACFP (since we are unable to control for Head Start because all Head Start children participate in CACFP). These results show clearly that children in Head Start are disadvantaged in family background (income, participation in other assistance programs, maternal education) compared to other low-income CACFP participants. Since disadvantaged backgrounds are generally associated with worse nutritional outcomes and a higher risk of food insecurity, lumping Head Start participants with other CACFP participants is likely to downwardly-bias estimates of CACFP program effects (i.e., understate beneficial effects or overstate adverse effects).
In sum, descriptive statistics clearly indicate the selective nature of participation in CACFP, including among low-income children. Children who participate are more disadvantaged than those who do not. These results, therefore, underscore the importance of controlling for family background and center characteristics in estimating associations between participation in CACFP and nutrition-related outcomes. Limiting the sample to low-income children increased the comparability of participants and nonparticipants, and narrowed, eliminated, or reversed differences in outcomes. However, even among low-income children, participants are disadvantaged in income and maternal education, and their centers differ in licensure status, accreditation, and size. Thus, the descriptive comparisons demonstrate the need for the propensity-score-weighted regression models that we present next to adjust simultaneously for the effects of many potential confounders.
Propensity Score Weighted Regression Analysis
We used propensity-score-weighted regressions to estimate covariate adjusted, associations between CACFP participation and nutritional outcomes. Table 2 presents these results. Each cell of this table represents an estimate of the effect of CACFP from a separate logistic regression. The measures of food intake are coded such that we expect positive values if participation in CACFP is beneficial: a higher proportion of children consuming two to three (or more) servings of healthy foods each day; a higher proportion of children consuming one to three (or fewer) servings of unhealthy foods each day. The weight-for-height and food insecurity variables are coded such that we expect negative values if participation in CACFP is beneficial (less underweight, less overweight, and lower food insecurity). The regression models include the extensive set of controls for child, family, and center characteristics listed in Table 1 and described in the Methods section, including lagged values of: milk consumption, BMI, and food insecurity measured at age two. The propensity-weighted descriptive statistics, the full set of coefficients from these regressions, and the models predicting participation in CACFP that are used in propensity score weighting are included in on-line supplementary material.
We estimate the effect of CACFP for all four-year-old children (column 2 of Table 2), or all low-income four-year-old children (column 3 of Table 2). As noted, to examine the possibility that the estimated effects of CACFP participation may partly capture effects of Head Start, in column 4 of Table 2 we report estimates for a sample of low-income children who do not participate in Head Start. To aid in the interpretation of effect magnitudes, in column 1 of Table 2 we present the mean of each of the outcome variables among low-income children who did not participate in CACFP.
For each estimate, we report three values: the estimate of the odds ratio, the 95% confidence interval of the odds ratio (in parentheses), and the difference between CACFP participants and non-participants in the model's predicted probability that the outcome occurs (in square brackets). For example, the first entry in column 3 of Table 2 is 1.39, which indicates that CACFP increases the odds that a low-income child will consume two or more cups of milk per day by nearly forty percent. The confidence interval for the odds ratio is 1.03 to 1.89; since the confidence interval does not contain one, the estimate is statistically significant at the 5% level (indicated in the table by an asterisk). The figure in brackets, 0.06, is the difference in the probability of drinking two or more cups of milk each day between participants and non-participants in CACFP. One way to gauge the magnitude of this effect is to compare it to milk consumption for a comparison group; therefore, we report the means of outcomes for low-income children who do not participate in CACFP in column 1 of Table 2. Since 66% of low-income children who do not participate in CACFP consume two or more cups of milk per day, and since CACFP is estimated to increase this proportion by six percentage points, we conclude that the effect is of moderate size: CACFP increases this proportion by nine percent (0.06/0.66).
Although some children whose families do not have low incomes attend centers that participate in CACFP, we focus our discussion on low-income children who are the primary targets for program benefits. For low-income children (the second and third columns of Table 2), the estimates indicate that, after we adjust for measured differences between participants and non-participants using propensity score weighting, attending a CACFP-participating center is associated with increased probabilities of recommended intake of milk (six to seven percentage points), fruit or fruit juice (two to four percentage points) and vegetables (9 to 11 percentage points), though the estimate for fruit/juice consumption is not statistically significant (the p-value for a two-sided test is 0.20 for the low-income sample). These effects are moderate in size since nearly two-thirds of non-participating low-income children consume the recommend number of servings of milk, about one-half consume the recommended amount of fruit or juice, and about one-third consume the recommended amount of vegetables (see column 1).
As for limiting intake of less healthy foods, the results are mixed and inconsistent. Low-income children in CACFP-participating centers are more likely to limit consumption of salty snacks and less likely to limit consumption of soda, though these effects are modest in size and only the soda effect is significant at the p<.10 level for low-income children (but is insignificant if Head Start enrollees are dropped from the sample). There is no evidence that CACFP participation is associated with consumption of either “fast food” or sweets.
In terms of weight and food insecurity, CACFP participation is associated with reduced likelihood of being underweight among low-income children, a difference that is statistically significant in the low-income non-Head Start subsample, but is of too small magnitude to be substantively important (less than one-half percentage point). CACFP participation is associated with reduced risk of overweight (three to six percentage points), a difference that is statistically significant at the p<.10 level and moderately sizable for the low-income non-Head Start sample (the six percentage point effect represents a reduction of one-quarter in the risk of overweight). Participation in CACFP is also associated with a four percentage point reduction in household (but not child) food insecurity among low-income families, but the effect is not statistically significant in any sample.
The results discussed above suggest that grouping Head Start children with other CACFP participants (as in the models summarized in the second and third columns), generally does not lead to overstated associations of CACFP with beneficial nutritional outcomes. Instead, the results suggest that dropping them from the low-income sample may reduce selection bias owing to the disadvantages of children in Head Start compared to other low-income children. Specifically, when we omitted the Head Start children from the low-income sample (column 4), the effects of CACFP on milk and vegetable intake remain statistically significant and similar in magnitude to the corresponding estimates for all low-income children (column 3). The beneficial effects of CACFP on reducing underweight and overweight become slightly larger and statistically significant.
In summary, among lower-income four-year-olds, attending a CACFP-participating center is associated with greater consumption of milk and vegetables. According to measured height and weight, low-income children in CACFP-participating centers are no more likely to be overweight and, in fact, are slightly less likely to be either underweight or overweight than similar children at non-participating centers. CACFP may also reduce the risk of food insecurity for families of children attending CACFP-participating centers, though the estimates of effects of CACFP on food security are not statistically significant.
Discussion
To our knowledge, this is the first study to provide estimates of associations between CACFP participation and children's nutrition-related outcomes for a national sample. In a sample of low-income four-year-olds cared for in centers, CACFP participation is associated with increased consumption of milk and vegetables, and does not increase (and may reduce) the chance that a child is overweight. There is also evidence that CACFP participation is associated with reduced prevalence of underweight, but, because the prevalence of underweight in our sample is very low, the effect is small and not substantively meaningful. Finally, there is some evidence that CACFP participation is associated with a moderate, four percentage point, reduction in food insecurity among low-income households, though, this effect does not reach statistical significance. There is little consistent evidence for an effect of CACFP on consumption of less-nutritious foods.
These associations were obtained from propensity-score-weighted regression models that included extensive controls for child, family, and provider characteristics, including child outcomes measured at two-years-old (BMI, milk consumption, and food insecurity). Although propensity score methods help to make participants and nonparticipants more comparable, they do not eliminate bias from selection into the program on unmeasured characteristics related to nutritional outcomes. Including outcomes measured at age two as controls in models of outcomes at age four is intended to reduce this type of selectivity bias, but whether that is sufficient to eliminate bias is unknown. The restriction of the sample to four year olds in child care centers means that results presented here may not generalize to children of other ages or cared for in other settings. Basing dietary quality outcomes on seven-day parental recall rather than direct observation of feeding practices is another limitation.
Despite these limitations, our findings are important, especially given the paucity of prior research comparing CACFP participants to non-participants. Our estimates provide the first national evidence that this growing program can improve nutritional outcomes of children in child care. Future studies are needed to confirm this finding and to identify mechanisms through which the program may produce benefits. For example, studies that explore the link between children's outcomes and the extent to which providers serve food that follows USDA guidelines and children eat served foods would be particularly valuable. This will require studies that combine designs like the ECLS-B (longitudinal, population-based samples including measures of child outcomes) with the kinds of intensives studies that have been conducted in small, localized samples of CACFP participants that have gathered menus and observed meals and snack times (e.g., Bruening et al., 1999; Erinosho et al., 2011; Oakley et al. 1995). Studies that also experimentally assign providers to CACFP participation would be even more informative, allowing researchers to observe how menus and meals and snacks consumed change after random assignment and link such changes in practices to changes in child outcomes. In the ECLS-B data, we also do not know the extent to which providers use the food subsidy to improve the quantity and quality of food served rather than reduce the price of care to parents, increase provider compensation, or improve program quality in other areas. Future studies might gather information about provider expenditures, again ideally before and after program adoption, so that expenditure changes can be associated with child outcomes.
The importance of our finding of apparent program benefits is underscored by our earlier research that demonstrated that the CACFP fails to reach substantial portions of poor children who are most likely at risk of being food insecure and of having poor nutritional outcomes. Estimates based on the ECLS-B indicate that only eight percent of low-income two-year-olds and 37% of low-income four-year-olds received CACFP (Gordon et al., 2011). Low receipt of CACFP is partly the result of program rules about eligibility, since 77% of low-income two-year-olds and 48% of low-income four-year-olds were cared for in settings that are not eligible for CACFP reimbursement in most states (in exclusive parental care or in a license-exempt day care home).
While our estimates suggest that low-income children benefit from the program, the benefits of extension of the program to include more low-income children will come at some cost to taxpayers. Given the tight budgetary situation that federal discretionary programs face in the years ahead, it is worth considering whether the costs of serving more low-income children might be financed though better targeting of CACFP expenditures. In particular, a substantial proportion of children who receive CACFP are not from low-income families, but are cared for in centers (and other settings) that participate. It would be worth exploring ways to enroll more low-income children through re-focusing expenditures on them and their providers. Steps were taken in this direction in 1996 with the introduction of “tiered” reimbursement levels for family day care homes. Similarly “tiering” reimbursement for centers may be necessary to bring more low-income children into the program under difficult fiscal circumstances. In addition, for-profit centers are currently eligible to participate in CACFP only if at least one-quarter of the children in their care are from low-income families. Extending this eligibility criterion to non-profit centers could also be used to improve the targeting of CACFP benefits to low-income children.
Congress has indicated support for research related to the CACFP and advancing its role in promoting good nutrition and health in the Healthy, Hunger-Free Kids Act of 2010 (PL-111-296). The Act requires State and local cooperation with USDA research and evaluation of the CACFP and other nutritional assistance programs. Further, it raises the prominence of child care generally, and the CACFP in particular, in early childhood nutrition and health. Notably, Title II of the Act, “Reducing Childhood Obesity and Improving the Diets of Children,” includes as Subtitle B: “The Child and Adult Care Food Program.” Under this subtitle, Section 223 provides five million dollars to USDA to conduct a nationally representative study of child care settings to determine the nutritional quality of foods provided, the opportunities for physical exercise, the extent of sedentary activity, and also to identify “barriers and facilitators” of participation in the CACFP and nutritional and wellness quality. This study, and the requirement of State and local cooperation in research and evaluation, provides an unprecedented opportunity for USDA to advance understanding of the effects of the CACFP program on the nutritional health of low-income children.
In summary, as far as we are aware, our study is the first with a sizable, national sample to provide evidence that low-income preschoolers who participate in the CACFP program consume healthier foods and have healthier weights than those who do not participate. It provides additional motivation for research into the mechanisms through which the program may have these effects and for future policy analyses to better target program benefits on poor children.
Supplementary Material
Highlights
There has been little research on the effects of the federal CACFP on children's weight, diet, and food insecurity.
This is the first large-scale evaluation of the effects of the CACFP to compare participants to similar nonparticipants.
Propensity-score regressions indicate CACFP participation among low-income preschoolers associates with moderate improvements in diet.
There is little evidence that CACFP increases overweight/obesity or consumption of less-healthy foods.
Acknowledgments
The authors gratefully acknowledge funding from the USDA Nutrition Research Innovation and Development Grants in Economics (RIDGE) Program and by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, through Grant R01HD060711. The opinions expressed are those of the authors and do not represent views of the Institute or the USDA. This paper benefited from two RIDGE workshops held at the Irving B. Harris School of Public Policy Studies at the University of Chicago and the 2009 RIDGE Conference held in Washington DC. We also thank seminar participants at Chapin Hall at the University of Chicago and the School of Public Affairs, Baruch College/CUNY for their comments.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Dietetic Association Position of the American Dietetic Association: Benchmarks for nutrition programs in child care settings. Journal of the American Dietetic Association. 2005;105:979–986. doi: 10.1016/j.jada.2005.04.015. [DOI] [PubMed] [Google Scholar]
- American Heart Association . Milk products: AHA recommendation. Author; Dallas, TX: n.d. Retrieved from http://www.americanheart.org/presenter.jhtml?identifier=4684. [Google Scholar]
- Anderson PM, Butcher KF. Childhood obesity: Trends and potential causes. The Future of Children. 2006;16(1):19–45. doi: 10.1353/foc.2006.0001. doi: 10.1353/foc.2006.0001. [DOI] [PubMed] [Google Scholar]
- Aud S, Hussar W, Kena G, Bianco K, Frohlich L, Kemp J, Tahan K. U.S. Department of Education, National Center for Education Statistics. U.S. Government Printing Office; Washington, DC: 2011. The condition of education 2011 (NCES 2011-033) [Google Scholar]
- Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966–2007. Preventing Chronic Disease. 2009;6:1–10. [PMC free article] [PubMed] [Google Scholar]
- Boushey CJ. Nutritional epidemiology: Dietary assessment methods. In: Weaver CM, Heaney RP, editors. Calcium in human health. Human Health; Totowa, NJ: 2006. pp. 39–64. [Google Scholar]
- Briley M, McAllaster M. Nutrition and the child care setting. Journal of the American Dietetic Association. 2011;111:1298–1300. doi: 10.1016/j.jada.2011.06.012. [DOI] [PubMed] [Google Scholar]
- Bruening KS, Gilbride J, Passannante M, McClowry S. Dietary intake and health outcomes among young children attending 2 urban day-care centers. Journal of the American Dietetic Association. 1999;99:1529–35. doi: 10.1016/S0002-8223(99)00375-2. doi:10.1016/S0002-8223(99)00375-2. [DOI] [PubMed] [Google Scholar]
- Busso M, DiNardo J, McCrary J. New evidence on the finite sample properties of propensity score matching and reweighting estimators (Discussion Paper No. 3998) 2009 Retrieved from: ftp://ftp.iza.org/RePEc/Discussionpaper/dp3998.pdf.
- Center for Disease Control and Prevention . Growth charts. Author; Atlanta, GA: 2000. Retrieved from http://www.cdc.gov/growthcharts/ [Google Scholar]
- Crepinsek MK, Burstein NR, Lee EB, Kennedy SD, Hamilton WL. Meals offered by Tier II CACFP family child care providers: Effects of lower meal reimbursements (Food Assistance and Nutrition Research Program Report No. 02-006) U.S. Department of Agriculture, Economic Research Service; Washington, DC: 2002. [Google Scholar]
- Currie JM. The invisible safety net: Protecting the nation's poor children and families. Princeton University Press; Princeton, NJ: 2006. [Google Scholar]
- Erinosho T, Dixon B, Young C, Brottman LM, Hayman L. Nutrition practices and children's dietary intakes at 40 child-care centers in New York City. Journal of the American Dietetic Association. 2011;111:1391–1397. doi: 10.1016/j.jada.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Ferguson JL, Ready DD. Expanding notions of social reproduction: Grandparents' educational attainment and grandchildren's cognitive skills. Early Childhood Research Quarterly. 2011;26:216–226. [Google Scholar]
- Fleischhacker S, Cason KL, Achterberg C. `You had peas today?': A pilot study comparing a Head Start child-care center's menu with the actual food served. Journal of the American Dietetic Association. 2006;106(2):277–280. doi: 10.1016/j.jada.2005.10.038. doi: 10.1016/j.jada.2005.10.038. [DOI] [PubMed] [Google Scholar]
- Frisvold D, Lumeng J. Expanding exposure: Can increasing the daily duration of Head Start reduce childhood obesity? Journal of Human Resources. 2011;46(2):373–402. [Google Scholar]
- Glantz FB. Fox MK, Hamilton W, Lin BH, editors. Child and Adult Care Food Program. Effects of food assistance and nutrition programs on nutrition and health: Volume 3, literature review (Food Assistance and Nutrition Research Report no. FANRR 19-3) 2004:236–249. Retrieved from: http://www.ers.usda.gov/publications/fanrr19-3/fanrr19-3g.pdf.
- Gordon RA, Kaestner R, Korenman S, Abner K. The Child and Adult Care Food Program: Who is served and why? Social Service Review. 2011;85(3):359–400. [Google Scholar]
- Graham J, Olchowski A, Gilreath T. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention Science. 2007;8:206–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- Healthy Hunger-Free Kids Act of 2010, Pub. L. No. 111–296, § 4. Retrieved from: http://www.gpo.gov/fdsys/pkg/PLAW-111publ296/pdf/PLAW-111publ296.pdf.
- Hirano K, Imbens GW. Estimating of causal effects using propensity score weighting: Application to data on right heart catheterization. Health Services and Outcomes Research Methodology. 2002;2:259–278. [Google Scholar]
- Imbens GW, Wooldridge JM. Recent developments in the econometrics of program evaluation. Journal of Economic Literature. 2009;47(1):5–86. doi: 10.1257/jel.47.1.5. [Google Scholar]
- Johnson D. Two-wave panel analysis: Comparing statistical methods for studying the effects of transitions. Journal of Marriage and Family. 2005;67:1061–1075. [Google Scholar]
- Klohe DM, Clarke KK, George GC, Milani TJ, Hanss-Nuss H, Freeland-Graves J. Relative validity and reliability of a food frequency questionnaire for a triethnic population of 1-year-old to 3-year-old children from low-income families. Journal of the American Dietetic Association. 2005;105(5):727–734. doi: 10.1016/j.jada.2005.02.008. [DOI] [PubMed] [Google Scholar]
- Korn EL, Graubard BI. Analysis of large health surveys: Accounting for the sampling designs. Journal of the Royal Statistical Society A. 1995a;158:263–295. [Google Scholar]
- Korn EL, Graubard BI. Examples of differing weighted and unweighted estimates from a sample survey. The American Statistician. 1995b;49:291–295. [Google Scholar]
- Kuratko CN, Martin RE, Lan WY, Chappell JA, Ahmad M. Menu planning, food consumption, and sanitary practices in day care facilities. Family and Consumer Sciences Research Journal. 2000;29(1):81–91. doi: 10.1177/1077727X00291004. [Google Scholar]
- National Child Care Information Center, & National Association for Regulatory Administration . The 2007 Child Care Licensing Study. National Association for Regulatory Administration; Lexington, KY: 2009. Retrieved from http://www.naralicensing.org/associations/4734/files/2007%20Licensing%20Study_full_report.pdf. [Google Scholar]
- National Institute of Child Health and Human Development Early Child Care Research Network. Duncan GJ. Modeling the impacts of child care quality on children's preschool cognitive development. Child Development. 2003;74(5):1454–1475. doi: 10.1111/1467-8624.00617. [DOI] [PubMed] [Google Scholar]
- Nord M. Food insecurity in households with children: Prevalence, severity, and household characteristics (Economic Research Report No. 56) 2009 Retrieved from: http://www.ers.usda.gov/Publications/EIB56/EIB56.pdf.
- Nord M, Andrews M, Carlson S. Household food security in the United States, 2008 (Economic Research Report No. 83) U.S. Department of Agriculture, Economic Research Service; Washington, DC: 2009. [Google Scholar]
- Oakley CB, Bomba AK, Knight KB, Byrd SH. Evaluation of menus planned in Mississippi child-care centers participating in the Child and Adult Care Food Program. Journal of the American Dietetic Association. 1995;95(7):765–768. doi: 10.1016/S0002-8223(95)00213-8. doi: 10.1016/S0002-8223(95)00213-8. [DOI] [PubMed] [Google Scholar]
- Potter F, Grau E, Williams S, Diaz-Tena N, Lepidus Carlson B. An application of propensity modeling: Comparing unweighted and weighted logistic regression models for nonresponse adjustments. Paper presented at the Joint Statistical Meetings; Seattle, WA. 2006. Retrieved from: http://www.amstat.org/sections/srms/proceedings/y2006/Files/JSM2006-000801.pdf. [Google Scholar]
- Richard B. Russell National School Lunch Act of 2010, Pub. L. No. 111–296, § 4. Retrieved from: http://www.fns.usda.gov/cnd/governance/Legislation/NSLA_12-13-10.pdf.
- Rogers WH. Regression standard errors in clustered samples. Stata Technical Bulletin. 1993;13:19–23. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update of ice. The Stata Journal. 2005;5:527–536. [Google Scholar]
- Ryan RM, Johnson A, Rigby E, Brooks-Gunn J. The impact of child care subsidy use on child care quality. Early Childhood Research Quarterly. 2011;26:320–331. doi: 10.1016/j.ecresq.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow K, Thalji L, Derecho A, Wheeless S, Lennon J, Kinsey S, Park J. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Preschool Year data file user's manual (2005–06) (National Center for Education Statistics No. 2008–024.) U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics; Washington, DC: 2007. [Google Scholar]
- Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Future of Children. 2006;16:143–168. doi: 10.1353/foc.2006.0010. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Service . CACFP reimbursement rates for meals served in homes and centers. Author; Alexandria, VA: n.d. Retrieved from http://www.fns.usda.gov/CND/Care/ProgramBasics /Rates/2005HomesContig.htm and http://www.fns.usda.gov/CND/Care/ProgramBasics/Rates/2005CentersContig.htm. [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Service . Meal patterns. Author; Alexandria, VA: 2009. Retrieved from http://www.fns.usda.gov/CND/Care/Program Basics/Meals/Meal_Patterns.htm. [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Service . Final Rule: For-profit center participation in the CACFP (Federal Register 7 CFR Part 226) Author; Alexandria, VA: 2008. [Google Scholar]
- von Hippel PT. Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology. 2007;37:83–117. [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States: Gender, age, socioeconomic status, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Williamson E, Morley R, Lucas A, Carpenter J. Propensity scores: From naϊve enthusiasm to intuitive understanding. Statistical Methods in Medical Research. 2012;21(3):273–293. doi: 10.1177/0962280210394483. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM. Econometric analysis of cross-section and panel data. MIT Press; Cambridge, MA: 2002. [Google Scholar]
- Wooldridge JM. Cluster-sample methods in applied econometrics. 2006 Retrieved from: https://www.msu.edu/~ec/faculty/wooldridge/current research/clus1aea.pdf.
- Ziegler P, Briefel R, Ponza M, Novak T, Hendricks K. Nutrient intakes and food patterns of toddlers' lunches and snacks: Influence of location. Journal of the American Dietetic Association. 2006;106(1):S124–S134. doi: 10.1016/j.jada.2005.09.036. doi:10.1016/j.jada.2005.09.036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.