Abstract
In-hospital falls (IFs) increase morbidity, cost, and may result in litigation. We analyzed the Nationwide Inpatient Sample to quantify the incidence of IFs in patients who underwent hip and knee arthroplasty and to define trends, patient’s demographics, risk factors, complications, and hospital cost. Patients operated on between 1998 and 2007 were identified and grouped depending on the presence of a diagnosis of IF. Of those, 0.85% had an IF, representing 2.1 falls per 1000 inpatient days. The incidence of IF increased from 0.4% to 1.3% during the study period. Independent risk factors included revision surgery, advanced age, male sex, minority race, and the presence of comorbidities. Patients having IF had a longer hospital stay and were less likely to be discharged to their primary residence. In-hospital mortality, complications, and cost were higher in patients sustaining IF. Given the associated morbidity, mortality, and increased cost, resources should be allocated to minimize the risk of IF in this population.
Keywords: total joint anthroplasty, complications, in-patient falls, safety
In-hospital falls (IF) occur in 2% to 17% of patients during short-term hospitalization [1–3]. Of those, up to 50% of patients sustain a fall-related injury, with 1% to 10% classified as serious, including fractures and head injuries [4–14]. In our academic institution devoted to orthopedic surgery, 868 patients sustained at least 1 IF in the period between 2000 and 2009 [15].
Aside from their immediate impact on the patient, IF contributes additional burden to the health care system given the prolongation of hospitalization and the potential for litigation [16]. Accordingly, prevention of IF has become a patient safety goal that is evaluated during hospital accreditation in the United States [17].
Undergoing orthopedic surgery inherently limits patient mobility in the immediate postoperative period and places patients at increased risk for falls, but to our knowledge, only 2 studies evaluated the risk of falls during hospitalization after orthopedic surgeries [15, 18] with an incidence of approximately 1% of hospitalizations. Considering the substantial increase in primary and revision total joint arthroplasty (TJA) projected in the coming decades [19] and the potential cost burden associated with this potentially preventable nonsurgical complication, further analysis of the incidence and the risk factors associated with IF after surgery is needed to develop strategies that can minimize this risk.
In the current study, we have analyzed a large administrative-level database with the goals of quantifying the incidence, trends, and risk factors associated with IF after primary or revision TJA. Furthermore, the incidence of in-hospital postoperative complications and hospital cost were compared between patients who did and did not sustain an IF.
Materials and Methods
Nationwide Inpatient Sample (NIS) data files sponsored by the Agency for Healthcare Research and Quality (AHRQ) were obtained from the Hospital Cost and Utilization Project and analyzed for this study. The NIS represents the largest all-payer inpatient discharge database in the United States. The NIS provides weighting procedures to allow for the generation of nationally representative estimates from the collected data. Detailed information on the NIS design can be accessed electronically [20, 21]. A large number of studies addressing various aspects across the spectrum of medical specialties have been published [22]. The data used in this study were sufficiently deidentified. Accordingly, this project was exempted from institutional review.
Selection of Study Sample and Statistical Methods
Our study sample consists of all data in NIS for each year between 1998 and 2007. Entries indicating the performance of primary and revision total hip arthroplasty (THA) and total knee arthroplasty (TKA) were identified using the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) procedure codes 81.51, 81.53, 81.54, and 81.55, respectively. Patients with bilateral THA or TKA performed during the same hospitalization were excluded. Entries with a diagnosis for inpatient fall (IF) were identified by using ICD-9-CM diagnosis code E849.7 (accidents occurring in residential institution). By restricting our sample to routine admissions and nonemergent procedures only, we logically excluded patients who fell in another institutionalized setting other than the hospital where the procedure was performed.
The incidence of IF by procedure subtype, patient demographics (age, sex, and race), disposition status, primary source of payment, distribution of procedures by hospital size, teaching status, and location were evaluated. The incidence of IF by year was tabulated. In addition, we calculated the number of falls per 1000 inpatient days by dividing the total number of falls by the sum of hospitalization days and multiplying the result by 1000. Comorbidity profiles were analyzed by determining the prevalence of several disease states as defined in the Comorbidity Classification Software and provided by the AHRQ [23] among IF and non-IF entries. Frequencies of procedure-related complications were analyzed by determining cases that listed ICD-9-CM diagnosis codes specifying complications of surgical and medical care (ICD-9-CM 997.X-999.X). The ICD-9-CM code 996.X, which specifies device-related complications, was not included because this code is often used as the indication for revision procedures and may not indicate a perioperative complication. In addition, we studied the prevalence of selected adverse diagnoses, including pulmonary embolism, venous thrombosis, respiratory insufficiency after trauma or surgery/adult respiratory distress syndrome, acute posthemorrhagic anemia, and the use of blood product transfusion using the ICD-9-CM diagnosis code system. To determine overall comorbid burden, comorbidity indices were calculated as described by Charlson et al [24] and adjusted for use with administrative data by Deyo et al [25].
Approximately 30% of entries in the race category were not available and were imputed as “white.” This step was based on an approach previously described and on the fact that facilities with high rates of missing data for race served populations with higher than average white/black patient ratios [26, 27]. However, to study the potential impact of this step on results, we repeated the regression analysis while treating “missing” race as a separate category. No significant differences in results were found.
All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). To facilitate analysis of data collected in a complex survey design and to obtain consistent estimates of mean and variance parameters taking into account the complex survey data setting, SAS procedures SURVEYMEANS, SURVEYFREQ, and SURVEYLOGISTIC were used for descriptive analyses and modeling efforts.
A multivariate logistic regression model was built to identify risk factors associated with higher odds of IF. To fit a parsimonious model with strong predictive covariates only, we took the following steps [28]. First, clinical judgment and significance at P value of 15% level in univariate analyses were used to select variables for the process of multivariable modeling. Covariates in the full logistic model included procedure subtype, age, sex, race, hospital location and bed size, alcohol abuse, chronic pulmonary disease, congestive heart failure, diabetes, liver disease, coagulopathy, neurologic disease, peripheral vascular disease, renal failure, valvular disease, electrolyte/fluid disorder, cancer, and pulmonary circulatory disease. To account for changes in practice over time, 2-year periods were created and included as variables in the model. Second, further variable selection was achieved through a nonparametric bootstrapping process [29]. In the bootstrap procedure, each bootstrap sample of size n was randomly drawn with replacement from all of the original observations. The sample size of n was equal to the original observations. One hundred bootstrap samples were created, and a stepwise procedure was applied to each sample using forward selection method (with selection entry level = 0.20). From this analysis, we calculated the percentage of samples for which each variable was included in the model from the 100 samples. Percent inclusion was used to determine the prognostic importance of a variable because it was expected that a prognostically important variable would be included in the model for most bootstrap samples. A model was formulated that contained the variables with percent inclusion greater than 80% (cutoff decided a priori). The c-statistic was the same as the area under the receiver operating characteristic curve and was used to measure how well the model discriminates between observed data at different levels of the outcome. Third, the model finalized at the second stage was processed one more time using the SURVEYLOGISTIC procedure instead of the LOGISTIC procedure to be able to obtain appropriate estimates of the variance for the weighted survey data. This step was necessary because the SURVEYLOGISTIC does not allow for forward selection procedure [30].
Results
We identified 1 088 002 entries for THA and TKA in the NIS. This represents a national estimate of 5 313 680 hospitalizations between 1998 and 2007. Of those, 0.85% (9198/1 088 002 unweighted, 44932/5 313 680 weighted) had an IF. This represents 2.1 falls per 1000 inpatient days. Demographics of patient groups are shown in Table 1 (available online at www.arthroplastyjournal.org). However, we observed a substantial increase in the incidence of IF from 0.4% in 1998 to 1.3% in 2007 (Fig. 1).
Table 1.
Demographics of TJA Patients With and Without IF
| Demographics of TJA Patients With and Without IF
| |||||||
|---|---|---|---|---|---|---|---|
| No fall
|
Fall
|
P | |||||
| F | WF | (%) | F | WF | (%) | ||
| Discharges | 1 078 804 | 5 268 757 | 99.2 | 9198 | 44 932 | 0.8 | <.0001 |
| Surgery type | <.0001 | ||||||
| Primary hip | 330 128 | 1 613 639 | 30.6 | 2755 | 13 476 | 30.0 | |
| Primary knee | 668 015 | 3 259 890 | 61.9 | 5281 | 25 787 | 57.4 | |
| Revision hip | 40 586 | 198 923 | 3.8 | 610 | 2973 | 6.6 | |
| Revision knee | 40 075 | 196 305 | 3.7 | 552 | 2695 | 6.0 | |
| Age groups (y) | <.0001 | ||||||
| 0–44 | 42 032 | 204 999 | 3.9 | 299 | 1452 | 3.2 | |
| 45–64 | 383 526 | 1 871 661 | 35.5 | 2885 | 14 072 | 31.3 | |
| 65–74 | 358 384 | 1 749 292 | 33.2 | 2934 | 14 369 | 32.0 | |
| 75+ | 294 848 | 1 442 738 | 27.4 | 3080 | 15 039 | 33.5 | |
| Sex | .03 | ||||||
| Male | 415 945 | 2 030 345 | 38.5 | 3646 | 17 829 | 39.7 | |
| Female | 662 793 | 3 238 090 | 61.5 | 5551 | 27 099 | 60.3 | |
| Race | .07 | ||||||
| White | 983 737 | 4 810 167 | 91.3 | 8350 | 40 788 | 90.8 | |
| Black | 51 224 | 247 866 | 4.7 | 459 | 2283 | 5.1 | |
| Hispanic | 24 547 | 116 545 | 2.2 | 237 | 1118 | 2.5 | |
| Other | 19 296 | 94 178 | 1.8 | 152 | 742 | 1.7 | |
| Insurance | <.0001 | ||||||
| Medicare | 633 356 | 3 094 112 | 58.9 | 5766 | 28 272 | 63.0 | |
| Medicaid | 27 866 | 136 913 | 2.6 | 239 | 1189 | 2.6 | |
| Private/HMO | 379 257 | 1 851 071 | 35.2 | 2875 | 13 937 | 31.0 | |
| Other | 36 059 | 175 460 | 3.3 | 309 | 1490 | 3.3 | |
| Hospital size | <.0001 | ||||||
| Small | 163 722 | 749 589 | 14.2 | 1523 | 7132 | 15.9 | |
| Medium | 270 612 | 1 312 353 | 24.9 | 2521 | 12 336 | 27.5 | |
| Large | 643 798 | 3 203 638 | 60.8 | 5145 | 25 420 | 56.6 | |
| Hospital location | .03 | ||||||
| Rural | 143 161 | 722 089 | 13.7 | 1302 | 6523 | 14.5 | |
| Urban | 934 971 | 4 543 491 | 86.3 | 7887 | 38 366 | 85.5 | |
| Teaching status | .003 | ||||||
| Nonteaching | 596 485 | 2 876 678 | 54.6 | 5239 | 25 218 | 56.2 | |
| Teaching | 481 647 | 2 388 902 | 45.4 | 3950 | 19 670 | 43.8 | |
F indicates frequency; WF, weighted frequency; HMO, health maintenance organization.
Fig. 1.
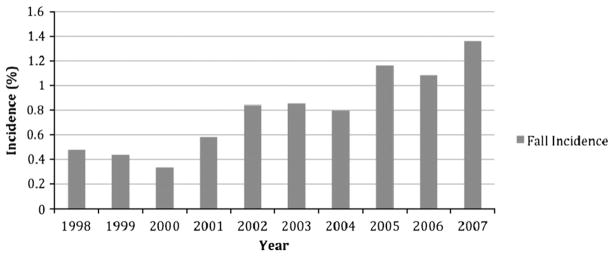
The annual incidence of in-patient falls during the study period.
On average, patients affected by an IF were older compared with non-IF hospitalizations (68.2 [confidence interval {CI}, 68.0–68.4] vs 66.6 [CI, 66.5–66.6] years, P < .0001) and thus, more frequently, were Medicare enrollees (63.0% vs 58.9%, respectively [P < .0001]). The incidence of IF was more frequent in small vs large and rural vs urban hospitals (P < .0001 and P = .03, respectively). Furthermore, male patients and those operated on in nonteaching hospitals had higher rates of IF (P = .03 and P = .003, respectively) (Table 1; available online at www.arthroplastyjournal.org).
Patients who had IF had significantly higher Deyo comorbidity scores (0.559 [CI, 0.541–0.577]) than those who did not have IF (0.531 [CI, 0.530–0.533], P < .0001), suggesting higher overall comorbidity burden. Comorbidities with a higher prevalence among patients having IF included congestive heart failure, coagulopathy, liver disease, neurologic disease, pulmonary circulatory disease, electrolyte/fluid abnormalities, and recent weight loss. No differences in the prevalence of obesity, hypothyroidism, uncomplicated diabetes, and cancer were seen (Fig. 2).
Fig. 2.
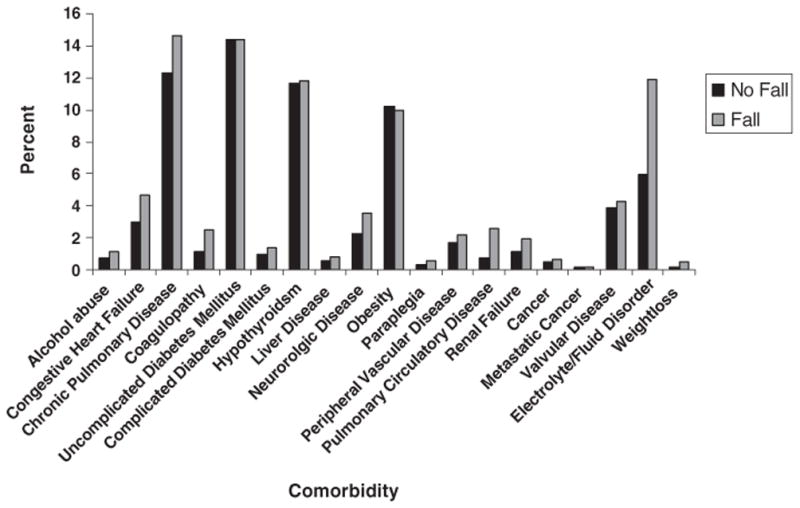
Prevalence of comorbidities amongst patients with and without in-patient falls.
In the multivariate regression analysis, independent risk factors for IF included revision vs primary procedures, with revision THA carrying the highest risk. Advanced age also increased the odds for IF as did male sex and minority race. Furthermore, more recent periods were also associated with higher odds for IF. Among comorbidities, pulmonary circulatory disease had the highest odds for IF (odds ratio, 3.17 [CI, 1.76–3.63]) (Table 2). The c-statistic to predict the power to distinguish presence or absence of IF was 0.64.
Table 2.
Risk Factors for IF—Regression Analysis
| Risk factors for Inpatient Fall—Multivariate Regression
| |||||
|---|---|---|---|---|---|
| Effect | Odds Ratio | 95% Confidence Limits | P | ||
| Procedure type (reference: revision TKA) | Primary THA | 0.52 | 0.47 | 0.57 | <.0001 |
| Revision THA | 1.11 | 0.99 | 1.25 | .0884 | |
| Primary TKA | 0.47 | 0.43 | 0.52 | <.0001 | |
| Sex (reference: women) | Male | 1.07 | 1.03 | 1.12 | .0015 |
| Age group (reference: 45–64 y) | 0–44 years | 0.95 | 0.84 | 1.07 | .4090 |
| 65–74 years | 1.14 | 1.08 | 1.20 | <.0001 | |
| ≥75 years | 1.38 | 1.31 | 1.45 | <.0001 | |
| Race (reference: white) | Black | 1.13 | 1.02 | 1.24 | .0144 |
| Hispanic | 1.14 | 1.00 | 1.30 | .0471 | |
| Other | 0.91 | 0.78 | 1.08 | .2783 | |
| Hospital location (reference: urban) | Rural | 1.16 | 1.09 | 1.23 | <.0001 |
| Hospital size (reference: small) | Medium | 1.03 | 0.96 | 1.10 | .3914 |
| Large | 0.83 | 0.79 | 0.88 | <.0001 | |
| Comorbidity (reference: absence of disease) | Alcoholism | 1.42 | 1.17 | 1.74 | .0005 |
| Chronic lung disease | 1.11 | 1.05 | 1.18 | .0007 | |
| Congestive heart failure | 1.25 | 1.13 | 1.38 | <.0001 | |
| Coagulopathy | 1.68 | 1.46 | 1.92 | <.0001 | |
| Neurologic disease | 1.42 | 1.27 | 1.59 | <.0001 | |
| Electrolyte/fluid abnormalities | 1.81 | 1.69 | 1.93 | <.0001 | |
| Pulmonary circulatory disease | 3.17 | 2.66 | 3.50 | <.0001 | |
| Periods (reference: 1998–1999) | 2000–2001 | 1.03 | 0.93 | 1.14 | .6140 |
| 2002–2003 | 1.91 | 1.75 | 2.08 | <.0001 | |
| 2004–2005 | 2.23 | 2.04 | 2.42 | <.0001 | |
| 2006–2007 | 2.96 | 2.71 | 3.22 | <.0001 | |
The length of hospital stay was longer in IF patients compare with that of non-IF patients (5.02 [CI, 4.96–5.09] vs 4.03 [CI, 4.03–4.03], P < .001). Patients with the diagnosis of IF were less frequently discharged to their primary residence (17.6% vs 25.6%) and more frequently transferred to other health care facilities (52.1% vs 46.6%) or in need of home health care (29.6% vs 27.6%) (P < .0001). In hospital mortality was significantly higher in patients with the diagnosis of IF 0.7% vs 0.2% (P < .0001). Procedure-related complications were also more frequent among IF patients (51.2% vs 6.8%, P < .0001) (Table 3).
Table 3.
Procedure-Related Complications
| Procedure-Related Complications
| |||
|---|---|---|---|
| No Falls (%) | Falls (%) | P | |
| Organ-specific complications | |||
| CNS | 0.1 | 1.0 | <.0001 |
| Cardiac | 0.9 | 6.1 | <.0001 |
| Peripheral vascular | 0.2 | 1.2 | <.0001 |
| Respiratory | 0.8 | 6.0 | <.0001 |
| Gastrointestinal | 0.8 | 4.9 | <.0001 |
| Genitourinary | 0.8 | 5.9 | <.0001 |
| Other procedure-related complications | |||
| Shock | 0.0 | 0.2 | <.0001 |
| Hematoma/seroma | 1.0 | 10.2 | <.0001 |
| Puncture vessel/nerve | 0.1 | 0.7 | <.0001 |
| Wound dehiscence | 0.0 | 1.0 | <.0001 |
| Infection | 0.2 | 1.7 | <.0001 |
| Other | 1.6 | 11.3 | <.0001 |
| Medical complication | 0.1 | 1.2 | <.0001 |
Postoperative complications including deep venous thrombosis (2% vs 0.6%, P < .0001), adult respiratory distress syndrome (1% vs 0.3%, P < .0001), pulmonary embolism (2% vs 0.3%, P < .0001) were also more common among IF patients. Patients with IF had higher rates of acute blood loss anemia (29.1% vs 16.9%, P < .0001) and need for blood transfusions compared with the non-IF group (30.6% vs 20.9%, P < .0001).
The average hospital costs were higher for IF vs non-IF patients ($15 574 [CI, 15,397–15 751] vs $13 327 [CI, 13 313–13 340], P < .0001).
Discussion
In the current study, we described an increased incidence of IF after THA and TKA in the United States from 0.4% to 1.3% in the period 1998–2007. The average prevalence of IF was 0.8%, which represents 2.1 falls per 1000 inpatient days.
There is limited research on IF after orthopedic surgery [15, 18]. Patients who had IF were older and had a higher burden of comorbidity. Male sex and minority race were found to be associated with an increased risk of having an IF. Length of stay, discharge disposition, postoperative complications, and in-hospital mortality were all adversely affected in patients who had IF. In addition, average hospital costs were significantly higher in those patients who had IF.
Orthopedic surgery distinctly affects mobility in the immediate postoperative period, potentially predisposing patients to IF. The IFs are not uncommon among those hospitalized but have not been studied extensively in the context of orthopedic surgery. Ackerman et al [18] conducted a retrospective chart review of patients who had predominantly undergone primary or revision TJA. Of the 6912 orthopedic patients admitted during a 2-year period, 70 sustained an IF, representing a 1% incidence and a fall rate of 2.5 falls per 1000 musculoskeletal inpatient days. Most falls occurred during bathroom transfers. Similarly, in our institution, Mandl et al [15] reported on 868 patients sustaining at least a fall during the hospitalization for a different number of orthopedic procedures in the period 2000 to 2009. This represented 0.9% of all admission and 2 falls per 1000 inpatient days. The authors observed no association between body mass index, age, or sex and the development of a severe injury associated with the fall.
The previously mentioned rates are similar to the ones reported by us at a national level. We calculated a national fall rate of 2.1 falls per 1000 inpatient days and a 0.8% incidence of IF among 1 090 095 patients who underwent primary or revision TJA over a 10-year period. However, we have observed a concerning increase in the incidence of IF during our study period.
An IF may be a manifestation of frailty among those hospitalized after orthopedic surgery. The postoperative anemia that most TJA patients have and the frequent use of opioid medication may compound to the risk of falling during the hospital stay. There was a higher comorbidity burden and higher incidence of congestive heart failure, pulmonary circulatory disease, liver disease, neurologic disease, and coagulopathy in the IF cohort. Furthermore, the age was significantly higher in those that sustained IF, which is in agreement with previous studies in patients who have undergone orthopedic surgery [18] or are hospitalized for other reasons [31, 32]. Based on the results of our investigations, we believe that advanced age and the presence of systemic comorbidity are probably risk factors for inpatient falls among patients who undergo TJA.
In our investigation, revision THA was the surgery associated with the highest risk for IF. Both revision THA and TKA were associated with higher risks of IF than primary TJA, which is intuitive given the more extensive nature of revision arthroplasty. However, the mean length of stay of patients undergoing primary joint arthroplasty is lower than that of patients undergoing revision surgery [33, 34], thus diminishing the likelihood of capturing a postoperative fall. Our study showed that the consequences of IF are substantial from both individual and societal perspectives. The frailty among these individuals who have IF is reflected in the higher comorbidity burden and prevalence of individual co-morbid conditions. Patients who had IF had 16.8% higher hospital costs than those who did not have IF. As cost-containment becomes increasingly important in health care, it will be critical to evaluate the efficacy and cost-effectiveness of strategies to prevent IF.
This investigation carries several limitations. The most notable ones are those associated with the use of administrative-level data. In particular, inaccuracy in the coding of diagnoses could potentially lead to under-reporting of IF. In addition, the NIS data did not include details that would be helpful in evaluating other factors that could potentially contribute to IF after TJA, such as type of anesthetic technique, use of regional anesthesia catheters, length of surgery, associated blood loss, or the activities associated with falling. The economic data in our study are based on charge data, which may not entirely reflect the actual costs associated with hospitalization. Some authors believe that the use of administrative claims data in orthopedic surgery outcomes research is not entirely concordant to clinical records [35, 36], but the use of administrative data allows a broad perspective on the incidence, risk factors, and implications of IF and has been used extensively by us evaluating the early outcome of TJA surgery [26, 33, 34, 37–39]. Despite these limitations, the data sample used was nationally representative of the United States and was able to provide clinically useful data for a potentially preventable complication after TJA.
Given the substantial comorbidity, mortality, and cost associated with IF and the increase in the incidence of these events, resources should be allocated to minimize fall risk among patients who have undergone joint arthroplasty. Patients who undergo revision arthroplasty, especially revision THA, should be considered at the higher risk for IF. The current investigation serves as a call for further study on the efficacy and cost-effectiveness of fall prevention strategies for patients undergoing orthopedic surgery.
Acknowledgments
This study was performed with funds from the Department of Anesthesiology at Hospital for Special Surgery (SGM), the Center for Education and Research in Therapeutics (AHRQ RFA-HS-05-14) (YC and MM), the Clinical Translational Science Center (NIH UL1-RR024996) (YM and MM), and the generous contributions of Mr Martin Berman, Mr Chill Goldfinger, and Ms Helen Goldfinger (AGDV).
Footnotes
Supplementary material available at www.arthroplastyjournal.org.
The Conflict of Interest statement associated with this article can be found at doi:10.1016/j.arth.2011.10.010.
References
- 1.Vlahov D, Myers AH, al-Ibrahim MS. Epidemiology of falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil. 1990;71:8. [PubMed] [Google Scholar]
- 2.von Renteln-Kruse W, Krause T. Fall events in geriatric hospital in-patients. Results of prospective recording over a 3 year period. Z Gerontol Geriatr. 2004;37:9. doi: 10.1007/s00391-004-0204-7. [DOI] [PubMed] [Google Scholar]
- 3.Mahoney JE. Immobility and falls. Clin Geriatr Med. 1998;14:699. [PubMed] [Google Scholar]
- 4.Morse JM, Morse RM. Calculating fall rates: methodological concerns. QRB Qual Rev Bull. 1988;14:369. doi: 10.1016/s0097-5990(16)30249-4. [DOI] [PubMed] [Google Scholar]
- 5.Nyberg L, Gustafson Y, Janson A, et al. Incidence of falls in three different types of geriatric care. A Swedish prospective study. Scand J Soc Med. 1997;25:8. doi: 10.1177/140349489702500103. [DOI] [PubMed] [Google Scholar]
- 6.Sehested P, Severin-Nielsen T. Falls by hospitalized elderly patients: causes, prevention. Geriatrics. 1977;32:101. [PubMed] [Google Scholar]
- 7.Alcee D. The experience of a community hospital in quantifying and reducing patient falls. J Nurs Care Qual. 2000;14:43. doi: 10.1097/00001786-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Ash KL, MacLeod P, Clark L. A case control study of falls in the hospital setting. J Gerontol Nurs. 1998;24:7. doi: 10.3928/0098-9134-19981201-05. [DOI] [PubMed] [Google Scholar]
- 9.Catchen H. Repeaters: inpatient accidents among the hospitalized elderly. Gerontologist. 1983;23:273. doi: 10.1093/geront/23.3.273. [DOI] [PubMed] [Google Scholar]
- 10.Fischer ID, Krauss MJ, Dunagan WC, et al. Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infect Control Hosp Epidemiol. 2005;26:822. doi: 10.1086/502500. [DOI] [PubMed] [Google Scholar]
- 11.Goodwin MB, Westbrook JI. An analysis of patient accidents in hospital. Aust Clin Rev. 1993;13:141. [PubMed] [Google Scholar]
- 12.Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19:732. doi: 10.1111/j.1525-1497.2004.30387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rohde JM, Myers AH, Vlahov D. Variation in risk for falls by clinical department: implications for prevention. Infect Control Hosp Epidemiol. 1990;11:521. doi: 10.1086/646085. [DOI] [PubMed] [Google Scholar]
- 14.Schwendimann R. Frequency and circumstances of falls in acute care hospitals: a pilot study. Pflege. 1998;11:335. [PubMed] [Google Scholar]
- 15.Mandl LA, Parks M, Quinlan P, et al. Who falls? A decade of experience at a musculoskeletal specialty hospital (abstract) Arthritis Rheum. 2010;62:S655. [Google Scholar]
- 16.Fiesta J. Liability for falls. Nurs Manage. 1998;29:24. doi: 10.1097/00006247-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Joint Commission on Accreditation of Healthcare Organizations. Standards FAQ details—fall reduction program. 2008 [Internet] Available from: http://www.jointcommission.org/standards_information/jcfaqdetails.aspx?StandardsFaqId=201&ProgramId=1.
- 18.Ackerman DB, Trousdale RT, Bieber P, et al. Postoperative patient falls on an orthopedic inpatient unit. J Arthroplasty. 2010;25:10. doi: 10.1016/j.arth.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Kurtz SM, Ong KL, Schmier J, et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89:144. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 20.HCUP databases. Healthcare cost and utilization project (HCUP) 2010 [Internet] Available from: http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 21.Introduction to the HCUP national inpatient sample (NIS) 2006. 2006 [Internet] Available from: http://www.hcup-us.ahrq.gov/db/nation/nis/2006NIS_INTRODUCTION.pdf.
- 22.Publications from the HCUP databases. 2010 [Internet] Available from: http://www.hcup-us.ahrq.gov/reports/pubsearch/pubsearch.jsp.
- 23.HCUP comorbidity software. Healthcare cost and utilization project (HCUP) 2010 [Internet] Available from: http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
- 24.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 26.Memtsoudis SG, Ma Y, Gonzalez Della Valle A, et al. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206. doi: 10.1097/ALN.0b013e3181bfab7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozak LJ. Underreporting of race in the national hospital discharge survey. Adv Data. 1995:1. [PubMed] [Google Scholar]
- 28.Harrell FE, editor. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. 2. New York: Springer; 2010. p. 87. [Google Scholar]
- 29.Sauerbrei W, Schumacher M. A bootstrap resampling procedure for model building: application to the Cox regression model. Stat Med. 1992;11:2093. doi: 10.1002/sim.4780111607. [DOI] [PubMed] [Google Scholar]
- 30.Hosmer DW, Lemeshow S, editors. Wiley series in probability and statistics. 2. New York: John Wiley & Sons, Inc; 2002. Applied logistic regression; p. 211. [Google Scholar]
- 31.Ashton J, Gilbert D, Hayward G, et al. Predicting patient falls in an acute care nursing setting. Kans Nurse. 1989;64:3. [PubMed] [Google Scholar]
- 32.Plati C, Lanara V, Mantas J. Risk factors responsible for patients’ falls. Scand J Caring Sci. 1992;6:113. doi: 10.1111/j.1471-6712.1992.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 33.Memtsoudis SG, Gonzalez Della Valle A, Besculides MC, et al. Trends in demographics, comorbidity profiles, inhospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty. 2009;24:518. doi: 10.1016/j.arth.2008.01.307. [DOI] [PubMed] [Google Scholar]
- 34.Liu SS, Gonzalez Della Valle A, Besculides MC, et al. Trends in mortality, complications, and demographics for primary hip arthroplasty in the united states. Int Orthop. 2009;33:643. doi: 10.1007/s00264-008-0549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bozic KJ, Chiu VW, Takemoto SK, et al. The validity of using administrative claims data in total joint arthroplasty outcomes research. J Arthroplasty. 2010;25:58. doi: 10.1016/j.arth.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 36.Matlock D, Earnest M, Epstein A. Utilization of elective hip and knee arthroplasty by age and payer. Clin Orthop Relat Res. 2008;466:914. doi: 10.1007/s11999-008-0122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bang H, Chiu YL, Memtsoudis SG, et al. Total hip and total knee arthroplasties: trends and disparities revisited. Am J Orthop (Belle Mead NJ) 2010;39:E95. [PubMed] [Google Scholar]
- 38.Memtsoudis SG, Ma Y, Gonzalez Della Valle A, et al. Demographics, outcomes, and risk factors for adverse events associated with primary and revision total hip arthroplasties in the United States. Am J Orthop (Belle Mead NJ) 2010;39:E72. [PubMed] [Google Scholar]
- 39.Memtsoudis SG, Ma Y, Chiu YL, et al. Perioperative mortality in patients with pulmonary hypertension undergoing major joint replacement. Anesth Analg. 2010;111:1110. doi: 10.1213/ANE.0b013e3181f43149. [DOI] [PubMed] [Google Scholar]


