Abstract
Background
Although there is some evidence of improved quality in nursing home care after the implementation of the 1987 Omnibus Budget Reconciliation Act regulations, the nursing processes that contribute to that improvement are not well understood. Assumptions that the mandated tools for resident assessment and care planning account for the change remain uninvestigated.
Objectives
To generate an empirically supported conceptual model of care planning integrity, incorporating five subconstructs: coordination, integration, interdisciplinary team, restorative perspective, and quality.
Methods
A correlational, model generation-model selection design guided the study. Using a random sample of 107 facilities, the research team combined primary data collected from care planning team members (n = 508) via a telephone survey, with variables extracted from the Medicaid Cost Reports and the Centers for Medicaid and Medicare Services Online Survey, Certification, and Reporting System (OSCAR) database. Primary and alternative models of care planning integrity were examined for fit to the data using structural equation modeling procedures.
Results
Using preliminary analyses, 18 observed indicators to represent the five latent subconstructs were identified. Fit indices for the primary model were borderline (comparative fit index = .892; root mean square error of approximation = .048), but were excellent for the alternative model (comparative fit index = .972; root mean square error of approximation = .026). Care planning integrity is demonstrated within nursing facilities through direct relationships with coordination, integration, and quality, and indirect relationships through integration with interdisciplinary team and restorative perspective.
Discussion
Care planning integrity captures differences in the way nursing facilities implement the care planning process, using the mandated standardized tools, that may make a difference in resident outcomes. Subsequent research is indicated to address those dynamics.
Keywords: care planning, nursing home residents, nursing homes
Care planning is the foundation of the nursing process. A Minimum Data Set for Resident Assessment and Care Screening (MDS) and specific standardized tools to support care planning in nursing facilities (Harrington & Carillo, 1999) are defined in the regulations resulting from the 1987 Omnibus Budget Reconciliation Act (OBRA). Also mandated in the regulations are that the resident assessment and care planning be a cyclical process, be coordinated by a registered nurse (RN), and be conducted by a multidisciplinary team. Long-term residents are assessed and a care plan initiated within 14 days of admission; they are reassessed, and the care plan reviewed and revised quarterly, annually, and after a significant change. Reassessment and care plan revision occur more frequently for short-term residents admitted under Medicare for recovery or rehabilitation after hospitalization.
Effective care planning and delivery processes that result in high-quality resident outcomes are difficult to establish and maintain. Current approaches to care planning may not be adequate for the growing, higher acuity, older adult population (Dellefield, 2006) and may not maximize the potential benefits to residents that might be expected through the standardized assessment tools and benchmarking quality indicator reports available from state and federal agencies. There is some evidence of improved quality (e.g., Harrington, Carrillo, Thollaug, Summers, & Wellin, 2000; Harrington, Zimmerman, Karon, Robinson, & Beutel, 2000) since OBRA 1987, but the nursing processes that contribute to that improvement are not well understood. Assumptions that the standardized tools for care planning account for the change remain uninvestigated.
Care planning integrity is the wholeness of the care planning process—the extent to which the process is comprehensive, pervasive, and constant. Care planning integrity encompasses five subconstructs: coordination, interdisciplinary team, integration, restorative perspective, and quality. The first four subconstructs have been derived through observation and document audit in the investigators’ preliminary qualitative research in nursing homes (Swagerty, Lee, Smith, & Taunton, 2005; Taunton, Swagerty, Lasseter, & Lee, 2005; Taunton, Swagerty, Smith, Lasseter, & Lee, 2004), whereas quality reflects the intent of the regulations stimulated by OBRA 1987.
The purpose of this study was to generate an empirically supported conceptual model of care planning integrity. The research reported here is part of a larger project intended to identify the associations between care planning integrity and nursing home resident outcomes (Taunton, 2002–2007).
Methods
Research Design
A correlational, model generation-model selection design was used to guide the study. Using a random sample of 107 facilities recruited in two Midwestern states, the research team explored the conceptualization of care planning integrity by combining primary data collected from care planning team members via a telephone survey with variables extracted from Medicaid Cost Reports and the Centers for Medicaid and Medicare Services Online Survey, Certification, and Reporting System (OSCAR) database. Correlation and structural equation modeling procedures were used to identify cogent indicators for five subconstructs. Findings reported in the subsequent pages are limited to the variables that were retained in the final model.1
Setting and Sample
A random sampling frame (n = 444) stratified by the state and number of beds was constructed to invite nursing facilities to participate in the study. Of the 331 contacted, 107 facilities were recruited and provided usable data (55 from State A and 52 from State B; participation rate = 32%). Facilities with fewer than 50 beds were excluded, as were facilities not certified for Medicaid. The number of licensed beds ranged from 50 to 288, with a mean of 100 (SD = 44). Of the sample facilities, 60% were rural, 63% were for profit, and 87% were Medicare certified. On average, 60% (SD = 15%, range = 17%–95%) of resident days were paid by Medicaid.
Respondents to the telephone survey for the participating facilities included 508 care planning team members. The facility staff invited to be interviewed were responsible for completing part of the MDS. Excluded were staff (e.g., nursing assistant and chaplain) who came to a care plan review meeting to provide input or obtain information but who did not participate in resident assessment. The sample is described in terms of discipline, education, and experience in Table 1. Most (93%) care planning team members were women; 91% were White, 5% were African American, 2% were Hispanic, and 2% reported “other” or “more than one race.”
TABLE 1.
Characteristics of the Telephone Survey Sample (N= 508)
| Education, n (%) |
|||||||
|---|---|---|---|---|---|---|---|
| Discipline (n) | Some high school |
High school diploma or general equivalency diploma |
Some higher educationa |
Technical or vocational school |
Diploma or associate degree |
Bachelor of science or bachelor of art degree |
Graduate degree |
| Nursing (174) | |||||||
| RN (132) | 96b | 33 (19) | 4 (2) | ||||
| LPNs (42) | 42 (24) | ||||||
| Activity (87) | 2 (2) | 29 (33) | 28 (32) | 6 (7) | 5 (6) | 15 (17) | 2 (2) |
| Dietary (88) | 4 (5) | 23 (26) | 22 (25) | 18 (21) | 2 (2) | 13 (15) | 6 (7) |
| Medical records (3) | 2 (67) | 1 (33) | |||||
| Occupational therapy (6) | 6 (100) | ||||||
| Physical therapy (17) | 1 (6) | 6 (35) | 5 (29) | 5 (29) | |||
| Restorative aide/LPN (25) | 2 (8) | 11 (44) | 5 (20) | 6 (24)c | 1 (4) | ||
| Social service (98) | 7 (7) | 26 (27) | 5 (5)d | 5 (5) | 35 (36) | 20 (20) | |
| Dual role (9)e | 4 (44) | 1 (11) | 1 (11) | 1 (11) | 2 (22) | ||
|
Experience |
|||||||
|
Role |
Facility |
Long-term care |
|||||
| Years | n | % | n | % | n | % | |
| ≤1 | 156 | 31 | 102 | 20 | 25 | 5 | |
| >1 to ≤2 | 92 | 18 | 69 | 14 | 25 | 5 | |
| >2 to ≤5 | 137 | 27 | 139 | 27 | 81 | 16 | |
| >5 to ≤10 | 73 | 14 | 98 | 19 | 124 | 24 | |
| >10 to ≤15 | 36 | 7 | 52 | 10 | 84 | 17 | |
| >15 | 14 | 3 | 48 | 9 | |||
| >15 to ≤20 | 82 | 16 | |||||
| >20 to ≤25 | 38 | 8 | |||||
| >25 to ≤30 | 31 | 6 | |||||
| >30 | 16 | 3 | |||||
| M (SD) | 3.96 (4.40) | 6.11 (6.15) | 12.51 (8.91) | ||||
| Median | 2.50 | 4.00 | 10.00 | ||||
| Minimum–Maximum | 0.08–27.00 | 0.08–36.00 | 0.08–52.00 | ||||
Note. RN = registered nurse; LPN = licensed practical nurse.
No degree.
These include 14 (8%) RNs with a hospital diploma and 82 (47%) with an associate degree.
These include 5 (20%) LPNs.
These include 2 (2%) LPNs.
These include seven activities or social services, one social service or dietary, and one activity or restorative aide.
Among the 125 care planning coordinators (MDSCs) interviewed, there were 20 directors of nursing, 1 assistant director of nursing, 7 nurse or unit managers, 96 staff RNs, and 1 contract RN. In addition, there were 39 licensed practical nurses (LPNs) and 1 social service designee who assisted in the coordination of the care planning process (MDSC helpers). The MDSCs consented to both an initial and follow-up interview when they agreed to participate in the study. There was no attrition.
Measures
Care planning integrity was operationalized as a latent construct comprised of the five latent subconstructs. Survey items were based on the investigators’ earlier observations of the care planning process (Swagerty et al., 2005; Taunton et al., 2005; Taunton, Swagerty, et al., 2004) and were field tested in a telephone survey of 20 facilities (Bott et al., 2002). Each subconstruct is described in the next paragraphs, and the measured indicators are described in Table 2.
TABLE 2.
Care Planning Integritya: Subconstructs With Definition and Indicators
| Definition | Indicator | Scoring, validity, and reliability |
|---|---|---|
| Coordination | ||
| Allocation of the responsibility, authority, accountability, and resources for coordinating the care planning process within the facility |
|
|
| Interdisciplinary team | ||
| Time allocated to care planning by the staff representing various disciplines who assume ongoing responsibility for the care planning process, including (a) assessing residents, (b) completing RAPs, (c) drafting the care plan, and (d) reviewing the care plan; excludes the staff who attend the care planning meeting to provide input or receive information but do not assume responsibility for other aspects of the process |
|
Participating disciplines confirmed by multiple members of the care planning team
|
| Integration | ||
| Synthesis of care planning and care delivery |
|
|
| Restorative perspective | ||
| Perception among the care planning team members that the staff can help residents to maintain or achieve improved physical and cognitive function for activities of daily living, including mobility, continence, eating, dressing, and cognition | Perception of residents:
|
Exploratory principal component factor analysis (n = 503, care planning team members) and confirmatory factor analysisb (n = 369, direct care staff): comparative fit index = .95, root mean square error of approximation = .14
|
| On-siteb data showed 80%–90% agreement between the care planning team’s and the staff’s responses to these items, indicating that the care planning team reasonably represented the staff’s perceptions of resident potential within the facility. | ||
| Quality | ||
| Deficiencies cited on nine F-Tags (Table 3) related to resident assessment, care planning, and overall care cited in the state survey process across 3 years | Weighted score on each of the nine F-Tags | Scored via Indiana Report Cardc system |
| Scores were reversed to reflect compliance rather than deficiencies. | ||
| Square-root transformation was used to improve distribution. | ||
| Repeated citations on six of the nine F-Tags supported combining data for each F-Tag across three surveys. | ||
| For the summed, weighted scores across nine F-Tags, Cronbach’s α = .70. |
Note. MDS = Minimum Data Set for Resident Assessment and Care Screening; MDSC = an RN coordinating the care planning process; RAPs = resident assessment protocols; LPN = licensed practical nurse.
Care planning integrity is the wholeness of the care planning process—the extent to which the process is comprehensive, pervasive, and constant.
On-site data were collected from the direct care staff in nine facilities (n = 373) to facilitate the validation of data reported by the care planning team members. The sample included RNs (n = 26), LPNs (n = 58), nursing assistants (certified nurse’s aid or certified medical assistant, n = 229), restorative aides (n = 15), and other (n = 39). Six participants did not report their role.
For details regarding application of the Indiana Report Card system, see Bott, Piamjariyakul, Adams-Wendling, Gajewski, and Taunton (2005)
Coordination refers to the management of the care planning process and captures the allocation of authority, responsibility, accountability, and resources to that function. The coordination of resident assessment and care planning may be centralized under one RN (MDSC) for the entire facility or decentralized under two or more RNs with designated responsibility for specific groups of residents. The MDSC may have 100% time dedicated to that role or may be assigned other clinical or management responsibilities. The MDSC sometimes has a permanently assigned helper, usually a LPN. Residents may be grouped for assessment and care planning by location (unit, household, or neighborhood), payment source (Medicare vs. other), or type of assessment (quarterly, annual, etc.). The coordination function facilitates the constant element of the care planning process.
Integration is the synthesis or fusion of care planning and delivery. It represents the degree to which the MDS system is assimilated within the facility along a continuum from purely paperwork to critical guide for resident care. Integration also reflects staff’s perceptions about the impact of the MDS reassessments and care plan reviews on resident care. It embodies the pervasive nature of the care planning process.
Interdisciplinary team denotes the diversity among providers and supports the comprehensive element of care planning. It captures the participation of nursing, social service, activity, dietary, restorative, and therapy staff who assume ongoing responsibility for the care planning process, including assessing residents, completing resident assessment protocols (RAPs), drafting the care plan, and reviewing the care plan.
Restorative perspective infers a philosophical orientation within the nursing facility that promotes and facilitates optimal resident function. The construct rests on the perception among the care planning team members that the staff can help residents to maintain or achieve improved physical and cognitive function for activities of daily living. It supports the comprehensive element of the care planning process.
Restorative perspective is based loosely on the characterization of rehabilitative nursing homes by Kane, Chen, Blewett, and Sangl (1996). However, rather than the focus of Kane et al. on subacute care for residents admitted for restoration of physical functioning and expected return to the previous living situation, this study is focused on the long-term care mission of nursing homes.
Quality of the care planning process incorporates deficiency citations in the state survey process for nursing homes reported in the OSCAR database. In the state survey process, the specific concepts in the federal regulations for nursing homes are labeled as F-Tags (e.g., F272: comprehensive, standardized, reproducible assessment of each resident’s functional capacity, etc.). Facilities are cited by surveyors for noncompliance with specific F-Tags.
The investigators’ measures of quality were derived from nine F-Tags (Table 3): Four were related to comprehensive resident assessment, two were related to the comprehensive care plan, and three were related to overall care consistent with the resident assessment and care plan. Two F-Tags (F273 and F275) related to the admission and annual assessments were eliminated from further consideration because of extremely limited variability in the data (Bott et al., 2005). The quality measures embody the constant, comprehensive, and pervasive characteristics of care planning integrity.
TABLE 3.
F-Tags and Regulations Related to the Care Planning Process
| F-Tag | Regulation |
|---|---|
| Assessment | |
| F272 | The facility must conduct initially and periodically a comprehensive, accurate, standardized reproducible assessment of each resident’s functional capacity (using the Resident Assessment Instrument specified by the state). |
| F274 | A facility must conduct a comprehensive assessment of a resident within 14 days after the facility determines, or should have determined, that there has been a significant change in the resident’s physical or mental condition. |
| F276 | A facility must assess a resident using the quarterly review instrument specified by the state and approved by the HCFA not less frequently than once every 3 months. |
| F278 | The assessment must reflect the resident’s status accurately. A registered nurse must conduct or coordinate each assessment with the appropriate participation of health professionals. |
| Comprehensive care plan | |
| F279 | The facility must develop a comprehensive care plan for each resident that includes measurable objectives and timetables to meet a resident’s medical, nursing, and mental and psychological needs that are identified in the comprehensive assessment. |
| F280 | A comprehensive care plan must be:
|
| Services | |
| F281 | The services provided or arranged by the facility must meet professional standards of quality. |
| F282 | The services must be provided by qualified persons in accordance with each resident’s written plan of care. |
| F309 | Each resident must receive and the facility must provide the necessary care and services to attain or maintain the highest practicable physical, mental, and psychosocial well-being, in accordance with the comprehensive assessment and plan of care. |
Note. HCFA = Health Care Financing Administration. From OBRA, 2001.
Using data from the three annual state surveys immediately preceding the primary data collection and the Indiana scoring system (Indiana State Department of Health, 2003; Nursing Home Report Cards, n.d.), the research team calculated a weighted score for each F-Tag that reflected the scope and severity of each citation and a longitudinal perspective of quality. Weights were assigned to each annual survey so that the one closest to the primary data collection for each facility counted most. The scores were reversed so that a higher score represents better quality of the care planning process. (For details regarding the application of the Indiana system, see Bott et al., 2005.)
Other Variables
Demographic characteristics of the survey respondents included role in the facility, education, experience, race or ethnicity, and gender. Several facility characteristics were measured: state, location (rural vs. urban), ownership (not for profit vs. for profit), number of licensed beds, Medicare certification, percentage of Medicare days, and percentage of Medicaid days. Designation as rural or urban was based the Metropolitan Statistical Area ZIP Code classification. Ownership and number of beds were extracted from the public Medicare Compare database on the Internet, and the facility staff verified the number of licensed beds. The data related to Medicare and Medicaid days per year were extracted from the facility Medicaid Cost Reports.
Procedures
Recruitment
The University of Kansas Medical Center Human Subjects Committee reviewed the project for protection of human rights and approved the proposed procedures and documents. The committee also reviewed and approved the documents and procedures for the Health Insurance Portability and Accountability Act compliance.
Packets of material describing the project were mailed in staggered groups of 50 to the administrators of facilities in the stratified random sample. The packet included a cover letter to explain the study and the requested participation, abstract, institutional consent form, and consent documents for other facility staff who would be invited to participate in the telephone survey. Project staff contacted the respective administrator by telephone to answer questions about the study, determine interest in participation, identify the care planning coordinator and obtain contact information, and facilitate return of the institutional consent form.
As the signed institutional consents were received, each facility was assigned to a specific project staff member who conducted the telephone survey with the MDSC and other members of the care planning team. Appropriate consents were obtained before interviews were scheduled. Except in facilities with prohibiting institutional or corporate policy, participants who were interviewed received an honorarium. The telephone interviews were conducted during on-duty hours and were tape recorded.
Data Collection
The survey items were assembled into three Web-based questionnaires (MDS-I, MDS-II, and Team Member) that were fed into an Excel database (Piamjariyakul, Bott, & Taunton, 2006). Within each facility, the project staff interviewed participants by telephone and recorded their responses directly on the questionnaire. The interviews were conducted sequentially, as described in the next paragraphs.
First, the MDSC responded to the MDS-I questionnaire (216 items). Detailed information about all aspects of the care planning process was elicited using the MDS-I, for example, who completed what components of the assessment, completed the RAPs, drafted the care plan, or entered the data. Time estimates were obtained for every aspect of the care planning process. Also addressed were problem-focused meetings in which decisions were made about an individual resident’s care. The MDS-I required 1.0–1.5 hours for completion. On the basis of data provided by the MDSC, the research staff drafted a process map (flowchart) depicting the respective facility’s care planning process.
Second, two questionnaires were used to verify or expand the information provided in the initial MDSC interview. The MDS-II questionnaire (105 items) was a shortened version of the MDS-I designed for use with a second MDSC or an MDSC helper; it required about 30 minutes. A Team Member questionnaire (83 items) was used for the staff from social services, dietary, activities, the therapies, and others who participated in the resident assessment; 30 minutes or less was required for the interview. The facility’s draft process map was reviewed as part of the interviews and modified to incorporate new information.
Upon completion of the Team Member interviews, a revised draft of the process map was sent to the MDSC for review by the care planning team. The MDSC was interviewed a second time, using a fourth questionnaire, MDS-I Follow-up (eight items). The follow-up telephone interview addressed each element in the revised process map, focusing on confirmation or suggestions for corrections; 30 minutes or less was required.
Training for Data Collection
The RN coprincipal investigator trained and supervised the research staff for the telephone survey of care planning team members. Included were a RN (PhD); the project manager (MA, psychology), who was experienced in aging research; and three graduate research assistants from the Health Policy and Management Department, School of Medicine.
Multiple training sessions were held for the project staff to (a) orient to and refine the survey tool, (b) record data on the Web-based questionnaire from a pretaped practice interview, and (c) conduct simulated interviews. Each data collector’s first actual participant interview was monitored and coached by the coprincipal investigator.
Interrater Reliability
Throughout the data collection, 10% of the interviews were rated independently by a clinical nurse specialist certified as a nursing home administrator. The documented participant’s responses were compared with the tape-recorded verbal responses. Percentage of agreement ranged from 95% to 100%. Errors were reported to the data collectors and corrected.
Data Analysis
Excel, SPSS, and Mplus software systems were used for data management and analysis. The analysis strategy began with scoring and descriptive analyses for the potential indicators for the respective latent subconstructs of care planning integrity. A square-root transformation was used to improve the distribution of scores on the quality F-Tag indicators.
A modified t score transformation was applied to the scores on integration and restorative perspective indicators. For each indicator, the scores were anchored to the midpoint of the respective response scale. First, the raw scores were transformed to z scores, with the midpoint of the scale set to 0 and the standard deviation set to 1. Second, the z scores were converted to t scores, with the midpoint set to 50 and the standard deviation to 10. A t score greater than 60 on any of the transformed indicators was more than 1 SD above the scale midpoint and could be reasonably interpreted as “high.” Basing the modified t score on the scale midpoint rather than on the group mean facilitated interpretation and comparison of scale scores within the same subconstruct (Taunton et al., 2004).
For multi-item scales, exploratory and confirmatory factor analyses were conducted to assess dimensionality, and internal consistency reliability was evaluated via Cronbach’s alpha. Each indicator was evaluated for association with facility characteristics (e.g., location and ownership). Correlations were examined for evidence of association among scores on the indicators within the same care planning integrity subconstruct and across the five subconstructs.
On the basis of the associations within and between subconstructs, measured indicators for each subconstruct were selected for entry into the structural equation modeling procedures to evaluate and compare primary and alternative models of care planning integrity. Both models incorporated the five latent subconstructs. Three fit indices were used in evaluating the models: chi-square test of model fit (χ2, criterion: p < .05), comparative fit index (CFI; criterion: ≥.90), and root mean square error of approximation (RMSEA; criterion: <.05).
Results
Descriptive Findings
Descriptive findings related to the variables representing the care planning integrity subconstructs (Table 4) are summarized in the paragraphs below. None of the scores on the care planning integrity indicators were associated with facility ownership (not for profit vs. for profit). The observed variables for care planning integrity were not influenced appreciably by Medicaid days, number of licensed beds, or urban location. Scores on indicators for coordination, interdisciplinary team, integration, and quality varied by state (r = −.22 to .25, p ≤ .05).
TABLE 4.
Descriptive Findings of Indicators for Planning Integrity Subconstructs (n = 107 facilities)
| Indicator | M | SD | Minimum | Maximum |
|---|---|---|---|---|
| Coordinationa | ||||
| MDSC time | 4.68 | 2.96 | 0.24 | 16.32 |
| MDSC helper time | 1.75 | 2.55 | 0.00 | 9.10 |
| Interdisciplinary teamb | ||||
| Basic care disciplines time | 11.94 | 4.35 | 3.71 | 31.02 |
| Restorative disciplines time | 0.76 | 1.37 | 0.00 | 13.00 |
| Integrationc | ||||
| MDS system assimilated | 65.14 | 10.00 | 32.89 | 80.80 |
| Care planning impact | 42.11 | 10.00 | 21.63 | 71.28 |
| Restorative perspectivec | ||||
| Mobility and continence | 75.47 | 10.00 | 37.80 | 100.09 |
| Dressing and eating | 82.18 | 10.00 | 43.17 | 104.64 |
| Cognition | 67.05 | 10.00 | 25.61 | 88.19 |
| Quality | ||||
| F-Tag scoresd | ||||
| F272 | 3.15 | 0.71 | 0.00 | 3.46 |
| F274 | 2.20 | 0.72 | 0.00 | 2.58 |
| F276 | 2.21 | 0.41 | 0.00 | 2.31 |
| F278 | 3.33 | 0.87 | 0.00 | 3.74 |
| F279 | 3.33 | 1.11 | 0.00 | 4.24 |
| F280 | 2.98 | 0.80 | 0.00 | 3.32 |
| F281 | 3.08 | 1.10 | 0.00 | 4.24 |
| F282 | 2.49 | 0.78 | 0.00 | 2.83 |
| F309e | 8.77 | 1.74 | 0.00 | 10.00 |
Note. MDS = Minimum Data Set for Resident Assessment and Care Screening; MDSC = an RN coordinating the care planning process.
Minutes per resident per day.
Hours per resident reviewed for care planning.
Modified t score; midpoint of scale was set to 50.00; SD was set to 10.00 to facilitate interpretation and comparison among indicators of the same subconstruct.
Square-root transformation and scores were reversed so that higher score represents higher quality. For a given F-Tag, the minimum value of 0.00 represents the most citations of the greatest scope and severity weighted across three surveys.
Score range includes additional points added to any annual survey in which a rating of substandard care is cited.
Coordination of the care planning process incorporated the structure and resources allocated to that function by the facility. The most common structure (57%) was one staff RN coordinating a care planning team; in facilities that were decentralized for care planning, that pattern translated to two or more teams, each coordinated by an RN. One facility contracted externally with an RN to complete the MDS; the director of nursing drafted the care plans and conducted the care planning meeting.
The director of nursing or a nurse manager served as an MDSC in 32% of the facilities; this model was less common in urban areas (r = −.27, p < .01). In 36% of the facilities, the MDSC had a helper; except for one social service designee, the helper was a LPN. The MDSC-with-helper model was more common in one state than the other (r = .22, p < .05). Facilities were more likely to use the helper model when the director of nursing or a nurse manager took the MDSC role (r = .89, p < .001).
Two time variables best represented the coordination subconstruct. The time variables were adjusted for the size of the facility by dividing by the average daily census. “MDSC minutes per resident per day” captured the amount of RN time assigned to the coordination function; all facilities assigned dedicated RN time. “MDSC helper minutes per resident per day” reflected the assistance given to the RN coordinator in those facilities that used the MDSC-with-helper approach; facilities with no helper scored 0 on that variable. Comparing the MDSC-withhelper facilities to facilities with no helper in regard to the total time dedicated to the coordination function, there was no significant difference, t(105) = −1.268, p = .21, between the combined time for the coordinator and helper (M = 6.81; SD = 1.83) and the MDSC minutes per resident per day in facilities with no helper (M = 6.21; SD = 2.58).
Integration of care planning and care delivery was represented by two indicators (Table 4). Generally, care planning team members viewed the MDS system as assimilated into care planning and delivery. However, on average, the teams estimated that less than half of the staff perceived that changes in residents’ daily care resulted from the MDS reassessments and care plan reviews.
Within interdisciplinary team, basic care disciplines scored higher on participation in the care planning process than restorative disciplines (Table 4). Nurses, social workers, dietary staff, and activity staff participated more often in assessing residents, completing RAPs, drafting care plans, and reviewing care plans than restorative aides and rehabilitation or physical therapists.
Overall, care planning team members reflected a strong restorative perspective (Table 4). Expectations that the staff could help residents maintain or improve function for dressing and eating were highest, whereas expectations about maintaining or improving cognitive function were lowest.
Quality of the care planning process was represented by scores on nine F-Tags (Tables 3 and 4) that captured the scope and severity of deficiencies cited by the state surveyors. Higher scores represented higher quality. Half or more of the facilities incurred no citations on the respective F-Tag. The lowest quality scores reflected less compliance related to the timeliness of significant change assessments (F274) and quarterly reassessments (F276). The highest quality scores documented more compliance related to the accuracy of the assessment, coordination by an RN, and interdisciplinary participation (F278) and to providing care and services to maintain the highest practicable well-being in accordance with the assessment and care plan (F309).
Modeling Care Planning Integrity
Correlation Within Subconstructs
There were significant weak to moderate relationships between the indicators within the respective care planning integrity subconstructs (r = .19 to −.65). The strongest relationship was between the two coordination indicators, and the weakest between two of the quality indicators, F279 and F280.
Correlation Between Subconstructs
There were modest associations between the indicators of the five care planning integrity subconstructs. Scores on quality generated the most relationships; one or more quality indicators were related to one or more indicators, respectively, for coordination, integration, and restorative perspective (additional information provided by the authors expanding this article is on the Editor’s Web site at http://www.nursing-research-editor.com). There were also multiple associations between integration and both interdisciplinary team and restorative perspective. Better integration of the care planning process was associated with more interdisciplinary participation and with the perception within the facility that the staff could help residents to maintain or improve mobility, continence, and cognition.
Primary Model
Parsimony was the guiding principle for the initial model. No parameters were constrained to 0 (q = 41 free parameters), and no paths were identified for cross-loadings of measured indicators among the subconstruct latent variables or for correlated error terms. Care planning integrity emerged through direct connections to the latent subconstruct variables for coordination, integration, interdisciplinary team, restorative perspective, and quality. In turn, each latent subconstruct variable connected directly to its observed indicators. The nine F-Tags were entered as a single latent quality variable because the correlations among the scores (additional information provided by the authors expanding this article is on the Editor’s Web site at http://www.nursing-research-editor.com) and a standardized Cronbach’s alpha of .70 reflected internal consistency.
Fit indices from the structural equation modeling procedures were borderline (χ2 = 161.40, df = 130, p = .032; CFI = .892; RMSEA = .048, 90% confidence interval [CI] = 0.015–0.070, p [RMSEA < .05] = .552). Negative parameters for coordination with the indicator MDSC time were consistent with the observed data. As helper time increased, MDSC time decreased (r = −.65, p ≤ .001). Also, MDSCs with a helper dedicated fewer minutes per resident per day to the care planning coordinator role than did their counterparts without helpers. The estimate and association parameters between care planning integrity and both coordination and interdisciplinary team were nonsignificant. The estimate and association parameters were also nonsignificant between interdisciplinary team and its observed indicators.
Alternative Model
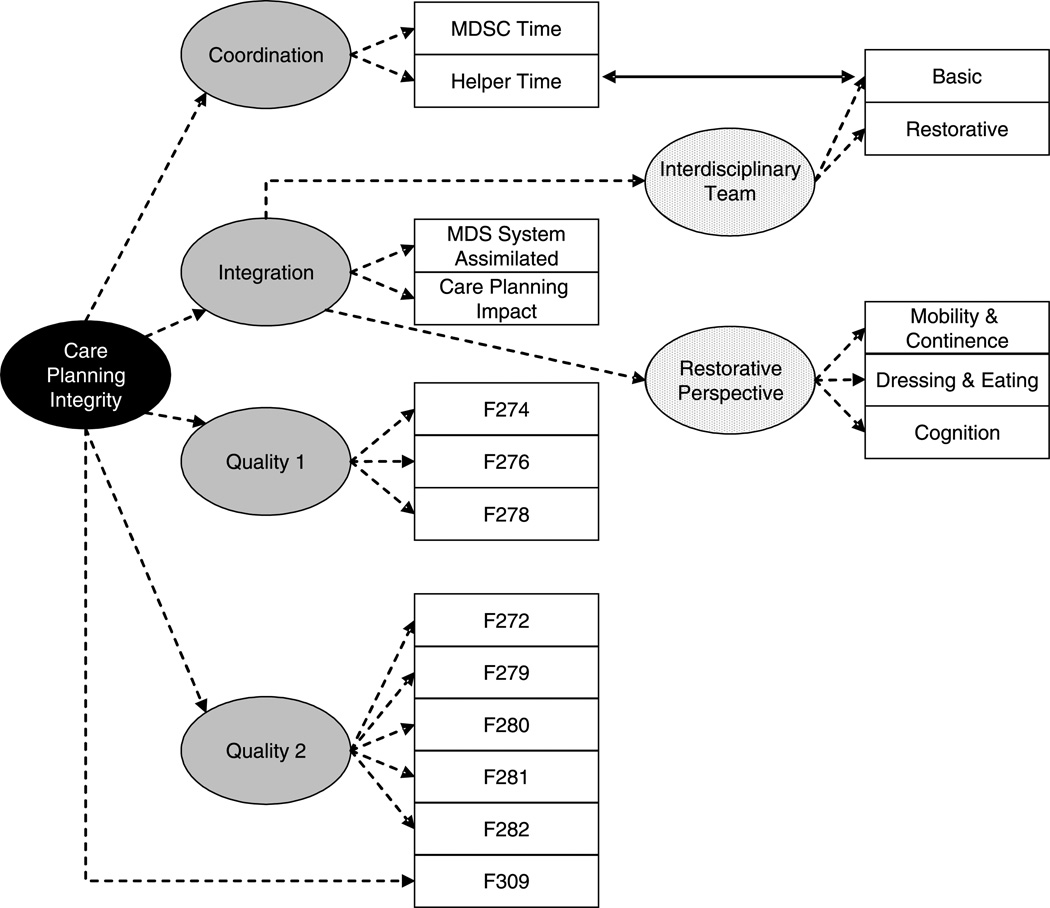
The alternative model of care planning integrity is depicted in Figure 1 (q = 43 free parameters). Care planning integrity emerged through direct relationships with coordination, integration, and quality and through indirect relationships through integration with interdisciplinary team and restorative perspective. Structurally, there were two differences from the primary model. Quality was entered as two latent subconstruct variables based on prior analyses (Bott et al., 2005), indicating that a two-factor model fit the data. Quality 1 attracted F-Tags related to the comprehensive resident assessment (F274, F276, and F278). Quality 2 attracted F-Tags that linked the services provided to the resident to the assessment and written care plan (F272, 2F79, F280, F281, F282, and F309).
FIGURE 1.
Care planning integrity in nursing facilities. MDS = Minimum Data Set for Resident Assessment and Care Screening; MDSC = an RN coordinating the care planning process.
The second structural modification involved removing the direct connections with care planning integrity for interdisciplinary team and restorative perspective and repositioning those subconstructs to receive that influence indirectly through integration. The alteration reflected the correlations between the observed indicators for integration and the indicators for both interdisciplinary team and restorative perspective. In addition, the scoring procedure for the basic care and restorative discipline indicators was refined to increase variability.
Fit indices improved appreciably for the alternative model (χ2 = 137.21, df = 128, p = .273; CFI = .972; RMSEA = .026, 90% CI = 0.00–0.055, p [RMSEA < .05] = .902). Estimate and association parameters were significant for all latent variables and measured indicators (Table 5). Care planning integrity directly increased compliance with F309, the regulation requiring that each resident receive the care and services to attain the highest practicable physical, mental, and psychosocial well-being, in accordance with the comprehensive assessment and plan of care. Increased helper time was associated with increased participation of basic care disciplines in the care planning process.
TABLE 5.
Care Planning Integrity: Model Parameters
| Parameters |
||||
|---|---|---|---|---|
| Variable | Est | SE | Est/SEa | StdYX |
| Coordination by indicators | ||||
| MDSC time | −2.309 | 0.408 | −5.655 | −0.853 |
| MDSC helper time | 1.778 | 0.309 | 5.759 | 0.759 |
| Integration by indicators | ||||
| MDS system assimilated | 8.190 | 1.374 | 5.960 | 0.886 |
| Care planning impact | 4.569 | 1.020 | 4.479 | 0.494 |
| Interdisciplinary team by indicators | ||||
| Basic disciplines | 2.504 | 0.719 | 3.481 | 0.687 |
| Restorative disciplines | 0.555 | 0.152 | 3.645 | 0.478 |
| Restorative perspective by indicators | ||||
| Mobility and continence | 5.969 | 1.052 | 5.673 | 0.654 |
| Dressing and eating | 6.104 | 1.059 | 5.763 | 0.669 |
| Cognition | 5.615 | 1.037 | 5.413 | 0.616 |
| Quality 1 by F-Tags | ||||
| F274 | 0.170 | 0.086 | 1.984 | 0.470 |
| F276 | 0.081 | 0.043 | 1.902 | 0.397 |
| F278 | 0.287 | 0.147 | 1.959 | 0.655 |
| Quality 2 by F-Tags | ||||
| F272 | 0.304 | 0.060 | 5.065 | 0.560 |
| F279 | 0.739 | 0.119 | 6.203 | 0.873 |
| F280 | 0.131 | 0.065 | 2.010 | 0.215 |
| F281 | 0.417 | 0.092 | 4.549 | 0.498 |
| F282 | 0.251 | 0.064 | 3.901 | 0.424 |
| F309 | ||||
| Integration by interdisciplinary team and restorative perspective | ||||
| Interdisciplinary team | 0.569 | 0.212 | 2.679 | 0.522 |
| Restorative perspective | 0.405 | 0.145 | 2.787 | 0.399 |
| Care planning integrity by subconstructs | ||||
| Coordination | 0.425 | 0.149 | 2.851 | 0.391 |
| Integration | 0.400 | 0.152 | 2.633 | 0.371 |
| Quality 1 | 1.706 | 0.979 | 1.743 | 0.863 |
| Quality 2 | 0.844 | 0.229 | 3.685 | 0.645 |
| Other parameters | ||||
| Care planning integrity by F309 | 1.183 | 0.191 | 6.200 | 0.685 |
| MDSC helper time with basic disciplines | 3.081 | 0.785 | 3.926 | 0.283 |
Note. Est = estimate; SE = standard error of the estimate; StdYX = standardized association coefficient; MDS = Minimum Data Set for Resident Assessment and Care Screening; MDSC = an RN coordinating the care planning process.
p ≤ .05 = Est/SE 1.65; p ≤ .01 = Est/SE 2.33; p ≤ .001 = Est/SE 3.08 (Glasnapp and Poggio, 1985).
Discussion
Descriptive findings on the observed indicators for the care planning integrity subconstructs tell a story about that process. Nursing facilities use different structures for coordinating the mandated MDS system for resident assessment and care planning. There is some evidence that the approach chosen makes a difference in the quality of the process. More MDSC minutes per resident per day (no helper) is associated with less compliance with the regulations related to cyclical comprehensive assessment (F272), quarterly reassessment (F276), the timely development and review of the resident care plan by an interdisciplinary team (F280), and provision of resident services in accordance with the assessment and care plan to maintain the highest well-being. In addition, more MDSC helper minutes per resident per day improves resident services (F309).
Although the total time allocated to coordination in facilities using the MDSC-with-helper model is slightly higher than that in other facilities, that difference is not significant. Further analysis (Taunton, Piamjariyakul, Gajewski, & Bott, 2006) indicates that the MDSC without a helper spends the most time in the care planning process. Thus, the advantage lies in having two persons rather than in the amount of RN time. Two persons can be in different places at the same time and can do different things.
Greater involvement of nursing, social service, dietary, and activity staff in the care planning process increases the likelihood that a resident’s initial assessment and care plan will be completed within the specified 14 days and that the services provided will meet professional standards of quality. The process is improved, and residents are more likely to receive high-quality services where the care planning team perceives the MDS system as an important guide for resident care and the staff perceive that changes in daily care result from the reassessments and care plan reviews.
As might be expected, the state in which facilities are located impacts scores on the observed indicators for the care planning integrity subconstructs. There are differences in state regulations and differences in the survey process. For-profit status is not driving the care planning process in this sample, and associations with other facility characteristics are not compelling.
Comparison of Primary and Alternative Models
The conceptualization of care planning integrity that emerges here is intended for use initially in complex, multilevel structural equation modeling procedures to evaluate its impact on resident outcomes and, subsequently, by both other researchers and clinicians. Although fit to the data is the most critical, property, parsimony, interpretability, and usability also are important characteristics.
The RMSEA values for both models are acceptable. Nevertheless, the 90% CI and probability that the RMSEA is less than .05 favor the alternative model. The chi-square is significant for the primary model but not significant for the alternative model. The CFI for the alternative model exceeds the criterion for acceptable fit, whereas it is borderline for the primary model. Although the primary model was more parsimonious than the alternative model, it lacks the clarity achieved by the alternative model.
Interpretation is straightforward for both models. There is logical clarification for the negative parameters between coordination and MDSC time. More explanation is required for the alternative model than the primary model, but that burden is not onerous.
A viable measurement model for the quality subconstruct is essential if investigators are to be confident about using care planning integrity as a research construct or about using the quality measure separately. The OSCAR database of state surveyor citations has been selected to operationalize quality of the care planning process because of its common use in research and national availability. In this instance, there are a finite number of F-Tags related to resident assessment and care planning, and their wording is fixed. Consequently, revising items or adding items, the usual strategies for improving the internal consistency within a factor, is not possible.
As expected, internal consistency across the nine indicators comprising the primary model’s single-factor quality variable is higher (α = .70) than that for the two factors in the alternative model (Quality 1, three indicators, α = .48; Quality 2, six indicators, α = 0.66). Internal consistency for each of the smaller factors is reasonable, given the respective number of items.
Researchers who use the care planning integrity model in complex research designs likely will find that the two-factor quality subconstruct works best. The single-factor measure may work very well as a measure of quality in less stringent research or clinical situations.
Limitations
The sample drawn from two contiguous Midwestern states may not have captured the possible variation among a more nationally representative sample of facilities in regard to the model for coordination of the care planning process and differences among the state survey processes that generate the OSCAR database. The study was limited to the existing variables available from the OSCAR database for measures of quality and to the variables available in the Medicaid Cost Reports to estimate the average daily census and percentage of Medicaid days.
Important data about how and where translation and communication of the MDS care plan occurred were not available to the statistical procedures. On-site observations and record audit in the nine facilities did not confirm care planning team reports in the telephone survey about transmission of the care plan to the staff providing daily care; those data were viewed as unreliable and excluded from analysis.
Thompson and Oliver (in press) suggest that palliative perspective would be an important subconstruct to incorporate into care planning integrity. Palliative perspective likely is an essential adjunct to restorative perspective in planning resident care and should be considered for inclusion in future studies.
Summary and Conclusions
Descriptive data document variations among the 107 facilities in the way the federally mandated MDS system is applied within the care planning process. Even though the standardized Resident Assessment Instrument is used in all nursing facilities certified for Medicaid and Medicare, facilities differ in regard to which RN coordinates the care planning process, whether that RN has a helper who is not an RN, and the amount of time the MDSC spends in that role. Across facilities, different disciplines participate in different parts of the process. Care planning team members’ perceptions vary in terms of the degree to which the MDS system is incorporated into care planning and delivery. Care planning team members also hold different perceptions about whether the staff can help residents to maintain or achieve improved physical and cognitive function for activities of daily living. Although substantial compliance with the nine federal regulations (F-Tags) related to resident assessment and care planning is reflected in the data, citations for noncompliance occurred among the sample on every F-Tag. Care planning integrity captures differences in the way nursing facilities implement the care planning process, including the mandated MDS system, that may impact care plan implementation and resident outcomes.
Findings from the study comprise an empirically derived conceptual model of care planning integrity for use in studying its impact on nursing processes and on resident outcomes. Within nursing facilities, care planning integrity manifests through the dedication of personnel resources to the coordination of the care planning process, assimilation of the MDS system, staff’s perceptions of the MDS system, and compliance with the regulations regarding comprehensive assessments and care plans as the core of resident care. Integration of the MDS system is reflected by increased participation of nursing, social service, activity, and dietary staff as well as restorative aides and physical therapy staff in resident assessment and care planning. Integration of the MDS system also promotes a belief within the facility that the staff can help residents to maintain or improve mobility, continence, and cognition.
Supplementary Material
Acknowledgments
The study reported in this article is part of a larger project, Care Planning Integrity & Nursing Home Resident Outcomes, supported by Grant 5RO1 NR008028 that is funded by the National Institute of Nursing Research to the University of Kansas School of Nursing and to Roma Lee Taunton, PhD, RN, FAAN, principal investigator.
Thank you to the care planning team members and other staff at the participating nursing homes who provided the primary data for this research. Thank you also to Linda Adams-Wendling, PhD, RN, CNHA, associate professor, Emporia State University Newman Division of Nursing; Nancy Dunton, PhD, associate professor, University of Kansas School of Nursing; Katy Nguyen, RN, clinical consultant, Minimum Data Set for Resident Assessment and Care Screening and quality research team, University of Missouri School of Nursing; and Daniel L. Swagerty, MD, MPH, professor, University of Kansas School of Medicine, for their invaluable contributions in the conceptualization and early phases of the project. Thank you to Valorie Coffland, Mary Lucas, Katie Luna, Patricio Padilla, and Sara Pedram for their dedication and diligence in data collection.
Footnotes
Information is available from the authors about other variables considered and eliminated as possible indicators of care planning integrity. For example, variables related to the impact of Medicare and the influence of rehabilitation therapists were examined, without success, for fit to restorative perspective.
References
- Bott MJ, Lee RH, Forbes-Thompson S, Redford L, Swagerty DL, Taunton RL. The care planning cycle in nursing facilities. 2002 Unpublished manuscript. [Google Scholar]
- Bott MJ, Piamjariyakul U, Adams-Wendling L, Gajewski B, Taunton RL. Measuring the quality of care planning using the Indiana system Unpublished manuscript. University of Kansas School of Nursing; 2005. [Google Scholar]
- Dellefield ME. Interdisciplinary care planning and the written care plan in nursing homes: A critical review. Gerontologist. 2006;46(1):128–133. doi: 10.1093/geront/46.1.128. [DOI] [PubMed] [Google Scholar]
- Glasnapp DR, Poggio JP. Essentials of statistical analysis for the behavioral sciences. Columbus, OH: Charles, E. Merill Publishing Co.; 1985. pp. 510–513. [Google Scholar]
- Harrington C, Carillo H. The regulation and enforcement of federal nursing home standards: 1991–1997. Medical Care Research and Review. 1999;56(4):471–494. doi: 10.1177/107755879905600405. [DOI] [PubMed] [Google Scholar]
- Harrington C, Carrillo H, Thollaug S, Summers P, Wellin V. Nursing facilities staffing, residents, and facility deficiencies. San Francisco: Department of Social and Behavioral Sciences, University of California; 2000. [Google Scholar]
- Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2000;55(5):S278–S287. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Indiana State Department of Health. Report card formula. Indianapolis, IN: Indiana State Department of Health, Long-term Care Division; 2003. [Google Scholar]
- Kane RL, Chen Q, Blewett LA, Sangl J. Do rehabilitative nursing homes improve the outcomes of care? Journal of the American Geriatrics Society. 1996;44(5):545–554. doi: 10.1111/j.1532-5415.1996.tb01440.x. [DOI] [PubMed] [Google Scholar]
- Nursing Home Report Cards. (n.d.) Retrieved January 10, 2003, from http://www.state.in.us/isdh/regsvcs/ltc/repcard/rptcrd. [Google Scholar]
- Omnibus Budget Reconciliation Act. Facility guide to OBRA regulations, interpretive guidelines, and the LTC survey process. Miamisburg, OH: Heaton Resources, MEDPASS, Inc; 2001. [Google Scholar]
- Piamjariyakul U, Bott MJ, Taunton RL. Strategies for an Internet-based, computer-assisted telephone survey. Western Journal of Nursing Research. 2006;28(5):602–609. doi: 10.1177/0193945906288582. [DOI] [PubMed] [Google Scholar]
- Swagerty DL, Lee RH, Smith B, Taunton RL. The context for nursing home resident care: The role of leaders in developing strategies. Journal of Gerontological Nursing. 2005;31(2):40–48. doi: 10.3928/0098-9134-20050201-09. [DOI] [PubMed] [Google Scholar]
- Taunton RL. Care planning integrity & nursing home resident outcomes (Grant # 5 R01 NR08028 awarded by the NIH National Institute of Nursing Research to the University of Kansas School of Nursing) Kansas City, KS: University of Kansas Medical Center; 2002–2007. [Google Scholar]
- Taunton RL, Bott MJ, Koehn ML, Miller P, Rindner E, Pace K, et al. The NDNQI-adapted index of work satisfaction. Journal of Nursing Measurement. 2004;12(2):101–122. doi: 10.1891/jnum.2004.12.2.101. [DOI] [PubMed] [Google Scholar]
- Taunton RL, Piamjariyakul U, Gajewski B, Bott MJ. Impact of the registered nurse coordinator and helper on the quality of care planning. Unpublished manuscript. University of Kansas School of Nursing; 2006. [Google Scholar]
- Taunton RL, Swagerty DL, Lasseter JA, Lee RH. Continent or incontinent? That is the question. Journal of Gerontological Nursing. 2005;31(9):36–44. doi: 10.3928/0098-9134-20050901-08. [DOI] [PubMed] [Google Scholar]
- Taunton RL, Swagerty DL, Smith B, Lasseter JA, Lee RH. Care planning for nursing home residents: Incorporating the minimum data set requirements into practice. Journal of Gerontological Nursing. 2004;30(12):40–49. doi: 10.3928/0098-9134-20041201-09. [DOI] [PubMed] [Google Scholar]
- Thompson SA, Oliver DP. A new model for long-term care: Balancing palliative and restorative care delivery. Journal of Housing for the Elderly. (in press) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.