Abstract
Background
Depressive symptoms display heterogeneous trajectories across adolescence and early adulthood. Identifying risk and protective factors for distinct trajectory groups, and their respective outcomes, may provide insight into the etiological underpinnings of different symptom courses and inform the targets and timing of intervention.
Methods
A school-based sample of 719 adolescents completed four diagnostic evaluations and up to 7 annually mailed questionnaires assessing psychiatric symptoms and psychosocial risk and protective factors. Parental history of psychiatric disorder was assessed. Growth mixture modeling (GMM) was used to identify latent depressive symptom trajectories from mid-adolescence through age 30, as well as their predictors in mid-adolescence and adult outcomes.
Results
A three class model consisting of high stable (32%), moderate decreasing (44%), and low decreasing (24%) depressive symptom trajectories emerged as the preferred solution. Demographic, psychosocial, and psychiatric characteristics differentiated the low and high symptom classes, and provided support for interpersonal models of depression chronicity. Members of the moderate and high symptom classes evidenced the worst psychosocial and psychiatric outcomes by age 30, with members of the high symptom class showing the greatest levels of impairment.
Limitations
Cross-sectional measurement and floor effects of several predictor variables may have obscured the relations between those predictors and trajectory class membership.
Conclusion
These findings suggest that prevention and intervention strategies may specifically target young women and those who experience poor interpersonal functioning in an effort to alter the course of depressive symptoms through early adulthood.
Keywords: Depression, Trajectories, Adolescence, Emerging adulthood, Growth mixture model
1. Introduction
Depression is a highly prevalent and impairing condition (Kessler et al., 2003). The onset of major depressive disorder (MDD) increases rapidly in adolescence and early adulthood (Hankin et al., 1998), making these critical periods to focus on the etiology and developmental course of depression. The general trajectory of depressive symptoms increases in early and middle adolescence and then decreases through early adulthood (Ge et al., 1994, 2006; Hankin et al., 1998; Pettit et al., 2010). A growing body of evidence is consistent with heterogeneity in the course of depressive symptoms, which is manifested by multiple subgroup trajectories within the general trajectory (Brendgen et al., 2005; Costello et al., 2008; Repetto et al., 2005; Rodriguez et al., 2005; Stoolmiller et al., 2005).
The identification of distinct trajectories of depressive symptoms may lead to more effective ways to prevent and treat depression. Knowledge of which adolescents are most likely to experience elevated symptom courses, as well as which courses lead to the greatest levels of impairment, would permit a more accurate identification of high-risk groups. Better understanding of the developmental timing of symptom increases and decreases would provide useful information for planning the timing of prevention and intervention efforts. Furthermore, the identification of trajectory-specific risk and protective factors may provide insight into the etiological underpinnings of different symptom courses. In conjunction, this information may allow clinicians to make more informed decisions about the intended recipients, therapeutic targets, and timing of their prevention and intervention efforts.
Several studies have examined heterogeneity in depressive symptom trajectories among adolescents and young adults. Among young adolescents (Brendgen et al., 2005) and high school students (Repetto et al., 2005; Rodriguez et al., 2005), stable high and stable low classes have been identified consistently, and some studies have identified stable moderate or increasing trajectory classes. Predictors of membership in elevated trajectory classes in adolescence include female gender, anxious symptoms, low self-esteem, high stress, and poor relationship quality with parents (Brendgen et al., 2005; Repetto et al., 2005).
A few studies have examined trajectory classes of depressive experiences from adolescence into emerging adulthood. Among 206 men from ages 15–24 years, Stoolmiller et al. (2005) identified four depressive symptom classes corresponding to very low, moderate decreasing, high decreasing, and high persistent. Predictors of membership in the high persistent class included lower family income, lower childhood academic achievement, higher childhood depressive symptoms, higher negative life events, and a higher number of changes in parental figures during childhood. Members of the high persistent and high decreasing classes displayed elevated rates of lifetime MDD in emerging adulthood, as compared to members of the moderate and low classes. Two studies (Costello et al., 2008; Wickrama et al., 2009) examined depression trajectories using data from the National Longitudinal Study of Adolescent Health, a nationally representative sample of youth ages 12–19 who were tracked for six years. Costello et al. identified four distinct depressed mood classes consisting of no depressed mood, stable low, early high declining, and late escalating. Significant predictors of elevated depressed mood trajectories included female gender, ethnic minority status, delinquent behavior, and substance use in adolescence. Protective factors that were associated with a decreased likelihood of elevated depressed mood included higher socioeconomic status, residing in a two-parent household, higher perceived social connection, and higher self-esteem. In the same sample, Wickrama et al. constructed four a priori depressive symptom trajectory groups corresponding to chronically high, increasing, decreasing, and consistently low symptom levels. Membership in the elevated classes was associated with ethnic minority status, female gender, and higher levels of poverty and parental rejection at baseline, and also with higher levels of physical health problems at the final assessment point.
Thus, although all prior studies on the transition from adolescence into emerging adulthood identified four depressive symptom trajectory classes, the nature of the classes differed somewhat across studies. Moreover, past studies have been limited by a small sample size and an exclusive focus on men (Stoolmiller et al., 2005), measurement of depressed mood rather than the spectrum of depressive symptoms (Costello et al., 2008), and little or no data on psychiatric history and adulthood outcomes of trajectory class membership. The absence of data on psychiatric history prevents conclusions about whether significant predictors of class membership may have been artifacts of pre-existing psychiatric disorders.
The primary purpose of the present study was to extend past research in this area by identifying specific classes of depressive symptom trajectories from mid-adolescence through age 30. Based on prior research, we expected to identify trajectory classes corresponding to stable low and stable high symptoms. We also expected to identify a decreasing symptom class based on the decreasing general trajectory of depressive symptoms seen in emerging adulthood. Because some researchers have also identified an increasing trajectory, we expected that might constitute a fourth class in our sample.
A secondary purpose of the present study was to identify adolescent predictors of trajectory class membership and clinically relevant outcomes at age 30 as a function of trajectory class membership. Predictors and outcomes selected for this study fall within four groups listed in Table 1: status attributes; personal and cognitive resources or stressors; social resources or stressors; and personal and parental psychiatric history. Each predictor was selected on the basis of prior research or theory linking it to elevated depressive symptoms and was therefore expected to differentiate the lowest severity trajectory class from higher severity trajectory classes. Multiple studies have found that female gender, impaired social relationships, and low self-esteem significantly distinguished class membership (Costello et al., 2008; Repetto et al., 2005; Wickrama et al., 2009). We expected those findings to replicate in the present study. Based on interpersonal models of depression chronicity (Coyne, 1976; Joiner, 2000; Lewinsohn and Atwood, 1969; Libet and Lewinsohn, 1973; Pettit and Joiner, 2006), in which maladaptive interpersonal behaviors are posited to maintain depressive symptoms over time, we hypothesized that a history of MDD and indicators of poor interpersonal functioning in adolescence would predict membership in a high severity trajectory class even after controlling for predictors from other domains. Finally, we hypothesized that members of a high severity trajectory class would display significantly greater impairment on age 30 outcomes as compared to members of lower severity trajectory classes.
Table 1.
Adolescent risk factors and early adulthood outcomes.
| Status Attributes | Personal and cognitive Resources or stressors | Social resources or stressors | Psychiatric and family history |
|---|---|---|---|
| Adolescent risks | |||
| Age | Academic impairment | Family support | Lifetime ANX |
| Gender | Coping skills | Friend support | Lifetime DBD |
| Dysfunctional attitudes | Interpersonal dependency | Lifetime MDD | |
| Health impairment | Loneliness | Lifetime SUD | |
| Self-esteem | Parental lifetime ANX | ||
| Parental lifetime | |||
| MDD | |||
| Parental lifetime SUD | |||
| Adult outcomes | |||
| Education level | Coping skills | Daily hassles | No. of lifetime ANX episodes |
| Income | Dysfunctional attitudes | Major life events | No. of lifetime SUD episodes |
| Marital status | Self-esteem | SAS family | No. of lifetime MDD episodes |
| SAS social/leisure | |||
| SAS work | |||
Note: ANX = anxiety disorder; DBD = disruptive behavior disorder; MDD = major depressive disorder; SUD = substance use disorder; SAS = social adjustment scale.
To test these predictions, we applied growth mixture modeling (GMM) to data from the Oregon Adolescent Depression Project (OADP) to jointly examine specific classes of depressive symptom trajectories. Key advantages of the OADP over prior investigations include the extension of data collection through age 30, inclusion of both women and men, the presence of a well-validated measure of depressive symptoms, and the repeated assessment of psychiatric disorders with structured clinical interviews. In addition, a substantially larger array of potential predictors and outcomes of trajectory class membership are available in the OADP than in previous studies.
2. Method
2.1. Participants
OADP probands were randomly selected from high schools in western Oregon. A total of 1709 adolescents (ages 14–18 years; mean age = 16.6) completed an initial (T1) assessment between 1987 and 1989. Approximately one year later, 1507 (88%) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined to participate or dropped out of the study before T2, were negligible (Lewinsohn et al. 1993). At age 24, all adolescents with a history of Axis I psychopathology by T2 (n = 644) and a random sample of adolescents with no history of psychopathology by T2 (n = 457) were invited to participate in a third (T3) evaluation. Of the 1101 T2 probands selected for a T3 interview, 941 (85%) completed the evaluation. At age 30, all T3 probands were invited to participate in a T4 evaluation. Of the 941 T3 probands, 816 (87%) completed the T4 diagnostic interview. The 816 T4 probands included 479 (59%) women. Among those invited to T3 and T4 assessments, women were more likely than men to complete evaluations, χ2 > 5.99, p’s < .05; participation did not differ as a function of other demographic variables or previous diagnoses. In addition to the four major assessment points, probands were asked to complete seven annual questionnaires that included the Center for Epidemiological Studies Depression scale (CES-D; Radloff, 1977). The period covered by the annual questionnaires ran on average from ages 21–28 (mean age at first mailer = 21.53 years, standard deviation = 1.51 years).
Seven-hundred nineteen probands who completed the four major assessments and had data available for all adolescent predictor variables represent the reference sample for this report1. Ninety-seven percent of the 719 probands completed at least four annual questionnaires, meaning that data from at least eight assessment points were available for almost all probands. This research was conducted as approved by the institutional review board.
2.2. Psychiatric measures
2.2.1. Depressive symptoms
The CES-D (Radloff, 1977) is a widely-used self-report measure of the frequency of 20 depressive symptoms that has been validated in adolescent and young adult samples (e.g., Roberts et al., 1991; Joiner et al., 2005). The CES-D was completed at up to 10 assessment waves (T1, T2, T4, and seven annual mailers) (α = .91–.92).
2.2.2. Proband diagnostic interviews
At T1, T2, and T3, probands were interviewed with a version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Orvaschel et al., 1982; Chambers et al., 1985). In conjunction with the K-SADS, the Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987) was used to evaluate the presence and course of disorders since participation in the previous diagnostic interview. T4 diagnostic assessments were based on the Structured Clinical Interview for Axis I DSM-IV Disorders—Non-Patient Edition (SCID-NP; First et al., 1995), with the LIFE also used to evaluate disorder presence and course since T3. Symptom endorsements during these interviews were subsequently evaluated in conjunction with DSM-III-R criteria (American Psychiatric Association, 1987) at T1 and T2 and DSM-IV criteria (American Psychiatric Association, 1994) at T3 and T4. Interviews at T3 and T4 were conducted by telephone, which generally provides comparable validity to face-to-face interviews (Sobin et al., 1993; Rohde et al., 1997).
2.2.3. Parental diagnostic interview
Lifetime psychiatric disorders in the biological parents of probands were assessed near the time of the T3 evaluation. Parents were directly interviewed using a version of the non-patient edition of the Structured Clinical Interview for DSM-III-R (SCID-NP) that had been modified for DSM-IV criteria (Spitzer et al., 1992). Parent history data were collected using the Family Informant Schedule and Criteria (FISC; Mannuzza and Fyer, 1990), supplemented with all items necessary to derive DSM-IV diagnoses. Five hundred forty-eight (76%) parents completed the SCID-NP, and psychiatric histories via the FISC were collected on all parents. As multiple data sources were available for most parents, lifetime best-estimate DSM-IV diagnoses were derived independently by two senior diagnosticians from all available information (Leckman et al., 1982).
3. Psychosocial predictors assessed in adolescence
An extensive battery of psychosocial measures was administered to probands at T1 (see Lewinsohn et al., 1994). Several measures of psychosocial functioning were either developed specifically for the purposes of the OADP or were adapted from pre-existing measures of psychosocial functioning. Four scales described below were developed from items administered to the OADP sample at T1. Past work has supported the single factor structure and internal reliability of each scale (see Mathew et al., 2011).
3.1. Family social support
This construct was measured with eight continuously-scored items. Example items include “How well do you get along with your siblings?” and “How well do you get along with your parents?”
3.2. Friend social support
This construct was assessed with seven continuously-scored items. Example items include “How many close friends do you have?” and “How well do you get along with other kids?”
3.3. Academic problems
This construct was assessed with seven items, such as “How many days of school did you miss over the last 6 weeks?” and “Were you satisfied with your grades?”
3.4. Health problems
This construct was assessed with six items, including “During the past 12 months, have you been treated for any illness, condition, or injury?” and “In the past year, have you been unable to work and/or participate in school activities because of some illness or injury?”
In addition to the four scales developed for the OADP, several well-validated and extensively used measures of psychosocial functioning were included. These measures and their reliability in the OADP sample have been described in detail in previous publications (Andrews et al., 1993; Lewinsohn et al., 1994). A brief description of each construct is given below.
3.5. Coping
Coping skills assessed the ways in which individuals cope with stressful situations, using 17 items originally selected from the self-control scale (Rosenbaum, 1980), the Antidepressive Activity Questionnaire (Rippere, 1977), modified by Parker and Brown (1979), and the Ways of Coping Questionnaire (Folkman and Lazarus, 1980).
3.6. Dysfunctional attitudes
Intensity of dysfunctional attitudes was assessed with nine items from the dysfunctional attitudes scale (DAS; Weissman and Beck, 1978).
3.7. Interpersonal dependency
The extent to which probands desired more support and approval from others, were anxious about being alone or abandoned, and were interpersonally sensitive was assessed with the emotional reliance subscale of the Interpersonal Dependency Inventory (Hirschfeld et al., 1977).
3.8. Loneliness
The adapted UCLA loneliness scale (Roberts et al., 1993) is an 8-item scale which measures feelings of solitude, disconnection, and lack of closeness.
3.9. Self-esteem
This scale assessed satisfaction with specific body parts (3 items; body parts satisfaction scale; Berscheid et al., 1973), general satisfaction with physical appearance (3 items; physical appearance evaluation subscale; Winstead and Cash, 1984), and global self-esteem (3 items; self-esteem scale, Rosenberg, 1965).
4. Distal outcomes assessed at age 30
At the time of the T4 assessment (mean age = 30 years), probands were asked to complete a questionnaire that elicited information about marital status, highest level of educational attainment, and household income. Additional constructs assessed at T4 included the following measures with established reliability and validity in the OADP sample: Coping (described above); Daily Hassles (unpleasant events schedule; Lewinsohn et al., 1985); dysfunctional attitudes (described above); major life events (Andrews et al., 1993); self-esteem (10 items from Rosenberg, 1965); and the social adjustment scale (SAS; Weissman and Bothwell, 1976).
5. Analytic approach
GMM was used to identify classes of depressive symptom trajectories, predictors of class membership, and outcomes of class membership using the statistical software program Mplus, Version 6.1 (Muthén and Muthén, 1998–2010). Given the stratified sampling procedure used at T3, weights reflecting the probability of selection for the T3 follow-up were used in analyses. Full Information Maximum Likelihood was used to estimate missing values that were missing at random and comprised on average 4.63% of the sample2.
Based on visual inspection of raw individual plots and preliminary analyses of single-group trajectory models, a quadratic growth model that specified time scores to assessment waves was fit and used in subsequent analyses, χ2(46) = 154.46, p < .0000; CFI = .96, RMSEA = .06. Class enumeration of the unconditional GMM was conducted through inspection of elbow plots of Bayesian Information Criterion (BIC) and sample-size adjusted BIC (adj. BIC), as well as through Lo–Mendell–Rubin (LMR) and Bootstrap likelihood ratio tests (BLRT) of k and k−1 class solutions (Nylund et al. 2007; Tofighi and Enders, 2008). Lower BIC and adj. BIC values are indicative of better model fit, and less pronounced declines in these values on the elbow plot indicate diminishing gains from estimating additional classes. Growth parameter invariance was tested across classes (Enders and Tofighi, 2008; Morin et al., 2011). Intercept, slope, and quadratic factor variances were fixed to zero values in the first class of models with two or more classes. This constraint was needed to identify growth parameters in the higher classes, and to allow them to freely vary. As was the case for Morin et al. (2011), these equality constraints led the first class to represent the low symptom severity cases, which consisted of probands who never endorsed clinically meaningful levels of depressive symptoms (i.e., CES-D > 16).
5.1. Predictors of class membership
Multinomial logistic regressions were used to identify predictors of trajectory class membership. Unless otherwise stated, the first class that described the low symptom severity group was used as the reference category. All continuous predictors were centered at their respective means to enhance interpretability. Categorical and count predictors retained their original scaling. Given the large number of potential predictors, pseudo-class regressions were first used to winnow down the pool of independent variables (Clark and Muthén, unpublished manuscript). Significant predictors were then entered directly into the GMM model, which allowed for a test of stability of the class solution and causal ordering of the predictors (Marsh et al., 2009). This approach allowed us to retain a high level of power to detect significant effects, without presenting undue bias to regression estimates (Clark and Muthén, unpublished manuscript).
5.2. Outcomes of class membership
Distal outcomes of class membership were entered directly into the model that included predictors of trajectory class membership and were allowed to covary freely within each class. In doing so, the distal outcomes served as indicators of latent trajectory classes, which provided an additional test of the stability of the unconditional GMM (Muthén, 2004). While alternate approaches that test equality of means across latent classes exist (cf. Petras and Masyn, 2010; Morin et al., 2011), their application assumes conditional independence among the outcomes that was not evidenced in our data.
6. Results
6.1. Identification of trajectory classes
Unconditional GMMs that estimated 1–5 classes were examined (see Table 2). Stable solutions were obtained for all but the 5-class model, which failed to converge even after the number of random starts was increased to 4000, and was therefore removed from further consideration. Heywood cases in the form of negative growth factor variances were observed in the second and third class of the 4-class model, and required constraints to zero values in order to reach a positive definite psi matrix.
Table 2.
Criteria used to decide on optimal solution for number of latent classes.
| Number of classes | BIC | Adj. BIC | BLRT | LMR | Entropy |
|---|---|---|---|---|---|
| 1 | 46378.41 | 46318.08 | – | – | – |
| 2 | 46143.38 | 46070.34 | 261.35*** | 251.78*** | .69 |
| 3 | 45957.02 | 45852.23 | 87.62*** | 84.41*** | .70 |
| 4a | 45952.44 | 45850.83 | 73.25*** | 41.68* | .73 |
Note: Adj. BIC = Sample size adjusted Bayesian Information Criteria. BLRT = Boot-strap likelihood ratio test. LMR = Lo-Mendell-Rubin likelihood ratio test.
p < .01.
Negative growth factor v**ariance and covariance were constrained to 0 in Classes 2–3.
p < .001.
Inspection of relative fit indices for the 1–4 class models provided mixed findings with regard to the preferred number of classes (see Table 2). While BIC and adj. BIC evidenced diminishing gains in estimating classes beyond a 3-class model, significant LMR and BLRT values indicated preference for the 4-class solution. Given the presence of inadmissible values in the 4-class solution, we retained the three-class solution as the preferred unconditional model. Growth parameters were non-invariant across the second and third class of the 3-class solution, which supported the need to retain class-specific growth parameters (χ2 [6] = 127.61, p < .0001) Table 3.
Table 3.
Unconditional general mixture model growth parameter estimates.
| Factor means | Class 1
|
Class 2
|
Class 3
|
M. Wald | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Est | SE | Std | Est | SE | Std | Est. | SE | Std | ||
| INT | 5.09*** | .32 | — | 10.77*** | .43 | 4.16 | 18.31*** | .64 | 2.31 | 429.32***a,b,c |
| SLO | −.49*** | .04 | — | −.59*** | .07 | −1.03 | −.13 | .09 | −.14 | 14.85***b,c |
| QUA | .01 | .01 | — | .02 | .01 | .24 | .02 | .01 | .14 | |
| INT | — | — | — | 6.70** | 2.25 | — | 62.89*** | 7.03 | — | — |
| SLO | — | — | — | .34*** | .08 | — | .75*** | .14 | — | — |
| QUA | — | — | — | .01*** | .00 | — | .03*** | .01 | — | — |
| Factor covariance | ||||||||||
| INT ↔ SLO | — | — | — | .38 | .27 | .27 | −1.53** | .65 | −.22 | — |
| INT↔ QUA | — | — | — | −.12* | .05 | −.63 | −.98*** | .15 | −.69 | — |
| SLO ↔ QUA | — | — | — | −.03** | .02 | −.65 | .07*** | .01 | .44 | — |
Note: INT = intercept, SLO = slope, QUA = quadratic, Est = estimate, SE = standard error, Std = standardized estimate. Due to the centering approach, intercept values represent scores at wave 5 (year 7). Class 1 = low decreasing; Class 2 = moderate decreasing; Class 3 = high stable. M. Wald = Multivariate Wald χ2 (df = 2).
Class 1 variance constrained to 0 for identification purposes.
C1 vs. C2, p < .0001.
C1 vs. C3, p ≤ .0002.
C2 vs. C3, p ≤ .004.
p < .001.
p < .01.
p < .05
The three trajectory classes, displayed in Fig. 1, were labeled high stable (n = 232, 32%), moderate decreasing (n = 314, 44%), and low decreasing (n = 173, 24%). These designations were based on the sign and significance of the intercept and slope parameters. Depressive symptoms decreased sharply across the first two measurement periods for all classes, but subsequently displayed class-specific trends (see Fig. 1). To reduce the influence of the dramatic decrease in depressive symptoms across the first two time points, the data were re-centered from the first assessment wave to the middle assessment wave (wave 5 or year 7 in Fig. 1; cf. Biesanz et al., 2004 for discussion on effects of centering on growth parameters). Re-centering did not change class membership or model fit.
Fig. 1.
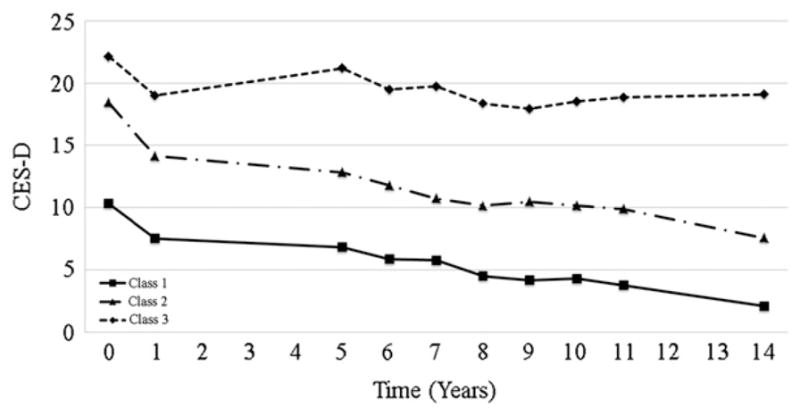
Growth Trajectories of CES-D Scores for the 3 class unconditional GMM. Class 1 = low decreasing; Class 2 = moderate decreasing; Class 3 = high stable.
Unconditional GMM results are presented in Table 2. Those in the high stable class began their trajectories at more severe levels of depressive symptoms that remained at higher levels at the middle measurement period than for those in the moderate and low decreasing classes, Wald χ2 (1) = 8.44–372, p < .01–.001. This pattern was also observed between those in the moderate and low decreasing classes, Wald χ2 (1) = 49.49–171.18, p < .001.
Significant differences in slope parameters were found across the classes, Wald χ2 (2) = 14.85, p < .001. Members of the high stable class maintained a steady level of depressive symptoms that did not significantly change over time (b = −.13, p = .15). Slope parameters for the moderate decreasing and low decreasing classes evidenced negative trajectories that did not significantly differ from one another in magnitude, (b = −.49to −59, p < .001, Wald χ2 [1] = 1.70, p = .19). These findings suggest that regardless of initial level of symptom severity in mid-adolescence, depressive symptoms declined during the transition from late adolescence to emerging adulthood (T1–T2), but stabilized thereafter for the high stable class. In contrast to the high stable class, depressive symptoms continued to decrease during emerging adulthood for the moderate decreasing and low decreasing classes.
6.2. Adolescent predictors of trajectory class membership
Adolescent risk factors were first tested through pseudo-class regressions within their respective risk/protective factor families (see Table 1). Of the initial 18 predictors, eight remained significant within their respective families. The ten non-significant predictors included age, four personal and cognitive variables (academic impairment, dysfunctional attitudes, health impairment, and self-esteem), two social variables (family support and friend support), and three psychiatric and family history variables (lifetime anxiety disorder, lifetime disruptive behavior disorder, and lifetime parental anxiety disorder). These nine variables were excluded from subsequent analyses.
The eight significant predictors from within-family analyses were retained and entered simultaneously as predictors of latent class membership. As expected, and in support of the validity of the distinction between the three classes, the majority of risk factors significantly predicted membership in the high stable and moderate decreasing classes versus membership in the low decreasing class (see Table 4). Compared to those in the low decreasing class, those in the high stable class were more likely to be women, endorsed lower levels of coping, and reported greater levels of loneliness and interpersonal dependency. Individuals in the high stable class were also more likely than those in the low decreasing class to endorse personal and parental histories of MDD and substance use disorders. The same adolescent risk factors significantly distinguished the moderate decreasing class from the low decreasing class, with exception of gender and parental history of substance abuse, which did not reach statistical significance. Finally, as compared to the moderate decreasing class, members of the high stable class were significantly more likely to be women, to report more loneliness, and to endorse more interpersonal dependency (at a nonsignificant trend level).
Table 4.
Predictors of latent class membership.
| Predictor | Odds ratio (95% confidence interval)
|
||
|---|---|---|---|
| 1 vs. 2a | 1 vs. 3a | 2 vs. 3b | |
| Female gender | 1.02 (.57–1.82) | 1.92*(1.02–3.62) | 1.89** (1.19–3.00) |
| Personal and cognitive | |||
| Coping | .95** (.91–.99) | .94** (.89–.99) | .99 (.96–1.03) |
| Social | |||
| Interpersonal dependency | 1.11** (1.05–1.18) | 1.16** (1.08–1.23) | 1.04† (1.00–1.08) |
| Loneliness | 1.12** (1.02–1.22) | 1.21** (1.11–1.33) | 1.09* (1.01–1.17) |
| Psychopathology | |||
| Major depressive disorder | 3.94** (1.37–11.32) | 3.97** (1.33–11.85) | 1.01 (.60–1.68) |
| Substance abuse disorder | 6.02* (1.12–32.35) | 8.51** (1.61–45.02) | 1.41 (.74–2.71) |
| Parental psychopathology | |||
| Major depressive disorder | 1.67* (1.06–2.63) | 1.99** (1.21–3.26) | 1.19 (.82–1.72) |
| Substance buse disorder | 1.40 (.92–2.14) | 1.76* (1.12–2.76) | 1.26 (.86–1.87) |
Note: Class 1 = low decreasing; Class 2 = moderate decreasing; Class 3 = high stable.
p = .06.
Class 1 is the reference class.
Class 2 is the reference class.
p < .01.
p < .05.
6.3. Distal outcomes of trajectory class membership
Mean scores or prevalence rates on distal outcomes in each trajectory class are presented in Table 5. Members of the high stable and moderate decreasing classes significantly differed from members of the low decreasing class on every outcome. As compared to members of the low decreasing class, those in the high and moderate symptom classes attained a lower level of education, reported lower annual household income, displayed poorer adjustment on each psychosocial measure, and experienced higher numbers of MDD, anxiety, and substance use disorder episodes. Members of the high stable class were also more likely to be separated or divorced than those in the low decreasing class. The same pattern of outcomes emerged when members of the moderate decreasing class were compared to those in the high stable class.
Table 5.
Mean scores on or prevalence of distal outcomes as a function of latent class membership.
| Outcome | Class 1 | Class 2 | Class 3 | M. Wald |
|---|---|---|---|---|
| Status variables | ||||
| Education | ||||
| Grade 7 to 12 (no diploma) | 0% | 3% | 2% | 166.93***a,b |
| High school/GED | 1% | 12% | 18% | 11.45*c |
| Trade school | 0% | 4% | 4% | 16.93***c |
| Part college | 23% | 30% | 35% | 31.41*** a,b,c |
| 2 year college | 3% | 9% | 7% | 37.66*.** a,b,c |
| 4 year college | 50% | 26% | 27% | 12.65** a,b,c |
| Part graduate school | 1% | 4% | 3% | 17.33*** a,b,c |
| Completed graduate school | 22% | 12% | 5% | — |
| Income‡ | ||||
| Lower class ($0–$14,999) | 2% | 9% | 20% | 16.86***c |
| Working class ($15,000–$29,999) | 5% | 18% | 31% | 45.78*** a,b,c |
| Middle class or higher ($30,000 or more) | 93% | 74% | 49% | — |
| Marital status | ||||
| Never married | 18% | 36% | 39% | 4.93 |
| Married | 73% | 56% | 44% | 17.64***b,c |
| Separated/divorced | 3% | 8% | 17% | — |
| Personal and cognitive | ||||
| Coping | 54.06*** | 50.54*** | 45.20*** | 84.60*** a,b,c |
| Dysfunctional attitudes | 50.67*** | 47.91*** | 43.06*** | 55.29*** a,b,c |
| Self-esteem | 38.12*** | 34.77*** | 28.13*** | 172.30*** a,b,c |
| Social | ||||
| Daily hassles | 35.48*** | 41.18*** | 50.45*** | 86.23*** a,b,c |
| No. of major events | 1.89*** | 2.83*** | 4.19*** | 59.12*** a,b,c |
| SAS family | 1.28*** | 1.44*** | 1.77*** | 102.47*** a,b,c |
| SAS work | 1.50*** | 1.73*** | 2.15*** | 106.75*** a,b,c |
| SAS social/leisure | 1.65*** | 1.82*** | 2.19*** | 65.55*** a,b,c |
| Psychopathology | ||||
| No. of ANX episodes | .02*** | .13*** | .53*** | 53.37*** a,b,c |
| No. of MDD episodes | .19*** | .68** | 1.53*** | 62.99*** a,b,c |
| No. of SUD episodes | .45*** | .79* | 1.27* | 24.24*** a,b,c |
Note. SAS = social adjustment scale, ANX = anxiety disorder, MDD = major depressive disorder, SUD = substance use disorder; Class 1 = low decreasing; Class 2 = moderate decreasing; Class 3 = high stable. M. Wald = multivariate wald χ2 (df = 2) and represents differences in the likelihood of falling at a higher category of education, income, or marital status.
Income classes based on Thompson and Hickey (2005). Significance level of independent contrasts presented after Benjamin-Hochberg correction (α = .05).
C1 vs. C2, p ≤ .04.
C1 vs. C3, p ≤ .04.
C2 vs. C3, p ≤ .03.
p < .001.
p < .01.
p < .05.
7. Discussion
The purposes of the present study were to identify groups of individuals who share distinct trajectories of depressive symptoms from adolescence through early adulthood and to describe these groups with respect to their predictors in adolescence and their outcomes in early adulthood. Support was obtained for three depressive symptom trajectory classes: low decreasing, moderate decreasing, and high stable. The nature of classes in the present study was similar to that of past work on depressive symptoms (Stoolmiller et al., 2005) and indicated a clear ordering of classes (i.e., at no point did the trajectories of different classes cross one another).
While the number of classes differed somewhat from the four class solution retained by others (i.e., Costello et al., 2008; Stoolmiller et al., 2005; Wickrama et al., 2009), this may be due to differences in sample characteristics and approaches to growth parameter specifications. For instance, in contrast to findings on stability of depressive symptoms, the nature of trajectory classes in studies that have assessed depressed mood (Repetto et al., 2005; Costello et al., 2008) reflects greater liability over time and unordered classes (i.e., trajectories of different classes crossed each other). In spite of these discrepancies, every study to our knowledge has found evidence for a persistently low symptom class and a persistently elevated symptom class, which supports the validity of these two groups.
Our findings indicate that late adolescence was accompanied by a decrease in depressive symptoms for members of all classes, and that this pattern of decreasing symptoms continued through emerging adulthood for two-thirds of the sample. For the other third of the sample (i.e., the high stable class), the decrease in symptoms halted during the transition to emerging adulthood and symptoms remained stable through age 30. Uniform declines in depressive symptoms during late adolescence and subsequent differentiation of depressive symptom trajectories during the transition to emerging adulthood have been noted others (i.e., Aseltine and Gore, 1993; Schulenberg and Zarrett, 2006). During the shift into emerging adulthood, role-transitions and changes in social contexts provide some individuals an opportunity to achieve greater autonomy and new interpersonal relationships (Arnett, 2000; Schulenberg and Zarrett, 2006), which may foster emotional well-being. For others, this transition period heralds novel stressors that strengthen existing maladaptive coping repertoires and promote distress (Schulenberg and Zarrett, 2006).
Consistent with previous findings (Costello et al., 2008; Wickrama et al., 2009), women and those with personal and parental histories of MDD and substance use disorders were overrepresented in the moderate and high trajectory classes. These findings reflect the gender imbalance in rates of depression (Nolen-Hoeksema et al., 1999) and the deleterious effects of personal (Essau, 2007; Lewinsohn et al., 2000) and familial histories of MDD and substance abuse (Beardslee et al., 1998; Su et al., 1997). Incremental to psychiatric histories, the risk conferred by interpersonal dependency, loneliness, and coping deficits for membership in the moderate and high classes is in line with interpersonal models of depression persistence (Coyne, 1976; Lewinsohn and Atwood, 1969; Libet and Lewinsohn, 1973; Pettit and Joiner, 2006).
Robust differences also emerged across the three trajectory classes in adulthood outcomes. Members of the low decreasing class uniformly displayed better psychosocial and psychiatric outcomes than those in either of the two elevated symptom classes, with members of the high stable class evidencing the worst level of functioning in adulthood. These significant differences are consistent with past findings that a more chronic course of depression predicts poorer distal outcomes (Jonsson et al., 2011; Pettit et al., 2009), and also support the predictive validity of the three classes.
The finding of differing adulthood outcomes between the moderate decreasing and high stable classes is notable, as few variables measured in adolescence distinguished these classes. In particular, academic impairment, dysfunctional attitudes, self-esteem, family support, and MDD and substance use histories in adolescence did not differentiate these classes, but the same or similar constructs assessed at age 30 did significantly differ across classes. This pattern of results suggests that persistently elevated depressive symptoms through adolescence and early adulthood may erode personal and social resources.
This study has a number of strengths, including the use of a large, school-based sample with repeated assessments over approximately 15 years. This study extends past work by assessing a range of depressive symptoms rather than sad mood, tracking participants through age 30, including women and men, assessing personal and parental psychiatric disorders using semi-structured interviews, and collecting detailed information on age 30 outcomes. In spite of these strengths, our findings should be interpreted in the context of several limitations. First, the analytic approach (GMM) is by nature exploratory and is affected by sample characteristics and variable distributions (Bauer and Curran, 2004; Tofighi and Enders, 2008). Second, we did not consider effects of psychiatric comorbidity or interaction effects of predictors in adolescence on latent trajectory classes. Future studies exploring such effects would provide a valuable extension to our work that would allow for more nuanced tests of interpersonal and cognitive models of depression. Finally, methodological limitations in the form of cross-sectional measurement and floor effects for lifetime anxiety, disruptive behavior, and parental history of anxiety disorders may have obscured the relation of these variables with the latent classes.
In summary, support was found for the existence of three depressive symptom trajectory classes from mid-adolescence through age 30. Approximately one-fourth of probands displayed persistently low depressive symptoms that decreased through early adulthood, over 40% displayed moderately elevated symptoms in adolescence that decreased through early adulthood, and about one-third displayed elevated symptoms throughout the study period. Numerous psychosocial risk factors in adolescence and personal and parental histories of psychiatric disorder distinguished probands who experienced persistently low depressive symptoms from those who experienced moderate or high symptoms. Female gender and poor interpersonal functioning in adolescence distinguished those who displayed a persistently elevated course of symptoms from those who displayed moderate symptoms in adolescence followed by a reduction in symptoms during early adulthood. Among adolescents who display elevated depressive symptoms, prevention and intervention strategies may specifically target young women and those who experience poor interpersonal functioning in an effort to alter the long-term course of depressive symptoms. Programs that address loneliness and a sense of interpersonal dependency in adolescence may hold promise for preventing a chronic course of depressive symptoms and corresponding psychosocial impairment through early adulthood.
Acknowledgments
Role of funding source
This research was supported by awards from the National Institute of Health. The funding source did not play a role in any aspect of this study.
This research was supported by NIH awards MH40501, MH50522, and MH52858 to Peter M. Lewinsohn, and MH75744 to Jeremy W. Pettit.
Footnotes
This group of participants did not significantly differ from the larger sample who completed all four assessment waves (N = 816) on any demographic, predictor, symptom, or outcome measure (ps > .10).
Given the potential for missing data to vary across classes, missing data patterns were re-analyzed using most likely class membership from the 3-class GMM that included predictors and outcomes. Patterns of missing values met the MCAR conditions for Class 1 and Class 2 (Little’s MCAR test: Class 1, χ2[838] = 873.03, p = .20; Class 2, χ2[1766] = 1635.39, p = .99), and were found to be MAR for Class 3 (all p-values non-significant after Benjamin–Hochberg correction at α = .05).
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Association; Washington, DC: 1987. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Andrews JA, Lewinsohn PM, Hops H, Roberts RE. Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychological Reports. 1993;73:1019–1046. doi: 10.2466/pr0.1993.73.3.1019. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. American Psychologist. 2000;55(5):469–480. http://dx.doi.org/10.1037/0003-066X.55.5.469. [PubMed] [Google Scholar]
- Aseltine RH, Gore S. Mental health and social adaptation following the transition from high school. Journal of Research on Adolescence. 1993;3:247–270. http://dx.doi.org/10.1207/s15327795jra0303_3. [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: a review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(11):1134–1141. doi: 10.1097/00004583-199811000-00012. http://dx.doi.org/10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. The integration of continuous and discrete latent variable models: potential problems and promising opportunities. Psychological Methods. 2004;9:3–29. doi: 10.1037/1082-989X.9.1.3. http://dx.doi.org/10.1037/1082-989X.9.1.3. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. Body image. Psychology Today. 1973;76:119–131. [Google Scholar]
- Biesanz JC, Deeb-Sossa N, Papadakis AA, Bollen KA, Curran PJ. The role of coding time in estimating and interpreting growth curve models. Psychological Methods. 2004;9:30–52. doi: 10.1037/1082-989X.9.1.30. http://dx.doi.org/10.1037/1082-989X.9.1.30. [DOI] [PubMed] [Google Scholar]
- Brendgen M, Wanner B, Morin AJS, Vitaro F. Relations with parents and with peers, temperament, and trajectories of depressed mood during early adolescence. Journal of Abnormal Child Psychology. 2005;33(5):579–594. doi: 10.1007/s10802-005-6739-2. http://dx.doi.org/10.1007/s10802-005-6739-2. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: test–retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of General Psychiatry. 1985;42 (7):696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Clark S, Muthén B. Relating Latent Class Analysis Results to Variables not Included in the Analysis. Retrieved from 〈 http://www.statmodel.com/download/relatinglca.pdf〉, unpublished manuscript.
- Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. Journal of Consulting and Clinical Psychology. 2008;76(2):173–183. doi: 10.1037/0022-006X.76.2.173. http://dx.doi.org/10.1037/0022-006X.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry: Journal for the Study of Interpersonal Processes. 1976;39 (1):28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. The impact of misspecifying class-specific residual variances in growth mixture models. Structural Equation Modeling. 2008;15(1):75–95. http://dx.doi.org/10.1080/10705510802154307. [Google Scholar]
- Essau CA. Course and outcome of major depressive disorder in non-referred adolescents. Journal of Affective Disorders. 2007;99(1–3):191–201. doi: 10.1016/j.jad.2006.09.010. http://dx.doi.org/10.1016/j.jad.2006.09.010. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research Department. New York State Psychiatric Institute; New York: 1995. Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (SCID-I/NP, Version 2.0) [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21(3):219–239. http://dx.doi.org/10.2307/2136617. [PubMed] [Google Scholar]
- Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. http://dx.doi.org/10.1037/0012-1649.30.4.467. [Google Scholar]
- Ge X, Natsuaki MN, Conger RD. Trajectories of depressive symptoms and stressful life events among male and female adolescents in divorced and nondivorced families. Development and Psychopathology. 2006;18:253–273. doi: 10.1017/S0954579406060147. http://dx.doi.org/10.1017/S0954579406060147164%207856210.1017/S0954579406060147200%206-03348-014. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. http://dx.doi.org/10.1037/0021-843X.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Klerman GL, Gouch HG, Barrett J, Korchin SJ, Chodoff P. A measure of interpersonal dependency. Journal of Personality Assessment. 1977;41:610–619. doi: 10.1207/s15327752jpa4106_6. http://dx.doi.org/10.1207/s15327752jpa4106_6. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Depression’s vicious scree: self-propagating and erosive processes in depression chronicity. Clinical Psychology: Science and Practice. 2000;7(2):203–218. http://dx.doi.org/10.1093/clipsy/7.2.203. [Google Scholar]
- Joiner TE, Walker RL, Pettit JW, Perez M, Cukrowicz KC. Evidence-based assessment of depression in adults. Psychological Assessment. 2005;17(3):267–277. doi: 10.1037/1040-3590.17.3.267. http://dx.doi.org/10.1037/1040-3590.17.3.267. [DOI] [PubMed] [Google Scholar]
- Jonsson U, Bohman H, von Knorring L, Olsson G, Paaren A, von Knorring A. Mental health outcome of long-term and episodic adolescent depression: 15-year follow-up of a community sample. Journal of Affective Disorders. 2011;130(3):395–404. doi: 10.1016/j.jad.2010.10.046. http://dx.doi.org/10.1016/j.jad.2010.10.046. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (NCS-R) JAMA: Journal of the American Medical Association. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. http://dx.doi.org/10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44 (6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Archives of General Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Atwood GE. Depression: a clinical-research approach. Psychotherapy: Theory, Research, & Practice. 1969;6(3):166–171. http://dx.doi.org/10.1037/h0088744. [Google Scholar]
- Lewinsohn PM, Mermelstein RM, Alexander C, MacPhillamy D. The unpleasant events schedule: a scale for the measurement of aversive events. Journal of Clinical Psychology. 1985;41:483–498. doi: 10.1002/1097-4679(198507)41:4<483::aid-jclp2270410407>3.0.co;2-0. http://dx.doi.org/10.1002/1097-4679(198507)41:4<483,AID-JCLP2270410407>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. http://dx.doi.org/10.1037/0021-843X.103.2.302. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102 (1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. The American Journal of Psychiatry. 2000;157(10):1584–1591. doi: 10.1176/appi.ajp.157.10.1584. http://dx.doi.org/10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- Libet JM, Lewinsohn PM. Concept of social skill with special reference to the behavior of depressed persons. Journal of Consulting and Clinical Psychology. 1973;40(2):304–312. doi: 10.1037/h0034530. http://dx.doi.org/10.1037/h0034530. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Fyer AJ. Family Informant Schedule and Criteria (July 1990 rev) New York State Psychiatric Institute, Anxiety Disorders Clinic; New York: 1990. [Google Scholar]
- Marsh HW, Lüdtke O, Trautwein U, Morin AJS. Classical latent profile analysis of academic self-concept dimensions: synergy of person- and variable-centered approaches to theoretical models of self-concept. Structural Equation Modeling. 2009;16(2):191–225. http://dx.doi.org/10.1080/10705510902751010. [Google Scholar]
- Mathew AR, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Comorbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychological Medicine. 2011;41(10):2023–2034. doi: 10.1017/S0033291711000407. http://dx.doi.org/10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin AJS, Maïano C, Nagengast B, Marsh HW, Morizot J, Janosz M. General growth mixture analysis of adolescents’ developmental trajectories of anxiety: the impact of untested invariance assumptions on substantive interpretations. Structural Equation Modeling. 2011;18(4):613–648. http://dx.doi.org/10.1080/10705511.2011.607714. [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for The Social Sciences. Sage Publications; Newbury Park, CA: 2004. pp. 345–368. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Muthén & Muthén; Los Angeles, CA: 1998–2010. [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77(5):1061–1072. doi: 10.1037//0022-3514.77.5.1061. http://dx.doi.org/10.1037/0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child and Adolescent Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. http://dx.doi.org/10.1016/S0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Parker G, Brown LB. Repertoires of responses to potential precipitants of depression. Australian & New Zealand Journal of Psychiatry. 1979;13:327–333. doi: 10.3109/00048677909159155. [DOI] [PubMed] [Google Scholar]
- Petras H, Masyn K. General growth mixture analysis with antecedents and consequences of change. In: Piquero A, Weisburd D, editors. Handbook of Quantitative Criminology. Springer; New York: 2010. pp. 69–100. [Google Scholar]
- Pettit JW, Joiner TE. Chronic Depression: Interpersonal Sources, Therapeutic Solutions. American Psychological Association; Washington, DC, US: 2006. [DOI] [Google Scholar]
- Pettit JW, Lewinsohn PM, Roberts RE, Seeley JR, Monteith L. The long-term course of depression: development of an empirical index and identification of early adult outcomes. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2009;39(3):403–412. doi: 10.1017/S0033291708003851. http://dx.doi.org/10.1017/S0033291708003851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE, Yaroslavsky I. Developmental relations between depressive symptoms, minor hassles, and major events from adolescence through age 30 years. Journal of Abnormal Psychology. 2010;119(4):811–824. doi: 10.1037/a0020980. http://dx.doi.org/10.1037/a0020980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Repetto PB, Caldwell CH, Zimmerman MA. A longitudinal study of the relationship between depressive symptoms and cigarette use among African American adolescents. Health Psychology. 2005;24(2):209–219. doi: 10.1037/0278-6133.24.2.209. http://dx.doi.org/10.1037/0278-6133.24.2.209. [DOI] [PubMed] [Google Scholar]
- Rippere V. Some cognitive dimensions of antidepressive behaviour. Behavior Research and Therapy. 1977;15:57–63. doi: 10.1016/0005-7967(77)90088-2. http://dx.doi.org/10.1016/0005-7967(77)90088-2. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. A brief measure of loneliness suitable for use with adolescents. Psychological Reports. 1993;72:1379–1391. doi: 10.2466/pr0.1993.72.3c.1379. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30(1):58–66. doi: 10.1097/00004583-199101000-00009. http://dx.doi.org/10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Rodriguez D, Moss HB, Audrain-McGovern J. Developmental heterogeneity in adolescent depressive symptoms: associations with smoking behavior. Psychosomatic Medicine. 2005;67(2):200–210. doi: 10.1097/01.psy.0000156929.83810.01. http://dx.doi.org/10.1097/01.psy.0000156929.83810.01. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews assessing Axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M. A schedule for assessing self-control behaviors: preliminary findings. Behavior Therapy. 1980;11:109–121. http://dx.doi.org/10.1016/S0005-7894(80)80040-2. [Google Scholar]
- Rosenberg M. Society and the Adolescent Self-Image. Princeton University Press; Princeton, NJ: 1965. [Google Scholar]
- Schulenberg JE, Zarrett NR. Mental health during emerging adulthood: continuity and discontinuity in courses, causes, and functions. In: Arnett JJ, Tanner JL, editors. Emerging Adults in America: Coming of Age in The 21st Century. American Psychological Association; Washington, DC, US: 2006. pp. 135–172. http://dx.doi.org/10.1037/11381-006. [Google Scholar]
- Sobin C, Weissman MM, Goldstein RB. Diagnostic interviewing for family studies: comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric disorders. Psychiatric Genetics. 1993;3(4):227–233. http://dx.doi.org/10.1097/00041444-199324000-00005. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID): I. History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: Identifying latent trajectories and early predictors. Journal of Abnormal Psychology. 2005;114(3):331–345. doi: 10.1037/0021-843X.114.3.331. http://dx.doi.org/10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su SS, Hoffman JP, Gerstein DR, Johnson RA. The effect of home environment on adolescent substance use and depressive symptoms. Journal of Drug Issues. 1997;22:851–877. [Google Scholar]
- Thompson W, Hickey J. Society in Focus. Allyn & Bacon, Pearson; Boston, MA: 2005. [Google Scholar]
- Tofighi D, Enders C. Identifying the correct number of classes in growth mixture models. In: Hancock GR, Samuelsen KM, editors. Advances in Latent Variable Mixture Models. Information Age Publishing; Charlotte, NC: 2008. pp. 317–341. [Google Scholar]
- Weissman AN, Beck AT. Development and validation of the dysfunctional attitude scale. Paper Presented at the Meeting of the Association for the Advancement of Behavior Therapy; Chicago, IL. 1978. [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Wickrama T, Lott R. Heterogeneity in youth depressive symptom trajectories: social stratification and implications for young adult physical health. Journal of Adolescent Health. 2009;45(4):335–343. doi: 10.1016/j.jadohealth.2009.04.018. http://dx.doi.org/10.1016/j.jadohealth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- Winstead BA, Cash TF. Reliability and Validity of the Body Self-Relationship Questionnaire. 1984 Unpublished manuscript. [Google Scholar]


