Abstract
Bicuspid aortic valve and/or coarctation of the aorta are consistently associated with ascending aortic and para-coarctation medial abnormalities. Medial abnormalities in the ascending aorta are prevalent in other types of patients with a variety of forms congenital heart disease (CHD), such as single ventricle, persistent truncus arteriosus, transposition of the great arteries, hypoplastic left heart syndrome, tetralogy of Fallot. These abnormalities encompass a wide age range, and may predispose to dilatation, aneurysm, and rupture that necessitates aortic valve and root surgery. This dilatation can develop in CHD patients without stenotic region. These CHDs exhibit ongoing dilatation of the aortic root and reduced aortic elasticity and increased aortic stiffness that may relate to intrinsic properties of the aortic root. The concept of aortic dilatation is shifting a paradigm of aortic dilatation, as so called post stenotic dilatation, to primary intrinsic aortopahy. These aortic dilatation and increased stiffness can induce aortic aneurysm, rupture of the aorta and aortic regurgitation, but also provoke left ventricular hypertrophy, reduced coronary artery flow and left ventricular failure. We can recognize this association of aortic pathophysiological abnormality, aortic dilation and aorto-left ventricular interaction as a new clinical entity: "aortopathy".
Keywords: Aortic disease, Congenital heart defects, Cystic medial necrosis of aorta, Tetralogy of fallot
Introduction
The ascending aorta in congenital heart disease (CHD) may dilate out of proportion to hemodynamic or morphogenetic expectations, may become aneurysmal, and may rupture.1),2) Aortic dilation in Marfan syndrome, Turner syndrome, bicuspid aortic valve (BAV), and coarctation of the aorta is well recognized; these disorders are associated consistently with ascending aortic and/or para-coarctation medial abnormalities.2),3) CHD such as single ventricle, persistent truncus arteriosus, transposition of the great arteries, hypoplastic left heart syndrome, and tetralogy of Fallot (TOF) are associated with aortic medial abnormalities, aortic dilatation, and aortic regurgitation (AR).1) Aortic medial abnormalities-incorrectly called cystic medial necrosis-reach their severest form in Marfan syndrome, and are prevalent and qualitatively similar, but seldom quantitatively as marked, in a wide variety of CHDs with a wide age range.1) These observations have led us to hypothesize that various types of CHD harbor an aortic medial abnormality that reflects a common developmental fault leading to a weakened and attenuated aortic wall. These CHDs with aortic dilatation are associated often with latent complications, which are decreased elasticity and increased stiffness of the aorta.4-6) These aortic pathophysiological changes have a negative influence on the systemic ventricular systolic and diastolic functions, due to increased afterload and ventricular hypertrophy.5)
In this review, we will discuss the aortic complications of CHD, emphasizing their history, pathophysiology, and importance of the new clinical entity "aortopathy".
Historical Perspective
In 1928, Maude Abbott, Montreal,7) mentioned in her textbook on CHD that the presence of a BAV appears to indicate, at least in a portion of the cases in which it occurs, a tendency for spontaneous rupture". In 1972, McKusick3) reported that the association of BAV and cystic medial necrosis is more than coincidental and cystic medial necrosis was defined as follows8): 1) Non-inflammatory smooth muscle cell loss; 2) Fragmentation of elastic fibers; and 3) Accumulation of basophilic ground substance within cell-depleted areas of the medial layer of the vessel wall.
In 1978, Edwards et al.9) reported that among 119 necropsy specimens with aortic dissection, 11 were from BAV (9%). In addition, Roberts et al.2) reported that among 186 necropsy specimens with aortic dissection, 14 were from BAV (7.5%) with a mean age of 52 and severe degeneration of the elastic fiber was found in the aortic wall in 90% of them. A high incidence of BAV among patients with aortic dissection is suggestive of a causative relationship between BAV and aortic dissecting aneurysm.
In 1990s, Hahn et al.10) and Nistri et al.11) reported that there is a high prevalence of aortic root enlargement in BAV that occurs irrespective of altered hemodynamics, suggesting that BAV and aortic root dilatation may reflect a common developmental defect. It has been recognized that patients with aortic valve have a tendency to have dilated aortic roots followed by aortic dissection and these patients harbor cystic medial necrosis in the aortic media. BAV was the first non-syndromic CHD in which aortic dissection and dilation were reported.12)
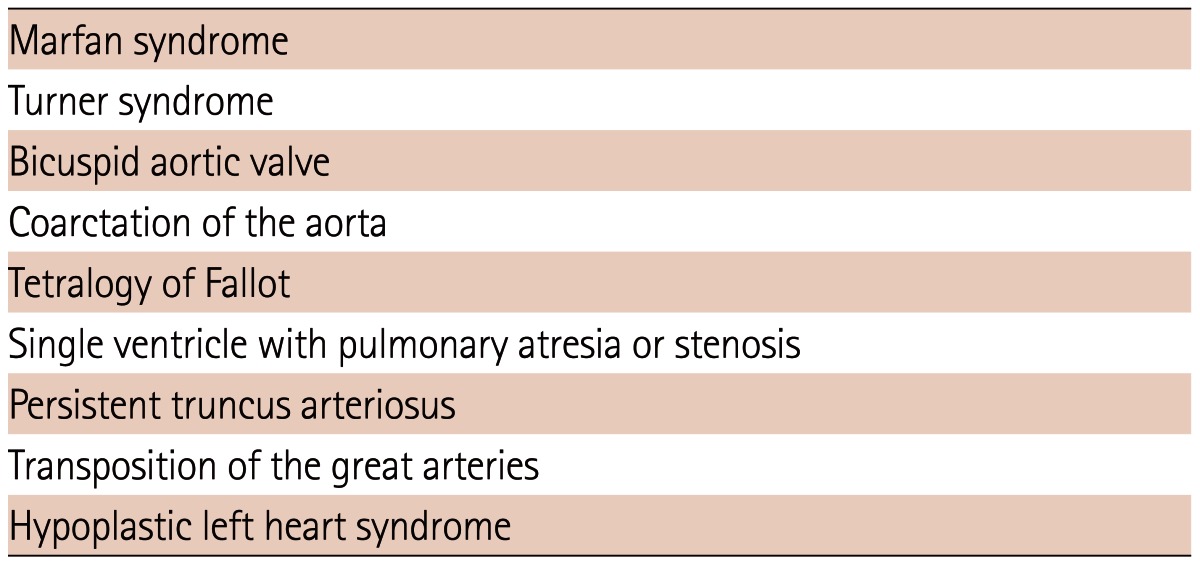
In 2001, Niwa et al.1) reported the first time that aortic medial abnormalities - so called cystic medial necrosis - are prevalent in a wide variety of CHDs with a dilated aortic root. Since that time, progressive aortic dilatation and regurgitation in various types of CHD, regardless of intracardiac repair, have been reported (Table 1).15-32)
Table 1.
Congenital heart diseases associated with aortic dilatation in adults
Congenital Heart Diseases Associated with Aortic Dilatation
Bicuspid aortic valve, aortic dissection, and Ross procedure
Aortic dissection is found to be 9 times more prevalent in BAV patients than in those with tricuspid valve.13) Aortic dilation begins during childhood in BAV patients, regardless of the presence of aortic stenosis.14) Histologic abnormalities in the ascending aorta in BAV patients are similar to those found in Marfan patients.3)
From recent reports on the Ross procedure15) in 118 patients with Ross procedure with age of 34 years and 44 months follow-up (BAV in 81%), the diameter of the sinuses of Valsalva increased from 31 +/- 0.4 mm to 33 +/- 0.5 mm. In 13 (11%), the diameter ranged from 40 mm to 51 mm, and 7 (6%) developed moderate AR and 3 (3%) required aortic valve replacement. The predicted probability of no or trivial AR decreased from 63% in the early postoperative period to 24% after 16 years. The most common cause for the failure of Ross is pulmonary autograft dilation.17) Dilation of the pulmonary autograft after the Ross procedure occurs because of an intrinsic abnormality of the pulmonary root in patients with congenital aortic valve disease.
Coarctation of the aorta
Isner et al.18) used a light microscopic to examine features of coarctation segments in 33 patients ranging in age from 1 day old to 15 years old, and observed cystic medial necrosis, deletion, and disarray of elastic tissue all 33 specimens. The remarkable findings observed in this pathological abnormality are found as early as in neonates, suggesting that cystic medial necrosis in the aortic wall in coarctation of the aorta is possibly intrinsic.
Aortic dilatation of tetralogy of Fallot
Among the cyanotic CHD, TOF was the first in which aortic dilation was recognized.19),20) Aortic dilatation is a well-known feature of unrepaired TOF and correlates well with severity of right ventricular outflow tract stenosis, and is greatest in TOF and pulmonary atresia. AR in unrepaired TOF imposes volume overload of both ventricles.21)
Late after repair of TOF, a significant subset of adults exhibit progressive aortic root dilatation that may lead to AR and predispose the patient to aortic dissection and to aortic rupture. The aortic dilatation relates medial abnormalities coupled with previous long-standing volume overload of the ascending aorta (right-to-left shunting through mal-alignment type ventricular septal defect). This dilatation and the histological abnormalities have been found from as early as in infants22); 15% of repaired TOF in adults had a dilated aortic root.23) Risk factors for aortic dilatation and regurgitation in TOF relate to specific hemodynamic abnormalities such as pulmonary atresia, right aortic arch, and a history of an aorto-pulmonary shunting, and patient demographics, such as male sex and the association of chromosome 22q11 deletion.23) Different from Marfan syndrome, aortic aneurysm and dissection/rupture have been reported rarely in association with TOF.23) It may be the case that this histological abnormality in the aorta in association with TOF is less severe than those cases associated with Marfan syndrome.1)
Neo-aortic dilation after arterial switch operation in complete transposition of the great artery
Aortic dilation and AR are well known complications after arterial switch operation in complete transposition of the great artery.22),23) Freedom from AR was 78% at 10 years and 69% at 15 years; freedom from AVR was 98% at 10 years and 97% at 15 years.24) Severe neo-aortic valve regurgitation was present in 3.7%, and trivial to mild regurgitation in 81% of patients at mid-term follow-up.25) Cystic medial necrosis is observed in the patients with arterial switch operation in both neo-aorta and pulmonary artery (20%) in the neonate; therefore, histological aortic abnormality in transposition of the great arteries is one of the causes of this aortic dilatation after repair.26) Progressive dilation of the neo-aortic root is out of proportion to somatic growth, and the incidence of AR increases with follow-up. Previous pulmonary artery banding is a risk factor for aortic dilation, while older age at which the arterial switch operation occurs and presence of ventricular septal defect are the other risk factors for AR.27)
Hypoplastic left heart syndrome
Neo-aortic root dilation and AR after staged reconstruction for hypoplastic left heart syndrome are known complications, and these complications progress over time. Cohen et al.28) followed 53 patients with hypoplastic left heart syndrome after having undergone a Fontan procedure for 9 years and found that neo-aortic root progressively dilated out of proportion to body size, with 98% having a Z-score >2 at most recent follow-up. Neo-AR was present in 61% of patients in this study. In general, mild pulmonary regurgitation can be physiologically seen in normal subjects, while any degree of AR is considered abnormal.29),30) Therefore, the difference in arterial histology may be one of the causes of this regurgitation.
Persistent truncus arteriosus
Dilated aortic root is found in the majority of operated truncus arteriosus patients; however, none has dissection or rupture.31) In this disorder, anatomical truncal valve abnormality and truncal valve regurgitation is common; therefore, the role of dilatation of the aorta in truncal valve regurgitation is unclear.
Other congenital heart diseases
Aortic dissection after CHD is found in patients with Fontan,32) but the incidence of aortic dissection in CHD other than BAV and COA is extremely rare.
Pathophysiology and Cause of Aortic Dilatation
Cause of aortic dilatation in congenital heart diseases and histology of the aortic media
Independent variables that alter the structure of ascending aortic media include Marfan syndrome, annuloaortic ectasia or Turner syndrome, and systemic hypertension,33) aging,34) pregnancy,35) and others (Table 2). In patients with systemic hypertension, abnormalities of aortic medial elastin and collagen are prevalent.33) With advancing age, layers of parallel aortic elastic fibers fragment, smooth muscle decreases especially in the thoracic aorta.34) In pregnancy, gestational changes in ascending aortic media are characterized by elastic fiber fragmentation and hypertrophy/hyperplasia of smooth muscle cells.35) Marfan syndrome is characterized by a defect in the chromosome 15 gene that codes for fibrillin-1,36) in the absence of which elastin is more readily degraded by metalloproteinase.37) Apoptosis reportedly plays a pathogenetic role in the medial abnormalities of abdominal aortic aneurysm.38),39) Deletion of transforming growth factor-β receptor is related to aortic dilatation.40) The genetic fault in Marfan syndrome apparently impairs aortic medial elastic fibers more extensively than impairment in CHD, and the incidence of ascending aortic dilatation, dissection or rupture is higher and the degree of aortic root medial lesions is greater in the former than in the latter.1)
Table 2.
Variables alter structure of ascending aortic media
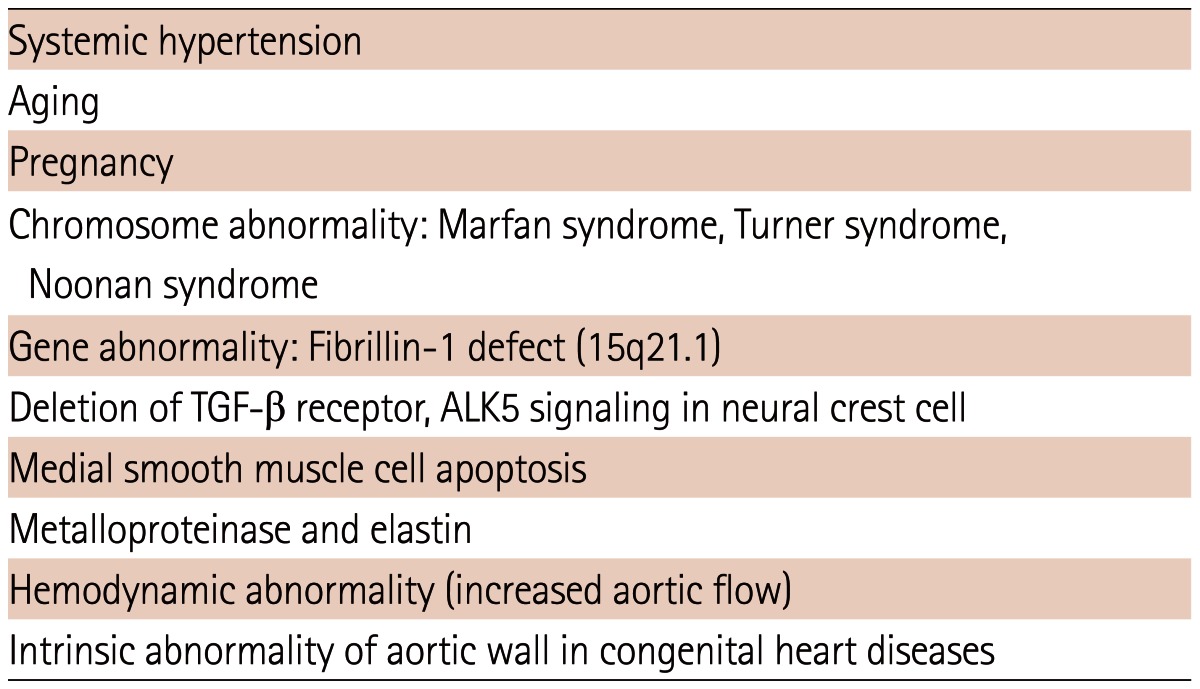
TGF-β: transforming growth factor-β, ALK5: activin receptor-like kinase 5
Histo-pathological abnormalities in various congenital heart diseases
Niwa et al.1) reported that in 88 CHD patients with dilated aorta with age of 3 weeks to 81 years (32 +/- 6 years) (48 males, 40 females), surgical biopsy aortic specimens was obtained, and cystic medial necrosis in the aortic media was observed in all of these patients.
Cause of aortic dilatation in tetralogy of Fallot
Higher histologic grading scores in TOF patients is found even in infants, which suggests the intrinsic abnormality has crucial role for this dilatation.22) Evidence for the role of aortic overflow over time in TOF includes the associations of higher age at operation, pulmonary atresia versus pulmonary stenosis, and longer presence of surgical aortopulmonary shunting with aortic dilation.41),42) There is a 12% increase in mean aortic diameter after surgical aortopulmonary shunting.42)
Aortic regurgitation in unrepaired TOF patients may be the result of annular dilation, weaker support of the right coronary cusp by the deficient outflow septum, and cusp prolapse.43) Only in a very small number of patients can surgical trauma potentiate AR. Frequency and degree of AR can be higher in case of late TOF repair.42)
Genetics in aortic dilatation in congenital heart diseases
Comparing patients with A-P phenotype (R-L cusp fusion) BAV with R-L phenotype (R-N cusp fusion), the former is more common in males, is larger and stiffer at the sinus of Valsalva, and is smaller at the ascending aorta and aortic arch than the latter.44),45) This aortic shape difference is possibly due to inborn errors of aortic wall than due to hemodynamic effects.46) Therefore, BAV phenotype can predict the elastic properties of ascending aorta and have potential impact on clinical outcomes.
In TOF patients with a dilated aorta, there is a 50.9% prevalence of fibrillin-1 gene polymorphisms or mutations and there is >8 times risk of aortic dilation in patients with these variants.47) In patients with chromosome 22q11.2 partial deletion, without conotruncal abnormality, aortic dilation is found in 10/93 (10.8%).48) Therefore, it is a possibility that aortic dilatation is a novel cardiovascular finding in patients with chromosome 22q11.2 partial deletion. In TOF patients after repair, chromosome 22q11.2 partial deletion is one of the risk factors of aortic dilatation.41)
New clinical entity "Aortopathy": Dilatation of aortic root, abnormality in aortic pathophysiological function, low coronary artery flow, and systemic ventricular dysfunction.
Aortic root dilation and aortic elastic properties in tetralogy of Fallot and arterial switch operation
In a study of 67 children at an average 8.3 years after TOF repair, Chong et al.49) found aortic dilation (z score >2) was observed in 88%, 87%, 61%, 63% at the annulus, sinus of Valsalva, sinotubular junction, and ascending aorta, respectively. Significantly increased stiffness, reduced strain, and distensibility of the aorta are observed in patients with aortic dilations.
Senzaki et al. reported that in 38 repaired TOF patients comparing with 55 controls, the former had higher characteristic of impedance and pulse wave velocity, lower total peripheral arterial compliance, higher arterial wave reflection, and also observed that the increase in aortic wall stiffness was closely associated with an increase in aortic root diameter. Therefore, central and peripheral arterial wall stiffness is characteristically increased after TOF repair. Abnormal arterial elastic properties have a negative impact on the left ventricle and provoke aortic dilatation, and it may induce left ventricular hypertrophy and systolic and diastolic dysfunction of left ventricle. Also in repaired TOF patients, decreased aortic elasticity and increased augmentation index are found.50)
After an arterial switch operation, patients decreased aortic elasticity and distensibility are confirmed by increased pulse-wave velocity51) and the stiffness index is increased.52)
These aortic pathophysiological abnormalities are observed in the other types of CHD with aortic dilatation, and these abnormalities may have a negative impact not only on aorta, but also on the left ventricle (or systemic right ventricle). These characteristics induce aortic dilation and AR,5),50) and increased pulsatile load on LV followed by decreased cardiac output;1) and also provoke decreased coronary blood flow that may negative influence on left ventricular function.45),47) In addition, AR may develop and progress due to stiffness of the aortic root.51)
We can recognize pathophysiologic abnormalities of the aorta and abnormal aortoventricular interaction (i.e., aortic dilation, AR, aortic pathophysiological abnormalities, and decreased coronary artery flow and left ventricular dysfunctions) as a new clinical entity "Aortopathy".
Conclusions
A subset of adult patients with CHD exhibits ongoing dilatation of the aortic root and reduced aortic elasticity that may relate to intrinsic properties of the aortic root. This new concept of aortic dilatation is shifting a paradigm of aortic dilatation from a so called post stenotic dilatation to primary intrinsic aortopathy. These aortic dilatation and increased stiffness can induce aortic aneurysm, rupture, and AR; and may also provoke left ventricular hypertrophy, reduced coronary artery flow, and left ventricular failure. We can recognize this association of aortic pathophysiological abnormality, aortic dilation, and aortic-ventricular interaction as a new clinical entity "Aortopathy".
Footnotes
The author has no financial conflicts of interest.
References
- 1.Niwa K, Perloff JK, Bhuta SM, et al. Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation. 2001;103:393–400. doi: 10.1161/01.cir.103.3.393. [DOI] [PubMed] [Google Scholar]
- 2.Roberts CS, Roberts WC. Dissection of the aorta associated with congenital malformation of the aortic valve. J Am Coll Cardiol. 1991;17:712–716. doi: 10.1016/s0735-1097(10)80188-3. [DOI] [PubMed] [Google Scholar]
- 3.McKusick VA. Association of congenital bicuspid aortic valve and erdheim's cystic medial necrosis. Lancet. 1972;1:1026–1027. doi: 10.1016/s0140-6736(72)91211-1. [DOI] [PubMed] [Google Scholar]
- 4.Seki M, Kurishima C, Kawasaki H, Masutani S, Senzaki H. Aortic stiffness and aortic dilation in infants and children with tetralogy of Fallot before corrective surgery: evidence for intrinsically abnormal aortic mechanical property. Eur J Cardiothorac Surg. 2012;41:277–282. doi: 10.1016/j.ejcts.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 5.Senzaki H, Iwamoto Y, Ishido H, et al. Arterial haemodynamics in patients after repair of tetralogy of Fallot: influence on left ventricular after load and aortic dilatation. Heart. 2008;94:70–74. doi: 10.1136/hrt.2006.114306. [DOI] [PubMed] [Google Scholar]
- 6.Chong WY, Wong WH, Chiu CS, Cheung YF. Aortic root dilation and aortic elastic properties in children after repair of tetralogy of Fallot. Am J Cardiol. 2006;97:905–909. doi: 10.1016/j.amjcard.2005.09.141. [DOI] [PubMed] [Google Scholar]
- 7.Perloff JK. Congenital aortic stenosis: Congenital aortic regurgitation. In: Perloff JK, Marelli AJ, editors. Clinical Recognition of Congenital Heart Disease. 6th ed. Philadelphia: Elsevier Saunders Company; 2012. pp. 74–100. [Google Scholar]
- 8.Erdheim J. Medionecrosis aortae idiopathica cystica. Virchows Arch Pathol Anat Physiol Klin Med. 1930;276:187–229. [Google Scholar]
- 9.Edwards WD, Leaf DS, Edwards JE. Dissecting aortic aneurysm associated with congenital bicuspid aortic valve. Circulation. 1978;57:1022–1025. doi: 10.1161/01.cir.57.5.1022. [DOI] [PubMed] [Google Scholar]
- 10.Hahn RT, Roman MJ, Mogtader AH, Devereux RB. Association of aortic dilation with regurgitant, stenotic and functionally normal bicuspid aortic valves. J Am Coll Cardiol. 1992;19:283–288. doi: 10.1016/0735-1097(92)90479-7. [DOI] [PubMed] [Google Scholar]
- 11.Nistri S, Sorbo MD, Marin M, Palisi M, Scognamiglio R, Thiene G. Aortic root dilatation in young men with normally functioning bicuspid aortic valves. Heart. 1999;82:19–22. doi: 10.1136/hrt.82.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reid RT. Bicuspid aortic valve associated with aneurysmal dilatation of the ascending aorta. Med J Aust. 1952;2:628–629. [PubMed] [Google Scholar]
- 13.Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol. 1984;53:849–855. doi: 10.1016/0002-9149(84)90418-1. [DOI] [PubMed] [Google Scholar]
- 14.Gurvitz M, Chang RK, Drant S, Allada V. Frequency of aortic root dilation in children with a bicuspid aortic valve. Am J Cardiol. 2004;94:1337–1340. doi: 10.1016/j.amjcard.2004.07.130. [DOI] [PubMed] [Google Scholar]
- 15.de Sa M, Moshkovitz Y, Butany J, David TE. Histologic abnormalities of the ascending aorta and pulmonary trunk in patients with bicuspid aortic valve disease: clinical relevance to the ross procedure. J Thorac Cardiovasc Surg. 1999;118:588–594. doi: 10.1016/S0022-5223(99)70002-4. [DOI] [PubMed] [Google Scholar]
- 16.Elkins RC, Thompson DM, Lane MM, Elkins CC, Peyton MD. Ross operation: 16-year experience. J Thorac Cardiovasc Surg. 2008;136:623–630. 630.e1–630.e5. doi: 10.1016/j.jtcvs.2008.02.080. [DOI] [PubMed] [Google Scholar]
- 17.David TE, Omran A, Ivanov J, et al. Dilation of the pulmonary autograft after the Ross procedure. J Thorac Cardiovasc Surg. 2000;119:210–220. doi: 10.1016/S0022-5223(00)70175-9. [DOI] [PubMed] [Google Scholar]
- 18.Isner JM, Donaldson RF, Fulton D, Bhan I, Payne DD, Cleveland RJ. Cystic medial necrosis in coarctation of the aorta: a potential factor contributing to adverse consequences observed after percutaneous balloon angioplasty of coarctation sites. Circulation. 1987;75:689–695. doi: 10.1161/01.cir.75.4.689. [DOI] [PubMed] [Google Scholar]
- 19.Bahnson HT, Spencer FC, Landtman B, Wolf MD, Neill CA, Taussig HB. Surgical treatment and follow-up of 147 cases of tetralogy of Fallottreated by correction. J Thorac Cardiovasc Surg. 1962;44:419–432. [PubMed] [Google Scholar]
- 20.Rieker RP, Berman MA, Stansel HC., Jr Postoperative studies in patients with tetralogy of Fallot. Ann Thorac Surg. 1975;19:17–26. doi: 10.1016/s0003-4975(10)65727-x. [DOI] [PubMed] [Google Scholar]
- 21.Capelli H, Ross D, Somerville J. Aortic regurgitation in tetrad of Fallot and pulmonary atresia. Am J Cardiol. 1982;49:1979–1983. doi: 10.1016/0002-9149(82)90218-1. [DOI] [PubMed] [Google Scholar]
- 22.Tan JL, Davlouros PA, McCarthy KP, Gatzoulis MA, Ho SY. Intrinsic histological abnormalities of aortic root and ascending aorta in tetralogy of Fallot: evidence of causative mechanism for aortic dilatation and aortopathy. Circulation. 2005;112:961–968. doi: 10.1161/CIRCULATIONAHA.105.537928. [DOI] [PubMed] [Google Scholar]
- 23.Niwa K. Aortic root dilatation in tetralogy of Fallot long-term after repair--histology of the aorta in tetralogy of Fallot: evidence of intrinsic aortopathy. Int J Cardiol. 2005;103:117–119. doi: 10.1016/j.ijcard.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Losay J, Touchot A, Capderou A, et al. Aortic valve regurgitation after arterial switch operation for transposition of the great arteries: incidence, risk factors, and outcome. J Am Coll Cardiol. 2006;47:2057–2062. doi: 10.1016/j.jacc.2005.12.061. [DOI] [PubMed] [Google Scholar]
- 25.Marino BS, Wernovsky G, McElhinney DB, et al. Neo-aortic valvar function after the arterial switch. Cardiol Young. 2006;16:481–489. doi: 10.1017/S1047951106000953. [DOI] [PubMed] [Google Scholar]
- 26.Takeuchi T, Imai Y, Takanashi Y, et al. Histological study of the great arteries in patients with arterial switch operation. Nihon Shoni Junkanki Gakkai Zasshi. 1996;12:506–512. [Google Scholar]
- 27.Schwartz ML, Gauvreau K, del Nido P, Mayer JE, Colan SD. Long-term predictors of aortic root dilation and aortic regurgitation after arterial switch operation. Circulation. 2004;110(11 Suppl 1):II128–II132. doi: 10.1161/01.CIR.0000138392.68841.d3. [DOI] [PubMed] [Google Scholar]
- 28.Cohen MS, Marino BS, McElhinney DB, et al. Neo-aortic root dilation and valve regurgitation up to 21 years after staged reconstruction for hypoplastic left heart syndrome. J Am Coll Cardiol. 2003;42:533–540. doi: 10.1016/s0735-1097(03)00715-0. [DOI] [PubMed] [Google Scholar]
- 29.Klein AL, Burstow DJ, Tajik AJ, et al. Age-related prevalence of valvular regurgitation in normal subjects: a comprehensive color flow examination of 118 volunteers. J Am Soc Echocardiogr. 1990;3:54–63. doi: 10.1016/s0894-7317(14)80299-x. [DOI] [PubMed] [Google Scholar]
- 30.Yoshida K, Yoshikawa J, Shakudo M, et al. Color Doppler evaluation of valvular regurgitation in normal subjects. Circulation. 1988;78:840–847. doi: 10.1161/01.cir.78.4.840. [DOI] [PubMed] [Google Scholar]
- 31.Carlo WF, McKenzie ED, Slesnick TC. Root dilation in patients with truncus arteriosus. Congenit Heart Dis. 2011;6:228–233. doi: 10.1111/j.1747-0803.2011.00520.x. [DOI] [PubMed] [Google Scholar]
- 32.Egan M, Phillips A, Cook SC. Aortic dissection in the adult Fontan with aortic root enlargement. Pediatr Cardiol. 2009;30:562–563. doi: 10.1007/s00246-009-9435-0. [DOI] [PubMed] [Google Scholar]
- 33.Carlson RG, Lillehei CW, Edwards JE. Cystic medial necrosis of the ascending aorta in relation to age and hypertension. Am J Cardiol. 1970;25:411–415. doi: 10.1016/0002-9149(70)90006-8. [DOI] [PubMed] [Google Scholar]
- 34.Schlatmann TJ, Becker AE. Histologic changes in the normal aging aorta: implications for dissecting aortic aneurysm. Am J Cardiol. 1977;39:13–20. doi: 10.1016/s0002-9149(77)80004-0. [DOI] [PubMed] [Google Scholar]
- 35.Manalo-Estrella P, Barker AE. Histopathologic findings in human aortic media associated with pregnancy. Arch Pathol. 1967;83:336–341. [PubMed] [Google Scholar]
- 36.Dietz HC, Pyeritz RE. Mutations in the human gene for fibrillin-1 (FBN1) in the Marfan syndrome and related disorders. Hum Mol Genet. 1995;4 Spec No:1799–1809. doi: 10.1093/hmg/4.suppl_1.1799. [DOI] [PubMed] [Google Scholar]
- 37.Segura AM, Luna RE, Horiba K, et al. Immunohistochemistry of matrix metalloproteinases and their inhibitors in thoracic aortic aneurysms and aortic valves of patients with Marfan's syndrome. Circulation. 1998;98(19 Suppl):II331–II337. discussion II337-8. [PubMed] [Google Scholar]
- 38.Bonderman D, Gharehbaghi-Schnell E, Wollenek G, Maurer G, Baumgartner H, Lang IM. Mechanisms underlying aortic dilatation in congenital aortic valve malformation. Circulation. 1999;99:2138–2143. doi: 10.1161/01.cir.99.16.2138. [DOI] [PubMed] [Google Scholar]
- 39.Ihling C, Szombathy T, Nampoothiri K, et al. Cystic medial degeneration of the aorta is associated with p53 accumulation, Bax upregulation, apoptotic cell death, and cell proliferation. Heart. 1999;82:286–293. doi: 10.1136/hrt.82.3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang J, Nagy A, Larsson J, Dudas M, Sucov HM, Kaartinen V. Defective ALK5 signaling in the neural crest leads to increased postmigratory neural crest cell apoptosis and severe outflow tract defects. BMC Dev Biol. 2006;6:51. doi: 10.1186/1471-213X-6-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niwa K, Siu SC, Webb GD, Gatzoulis MA. Progressive aortic root dilatation in adults late after repair of tetralogy of Fallot. Circulation. 2002;106:1374–1378. doi: 10.1161/01.cir.0000028462.88597.ad. [DOI] [PubMed] [Google Scholar]
- 42.Bhat AH, Smith CJ, Hawker RE. Late aortic root dilatation in tetralogy of Fallot may be prevented by early repair in infancy. Pediatr Cardiol. 2004;25:654–659. doi: 10.1007/s00246-003-0665-2. [DOI] [PubMed] [Google Scholar]
- 43.Rao BNS, Anderson RC, Edwards JE. Anatomic variations in the tetralogy of Fallot. Am Heart J. 1971;81:361–371. doi: 10.1016/0002-8703(71)90106-2. [DOI] [PubMed] [Google Scholar]
- 44.Schaefer BM, Lewin MB, Stout KK, Byers PH, Otto CM. Usefulness of bicuspid aortic valve phenotype to predict elastic properties of the ascending aorta. Am J Cardiol. 2007;99:686–690. doi: 10.1016/j.amjcard.2006.09.118. [DOI] [PubMed] [Google Scholar]
- 45.Schaefer BM, Lewin MB, Stout KK, et al. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Heart. 2008;94:1634–1638. doi: 10.1136/hrt.2007.132092. [DOI] [PubMed] [Google Scholar]
- 46.Jackson V, Petrini J, Caidahl K, et al. Bicuspid aortic valve leaflet morphology in relation to aortic root morphology: a study of 300 patients undergoing open-heart surgery. Eur J Cardiothorac Surg. 2011;40:e118–e124. doi: 10.1016/j.ejcts.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 47.Chowdhury UK, Mishra AK, Balakrishnan P, et al. Role of fibrillin-1 genetic mutations and polymorphism in aortic dilatation in patients undergoing intracardiac repair of tetralogy of Fallot. J Thorac Cardiovasc Surg. 2008;136:757–766. 766.e1–766.e10. doi: 10.1016/j.jtcvs.2007.12.044. [DOI] [PubMed] [Google Scholar]
- 48.John AS, McDonald-McGinn DM, Zackai EH, Goldmuntz E. Aortic root dilation in patients with 22q11.2 deletion syndrome. Am J Med Genet A. 2009;149A:939–942. doi: 10.1002/ajmg.a.32770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grotenhuis HB, Ottenkamp J, de Bruijn L, et al. Aortic elasticity and size are associated with aortic regurgitation and left ventricular dysfunction in tetralogy of Fallot after pulmonary valve replacement. Heart. 2009;95:1931–1936. doi: 10.1136/hrt.2009.175877. [DOI] [PubMed] [Google Scholar]
- 50.Cheung YF, Ou X, Wong SJ. Central and peripheral arterial stiffness in patients after surgical repair of tetralogy of Fallot: implications for aortic root dilatation. Heart. 2006;92:1827–1830. doi: 10.1136/hrt.2006.091199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murakami T, Nakazawa M, Momma K, Imai Y. Impaired distensibility of neoaorta after arterial switch procedure. Ann Thorac Surg. 2000;70:1907–1910. doi: 10.1016/s0003-4975(00)01837-3. [DOI] [PubMed] [Google Scholar]
- 52.Sievers HH, Lange PE, Arensman FW, et al. Influence of two-stage anatomic correction on size and distensibility of the anatomic pulmonary/functional aortic root in patients with simple transposition of the great arteries. Circulation. 1984;70:202–208. doi: 10.1161/01.cir.70.2.202. [DOI] [PubMed] [Google Scholar]


