Abstract
Background and Objectives
Stented segment length is a predictive factor for restenosis and stent thrombosis still in the drug-eluting stent (DES) era, and the benefit of routine intravascular ultrasound (IVUS) is still unclear. The aim of the present study was to investigate whether IVUS-guided percutaneous coronary intervention (PCI) improved the vascular outcomes as compared with conventional PCI in the treatment of diffuse coronary artery disease.
Subjects and Methods
From our registry database from January 2006 to May 2009, we identified 85 consecutive patients with de novo coronary lesions treated with at least 64 mm of multiple, overlapping DES. The 2-year rate of major adverse cardiovascular events (MACE), defined as the composite of cardiovascular death, non-fatal myocardial infarction, target lesion revascularization (TLR), or stent thrombosis, was compared according to the use of IVUS.
Results
The 2-year MACE rate was lower in the IVUS-guided group than that of the angiography-guided group (8% vs. 33.3%, p=0.005). The incidence of TLR was lower in patients with IVUS use than in those without IVUS use (0% vs. 27.8%, p<0.001). On Cox proportional hazard analysis, no IVUS use {hazard ratio (HR) 5.917, 95% confidence interval (CI) 1.037-33.770, p=0.045} and age (HR 1.097, 95% CI 1.006-1.138, p=0.032) were unfavorable predictors for the 2-year MACE.
Conclusion
The use of IVUS may improve the effectiveness and safety of multiple overlapping drug-eluting stenting for long, diffuse coronary lesions.
Keywords: Intravascular ultrasonography, Coronary stenosis, Drug-eluting stents, Percutaneous coronary intervention, Thrombosis
Introduction
The use of drug-eluting stents (DES) has been rapidly increasing in the treatment of coronary artery disease, as the superiority of DES over bare metal stents has been proven for the reduction of in-stent restenosis.1),2) It is reported that DES also seem to be safe and effective in multiple overlapping stenting for diffuse coronary lesions.3),4) Even in the DES era, however, stented length is an unfavorable predictor for in-stent restenosis5),6) and stent thrombosis.7)
The use of intravascular ultrasound (IVUS) has become popular for percutaneous coronary intervention (PCI), as it provides additional information in comparison to coronary angiography regarding the vessel size and lesion length, the degree of calcium in a plaque, the stability of the atheroma plate, stent expansion, stent-vessel apposition, and stent-related complications such as edge dissections.8) It remains unclear whether the strategy of IVUS-guided PCI leads to better clinical outcomes in patients with coronary artery disease undergoing DES implantation, especially for the high-risk subsets of coronary artery disease.9-13)
It is hypothesized that stent optimization using IVUS may improve clinical outcomes in patients with diffuse coronary lesions undergoing metal jacket stenting. The aim of the present study was to compare the vascular and clinical outcomes of IVUS-guided PCI to those of conventional PCI in the treatment of diffuse coronary artery disease, using multiple overlapping DES.
Subjects and Methods
Study population
Clinical, laboratory, and angiographic data were collected consecutively and prospectively in 2920 subjects who had undergone PCI with DES for de novo coronary artery stenosis at the Wonju Christian Hospital between January 1, 2006 and May 30, 2009. Twenty-nine patients expired during the procedure or the hospital stay. The patients presenting with ST-segment elevation myocardial infarction (MI) and who had coronary lesions involving left main vessel or bifurcation lesions requiring two stents were excluded from the study. Other exclusion criteria were: severe left ventricular dysfunction (ejection fraction <30%), cardiogenic shock, neoplastic disease, platelet count <150000/mL, and hemoglobin <10 g/L. Thus, the total study cohort included 85 consecutive patients with de novo coronary lesions treated with at least 64 mm of multiple overlapping DES. IVUS was not used for 36 patients who underwent stenting from January 1, 2006 to December 30, 2007. From January 1, 2008, IVUS was routinely performed at pre-intervention and/or post-intervention. Treatment by IVUS guidance was performed in 49 patients who underwent stenting from January 1, 2008 to May 30, 2009. A procedure was considered IVUS-guided when IVUS examinations were done during PCI for optimal stent implantation. Pre-PCI IVUS examination was done in 41 patients (83.7%) of the IVUS-guided group to evaluate the characterization of plaque and to estimate the reference diameter or the length of the lesion. Post-PCI IVUS examination was performed in all patients of the IVUS-guided group to detect suboptimal stent deployment, such as stent malapposition, stent underexpansion, and edge dissection. All patients gave written consent for the PCI procedure, and the study was conducted under the local Institutional Review Board approval.
Antithrombotic regimen
All patients received 300 mg of aspirin and at least 300-600 mg of clopidogrel before arriving to the catheterization room. A bolus of unfractionated heparin (70 U/kg) was administered immediately before coronary angiography through the introducer sheath. A second bolus of unfractionated heparin (70 U/kg) was delivered just prior to the PCI, and the additional heparin was administered to achieve an activated clotting time of 250-300 seconds. Aspirin and clopidogrel were required at a dose of 100 mg and 75 mg daily, respectively, for 1 year after PCI, followed by aspirin 100 mg indefinitely thereafter. The use of glycoprotein IIb/IIIa inhibitor and cilostazol in addition to the dual antiplatelet therapy were at the discretion of the primary physician.
Procedures
PCI was performed using balloon predilatation, followed by DES deployment via transradial or transfemoral arteries. Four types of DES were implanted as follows: 1) sirolimus-eluting stents (SES, Cypher, Cordis, Johnson & Johnson, Miami Lakes, FL, USA); 2) paclitaxel-eluting stents (PES, Taxus, Boston Scientific, MA, USA); 3) everolimus-eluting stents (EES, Xience V, Abbot Vascular, IL, USA); and 4) zotarolimus-eluting stents (ZES, Endeavor, Medtronic, Minneapolis, MN, USA). The choice regarding the specific type of DES was left to the operator's discretion. Procedural success was defined as a final diameter stenosis of <30% by quantitative coronary angiography (QCA) with normal flow. Adjuvant balloon dilation after stenting was performed in the following: if post-procedural angiography of the involved vessel showed a percent diameter stenosis ≥30%; if there was stent under-expansion defined as <5.0 mm2 of minimum stent area; or with malapposition on IVUS.
One of the two commercially available systems was used: iLAB (Boston Scientific Corp/SCIMED, Minneapolis, MN, USA); or Eagle Eye (Volcano Therapeutics Inc., Rancho Cordova, CA, USA). A dose of 100-200 µg of nitroglycerin was administered through the guiding catheter before IVUS examination. The IVUS catheter was positioned at more than 10 mm beyond the lesion/stent and was pulled back to a point more than 10 mm proximally to the lesion/stent using an automatic transducer pullback device at the speed of 0.5 mm/s or 1 mm/s. IVUS images were interpreted by the operator and at least one experienced IVUS technician. The treating physician decided if any additional treatment after IVUS examination was necessary.
All data concerning QCA parameters were measured and analyzed off-line using a primary diagnostic image review and analysis workstation (Centricity CA1000, GE Healthcare, United Kingdom) by a technician who was incognizant of the clinical information.
Clinical endpoints and data collection
The patients presented to follow-up at 1, 3, and 6 months, 1 year, and then yearly after the index procedure. Follow-up coronary angiography was not mandatory but recommended. The primary end point was the 2-year incidence of major adverse cardiovascular events (MACE) defined as the composite of death from cardiovascular (CV) causes, non-fatal MI, ischemia-driven target lesion revascularization (TLR), and stent thrombosis. All deaths were considered CV unless an unequivocal non-CV cause could be confirmed. The MI was defined according to the American College of Cardiology criteria as a rise in serum troponin I or an increase in creatine kinase-MB isoenzyme level of at least twice the upper normal limits, with at least one of the following: acute onset of prolonged (at least 20 minutes) typical ischemic chest pain; ST-segment elevation of at least 1 mm in two or more contiguous electrocardiography leads or ST-segment depression of at least 0.5 mm in at least two contiguous leads; and T-wave inversion more than 1 mm in leads with predominant R waves.14) Stent thrombosis was defined as definite or probable according to the Academic Research Consortium definitions.15)
A revascularization was considered ischemia-driven if angiography at follow-up showed a percent diameter stenosis ≥50% and if one of the following occurred: 1) a positive history of recurrent angina pectoris, presumably related to the target vessel; 2) objective signs of ischemia at rest or during exercise test, presumably related to the target vessel; 3) abnormal results of any invasive functional diagnostic test.15)
Statistical analysis
All continuous variables are presented as means±(SD) or the medians plus the range and the categorical variables as frequencies (percentage). Continuous variables were compared using the Student's t-test. The chi-square test was used for categorical variables, and Fisher's exact test was used when any expected cell count was lower than 5.
Major adverse cardiovascular event free survival curves for patients with and without the use of IVUS were generated by the Kaplan-Meier method and compared by the log-rank test. Predictors of clinical outcomes were identified using multivariate Cox regression models, including factors demonstrated on univariate analysis to predict the frequency of the event outcome at a significance level of p<0.1 and parameters associated with the event outcome from the previous studies (age, diabetes, chronic kidney disease, duration of dual anti-platelet therapy, acute MI, reduced left ventricular ejection fraction, multi-vessel PCI, total stent length, the use of SES or PES, and the use of IVUS). Significance level was defined as p<0.05. All analyses were performed with Statistical Package for the Social Sciences (SPSS) 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline clinical and laboratory characteristics on the basis of the use of IVUS are presented in Table 1. Treatment using DES under IVUS guidance was performed on 49 patients (57.6%), whereas 36 patients (42.4%) were treated without IVUS use. Both groups were balanced in mean age, history of diabetes mellitus, hypertension, hyperlipidemia, current smoking status, prior MI, and chronic kidney disease. The distribution of discharge medication use between the two groups was relatively similar, except for cilostazol (Pletaal, Otsuka Pharmaceutical, Tokyo, Japan) and β-blockers. Cilostazol was taken more frequently and β-blockers less frequently by patients without the use of IVUS (16.7% vs. 2%, p=0.038 for cilostazol, 44.4% vs. 77.6% for β-blockers, p=0.002). At 1-year follow-up, the patients with IVUS use had a better adherence to dual antiplatelet therapy than those without IVUS use (81.6% vs. 47.2%, p=0.002). The indication for PCI, the left ventricular ejection fraction, the level of B-type natriuretic peptide, and peak cardiac isoenzymes were not different between the two groups.
Table 1.
Baseline clinical and laboratory characteristics according to the use of IVUS
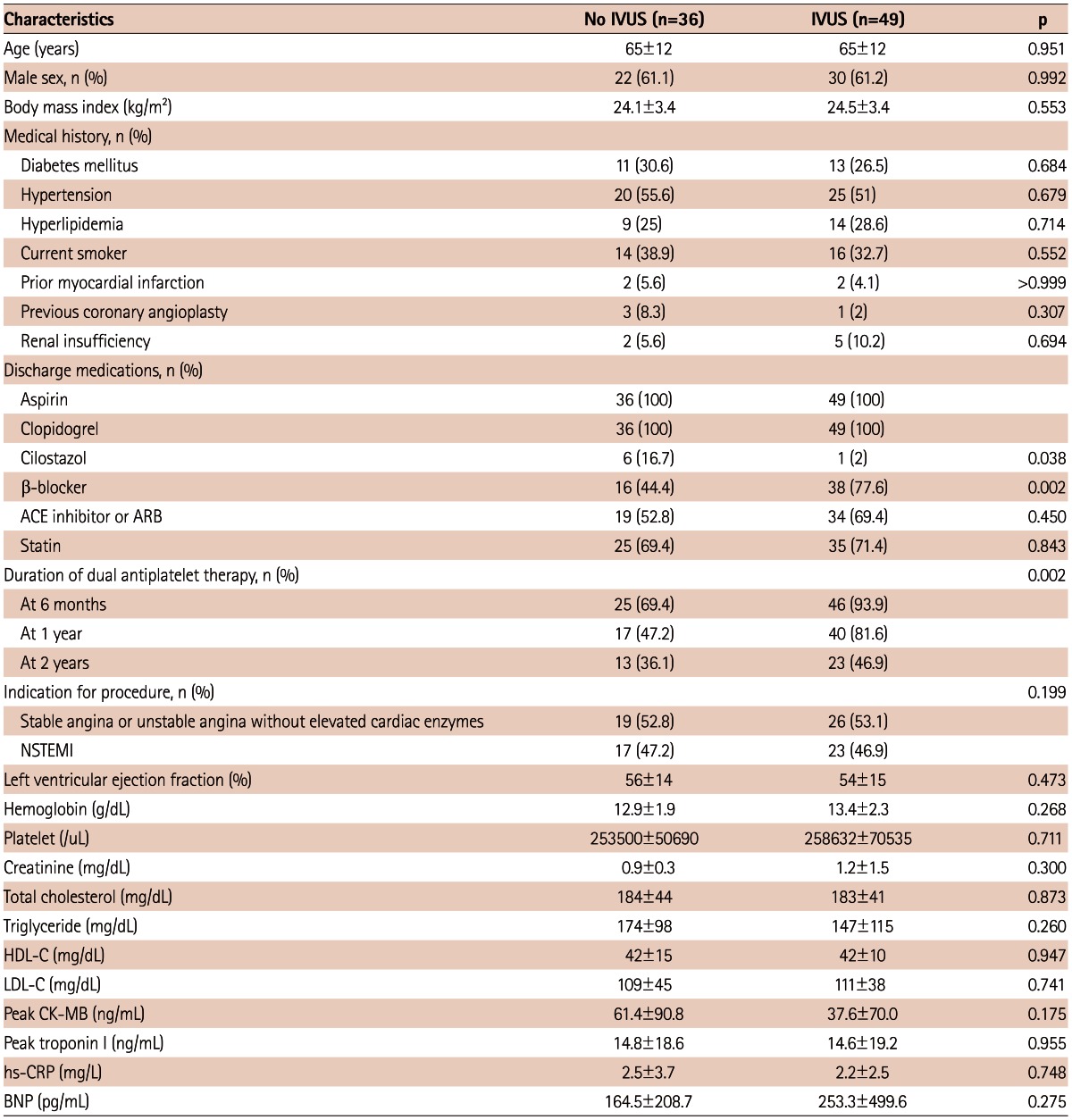
Values are expressed as number (%) or mean±SD. IVUS: intravascular ultrasound, ACE: angiotensin-converting enzyme, ARB: angiotensin receptor blocker, BNP: B-type natriuretic peptide, CK-MB: creatine kinase, muscle and brain, HDL-C: high density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein, LDL-C: low density lipoprotein-cholesterol, NSTEMI: non-ST-segment elevation myocardial infarction
Quantitative coronary angiography and percutaneous coronary intervention data
Table 2 depicts QCA and PCI data. Approximately 50% of the patients underwent PCI for coronary lesion in the left anterior descending artery. All lesions were the American Heart Association/American College of Cardiology classification type C. There was no difference on SYNTAX score between the groups (21.8±12.7 vs. 23.1±10.1, p=0.611). Lesion characteristics concerning the ostial lesions, bifurcation lesions, and chronic total occlusion were similar in the two groups. The mean number of stents per lesion was 2.2±0.5 and 2.8±0.5 in the angiography-guided and IVUS-guided group, respectively (p<0.001). The median stent length was 66 mm (range 64-99 mm) and 74 mm (range 64-120 mm) in patients without and with IVUS guidance, respectively (p=0.006). Multi-vessel PCI and post-stent adjuvant ballooning were performed less frequently in patients treated by coronary angiography alone (33.3% vs. 57.1%, p=0.03 for multi-vessel PCI; 63.1% vs. 91.3%, p=0.959 for adjuvant ballooning, respectively).
Table 2.
Baseline and follow-up coronary angiographic and procedural parameters
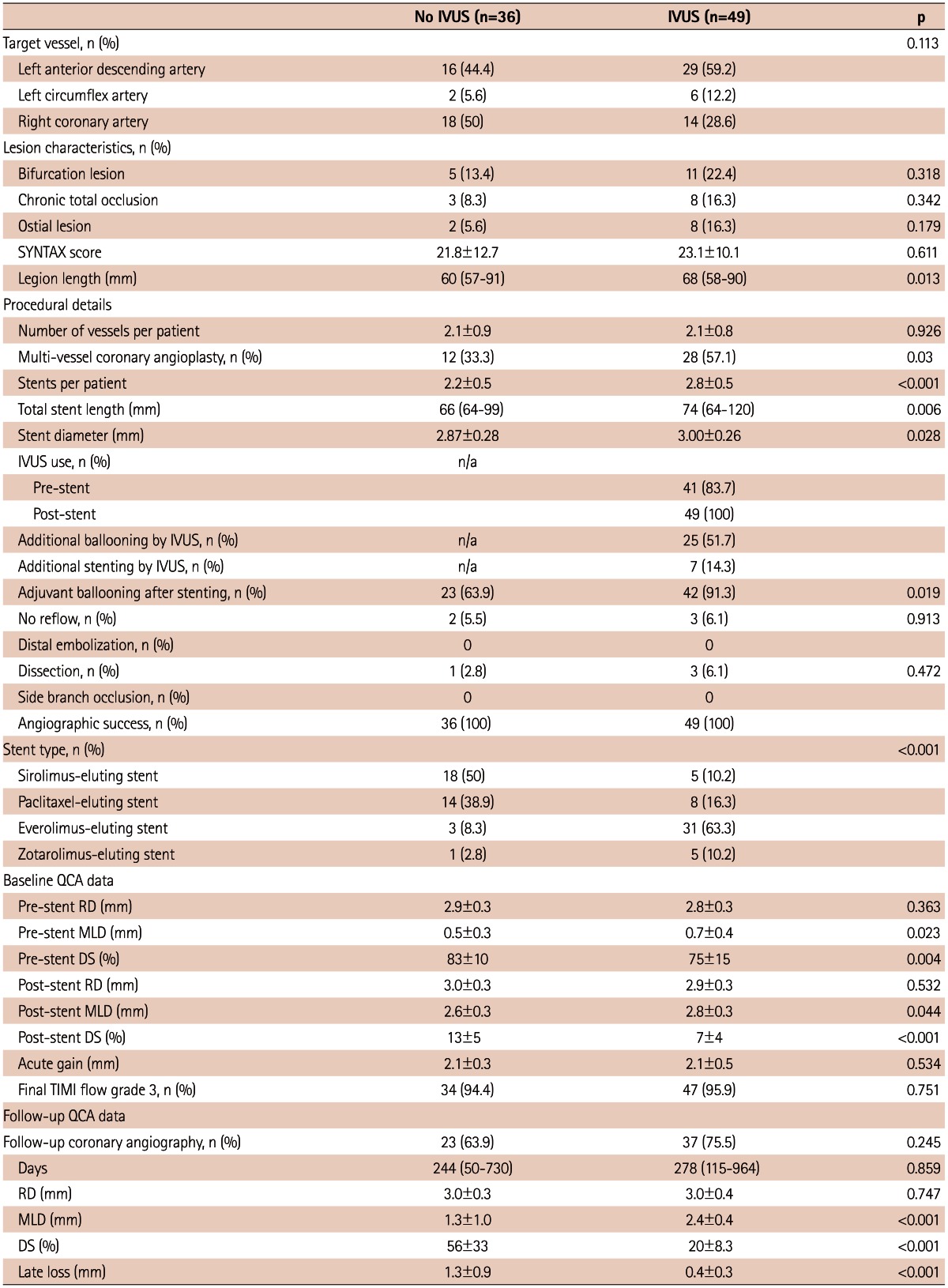
Values are expressed as number (%), mean±SD, or median (range). DS: diameter stenosis, IVUS: intravascular ultrasound, MLD: minimal luminal diameter, RD: reference diameter, QCA: quantitative coronary angiography, TIMI: Thrombolysis in Myocardial Infarction
Stent-related complications such as no reflow, distal embolization, dissection, and side branch occlusion occurred with similar frequency in both groups. SES (50%) and PES (38.9%) were used more frequently for coronary lesions treated with only angiography, while EES (63.3%) was used more frequently for lesions treated under IVUS guidance (p<0.001).
Baseline QCA data revealed that pre-stent and post-stent minimal luminal diameters (MLD) were smaller in the angiography-guided group than the IVUS-guided group (0.5±0.3 mm vs. 0.7±0.4 mm, p=0.023 for pre-stent MLD; 2.6±0.3 mm vs. 2.8±0.3 mm, p=0.044). Acute gain was attained similarly in the two groups (2.1±0.3 mm vs. 2.1±0.5 mm, p=0.534). Final Thrombolysis in Myocardial Infarction flow grade 3 was achieved in almost all lesions (95.3%). Follow-up coronary angiography was done in 63.9% of the patients in the angiography-guided group and for 75.5% of the patients in the IVUS-guided group (p=0.045). Late loss was higher in the angiography-guided group than in the IVUS-guided group (1.3±0.9 mm vs. 0.4±0.3 mm, p<0.001) (Fig. 1).
Fig. 1.
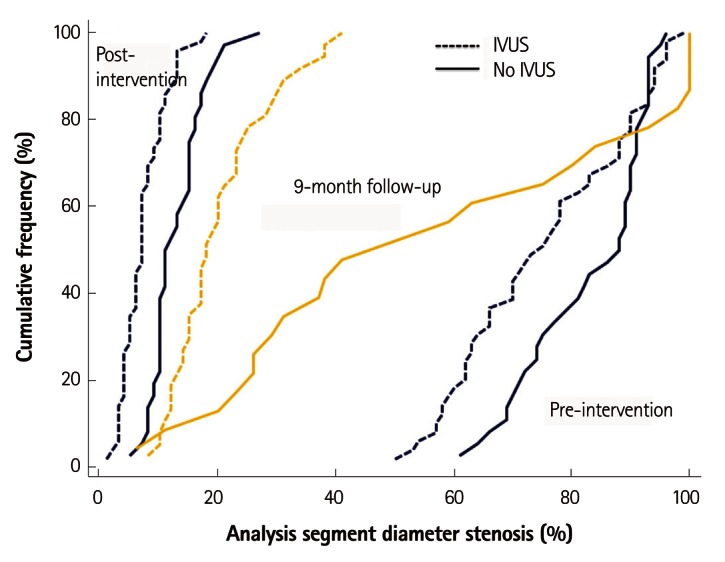
Cumulative frequency distribution curves for analysis segment percent diameter stenosis. At 9 months, the reduction in mean percent diameter stenosis for the IVUS-guided group relative to the angiography-guided group was -35.9% (95% confidence interval, -21.4% to -50.3%; p<0.001).
IVUS: intravascular ultrasound.
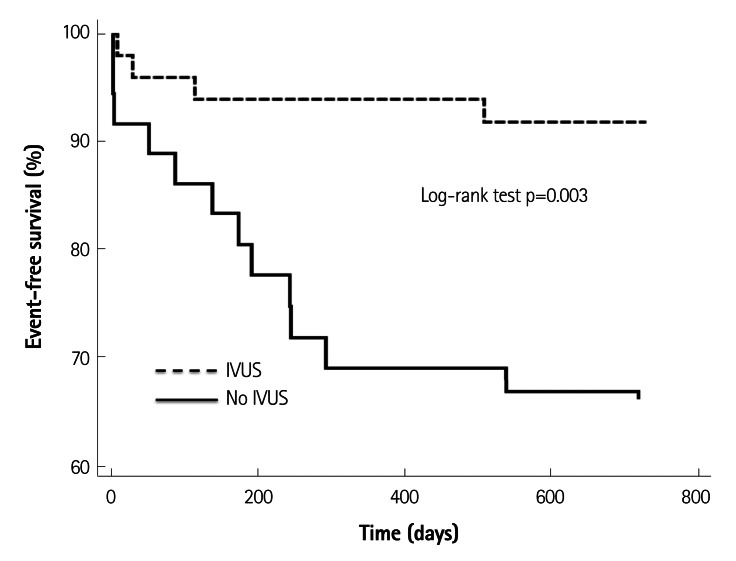
Clinical outcomes at two years in patients stratified by the use of IVUS
The 2-year MACE rate was lower in the IVUS-guided group than in the angiography-guided group (8% vs. 33.3%, p=0.001) (Fig. 2). No difference was found regarding CV death in the two groups (5.6% vs. 6.1%, p>0.999). Non-fatal MI and stent thrombosis occurred similarly in both groups (13.9% vs. 2.0%, p=0.079 for non-fatal MI; 11.1% vs. 2%, p=0.158 for stent thrombosis, respectively). In contrast, TLR was performed in 10 patients (27.8%) without IVUS guidance and none in the IVUS-guided group (p<0.001).
Fig. 2.
Kaplan-Meier event-free 2-year survival curves for the composite of cardiovascular death, myocardial infarction, target-lesion revascularization, and stent thrombosis in the intravascular ultrasound (IVUS) and no IVUS groups. The 2-year event rate was lower in the IVUS-guided group than that of the angiography-guided group (8% vs. 33.3%, p=0.003).
Predictors of major adverse cardiovascular events
Age, no use of IVUS, acute MI, use of 1st generation DES (SES or PES), shorter duration of dual antiplatelet therapy, and smaller stent diameter were univariate associated factors for higher 2-year MACE rate (Table 4). However, stent length was not associated with higher 2-year MACE rate {hazard ratio (HR) 1.012, 95% confidence interval (CI) 0.980-1.064, p=0.312}. On multivariate Cox proportional hazard analysis, no IVUS use (HR 5.917, 95% CI 1.037-33.770, p=0.045) and age (HR 1.097, 95% CI 1.006-1.138, p=0.032) were unfavorable predictive factors for 2-year MACE.
Table 4.
Univariate and multivariate predictors of poor clinical outcome on Cox proportional hazard analysis
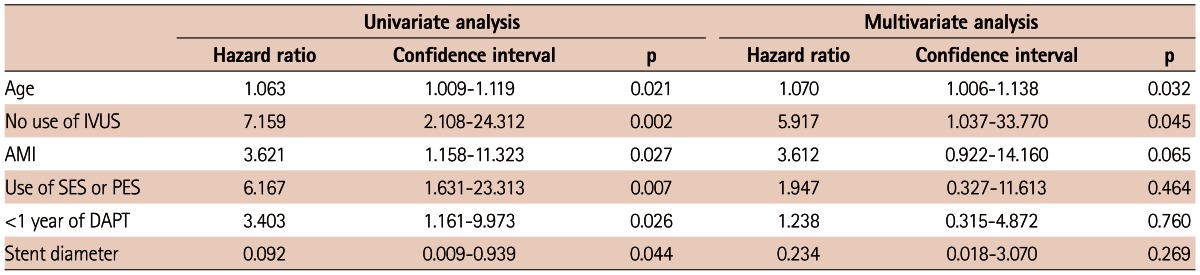
AMI: acute myocardial infarction, DAPT: dual antiplatelet therapy, IVUS: intravascular ultrasound, PES: paclitaxel-eluting stent, SES: sirolimus-eluting stent
Discussion
The main findings of the present study are that the incidence of adverse events in multiple overlapping stenting are still high in the DES era, and that IVUS use decreased those events in the treatment of diffuse coronary lesions.
The use of IVUS during PCI has been gaining in popularity with the interventional cardiology specialists, as it provides more detailed information than the conventional coronary angiography on the coronary lesions to be treated and the adequacy of the stent deployment. However, routine use of IVUS during PCI is not recommended in the current guidelines.17),18) Although there are few observational studies showing the superiority of IVUS use in the DES era,9),10),18) no randomized trial has yet been done to demonstrate whether IVUS-guided PCI improves clinical outcome in comparison to angiography-guided coronary angioplasty alone.
The benefits of IVUS may vary according to the clinical and lesional subsets. The event rate after PCI in patients with stable angina is relatively reduced, with the recent advances in PCI skills along with the advent of novel biocompatible DES and optimal medical therapy, including the use of statins and antiplatelet agents.2) One may expect a beneficial role of IVUS especially in patients with acute MI due to higher clinical event occurrence than in those with stable coronary disease. However, IVUS had not improved the clinical outcomes in patients with acute MI in a recent series of studies.11-13) The uncertainty in the usefulness of IVUS in acute MI setting may be due to the fact that there are many other clinical predictors for morbidity and mortality such as ischemia time, location of MI, infarct size, Killip classification, and treatment modalities. In contrast to the acute MI setting, IVUS-guided PCI seemed beneficial in the left main19) and bifurcation coronary lesions.19),20) Clinical outcomes in these lesions following DES implantation can be affected with similar importance by procedural as well as clinical factors. The theoretical benefit of IVUS over conventional coronary angiography may translate into better clinical outcomes in the treatment of sophisticated coronary lesions such as left main and bifurcation disease. The benefit of IVUS use in the treatment of long diffuse lesions has not been tested as yet. The present study revealed that IVUS-guided PCI showed better clinical outcomes than angiography-guided PCI in this study population who had diffuse coronary artery occlusive disease and who received at least 64 mm of overlapping DES. No use of IVUS was independently associated with higher MACE rate. As such, although the benefit of routine IVUS during PCI remains unclear, its usefulness may be maximized in certain lesion subsets, such as left main disease, bifurcation lesion and long diffuse lesion, in which the procedural factors can be more prominent.
The mechanism allowing IVUS-guided PCI to have a better clinical outcome in the treatment of long diffuse lesion in comparison to angiography-guided PCI is not evident. Stent length and stent diameter are still important predictors of in-stent restenosis and stent thrombosis following PCI in the DES era.22),23) Patients with IVUS-guided PCI had longer stents and used more stents compared with those with angiography-guided PCI in the present study. When treating diffuse coronary occlusive disease, full coverage of the diseased segment by the help of IVUS may obtain a better outcome, because the residual disease can cause subsequent stent thrombosis following PCI.24) The use of IVUS may have helped the treating physicians to detect inflow and/or outflow residual disease leading to the selection of a longer stent or additional stents. The IVUS-guided group also had a wider stent diameter, one of the possible explanations for the benefits of IVUS. The treating interventional cardiology specialists could have chosen the proper size of the stent as well as optimal stent length through IVUS interrogation before stent implantation. IVUS-guided PCI could optimize coronary stenting, avoiding stent underexpansion, malapposition, and residual lesion, a possible cause of stent thrombosis or in-stent restenosis. In fact, adjuvant ballooning was performed more frequently in the IVUS-guided group in this study. Other potential mechanisms for the better outcomes in the IVUS-guided group are the early detection of stent edge dissection, intra-stent thrombus, and tissue prolapse.
Limitations
There are several limitations in the present study. First, this is a single-center observational study in a small-sized population. Second, the periods of PCI with and without IVUS were different. This difference may cause various factors to impact on PCI outcomes, including the operator's skills, alteration of PCI strategy, and stents used etc. The DES type may have influenced the poor outcome in angiography-guided PCI group, as the patients in this group received more 1st generation DES such as SES or PES as compared to the IVUS-guided group. However, no IVUS use and age were the only predictors for poor clinical outcome on multiple Cox regression analysis. Third, the rates of follow-up angiography were around 60-70% in both groups. These rates are too low to precisely evaluate the follow-up parameters in QCA. Fourth, quantitative IVUS assessment was not performed. For this reason, the mechanism responsible for the superiority of IVUS-guided PCI over angiography-guided PCI is lacking. Fifth, since we excluded the high-risk patients, such as those with ST-segment elevation MI, our findings could not be extrapolated to every PCI patient.
Conclusions
In summary, the use of IVUS may improve efficiency and safety in multiple overlapping DES for long diffuse coronary lesions. To certify this hypothesis, further randomized, controlled trials are warranted.
Table 3.
Two-year major adverse cardiovascular events (MACE) according to the use of intravascular ultrasound (IVUS)
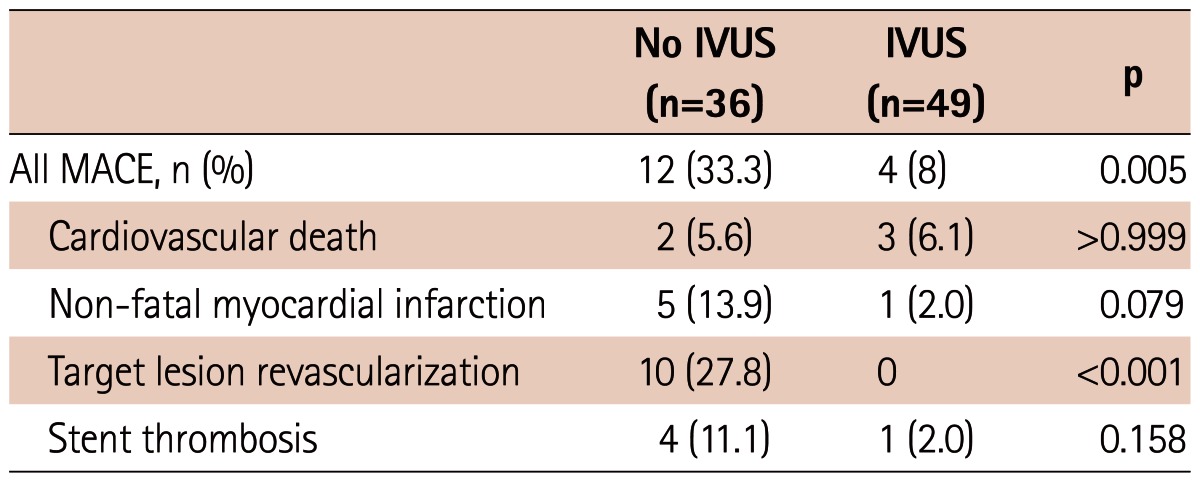
Values are expressed as number (%)
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Stettler C, Wandel S, Allemann S, et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370:937–948. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 2.Hannan EL, Racz M, Holmes DR, et al. Comparison of coronary artery stenting outcomes in the eras before and after the introduction of drug-eluting stents. Circulation. 2008;117:2071–2078. doi: 10.1161/CIRCULATIONAHA.107.725531. [DOI] [PubMed] [Google Scholar]
- 3.Aoki J, Ong AT, Rodriguez Granillo GA, et al. "Full metal jacket" (stented length > or =64 mm) using drug-eluting stents for de novo coronary artery lesions. Am Heart J. 2005;150:994–999. doi: 10.1016/j.ahj.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 4.Lee CW, Park KH, Kim YH, et al. Clinical and angiographic outcomes after placement of multiple overlapping drug-eluting stents in diffuse coronary lesions. Am J Cardiol. 2006;98:918–922. doi: 10.1016/j.amjcard.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010;56:1897–1907. doi: 10.1016/j.jacc.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 6.Hong SJ, Kim MH, Ahn TH, et al. Comparison of the predictors of coronary restenosis after drug-eluting stent implantation in diabetic and nondiabetic patients. Korean Circ J. 2007;37:530–537. [Google Scholar]
- 7.Tin-Hay EL, Poh KK, Lim YT, et al. Clinical predictors of stent thrombosis in the "real world" drug-eluting stent era. Int J Cardiol. 2010;145:422–425. doi: 10.1016/j.ijcard.2009.05.038. [DOI] [PubMed] [Google Scholar]
- 8.Brugaletta S, Costa JR, Jr, Garcia-Garcia HM. Assessment of drug-eluting stents and bioresorbable stents by grayscale IVUS and IVUS-based imaging modalities. Int J Cardiovasc Imaging. 2011;27:239–248. doi: 10.1007/s10554-010-9788-8. [DOI] [PubMed] [Google Scholar]
- 9.Roy P, Steinberg DH, Sushinsky SJ, et al. The potential clinical utility of intravascular ultrasound guidance in patients undergoing percutaneous coronary intervention with drug-eluting stents. Eur Heart J. 2008;29:1851–1857. doi: 10.1093/eurheartj/ehn249. [DOI] [PubMed] [Google Scholar]
- 10.Claessen BE, Mehran R, Mintz GS, et al. Impact of intravascular ultrasound imaging on early and late clinical outcomes following percutaneous coronary intervention with drug-eluting stents. JACC Cardiovasc Interv. 2011;4:974–981. doi: 10.1016/j.jcin.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed K, Jeong MH, Chakraborty R, et al. Role of intravascular ultrasound in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol. 2011;108:8–14. doi: 10.1016/j.amjcard.2011.02.339. [DOI] [PubMed] [Google Scholar]
- 12.Youn YJ, Yoon J, Lee JW, et al. Intravascular ultrasound-guided primary percutaneous coronary intervention with drug-eluting stent implantation in patients with ST-segment elevation myocardial infarction. Clin Cardiol. 2011;34:706–713. doi: 10.1002/clc.20966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maluenda G, Lemesle G, Ben-Dor I, et al. Impact of intravascular ultrasound guidance in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Catheter Cardiovasc Interv. 2010;75:86–92. doi: 10.1002/ccd.22198. [DOI] [PubMed] [Google Scholar]
- 14.Cannon CP, Battler A, Brindis RG, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee) J Am Coll Cardiol. 2001;38:2114–2130. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- 15.Kappetein AP, Head SJ, Généreux P, et al. Updated standardized end-point definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012;60:1438–1454. doi: 10.1016/j.jacc.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI) Winjs W, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 17.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574–e651. doi: 10.1161/CIR.0b013e31823ba622. [DOI] [PubMed] [Google Scholar]
- 18.Hur SH, Kang SJ, Kim YH, et al. Impact of intravascular ultrasound-guided percutaneous coronary intervention on long-term clinical outcomes in a real world population. Catheter Cardiovasc Interv. 2011 doi: 10.1002/ccd.23279. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Park SJ, Kim YH, Park DW, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009;2:167–177. doi: 10.1161/CIRCINTERVENTIONS.108.799494. [DOI] [PubMed] [Google Scholar]
- 20.Kim SH, Kim YH, Kang SJ, et al. Long-term outcomes of intravascular ultrasound-guided stenting in coronary bifurcation lesions. Am J Cardiol. 2010;106:612–618. doi: 10.1016/j.amjcard.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 21.Kim JS, Hong MK, Ko YG, et al. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a Korean multicenter bifurcation registry. Am Heart J. 2011;161:180–187. doi: 10.1016/j.ahj.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Hong MK, Mintz GS, Lee CW, et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006;27:1305–1310. doi: 10.1093/eurheartj/ehi882. [DOI] [PubMed] [Google Scholar]
- 23.Okabe T, Mintz GS, Buch AN, et al. Intravascular ultrasound parameters associated with stent thrombosis after drug-eluting stent deployment. Am J Cardiol. 2007;100:615–620. doi: 10.1016/j.amjcard.2007.03.072. [DOI] [PubMed] [Google Scholar]
- 24.Cook S, Ladich E, Nakazawa G, et al. Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation. 2009;120:391–399. doi: 10.1161/CIRCULATIONAHA.109.854398. [DOI] [PubMed] [Google Scholar]