Abstract
OBJECTIVE:
To determine whether curcumin reverses the multidrug resistance of human colon cancer cells in vitro and in vivo.
METHODS:
In a vincristine-resistant cell line of human colon cancer, the cell viability of curcumin-treated cells was determined using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay. Rhodamine123 efflux was evaluated to detect P-glycoprotein transporter activity, and expression of the multidrug resistance protein 1 and survivin genes was analyzed by reverse transcription polymerase chain reaction and western blotting. In addition, xenograft mouse tumors were grown and treated with curcumin. The morphology of the xenografts was investigated by hematoxylin-eosin staining. The in vivo expression of the multidrug resistance gene and P-glycoprotein and survivin genes and proteins was observed using reverse transcription-polymerase chain reaction and western blotting, respectively.
RESULTS:
Curcumin was not obviously toxic to the vincristine-resistant human colon cancer cells at concentrations less than 25 μM, but the growth of cells was significantly inhibited. At concentrations greater than 25 μM, curcumin was toxic in a concentration-dependent manner. The sensitivity of cells to vincristine, cisplatin, fluorouracil, and hydroxycamptothecin was enhanced, intracellular Rhodamine123 accumulation was increased (p<0.05), and the expression of the multidrug resistance gene and P-glycoprotein were significantly suppressed (p<0.05). The combination of curcumin and vincristine significantly inhibited xenograft growth. The expression of the multidrug resistance protein 1 and survivin genes was significantly reduced in xenografts of curcumin-treated mice and mice treated with both curcumin and vincristine relative to control mice.
CONCLUSION:
Curcumin has strong reversal effects on the multidrug resistance of human colon carcinoma in vitro and in vivo.
Keywords: Curcumin, Multidrug Resistance, Colorectal Carcinoma, Reversal
INTRODUCTION
Colon cancer is the third leading cause of cancer death in the USA, and the incidence is rapidly increasing in developing countries, including China (1). Chemotherapy plays an important role in the management of patients with colon carcinoma (2). Multidrug resistance (MDR) is one of the main impediments to the successful treatment of colon cancer (3) and consists of simultaneous resistance to many structurally unrelated cytotoxic agents (4). MDR in tumors involves different mechanisms, and a common mechanism of MDR is the active export of the drug from cells by the overexpression of P-glycoprotein (P-gp) (5) and other ATP-binding cassette (ABC) transporters. P-gp plays an important role in mediating resistance to apoptosis, which is important for MDR (6). Recently, resistance to chemotherapy has been associated with the inhibition of apoptosis. Induction of apoptosis can reverse the MDR of colon cancer (7). Agents that effectively reverse MDR are highly desirable.
Curcumin is a natural phenolic yellow-colored compound that is found in the plant Curcuma longa and has a wide range of biological and pharmacological activities, including antioxidant and anti-inflammatory properties, anti-mutagenic activity, and anti-carcinogenic, hypocholesterolemic, and hypoglycemic effects (8). In vitro studies have demonstrated that curcumin can overcome MDR in many tumors (9). However, it is not known whether curcumin can reverse the MDR of colon cancer cells, which led us to evaluate the effect of curcumin on the MDR of cancer cells.
In the present work, we investigated the effect of curcumin on vincristine resistance in the human colon cancer cell line HCT-8/VCR in vitro and in vivo and the mechanisms underlying this effect. We found that co-treatment of HCT-8/VCR cells with curcumin increased their sensitivity to vincristine (VCR), cisplatin (DDP), fluorouracil (5-FU), and hydroxycamptothecin (HCPT). Curcumin decreased the expression of P-gp and survivin and enhanced the accumulation of intracellular rhodamine123 (Rh123) in HCT-8/VCR cells. The combination of curcumin and VCR in vivo significantly inhibited xenograft growth, decreased tumor weight, and increased tumor cell apoptosis. Our results suggest that curcumin can reverse the MDR of colon cancer in vitro and in vivo. Curcumin could thus be useful in the treatment of MDR in human colon cancer cells as a MDR modulator.
MATERIALS AND METHODS
Reagents
Curcumin, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), ethidium bromide, acridine orange (AO), and rhodamine123 (Rh123) were obtained from Sigma (St. Louis, MO, USA); vincristine (VCR), hydroxycamptothecin (HCPT), cisplatin (DDP), and fluorouracil (5-FU) were obtained from Shenzhen Main Luck Pharmaceuticals Inc. (Shenzhen, China); P-gp and survivin antibodies and HRP-conjugated goat anti-rabbit IgG were purchased from Biosynthesis Biotechnology (Beijing, China); Trizol, the reverse transcription-polymerase chain reaction (RT-PCR) kit, and the western blot kit were purchased from Takara Biotechnology Co., Ltd. (Dalian, China).
Cell lines and cell culture
The vincristine-resistant human colon cancer cell line HCT-8/VCR was obtained from the Shanghai Cell Collection (Shanghai, China). The cells were routinely cultured in RMPI-1640 supplemented with 10% heat-inactivated fetal bovine serum (Gibco), 100 IU/ml penicillin, and 100 IU/ml streptomycin at 37°C in a 5% CO2 atmosphere. The medium for HCT-8/VCR cells was further supplemented with 2 μg/ml VCR. The HCT-8/VCR cells were cultured in drug-free medium for 1 week prior to use in experiments.
Determination of curcumin concentration
Cells were seeded in 96-well plates at a density of 5×103 HCT-8/VCR cells per well and incubated in a humidified atmosphere of 5% CO2 and 95% air overnight. Then, 6.25, 12.5, 25, 50, or 100 μM curcumin (20 μl) was added. After incubation for 48 h, 20 μl of MTT (5 g/L) was added. The plates were incubated for 4 h, and the blue dye formed was dissolved in 100 μl of dimethyl sulfoxide (DMSO). The absorbance at 570 nm was recorded using a microplate reader, and the inhibition rate was calculated.
Cell viability assay
Cells were seeded in 96-well plates at a density of 3×103 cells per well and cultured for 24 h before treatment with 6.25, 12.5, or 25 μM curcumin and 0.5 μg/ml VCR (20 μl). After the indicated incubation time, 20 μl of MTT [5 mg/ml in phosphate-buffered saline (PBS)] was added to each well, and the cells were incubated for an additional 4 h at 37°C. Finally, 150 μl of DMSO was added to stop the reaction. The absorbance at 570 nm was measured to determine the cell viability in each well.
Cell MDR assay
The control group (HCT-8/VCR cells not treated with curcumin) and the experimental group (HCT-8/VCR cells treated with 25 μM curcumin for 24 h) were used. HCT-8/VCR cells in the logarithmic growth phase were seeded in 96-well plates at a density of 3×103 cells per well, incubated for 24 h, and treated with increasing concentrations of VCR, DDP, 5-FU, and HCPT based on the plasma peak concentration obtained during chemotherapy. After incubation for 72 h, 20 μl of MTT (5 mg/ml in PBS) was added to each well, and the cells were incubated at 37°C for 4 h. Then, 150 μl of DMSO was added to each well to stop the reaction. The absorbance at 570 nm was measured to determine the growth inhibition in each well. The IC50 values were determined using Bliss software(DAS 2.0,Mathematical Pharmacology Professional Committee of China, Shanghai, China). The reversal fold (RF) was calculated.
Efflux and accumulation of Rh123 was measured by flow cytometry
For determination of Rh123 efflux, cells were loaded for 60 min with Rh123 in the absence of curcumin, and then the medium was replaced with Rh123-free medium containing curcumin or the vehicle (DMSO). Following efflux intervals of 60 min, the medium was removed, and the cells were washed twice with ice-cold Hanks' balanced salt solution (HBSS) and placed in HBSS containing 10% fetal bovine serum on wet ice. The green fluorescence of Rh123 was measured using a FACScan flow cytometer.
The measurement of Rh123 accumulation was performed as previously described (10). Briefly, cells (5×105 per sample) were incubated in the dark with 1 μg/ml Rh123 at 37°C in 5% CO2 for 2 h. Curcumin (25 μM, dissolved in 0.1% DMSO) was added to the cells at the same time as the Rh123. Following Rh123 accumulation, the cells were washed twice with ice-cold HBSS and prepared for flow cytometry as described above.
RT-PCR analysis
Total RNA from cells and snap-frozen tumor samples was isolated using TRIzol, as recommended by the manufacturer. RT-PCR was used for the analysis of multidrug resistance gene (MDR1) and survivin mRNA with GAPDH as an internal control. Primers for MDR1 were as follows: forward primer 5′-CAAGGAAGCCAATGCCTATGAC-3′, reverse primer 5′-ATCCAGAGCCACCTGAACCACT-3′. Survivin mRNA primers were as follows: forward 5′-GACCACCGCATCTCTACATTC-3′ and reverse 5′-GTTCTTGGCTCTTTCTCTGTCC-3′. GAPDH primers were as follows: forward 5′-ACCACAGTCCATGCCATCAC-3′ and reverse 5′-TCCACCACCCTGTTGCTGTA-3′. The reactions were performed in accordance with standard protocols. PCR was performed by an initial denaturation at 94°C for 5 min followed by 30 cycles of 94°C for 30 s, 58°C for 30 s, and 72°C for 60 s. The products were separated by electrophoresis in 2% agarose and visualized using ethidium bromide. The experiments were performed in triplicate.
Western blot analysis
The cells were either treated with curcumin or left untreated (control) and incubated for 48 h. Next, they were harvested, lysed in lysis buffer containing 150 mM sodium chloride, 0.1 M Tris, 1% Tween-20, 50 mM diethyldithiocarbamic acid, 1 mM ethylenediamine tetraacetic acid, and protease inhibitors at pH 8.0. The lysates were centrifuged at 12,500 rpm at 4°C for 15 min, and the supernatants were collected. The protein extracts were separated by sodium dodecyl sulfate-polyacdene gel electrophoresis and transferred onto nitrocellulose membranes. The membranes were then blocked with rabbit anti-survivin, anti-P-gp, and anti-β-actin primary polyclonal antibodies, respectively, at 4°C overnight. After washing with PBS containing 0.05% Tween 20, the membranes were incubated with the secondary antibody (goat anti-rabbit) for 2 h. Then, they were visualized using chemiluminescence detection reagents according to the manufacturer's instructions.
Animal studies
Five-week-old, female BALB/C nude mice were obtained from the Laboratory Animal Center of Chongqing Medical University. They were maintained in a specific pathogen-free unit under isothermal conditions. All of the experimental procedures were conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. HCT-8/VCR cells (4×106) suspended in 0.1 ml of PBS were implanted subcutaneously into the right flank of nude mice to form xenograft tumors. When the tumor size reached approximately 100 mm3, the mice were randomly divided into four groups with five mice in each group. Curcumin (50 mg/kg) and VCR (2 mg/kg) were administered twice daily by peritumoral injections for 14 days. The tumors were monitored by measuring the tumor volume with vernier calipers. The volume was calculated using the formula: V (mm3) = length × width2/2. After 14 days, the tumors were harvested for western blot and RT-PCR analysis. In addition, each tumor was fixed in 4% formaldehyde, dehydrated, paraffin-embedded, sectioned, and stained with hematoxylin-eosin to observe changes in pathological cell morphology in the different groups using a light microscope.
P-gp and survivin protein expression in xenograft tumors
Snap-frozen tumor samples were mechanically homogenized in the lysis buffer, and the lysates were collected by centrifugation as described above. The following steps were the same as described above for the western blot analysis.
Statistical analysis
All data were displayed as the mean ± standard deviation (SD), analyzed by analysis of variance (ANOVA) and Student's t-test as appropriate, and processed using the statistical software SPSS 13.0. Differences were considered significant at p<0.05. All experiments were repeated in triplicate.
RESULTS
Concentration of curcumin
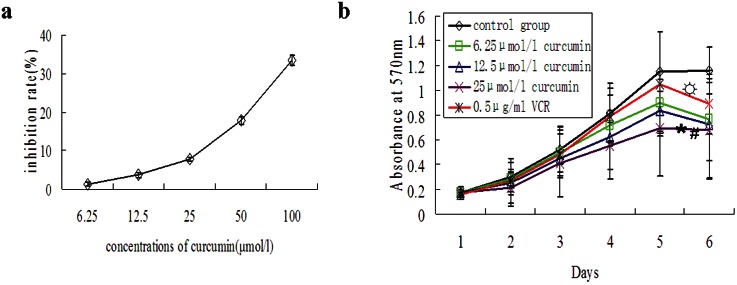
After HCT-8/VCR cells were treated with increasing concentrations of curcumin, cell growth was inhibited to different degrees. There was no significant toxicity observed in cells treated with curcumin at a concentration of 25 μM or less; at concentrations greater than 25 μM, concentration-dependent cell toxicity was observed (Figure 1A). Therefore, 25 μM curcumin was selected as the maximum curcumin concentration for the experiments.
Figure 1.
Suppression of HCT-8/VCR cell growth by curcumin treatment. A) Concentration-response curves in HCT-8/VCR cells treated with different concentrations of curcumin. Curcumin inhibited the growth of HCT-8/VCR cells in a concentration-dependent manner (mean ± SD, n = 3). B) The effects of curcumin on HCT-8/VCR cell growth were detected by flow cytometry. The cells were treated with various curcumin concentrations and 0.5 μg/ml VCR for 6 days. The inhibitory effect of curcumin on cells was significantly higher at 25 μM than at other concentrations (mean ± SD, n = 3) *p<0.01 vs. control group, #p<0.05 vs. VCR group, *p>0.01 vs. control group.
Influence of curcumin on cellular growth
When different concentrations of curcumin (6.25, 12.5, and 25 μM) were applied to the colon cancer cell line HCT-8/VCR, the MTT assays showed that with increasing concentrations of curcumin and longer incubation times, the inhibition of cellular growth also increased, and the inhibition of cell growth by curcumin was significantly greater than the inhibition mediated by VCR (0.5 μg/ml) (Figure 1B) (p<0.05).
Curcumin-mediated reversal of MDR in HCT-8/VCR cells
From the MTT assay, the IC50 values of VCR, DDP, 5-FU, and HCPT were calculated to be 62.3±1.2 μg/ml, 47.9±3.6 μg/ml, 13.4±1.3 μg/ml, and 34.2±2.1 μg/ml, respectively, in HCT-8/VCR cells. In HCT-8/VCR cells treated with 25 μM curcumin for 24 h, the sensitivity of HCT-8/VCR to VCR, DDP, 5-FU, and HCPT was enhanced, and the IC50 values were significantly decreased, with values of 13.6±0.9 μg/ml, 16.1±1.7 μg/ml, 8.3±0.8 μg/ml, and 29.7±1.8 μg/ml, respectively (p<0.05). The RF values were 4.6, 3.0, 1.6, and 1.2 times, respectively (Table 1).
Table 1.
Reversal of multidrug-resistance in the colon cancer cell line HCT-8/VCR by curcumin (mean ± SD, n = 3).
| Drugs | IC50 (μg/ml) | RF | |
| HCT-8/VCR | HCT-8/VCR+curcumin | ||
| VCR | 62.3±1.2 | 13.6±0.9*) | 4.6 |
| DDP | 47.9±3.6 | 16.1±1.7*) | 3.0 |
| 5-FU | 13.4±1.3 | 8.3±0.8*) | 1.6 |
| HCPT | 34.2±2.1 | 29.7±1.8*) | 1.2 |
p<0.05 vs. HCT-8/VCR, RF = reversal fold.
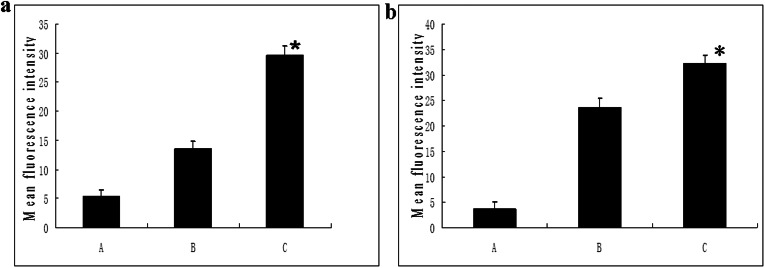
Efflux and accumulation of Rh123 in HCT-8/VCR cells
Flow cytometry experiments demonstrated that the efflux and accumulation of Rh123 in HCT-8/VCR cells treated with 25 μM curcumin was significantly higher than that in control cells (p<0.05). As shown in Figure 2, the fluorescence intensity of the group treated with curcumin was significantly higher than that of the negative control group. These results indicate that curcumin inhibits the efflux of P-gp, thereby increasing the accumulation of drugs in MDR cells.
Figure 2.
Effects of curcumin on Rh123 retention (a) and accumulation (b) in HCT-8/VCR cells. a. The cells were incubated with Rh123 for 60 min, washed, and resuspended in medium with 10 μM curcumin or the vehicle control (0.1% DMSO) for 60 min. Rh123 fluorescence was measured using FACScan. b. The cells were treated with 25 μM curcumin or the vehicle control (0.1% DMSO). Rh123 (1 μg/ml) was added, and the cells were incubated for 120 min. Rh123 fluorescence was measured using flow cytometry. Data are presented as the mean ± SD (n = 3). A: Blank control group; B: Negative control group; C: Curcumin group. The mean fluorescence intensity of the curcumin group was significantly higher than that of the negative control group.** p<0.01 vs. negative control group.
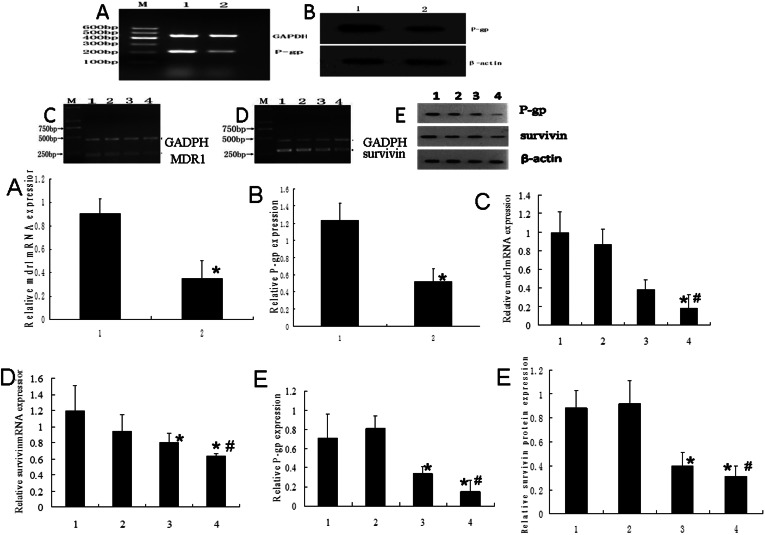
Inhibition of MDR1 gene expression
As shown by RT-PCR assays (Figure 3aA), curcumin significantly suppressed the expression of MDR1 mRNA in HCT-8/VCR cells. P-gp protein expression analyzed by western blotting was consistent with the RT-PCR results (Figure 3aB).
Figure 3.
Inhibition of the expression of MDR1 mRNA and P-gp and survivin mRNA and protein in HCT-8/VCR cells and xenograft tumors. A and B, MDR1 mRNA and P-gp protein expression in HCT-8/VCR cells. 1: control group, 2: curcumin group. RT-PCR showed significant reduction of MDR1 mRNA in curcumin-treated cells. P-gp protein levels detected by western blotting in the above-mentioned groups were consistent with the mRNA expression levels. C, D and E, MDR1 mRNA and P-gp and survivin mRNA and protein expression in xenograft tumors. 1: control group; 2: VCR group; 3: curcumin group; 4: curcumin+VCR group. (C) and (D): RT-PCR showed significant reduction of survivin mRNA and MDR1 mRNA in tumors treated with curcumin or curcumin+VCR. (E) Survivin and P-gp protein levels determined by western blotting in the above-mentioned groups were consistent with the mRNA expression levels. *: vs. control group, p<0.05, #: vs. curcumin group, p<0.05.
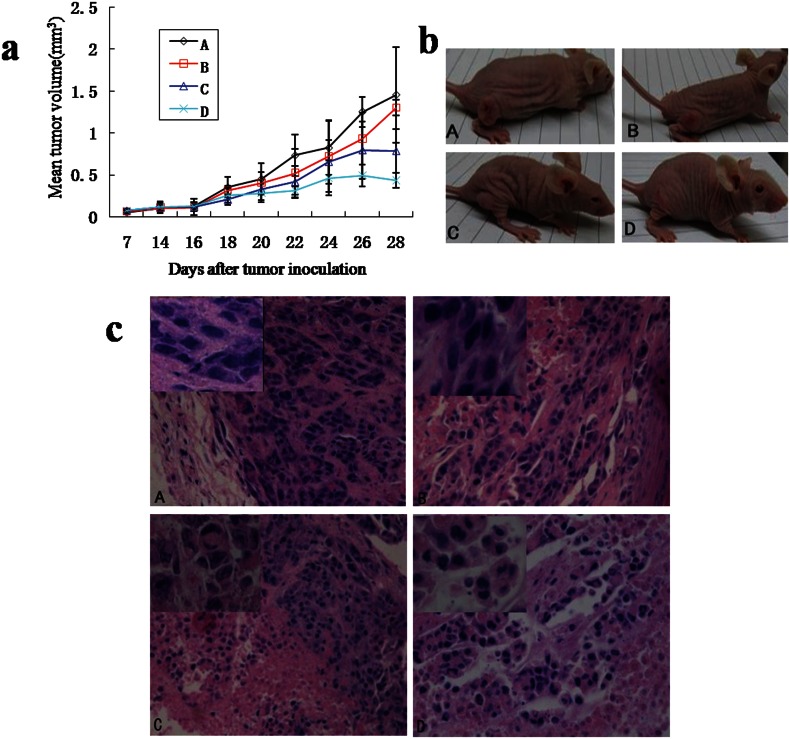
Effects of curcumin on an in vivo xenograft tumor model
After 14 days of treatment, xenografted mice were sacrificed and the tumors were resected. The PBS-treated group had larger tumors than the other groups (volume of 7,033.00 mm3). The mean tumor volume of the group treated with a combination of curcumin and VCR was 402.3 mm3, which was much smaller than that of the VCR-treated group (1338.4 mm3), the curcumin-treated group (782.5 mm3), and the PBS-treated group (Table 2, Figure 4A).
Table 2.
Effects of curcumin and VCR on the weight and volume of HCT-8/VCR tumors in nude mice and the inhibition rates of tumors (mean ± SD).
| Group | Mean tumor weight (g) | Inhibition rate of tumors | Mean volume (mm3) | |
| Before intervention | 14 days after intervention | |||
| A | 1.21±0.25 | / | 98.2±34.5 | 1406.6±128.3 |
| B | 1.13±0.27 | 9.3% | 106.1±39.3 | 1338.4±109.5 |
| C | 0.75±0.27 | 39.1% | 102.3±41.5 | 782.5±109.2 * #) |
| D | 0.42±0.23 | 65.3% | 103.5±40.8 | 402.3±58.4 * # ☆) |
vs. control group, p<0.01;
vs. VCR group, p<0.05;
vs. curcumin group, p<0.05.
A: control group; B: VCR group; C: curcumin group; D: curcumin+VCR group.
Figure 4.
Effect of curcumin on MDR in a HCT-8/VCR nude mice xenograft tumor model. Five-week-old female BALB/C nude mice were injected subcutaneously with HCT-8/VCR cells. Curcumin (50 mg/kg) and VCR (2 mg/kg) were administered twice daily through peritumoral injections for 14 days. After two weeks, the mice were sacrificed, and the tumors were harvested. A: control group; B: VCR group; C: curcumin group; D: curcumin+VCR group. (a) Effect of curcumin on the growth of HCT-8/VCR cells xenografted in nude mice, showing that curcumin inhibited tumor growth. (b) Representative tumor formation 14 days after intervention. (c) Hematoxylin-eosin staining of the tumors. (HE staining, ×200) A: control group; B: VCR group; C: curcumin group; D: curcumin+VCR group. The insets show magnified images representing typical changes of the tumor tissue.
Morphology of xenograft tumors
Light microscopy revealed that the tumor cells in the control group were round, oval, polygonal, and large, and they had hyperchromatic nuclei, larger nuclear slurry ratios, more caryokinesis, more heterogeneity, less karyopyknosis, fewer lymphocytes, and less necrosis than the tumor cells in the curcumin group and the curcumin plus VCR group (Figure 4C).
RT-PCR analysis of MDR1 and survivin mRNA in xenograft tumors
To determine the effects of curcumin on MDR1 and survivin mRNA expression in vitro, we analyzed MDR1 and survivin mRNA levels in tumors using RT-PCR. As shown in Figure 3bAB, RT-PCR demonstrated that curcumin significantly suppressed the expression of MDR1 and survivin mRNA in the xenograft tumors. The combination of VCR and curcumin suppressed the expression of MDR1 and survivin mRNA to a greater extent, whereas VCR produced little inhibition of MDR1 and survivin mRNA expression.
Western blot analysis of P-gp and survivin in xenograft tumors
To determine the effect of curcumin on P-gp and survivin protein expression in vivo we analyzed P-gp and survivin protein expression in tumors by western blot analysis. As shown in Figure 3bC, curcumin and the combination of curcumin and VCR in xenograft tumors significantly decreased the expression of P-gp and survivin protein. In contrast, VCR had little effect on survivin expression.
DISCUSSION
Colorectal carcinoma (CRC) is the most frequent malignancy of the alimentary system and accounts for approximately 40% of new cancer cases of the digestive tract (11). With increasing social and economic development and changes in lifestyle and diet, the incidence of CRC has increased annually. Currently, CRC treatment is surgery-based and supplemented by comprehensive treatments based on chemotherapy, radiation therapy, and Chinese medicine. Chemotherapy plays an important role in the comprehensive treatment of CRC, but MDR tumors are resistant to chemotherapy. There is an urgent need to establish an effective modality for overcoming MDR.
MDR is the major cause for the reduced effects of chemotherapy on tumors. It is necessary to find a strong agent with minimal side effects that can reverse the effects of MDR to improve the effect of chemotherapy on MDR tumors. Kuttan et al. (12) first raised the possibility of anti-tumor activity for turmeric and curcumin, as they initially showed that turmeric extract and curcumin reduced the development of animal tumors. Subsequent studies have shown that the inhibitory mechanism of curcumin on tumors is related to the induction of tumor cell apoptosis and the inhibition of tumor angiogenesis and invasion and metastasis of tumor cells. Anuchapreeda et al. found that curcumin decreased the MDR1 mRNA level in patient leukemic cells, especially in those with a high level of the MDR1 gene (13). In addition, Hui et al. (14) found that curcumin reversed the MDR of the melphalan-resistant multiple myeloma cell line MOLP-2/R by inhibiting the FA/BRCA pathway. A short treatment with curcumin induced DNA damage, decreased cell viability, and triggered apoptosis in MDR K562/A02 cells, and Cu2+ enhanced curcumin-mediated apoptosis through the generation of reactive oxygen species (15). The treatment of drug-resistant human cervical carcinoma KBV1 cells with curcumin increased their sensitivity to vinblastine, which was consistent with downregulation of the MDR-1 gene product, P-gp, on the cell plasma membrane (16). Curcumin (1–10 μM) was shown to decrease P-gp expression and reduced P-gp-mediated efflux in drug-resistant human cervical carcinoma cells (KBV1). Curcumin was also shown to increase Rh123 accumulation in a concentration-dependent manner (1–55 μM) and inhibit the efflux of Rh123 from these cells (17). Furthermore, curcumin was shown to sensitize human colorectal cancer to capecitabine through modulation of the expression of cyclin D1, cyclooxygenase-2 (COX-2), matrix metalloproteinases (MMP-9), vascular endothelial growth factor (VEGF), and C-X-C chemokine receptor type 4 (CXCR4) in an orthotopic mouse model (18). These findings suggest that curcumin may represent a new reversal agent for the chemosensitization of cancer cells.
In our study, the treatment of HCT-8/VCR cells with 6.25, 12.5, 25, 50, or 100 μM curcumin inhibited the growth of the cells in a concentration-dependent manner. It is assumed that curcumin induced apoptosis or necrosis of the cells; however, determination of the specific mechanism requires further investigation. Curcumin significantly increased the sensitivity of HCT-8/VCR cells to VCR, DDP, 5-FU, and HCPT. In an animal model, we demonstrated that curcumin inhibits xenograft growth. Cotreatment of curcumin and VCR significantly inhibited xenograft growth, showing a synergistic effect.
The mechanism of MDR formation is complex. P-gp-mediated MDR is considered to be the classic mechanism of resistance. P-gp is an ATP-dependent membrane transport protein encoded by the MDR1 gene, and it pumps exogenous cell substances from the inside to the outside of cells to protect tissues from exogenous toxic substances (19,20). In the MDR phenotype of tumors, P-gp can pump hydrophobic pro-lipid anti-cancer drugs out of cells, reduce the intracellular drug concentration, and cause MDR (21). Various studies have shown that the MDR of tumor cells can be reversed by inhibition of P-gp expression and function, which restores their sensitivity to chemotherapeutic drugs (22,23). Rh123 is a substrate of P-gp, which pumps Rh123 out of the cell to decrease the intracellular concentration. The accumulation or efflux of Rh123 in tumor cells can be used to assess the function of P-gp (24).
In the present study, we found that curcumin significantly increased the accumulation and retention of Rh123 in the colon cancer cell line HCT-8/VCR and reduced the efflux of Rh123. We speculated that curcumin could inhibit the drug transport function of P-gp to regulate the intracellular content of Rh123. The MTT assay showed that curcumin enhanced the sensitivity of HCT-8/VCR cells to a variety of chemotherapeutic drugs to reverse their MDR by inhibiting the transport function of P-gp so that the drugs could enter the cells. In the RT-PCR and western blot experiments, curcumin (25 μM)-treated cells had significantly lower levels of MDR1 gene and P-gp protein expression after treatment. In animal models, we demonstrated expression of the MDR1 gene and P-gp protein in xenografts treated with curcumin was lower than that in the control group and the VCR group. Expression of the MDR1 gene and the P-gp protein in xenografts that were cotreated with curcumin and VCR was lower than that in xenografts treated with curcumin alone. These results suggest that curcumin inhibited P-gp pump function and reduced the expression of P-gp protein, thereby reducing intracellular drug efflux, increasing the intracellular drug concentration, and enhancing the sensitivity of resistant cells to the chemotherapeutic drug. Thus, curcumin could partially reverse MDR.
Survivin is a regulator of apoptosis that may participate in cancer development (25,26), and it blocks apoptosis induced by a variety of nonrelated apoptosis triggers, including various anti-tumor agents (27-29). It has been reported that survivin is involved in chemotherapy resistance (30,31) and may serve as a radio- and chemo-resistance factor (32). Studies have shown that survivin expression is significantly higher in various cancer cells after treatment with anti-cancer drugs (33,34); therefore, survivin may potentially play a key role in resistance to anti-cancer drugs. In our study, we demonstrated that expression of the survivin gene and protein in xenografts treated with curcumin was lower than that in the control group and the VCR group, as shown by RT-PCR and western blot assays. Expression of the survivin gene and protein in xenografts that were cotreated with curcumin and VCR was lower than that in xenografts treated with curcumin alone. The mRNA and protein levels of survivin were decreased, which resulted in a decline in the anti-apoptotic function of survivin. Induction of tumor cell apoptosis or decreased survivin levels may decrease the turnover of P-gp or transport by P-gp in cells, thereby blocking the mechanism of resistance of tumor cells and reversing drug resistance.
In summary, curcumin reversed the MDR of tumor cells in vitro and in vivo. Despite these encouraging results, this study was limited in that it does not explain the specific mechanism underlying the effect of curcumin on P-gp and survivin and the relationship between P-gp and survivin in colon cancer. However, our results suggest that curcumin could be a promising chemosensitizer to counteract MDR in colon cancer.
ACKNOWLEDGMENTS
This study was supported by grants from the Key Project of Chinese Medicine of the Chongqing Municipal Health Bureau (2009-1-2). We thank the Key Laboratory of General Surgery, The First Affiliated Hospital, Chongqing Medical University for equipment and technical support.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. Ca-Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Pisani P, Bray F, Parkin DM. Estimates of the world-wide prevalence of cancer for 25 sites in the adult population. Int J Cancer. 2002;97(1):72–81. doi: 10.1002/ijc.1571. [DOI] [PubMed] [Google Scholar]
- 3.Song M, Zang W, Zhang B, Cao J, Yang G. GCS overexpression is associated with multidrug resistance of human HCT-8 colon cancer cells. J Exp Clin Canc Res. 2012;31 doi: 10.1186/1756-9966-31-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ross DD. Novel mechanisms of drug resistance in leukemia. Leukemia. 2000;14(3):467–73. doi: 10.1038/sj.leu.2401694. [DOI] [PubMed] [Google Scholar]
- 5.Roninson IB. The role of the MDR1 (P-glycoprotein) gene in multidrug resistance in vitro and in vivo.Biochem. Pharmacol. 1992;43(1):95–102. doi: 10.1016/0006-2952(92)90666-7. [DOI] [PubMed] [Google Scholar]
- 6.Shabbits JA, Mayer LD. P-glycoprotein modulates ceramide-mediated sensitivity of human breast cancer cells to tubulin-binding anticancer drugs. Mol. Cancer Ther. 2002;1(3):205–13. [PubMed] [Google Scholar]
- 7.Shan JZ, Xuan YY, Ruan SQ, Sun M. Proliferation-inhibiting and apoptosis-inducing effects of ursolic acid and oleanolic acid on multi-drug resistance cancer cells in vitro. Chin J Integr Med. 2011;17(8):607–11. doi: 10.1007/s11655-011-0815-y. [DOI] [PubMed] [Google Scholar]
- 8.Lin JK, Lin-shiau SY. Mechanisms of cancer chemoprevention by curcumin. Proc Natl Sci Counc Roe(B) 2001;25(2):59–66. [PubMed] [Google Scholar]
- 9.Tang XQ, Bi H, Feng JQ, Cao JG. Effect of curcumin on multidrug resistance in resistant human gastric carcinoma cell line SGC7901/VCR. Acta Pharmacol Sin. 2005;26(8):1009–16. doi: 10.1111/j.1745-7254.2005.00149.x. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhary PM, Roninson IB. Expression and activity of Pglycoprotein, a multidrug efflux pump, in human hematopoietic stem cells. Cell. 1991;66(1):85–94. doi: 10.1016/0092-8674(91)90141-k. [DOI] [PubMed] [Google Scholar]
- 11.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 12.Kuttan R, Bhannmathy P, Nirmala K, George MC. Potential anticancer activity of turmeric (Curcuma longa) Cancer Lett. 1985;29(2):197–202. doi: 10.1016/0304-3835(85)90159-4. [DOI] [PubMed] [Google Scholar]
- 13.Anuchapreeda S, Thanarattanakorn P, Sittipreechacharn S, Tima S, Chanarat P, Limtrakul P. Inhibitory effect of curcumin on MDR1 gene expression in patient leukemic cells. Arch Pharm Res. 2006;29(10):866–73. doi: 10.1007/BF02973907. [DOI] [PubMed] [Google Scholar]
- 14.Xiao H, Xiao Q, Zhang K, Zuo X, Shrestha UK. Reversal of multidrug resistance by curcumin through FA/BRCA pathway in multiple myeloma cell line MOLP-2/R. Ann Hematol. 2010;89(4):399–404. doi: 10.1007/s00277-009-0831-6. [DOI] [PubMed] [Google Scholar]
- 15.Lu JJ, Cai YJ, Ding J. The short-time treatment with curcumin sufficiently decreases cell viability, induces apoptosis and copper enhances these effects in multidrug-resistant K562/A02 cells. Mol Cell Biochem. 2012;360(1-2):253–60. doi: 10.1007/s11010-011-1064-2. [DOI] [PubMed] [Google Scholar]
- 16.Limtrakul P, Anuchapreeda S, Buddhasukh D. Modulation of human multidrug-resistance MDR-1 gene by natural curcuminoids. BMC Cancer. 2004;4:13. doi: 10.1186/1471-2407-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anuchapreeda S, Leechanachai P, Smith MM, Ambudkar SV, Limtrakul PN. Modulation of P-glycoprotein expression and function by curcumin in multidrug-resistant human KB cells. Biochem Pharmacol. 2002;64(4):573–82. doi: 10.1016/s0006-2952(02)01224-8. [DOI] [PubMed] [Google Scholar]
- 18.Kunnumakkara AB, Diagaradjane P, Anand P, Harikumar KB, Deorukhkar A, Gelovani J, et al. Curcumin sensitizes human colorectal cancer to capecitabine by modulation of cyclin D1, COX-2, MMP-9, VEGF and CXCR4 expression in an orthotopic mouse model. Int J Cancer. 2009;125(9):2187–97. doi: 10.1002/ijc.24593. [DOI] [PubMed] [Google Scholar]
- 19.Van der Holt B, Van den Heuvel-Eibrink MM, Van Schaik RH, van der Heiden IP, Wiemer EA, Vossebeld PJ, et al. ABCB1 gene polymorphisms are not associated with treatment outcome in elderly acute myeloid leukemia patients. Clin Pharmacol Ther. 2006;80(5):427–39. doi: 10.1016/j.clpt.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Leonard GD, Fojo T, Bates SE. The role of ABC transporters in clinical practice. Oncologist. 2003;8(5):411–24. doi: 10.1634/theoncologist.8-5-411. [DOI] [PubMed] [Google Scholar]
- 21.Al-Awqati Q. Regulation of ion channels by ABC transporters that secrete ATP. Science. 1995;269(5225):805–06. doi: 10.1126/science.7543697. [DOI] [PubMed] [Google Scholar]
- 22.Chen BA, Shan XY, Chen J, Xia GH, Xu WL, Schmit M. Effects of imatinib and 5-bromotetrandrine on the reversal of multidrug resistance of the K562/A02 cell line. Chin J Cancer. 2010;29(6):591–5. doi: 10.5732/cjc.009.10540. [DOI] [PubMed] [Google Scholar]
- 23.Shi LX, Ma R, Lu R, Xu Q, Zhu ZF, Wang L, et al. Reversal effect of tyroservatide (YSV) tripeptide on multi-drug resistance in resistant human hepatocellular carcinoma cell line BEL-7402/5-FU. Cancer Lett. 2008;269(1):101–10. doi: 10.1016/j.canlet.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 24.Chen LM, Liang YJ, Ruan JW, Ding Y, Wang XW, Ahi Z, et al. Reversal of P-gp mediated multidrug resistance in-vitro and in-vivo by FG020318. J Pharm Pharmacol. 2004;56(8):1061–6. doi: 10.1211/0022357043879. [DOI] [PubMed] [Google Scholar]
- 25.Ambrosini G, Adida C, Altieri DC. A novel anti-apoptosis gene, survivin, expressed in cancer and lymphoma. Nat. Med. 1997;3(8):917–21. doi: 10.1038/nm0897-917. [DOI] [PubMed] [Google Scholar]
- 26.Li F, Ambrosini G, Chu EY, Plescia J, Tognin S, Marchisio PC, et al. Control of apoptosis and mitotic spindle checkpoint by survivin. Nature. 1998;396(6711):580–4. doi: 10.1038/25141. [DOI] [PubMed] [Google Scholar]
- 27.LaCasse EC, Baird S, Korneluk RG, MacKenzie AE. The inhibitors of apoptosis (IAPs) and their emerg-ing role in cancer. Oncogene. 1998;17(25):3247–59. doi: 10.1038/sj.onc.1202569. [DOI] [PubMed] [Google Scholar]
- 28.Tamm I, Wang Y, Sausville E, Scudiero DA, Vigna N, Oltersdorf T, et al. IAP-family protein survivin inhibits caspase activity and apoptosis induced by Fas (CD95), Bax, caspases, and anticancer drugs. Cancer Res. 1998;58(23):5315–20. [PubMed] [Google Scholar]
- 29.Deveraux QL, Reed JC. IAP family proteins--suppressors of apoptosis. Genes Dev. 1999;13(3):239–52. doi: 10.1101/gad.13.3.239. [DOI] [PubMed] [Google Scholar]
- 30.Zhang M, Latham DE, Delaney MA, Chakravarti A. Survivin mediates resistance to antiandrogen therapy in prostate cancer. Oncogene. 2005;24(15):2474–82. doi: 10.1038/sj.onc.1208490. [DOI] [PubMed] [Google Scholar]
- 31.Tran J, Master Z, Yu JL, Rak J, Dumont DJ, Kerbel RS. A role for survivin in chemoresistance of endothelial cells mediated by VEGF. Proc Natl Acad Sci. 2002;99(7):4349–54. doi: 10.1073/pnas.072586399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodel C, Haas J, Groth A, Grabenbauer GG, Sauer R, Rodel F. Spontaneous and radiation-induced apoptosis in colorectal carcinoma cells with different intrinsic radiosensitivities: survivin as a radioresistance factor. Int J Radiat Oncol Biol Phys. 2003;55(5):1341–7. doi: 10.1016/s0360-3016(02)04618-7. [DOI] [PubMed] [Google Scholar]
- 33.Wang ZH, Xie Y H, Wang HB. Changes in survivin messenger RNA level during chemotherapy treatment in ovarian cancer cells. Cancer Biol Ther. 2005;4(7):716–9. doi: 10.4161/cbt.4.7.1782. [DOI] [PubMed] [Google Scholar]
- 34.Ikeguchi M, Liu J, Kaibara N. Expression of survivin mRNA and protein in gastric cancer cell line (MKN-45) during cisplatin treatment. Apoptosis. 2002;7(1):23–9. doi: 10.1023/a:1013556727182. [DOI] [PubMed] [Google Scholar]