Abstract
Background
Promoting help-seeking for mental health problems can result in improved treatment rates. For the most impact, social marketing interventions need to be tailored to targeted demographic subgroups. We investigated the influence of interactions between attitudes toward treatment and age, gender, ethnicity/race and education for both general medical and specialty care.
Method
Cross-sectional data from the 2001–2003 National Comorbidity Survey Replication (NCS-R) were analyzed using multivariate models adjusted for the sampling design and controlled for relevant clinical and sociodemographic factors.
Results
Greater comfort talking to a professional was associated with greater past-year specialty care across all demographic groups, while strongest for non-Latino whites and not evident for those 50–64 years old. For all demographic groups, reported willingness to seek professional help was associated with general medical care. However, for specialty care the association was much stronger for men compared to women. For African Americans, but not non-Latino whites, the perceived efficacy of mental health treatment improved the likelihood of past-year specialty use.
Conclusion
Our analyses suggest both the importance of understanding demographic differences in relevant attitudes and potential directions for marketing campaigns.
Keywords: Attitudes, Health services, Ethnicity, Race, Help seeking
Introduction
Multi-national epidemiological studies report that attitudes toward mental health treatment have a positive relationship with actual service use [1–5]. Prospective studies have also demonstrated that positive attitudes are associated with later mental health care [6, 7]. Attitudes toward mental health treatment may differ by age, gender, ethnicity/race and other key demographic variables.
Younger adults and males often report more negative attitudes toward mental health treatment, as compared to middle-aged adults and females [8]. Young adults may have worse attitudes because they are fearful about the nature of mental health treatment [9]. Females may not necessarily show more positive attitudes toward mental health treatment within ethnic/racial minority groups. A study of Mexican Americans found females to have more positive attitudes toward help seeking [10], while other studies have reported that U.S. African American and Latino males and females did not differ in certain attitudes toward mental health treatment [8, 11].
Some studies report more negative attitudes toward mental health treatment in ethnic/racial minority groups [12–15], while other studies find no differences or more positive attitudes [16–21]. Ethnic/racial group sampling differences (i.e., foreign versus U.S. born, college students vs. U.S. population) may account for these differences. Or, measuring attitudes as an overall concept rather than attitudes toward specific treatments may obscure more specific attitudinal differences. For example, one study found no differences for a general “receptivity to mental health services” between non-Latino whites and non-whites; however, when asked specifically about seeking out clergy for mental health problems, non-whites were more likely to believe in the efficacy of the clergy [16].
African American families report fearing institutionalization as a reason for not seeking mental health treatment [22] and non-white patients report greater perceptions of coercion into psychiatric hospitalization [23]. For African Americans and Latinos, mistrust of health care professionals and/or concerns about provider competence with their ethnic/racial group may decrease their comfort talking to professionals [24–26]. A qualitative analysis of an Afro-Caribbean community revealed that experiences of mistreatment and social exclusion by mental health professionals discouraged members from accessing mental health and substance abuse services [27]. Ethnic/racial minorities may be more inclined to utilize the family as primary support or alternative sources of care [16, 28–30], perhaps due to lack of belief in the efficacy of professional mental health treatments.
A higher education level may improve attitudes toward mental health treatment [16, 31], a finding likely related to increased awareness of the benefits of mental health treatments. A lower education level is associated with a greater likelihood of seeking mental health care in a general medical setting, as opposed to a specialty service setting [31, 32]. Persons with lower education levels may have had less exposure to specialty mental health treatment due to economic or social constraints.
Attitudes toward mental health treatment may be more strongly associated with specialty care than general medical care [6]. To follow through with specialty care, a certain attitudinal set may be required [33]. In general medical settings, a person may have sought care initially for a medical reason, requiring no prerequisite attitude. Or, attitudes associated with receptivity to general medical care for emotional problems may not yet have been adequately studied. Attitudes toward mental health treatment are more positive with previous treatment, also known as the ‘contact hypothesis’ [34, 35]. One study found the opposite where African Americans with prior mental health treatment had worse attitudes than African Americans with no prior treatment [36].
Attitudes can also interact with demographic characteristics. For example, females with more positive attitudes toward treatment may be more likely to seek general medical care than males with positive attitudes [6, 37]. In summary, numerous prior research studies have shown that attitudes may differ across demographic groups, and age, gender, ethnicity/race and education level are often associated with mental health care of any kind. However, only a few have examined whether differences in attitudes by demographic group are then associated with general medical or specialty care [6, 31, 32, 37].
Why would understanding differences in attitudes by sociodemographic subgroups be important? Discernment of which groups have negative attitudes and how such views differ can guide interventions tailored to improve attitudes. Negative attitudes toward mental health are related to perceptions of social norms, which often vary by demographic groups [38]. In the current study, we investigate the relationship of attitudes toward mental health treatment and past-year care in the National Comorbidity Survey-Replication (NCS-R), adjusting for variables that may also influence mental health care. We will examine whether age, gender, ethnicity/race and education level modify the relationship of attitudes toward mental health treatment and past-year care. We tested the following hypotheses: (1) younger age groups (18–34) will show stronger associations between comfort level talking to a professional and service use, compared to the older age groups (50–64, 65+), (2) males’ attitudes toward mental health treatment will be more strongly associated with service use than for women, (3) for African Americans and Latinos, increased comfort talking to a professional and greater belief in the efficacy of professional treatment will show stronger links to mental health care, as compared to non-Latino whites, and (4) for those with less education, attitudes toward mental health treatment will have stronger associations with general medical care, as opposed to those with more education.
Methods
Study population and data
The data are from the 2001–2003 NCS-R [39], a cross-sectional nationwide probability sample survey of non-institutionalized English-speaking U.S. residents ages 18 and older, designed to provide data on the prevalence of DSM-IV disorders and use of mental health services in the U.S. Study methods have been previously described (e.g., [40, 41]). The NCS-R is the largest data set measuring attitudes towards mental health service use across a broad range of sociodemographic groups which also includes a rich array of diagnostic and service use variables. In order to examine attitudes toward mental health treatment, we examined respondents who completed parts I and II of the survey (n = 5,691). Part II respondents included all Part I respondents with a DSM-IV disorder plus a random sample of respondents without disorders.
Measures
Age, gender, ethnic/racial identification and educational attainment
Table 1 provides categories and the weighted and unweighted numbers and proportions for demographic data. Respondents were asked whether they self-identified as being of Spanish or Latino descent. Persons who self-reported Latino descent, independent of how they coded themselves regarding race, were categorized as Latino. Other respondents self-classified as African American, non-Latino white or other groups.
Table 1.
Demographic characteristics of national comorbidity survey-replication respondents
| Unweighted frequency | Weighted frequency | Percent | |
|---|---|---|---|
| Sex | |||
| Female | 3,309 | 3,019 | 53.0 |
| Male | 2,382 | 2,673 | 47.0 |
| Age | |||
| 18–34 | 1,938 | 1,795 | 31.5 |
| 35–49 | 1,831 | 1,757 | 30.9 |
| 50–64 | 1,213 | 1,188 | 20.9 |
| 65+ | 709 | 952 | 16.7 |
| Race/ethnicity | |||
| Latino | 527 | 630 | 11.1 |
| African American/Black | 717 | 704 | 12.4 |
| Other | 268 | 217 | 3.8 |
| Non-Latino white | 4,179 | 4,141 | 72.8 |
| Education | |||
| 0–11 years | 848 | 954 | 16.8 |
| 12 years | 1,712 | 1,851 | 32.5 |
| 1 3–15 years | 1,709 | 1,568 | 27.5 |
| ≥16 years | 1,422 | 1,319 | 23.2 |
| Marital status | |||
| Married/cohabitating | 3,235 | 3,184 | 55.9 |
| Separated/widowed/divorced | 1,239 | 1,184 | 20.8 |
| Never married | 1,217 | 1,323 | 23.2 |
| Income | |||
| $0–$19,999 | 1,182 | 1,250 | 22.0 |
| $20–$34,999 | 920 | 905 | 15.9 |
| $35–$69,999 | 1,811 | 1,744 | 30.6 |
| $70,000+ | 1,778 | 1,793 | 31.5 |
| Insurance | |||
| None | 813 | 813 | 14.3 |
| Public | 715 | 715 | 12.8 |
| Private | 4,163 | 4,163 | 72.9 |
Additional covariates
In order to adjust for the influence of other factors associated with service use, we included the following variables: marital status, income, insurance status [2, 42–44], psychiatric need [43, 45, 46] and previous mental health treatment [43, 47]. Gender [6], socioeconomic status [31, 48, 49], and severity of psychiatric problems or distress have been shown to be associated with service use and sector of care [45, 47, 50] and were also included.
Previous use of mental health treatment was defined as any use of mental health services at least 1 year prior to the interview, irrespective of past-year use. Categories were: previous specialty mental health treatment (psychiatrist, psychologist and counselor) and previous general medical mental health treatment (i.e., non-psychiatric physicians). Respondents who reported use of both specialty and general medical treatment were categorized as having specialty mental health treatment only. Psychiatric need was categorized as the number of psychiatric disorders in the previous year (none, one, two, and three or more), determined by the World Mental Health Survey Initiative Version of the Composite International Diagnostic Interview (CIDI), using an algorithm based on ICD10/DSM IV criteria [51]. The WMH-CIDI is a structured interview, given by trained non-clinician interviewers, and generates diagnoses of mood disorders, anxiety disorders, and substance use disorders.
Attitudes toward mental health treatment
Our primary explanatory factors of interest reflected respondents’ attitudes toward mental health treatment. We used four questions to assess attitudes toward mental health treatment. These included (1) “If you had a serious emotional problem, would you go for professional help?” (2) “How comfortable would you feel talking about personal problems with a professional?” and (3) “How embarrassed would you be if your friends knew you were getting professional help for an emotional problem?” For the 4th question, respondents were asked to provide a percent of persons they believed benefited from professional treatment (range 0–100). The four attitudinal variables were not conceived or validated as a scale, and we hypothesized that each attitude might contribute independently to service use. A multicollinearity analysis of variance inflation factors among each of the four attitudes showed independence (variance inflation factors all fell below 1.26). Thus, we examined each attitude toward mental health treatment separately. The first three questions were rated on a 4-point scale, anchored with “definitely”, “probably”, “probably not”, and “definitely not”; these responses were dichotomized into a positive or negative attitude.
Past-year care
Respondents were asked whether they had talked to a professional about treatment for “emotions or nerves or use of alcohol or drugs”. Respondents were asked provider type and the month or year of their last mental health treatment. Past-year specialty care was coded when treatment was received from a psychiatrist, psychologist or counselor in the last 12 months. Past-year general medical care was coded when respondents received professional treatment for mental health problems from any non-psychiatric physician in the last 12 months. Respondents who reported any past-year specialty care were included only in past-year specialty care.
Statistical analysis
Descriptive statistics of the sample included means and proportions, adjusting for the complex sampling scheme (Table 1). We then applied multivariate methods in three stages, using logistic regression models. In the first stage, the four attitudes toward mental health treatment were entered into a model simultaneously, to assess their association with the outcomes of (1) past-year specialty care (yes/no), and then (2) past-year general medical care (yes/ no) for a mental health problem. In the second stage, we entered the four attitudes from stage one with the additional variables of interest (age, gender, ethnicity/race, and education level) and covariates known to be related to past-year care (marital status, income, insurance status, psychiatric need, previous use of specialty mental health treatment and previous use of general medical mental health treatment). Outcomes were again (1) past-year specialty care, and (2) past-year general medical care. For the third stage, all variables from the second stage were included in the regression analyses and we tested the effects of demographics on attitudes. Interactions assessed included age, gender, ethnicity/race or education by: (1) willingness to seek help, (2) comfort level talking to a mental health professional, (3) embarrassment about help seeking, and (4) the percentage of persons helped by professional treatment (i.e. treatment efficacy) per respondent’s perception. Each set of interactions with attitudes was included in one model, eliminating interactions until only those significant at p ≤ 0.25 [52, 53] remained in the model. We utilized backward elimination in the final model to ascertain the best model when considering all interactions and main effects of interest while not inflating the variance which may occur when including all significant and non-significant variables [53, 54]. We examined the area under the receiver operating characteristic curve to determine the strength of final models to distinguish specialty from non-specialty users, and general from non-general medical users for mental health care. All descriptive statistics and results report weighted data. All analyses were conducted in SAS Version 9.1 using the survey commands, which adjust for NCS Part II weights in the sampling design.
Results
The majority of U.S. residents represented by the survey were non-Latino white (72.8%) and married (55.9%) with private medical insurance (72.9%) (see Table 1). Half of respondents had more than a high school education (50.7%), with 23% having earned a college degree. Thirty percent of the population was estimated to have had previous lifetime specialty mental health treatment and 10% reported lifetime use of general medical providers only for mental health treatment.
Attitudes toward mental health treatment were generally positive, with the majority reporting a willingness to go for professional help if they had a serious emotional problem (83.7%) and feeling comfortable talking with a mental health professional (79.3%). About one-third of respondents said they would be somewhat or very embarrassed if their friends knew they were getting professional help for an emotional problem (33.3%). Approximately 72% of respondents believed that at least half of those who sought professional help for a serious emotional problem would benefit.
Stage one and two
For stage one, willingness to seek help for serious emotional problems was positively associated with past-year specialty care (data not shown) (OR = 2.52, 95% CI 1.57–4.06) and comfort talking with a professional (OR = 1.65, 1.12–2.44). The odds of past year specialty care were decreased with greater embarrassment if others were to know about their seeking professional help (OR = 0.66, 0.51–0.85). Perceived treatment efficacy was not significantly related to past-year specialty care. In the stage one model, use of past-year general medical care for emotional problems was not associated with any of the four attitudes examined.
For stage two, we examined the effect of the four attitudes on past-year specialty and general medical care, controlling for the covariates of age group, gender, ethnicity/race, marital status, income, education level, insurance status, psychiatric need, and (1) previous specialty mental health treatment for the model of specialty care or (2) previous general medical mental health treatment for the model of general medical care. The relationship of attitudes toward mental health treatment on past-year specialty care were similar to the stage one models, except that comfort level talking to a professional about personal problems was no longer statistically significant (p = 0.07). All covariates entered except gender and ethnicity/race were significantly related to past-year specialty care. For general medical care, attitudinal measures remained non-significant while income, psychiatric need and a history of general medical care were significantly related to past-year use.
Stage three
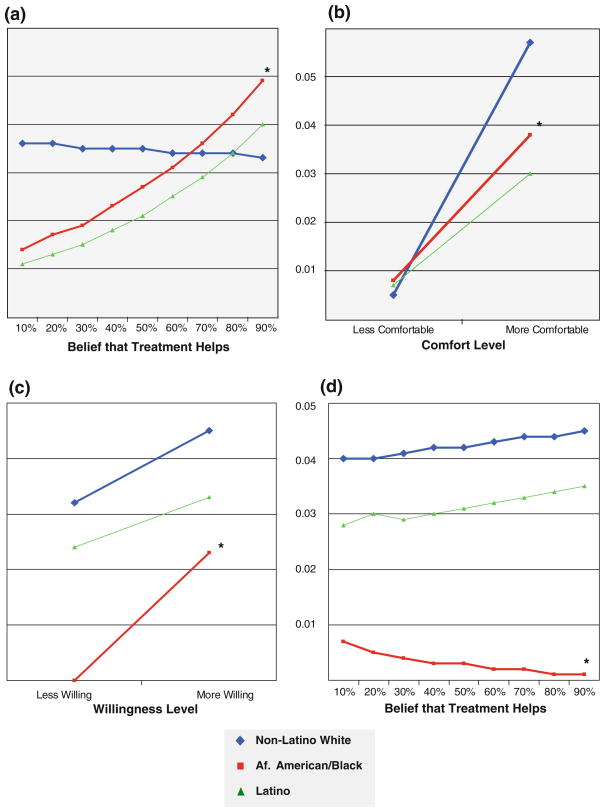
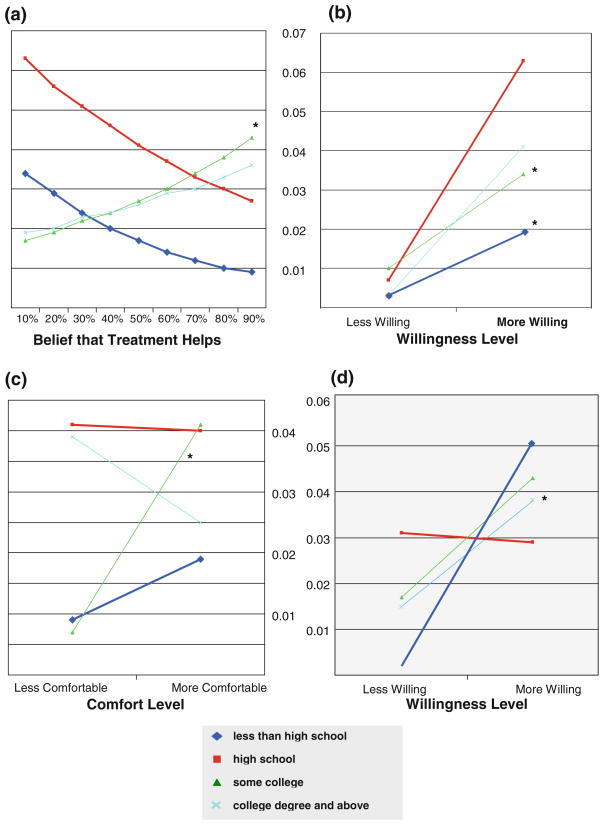
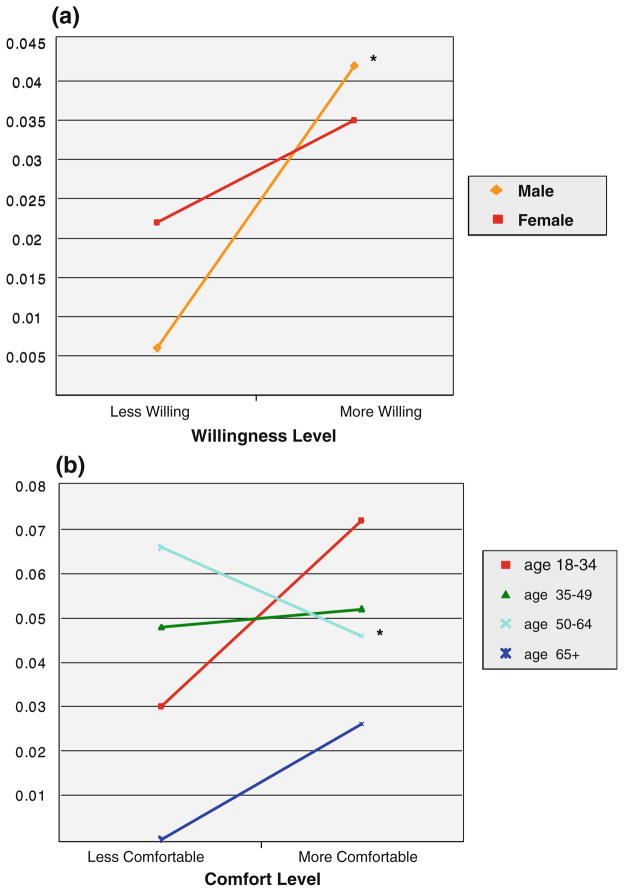
Two stage-three models were evaluated for (1) specialty care and (2) general medical care (Table 2). Figures 1, 2 and 3 depict the best-fitting probability of use to aid in interpretation of significant interactions from stage three. Each model evaluated interactions between age, gender, ethnicity/race and education level for each of the four attitudes on past-year use. We included all interactions of interest (n = 16) and added to the variables in the stage two model. When all interactions above a p-value of 0.25 were removed by backwards elimination from the model, this was considered the final model. The area under the receiver operating curve for the specialty care final model was 0.863, indicating excellent ability to identify those who seek help and those who do not. In the final specialty care model, comfort talking to a professional remained positively associated with past-year specialty care (p < 0.01) and five significant interaction effects were noted (see Figs. 1, 2, 3). For past-year general medical care, the area under the receiver operating cure was 0.897, indicating excellent ability to identify those who seek general medical care and those who do not, based on the variables in the model. In this model the main effect of willingness to seek help on general medical use was significant (p = 0.02), in contrast to prior models, and six interactions effects were observed (Figs. 1, 2, 3).
Table 2.
Stage three backward elimination model for past-year service use (results for attitude main effects and interactions)
| Model variables or interactions | Interaction effect odds ratio | 95% CI |
|---|---|---|
| Final model for specialty mental health care | ||
| Willingness to seek professional help | 1.95 | 0.87–−4.35 |
| Comfort level talking to a professional** | 3.20 | 1.50–6.84 |
| Embarrassed if others knew | 0.83 | 0.54–1.27 |
| Belief that professional treatment helpsa | 0.99 | 0.93–1.06 |
| Willingness to seek help by gender* | ||
| Female | 0.48 | 0.51–0.94 |
| Male | 1.00 | – |
| Willingness to seek help by education level** | ||
| Less than high school | 0.65 | 0.22–1.99 |
| High school | 1.00 | – |
| Some college | 1.42 | 0.50–4.05 |
| College degree | 10.52 | 2.20–50.35 |
| Comfort level by age group*** | ||
| 18–34 | 1.00 | – |
| 35–49 | 0.44 | 0.17–1.17 |
| 50–64 | 0.27 | 0.09–0.84 |
| 65+ | 0.81b | 0.32–2.08b |
| Comfort level by ethnicity/race* | ||
| Non-Latino white | 1.00 | – |
| African American/Black | 0.35 | 0.12–1.00 |
| Latino | 0.33 | 0.06–1.71 |
| Belief that professional treatment helps by ethnicity/race* | ||
| Non-Latino white | 1.00 | – |
| African American/Black | 1.41 | 1.04–1.90 |
| Latino | 1.41 | 0.96–2.07 |
| Final model for general medical mental health care | ||
| Willingness to seek professional help* | 12.68 | 1.43–112.38 |
| Comfort level talking to a professional | 1.00 | 0.34–2.96 |
| Embarrassed if others knew | 1.20 | 0.54–2.63 |
| Belief that professional treatment helpsa | 0.91 | 0.76–1.10 |
| Willingness to seek help by education level*** | ||
| Less than high school | 0.12 | 0.02–0.64 |
| High school | 1.00 | – |
| Some college | 0.15 | 0.03–0.65 |
| College degree | 0.69 | 0.06–7.98 |
| Willingness to seek help by ethnicity/race*** | ||
| Non-Latino white | 1.00 | – |
| African American/Black | 11b | 2.70b–4.50b |
| Latino | 0.99 | 0.14–7.00 |
| Comfort level by education level* | ||
| Less than high school | 2.08 | 0.34–12.52 |
| High school | 1.00 | – |
| Some college | 6.58 | 1.13–38.24 |
| College degree | 0.64 | 0.08–5.47 |
| Embarrassed by ethnicity/race* | ||
| Non-Latino white | 1.00 | – |
| African American/Black | 0.18 | 0.04–0.73 |
| Latino | 0.77 | 0.14–4.16 |
| Belief that professional treatment helps by ethnicity/race* | ||
| Non-Latino white | 1.00 | – |
| African American/Black | 0.60 | 0.38–0.96 |
| Latino | 1.03 | 0.64–1.68 |
| Belief that professional treatment helps by education level* | ||
| Less than high school | 0.88 | 0.55–1.40 |
| High school | 1.00 | – |
| Some college | 1.57 | 1.01–2.44 |
| College degree | 1.46 | 0.94–2.29 |
O.R. denotes how subgroup odds ratios differ from a comparison subgroup’s odds ratio. The O.R. of 1 is the standard effect of the attitude to compare to for interactions as it improves from negative to positive. A significant O.R. below 1 shows a reduced effect of the attitude, compared to the standard effect. An O.R. above 1 shows an increased effect of the attitude, compared to the standard effect
Models included four attitudes toward mental health treatment, age, ethnicity/race, education level, marital status, income, insurance status, psychiatric disorder, previous use of specialty (or general) mental health treatment and significant interactions
Significant at p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001
Odds reported for likelihood of a 10 point change on a scale of 0–100
O.R.s should be (×105)—odds are large due to small predicted probability of use for less than willing African American/Black group
Fig. 1.
Health attitudes and mental health service utilization, by ethnicity/race. Last year predicted probability of specialty service use by: a belief that professional treatment helps, b comfort level talking to a professional. Last year predicted probability of general medical service use by: c willingness to seek professional help, d belief that professional treatment helps. *Statistically significant difference with non-Latino Whites as reference group. The figures depict probability of use in separate groups (e.g., less willing group versus a more willing group). Final model included four attitudes toward mental health treatment, age, ethnicity/race, education level, marital status, income, insurance status, psychiatric disorder status, previous use of mental health treatment and interactions at p < 0.25 (only < 0.005 reported)
Fig. 2.
Health attitudes and mental health service utilization, by education level. Last year predicted probability of general medical service use by: a belief that professional treatment helps, b willingness to seek professional help. Last year predicted probability of: c general medical service use by comfort level talking to a professional, d specialty service use willingness to seek professional help. *Statistically significant difference with high school as the reference group. The figures depict probability of use in separate groups (e.g., less willing group vs. a more willing group). Final model included four attitudes toward mental health treatment, age, ethnicity/ race, education level, marital status, income, insurance status, psychiatric disorder status, previous use of mental health treatment and interactions at p < 0.25 (only< 0.005 reported)
Fig. 3.
Health attitudes and mental health service utilization, by gender/age group. a Last year predicted probability of specialty service use by willingness to seek professional help, b last year predicted probability of specialty service use by comfort level talking to a professional. *Statistically significant difference with 18–34 as the reference group. The figures depict probability of use in separate groups (e.g., less willing group vs. a more willing group). Final model included four attitudes toward mental health treatment, age, ethnicity/ race, education level, marital status, income, insurance status, psychiatric disorder status, previous use of mental health treatment and interactions at p < 0.25 (only< 0.005 reported)
Ethnicity/race
The association with past-year specialty care by belief in treatment efficacy differed by ethnicity/race (p = 0.02). As African Americans reported a belief that more people would benefit from mental health treatment, use of past-year specialty care improved significantly (Fig. 1a), while this association was not evident for non-Latino whites. For non-Latino whites, as comfort level talking to a professional improved, so did past-year specialty care (Fig. 1b). However, for African Americans, greater comfort was not associated with increased likelihood of specialty care to the same degree as non-Latino whites. Latinos showed a similar trend as African Americans but did not differ significantly from non-Latino whites.
For general medical care, willingness to seek help had a different association by ethnicity/race (p < 0.001). For African Americans, greater willingness to seek help was related to more past-year general medical care, as compared to non-Latino whites (see Fig. 1c). A belief in the efficacy of treatment had a different effect for non-Latino whites as compared to African Americans (Fig. 1d) on general medical care. That is, for non-Latino whites and Latinos, the more respondents believed in treatment efficacy, the more they reported using general medical services for mental health care. However, for African Americans, greater belief in treatment efficacy was not associated with an increased likelihood of past-year general medical care. Embarrassment about help seeking and its association with general medical care was different when comparing non-Latino whites and Latinos to African Americans (p = 0.05). For non-Latino whites and Latinos, the likelihood of use was significantly higher with less embarrassment if others knew about their help seeking (figure not shown).
Education level
For general medical care, belief in treatment efficacy showed an interaction by education level. That is, for those reporting a high school education, as belief in treatment efficacy increased, past-year general medical care generally declined (Fig. 2a). However, for those reporting some college, belief that professional treatment would be beneficial was associated with increased likelihood of past-year general medical care (p < 0.05). Willingness to seek help did appear to be an important attitude for persons with a high school education, as the likelihood of past-year general medical care increased with greater willingness (p = 0.01). However for those with a less than high school education and those with some college, the effect of a willingness to seek care was minimal compared to their high school counterparts (see Fig. 2b). Comfort level was associated with increased odds of past-year general medical care for those with some college, while high school educated persons did not have increased use with increased comfort seeking care (p < 0.05) (Fig. 2c).
For past-year specialty care, willingness to seek help was associated with increased use for persons with a college degree and above, as compared to persons with a high school education (p = 0.006) (see Fig. 2d).
Gender and age
The effect of willingness to seek help on specialty service use differed by gender (p = 0.02). Males reporting a low willingness to seek help were less than half as likely as females reporting low willingness to have sought specialty services in the past year (see Fig. 3a). As males’ willingness to seek help improved, the likelihood of care greatly improved. Thus, the impact of this attitude on specialty care appeared particularly relevant for males. A greater comfort level talking to a professional and its effect on specialty care differed by age group (p < 0.001). For 18–34 year olds, as comfort level improved, so did past-year specialty use. However, for each of the other age groups, greater comfort level did not increase the use of specialty services to the same degree (see Fig. 3b) as for the younger age group. For the 50–64 year olds, this difference was statistically significant (p ≤ 0.01).
Discussion
This study augments the knowledge base on the importance of positive attitudes in seeking mental health care by quantifying the contribution of specific interactions for key sociodemographic groups for U.S. non-institutionalized adults. We found significant variation in the use of mental health care by age, ethnicity/race, gender, and education, further varying with attitude toward mental health treatment: an interaction effect. Attitudes coupled with demographic factors can be used to target those who at some future point may need mental health treatment but have attitudes that would be a barrier to treatment. Changing attitudes could be central to increasing professional mental health treatment for targeted subgroups of the population with poor attitudes.
The major interaction effects noted for specialty care were increased use by African Americans with stronger beliefs in treatment efficacy, increased use by Latinos and non-Latino whites who had greater comfort levels talking to a professional, increased use by males who reported greater willingness to seek help, and greater use for higher education levels with greater willingness to seek help. General medical care for mental health issues increased for African Americans more willing to seek help, for Latinos and non-Latino whites with a stronger belief in treatment efficacy, and attitudes differed in their impact on use by education level. We discuss these interactions more fully below. As to main effects, for specialty care, comfort level remained important for all demographic groups, and for general medical care, greater willingness to seek help remained important for all demographic subgroups.
General medical care patients with emotional problems report reluctance to see mental health specialists [55, 56], which may be related to specialty care carrying the label of “psychiatric patient” and related stigma. We found support for findings that unique attitudinal sets may lead one to different sectors of care for the treatment of emotional problems [57]. In some cases we found that positive attitudes appeared inversely related to care. For example, belief in treatment efficacy was associated with less general medical care for persons with high school and less than high school educations. One explanation may be that improved attitudes are associated with use of one sector while lowering use in another sector.
For 18–34 year olds, greater comfort levels talking to a professional showed a greater likelihood of seeking specialty services than 50–64 year olds, consistent with our hypothesis. This age group is likely to have had limited experiences with psychiatrists, psychologists and counselors, potentially increasing their apprehension to seek care. Adolescents and college students report feeling uncomfortable talking with professionals, such as feeling the problem is too personal to tell anyone, or fearfulness about what the treatment involves [9, 58, 59].
For males, a greater willingness to seek help was associated with greater odds of specialty care, whereas for females this attitude was not associated with greater use to the same degree. Other attitudes we studied were not more strongly associated to care in males compared to females as we had predicted. A previous study found a somewhat opposite finding, where attitudes toward mental health treatment in males were not significantly associated with care but were associated to use in females [6]. Differences in results could be attributed to our inclusion of interactions and additional covariates in the use of specialty services, and also the attitudes differed in content. In a previous study, African American and Latino males and females reported similar attitudes toward mental health treatment [8]. It would be helpful to examine these subgroups further, examining gender differences within each subgroup (i.e. a three-way interaction). It may be that generational and cultural experiences influence the formation of attitudes toward mental health treatment more than gender-related experiences.
We did not find support for our hypothesis that comfort level talking to professionals would be associated with greater use for African Americans. For African Americans, we did find support for our hypotheses that a greater belief in treatment efficacy was associated with increased likelihood of specialty care. These findings are consistent with an epidemiological survey which found that for African Americans, perceived efficacy of psychiatric medication and medication side effects were the variable most strongly associated to willingness to use medication [60]. Ethnic/racial minorities may be more inclined to utilize the family as the primary support or alternative sources of care [16, 28], perhaps due to lack of belief in treatment efficacy. For African Americans, greater willingness to seek help was particularly relevant. According to Dana [61], ethnocentric models of service delivery may inadvertently overpathologize minority behaviors that differ from those of the majority culture [62] and as a consequence, require that minorities strongly value professional treatment to enter mental health care. For Latinos and non-Latino whites, reporting less embarrassment about treatment seeking was associated with general medical care, in contrast to African Americans. For any group, behaving in contradiction to social norms may increase stigmatization about mental illness and help seeking behaviors [38]. A social marketing strategy for non-Latino whites and Latinos should consider current social norms and the inclusion of community role models who have sought mental health treatment.
For non-Latino whites and Latinos a belief in treatment efficacy was associated with general medical care, a consistent finding with our hypotheses for Latinos. In strong and tightly meshed Latino family networks, individuals may be hesitant or be discouraged from seeking mental health services in the specialty sector [28, 29]. It is only when family support systems are lacking or become ineffectual in handling a crisis that Latinos may seek professional help [63]. A greater belief in treatment may then lead Latinos more often to general medical care; social marketing campaigns might target this attitude. The differences between African Americans and Latinos serve as a reminder that these groups have unique histories of interaction with the U.S. mental health system, and likely different barriers associated with entry into and retention in mental health treatment [13, 25, 26].
We found general support for our hypotheses that education level and the attitudes we studied would have stronger associations to general medical care. For general medical care, persons reporting a high school education and a greater willingness to seek help had the strongest association to past-year use, consistent with findings and our hypothesis that a lower education level is associated with preferring treatment in a general medical setting [31, 32]. The associations were not always greatest for lower education levels. For the some-college group, comfort level talking to a professional and belief in treatment efficacy were associated with greater general medical use than for those with a high school education level. While about 18% of the some-college group was perhaps in college (18–24 years old), the majority were older (25–93 years). These findings are particularly relevant because the “some college” group comprises more than a quarter of United States citizens, and we provide preliminary information on which attitudes might be most salient in this understudied demographic group. For persons with a college degree, willingness to seek help was associated with increased odds of past-year specialty care, consistent with prior reports [31]. However, one survey reported contradictory findings that higher education levels decreased willingness to take psychiatric medications [64]; thus, marketing campaigns should clarify that mental health treatment can involve medications or counseling/psychotherapy, which may be preferred by some [56]. Interestingly, we found no main effect of education level on mental health care in multivariate models; thus, targeting subgroups of education levels may be less effective when specific attitudes are not taken into consideration.
An important limitation to this study is the cross-sectional design and we report on associations to service use as opposed to having assessed respondents’ attitudes prior to any service use. Prospective follow-up would allow for greater certainty about the temporal relationships among the constructs. Although we found that demographic variables do modify the association of attitudes toward mental health treatment and care, we cannot conclude that a causal relationship between attitudes and care exists. In this study we adjusted for numerous variables, including previous mental health treatment which was defined as any treatment greater than one year prior to data collection. Previous mental health treatment may be associated to either negative or positive attitudes toward mental health treatment, with differential effects by race. Diala et al. [36], using the original NCS dataset, found that African Americans with prior mental health treatment had more negative attitudes toward treatment than whites with prior mental health treatment. The current study included lifetime previous mental health treatment as a covariate only (i.e. no interaction effects were tested with prior use) and therefore did not replicate the Diala models. Additionally, retrospective questions about prior mental health treatment may be subject to recall bias. In this study, Latinos were English speaking and thus not representative of all Latinos in the U.S. Further, Latinos were grouped under an umbrella category; subgroups (e.g., Mexican Americans, Puerto Ricans) may have different associations of attitudes toward mental health treatment with care. These findings should be replicated in future studies disaggregating the Latino subgroups.
We provide a summary of our integration of the most relevant findings from this study in Table 3, with a specific focus on social marketing strategies. The table describes the target group for whom the message may be most applicable and for which setting the message is targeted, either general or specialty care. We provide some ideas about content that should be central to the message. Willingness to seek help is a non-specific attitude. In this regard, this attitude may be salient because it is capturing other barriers that are not assessed by other more specific questions about comfort level, embarrassment, or benefits. To target this attitude, we suggest “getting facts” and talking to the doctor about concerns and barriers decreasing willingness to seek help. We suggest that talking to the doctor is “worth the discussion”, which may then improve attitudes toward treatment. We believe these social marketing messages would be useful content for the planning stages of mental health services social marketing campaigns [65].
Table 3.
Summary of study findings: main effects and important interactions
| Target attitude | Target audience | Potential intervention messages/central theme |
|---|---|---|
| Willingness to seek professional help for an emotional or substance- related problem | Males (to improve specialty care use) Persons with a college degree and higher (to improve specialty care use) All demographic groups (to improve general medical care use) Particularly helpful for African Americans (to improve general medical care use) Particularly helpful for persons with a “ high school education only” and “ a college degree and higher” (to improve general medical care use) |
Have an open mind about what’s on your mind Talk to your doctor for more information, get the facts about treatment Talk about any concerns you may have about professional mental health treatment To increase general medical care use, specify “ Your family (or primary care) doctor” has an open mind about what’s on your mind Family doctors help as many people with emotional concerns as other professionals |
| Comfort level talking to a professional about personal problems | All demographic groups (to improve specialty care use) Particularly helpful for Latinos and non-Latino whites (to improve specialty care use) Helpful to target all adult age groups except 50–64 year olds (to improve specialty care use) Particularly helpful to target persons reporting “ some college” (to improve general medical care) |
Talking to a doctor about your emotional problems can be unfamiliar and uncomfortable. Most people feel much more comfortable after taking the first step to talk Talking about personal problems is confidential. Mental health providers are licensed health professionals: Problems you may be experiencing are commonly treated by mental health professionals (replace with a general medical provider description when targeting improved use for general medical) E.g. XX% of family doctor’s patients are treated for emotional problems (to improve general medical care use) |
| Embarrassment if others knew | Particularly helpful for Latinos and non- Latino whites (to improve general medical care) | Overarching goal: reduce stigma Depict a role model seeking help; communicate information that xx% of the demographic being targeted seeks help at some point E.g. did you know XX% Latinas seek help for emotional problems from their family doctor? |
| Belief in the benefits of mental health treatment (treatment efficacy) | Particularly helpful for African Americans and to a lesser extent Latinos (to improve specialty care use) Particularly helpful for Latinos and non-Latino whites (to improve general medical care) Particularly helpful for persons with at least some college and higher (to improve general medical care use) |
Mental health treatments by specialists (or by general medical providers) can work for everyone. Ask about what treatments might work for you. Most people find relief from a variety of treatment options for emotional problems Important to depict a role model here and provide specific relevant facts as a person may believe “ Treatment works for others but not for me (ex: an African American male)” |
“Target audience” is those groups who had a positive attitude which was then associated to service use. All messages should be marketed using similar demographic role models in media message (e.g., males if targeting males)
Contributor Information
Jodi M. Gonzalez, Email: gonzalezjm1@uthscsa.edu, Department of Psychiatry, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA
Margarita Alegría, Email: malegria@charesearch.org, Center for Multicultural Mental Health Research, Somerville, USA.
Thomas J. Prihoda, Email: prihodat@uthscsa.edu, Department of Psychiatry, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA
Laurel A. Copeland, Email: copelandl@uthscsa.edu, Department of Psychiatry, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA. Veterans Affairs HSR&D (VERDICT), San Antonio, TX, USA
John E. Zeber, Email: zeber@uthscsa.edu, Department of Psychiatry, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA. Veterans Affairs HSR&D (VERDICT), San Antonio, TX, USA
References
- 1.Leaf PJ, Livingston MM, Tischler GL, Weissman MM, Holzer CE, III, Myers JK. Contact with health professionals for the treatment of psychiatric and emotional problems. Med Care. 1985;23:1322–1337. doi: 10.1097/00005650-198512000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lin E, Parikh SV. Sociodemographic, clinical, and attitudinal characteristics of the untreated depressed in Ontario. J Affect Disord. 1999;53:153–162. doi: 10.1016/s0165-0327(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 3.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 4.Smith LD, McGovern RJ, Peck PL. Factors contributing to the utilization of mental health services in a rural setting. Psychol Rep. 2004;95:435–442. doi: 10.2466/pr0.95.2.435-442. [DOI] [PubMed] [Google Scholar]
- 5.Edlund MJ, Fortney JC, Reaves CM, Pyne JM, Mittal D. Beliefs about depression and depression treatment among depressed veterans. Med Care. 2008;46:581–589. doi: 10.1097/MLR.0b013e3181648e46. [DOI] [PubMed] [Google Scholar]
- 6.Leaf PJ, Bruce ML. Gender differences in the use of mental health-related services: a re-examination. J Health Soc Behav. 1987;28:171–183. [PubMed] [Google Scholar]
- 7.Jorm AF, Medway J, Christensen H, Korten AE, Jacomb PA, Rodgers B. Public beliefs about the helpfulness of interventions for depression: effects on actions taken when experiencing anxiety and depression symptoms. Aust N Z J Psychiatry. 2000;34:619–626. doi: 10.1080/j.1440-1614.2000.00761.x. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez JM, Alegria M, Prihoda TJ. How do attitudes toward mental health treatment vary by age, gender, and ethnicity/race in young adults? J Community Psychol. 2005;33:611–629. [Google Scholar]
- 9.Kushner MG, Sher KJ. Fear of psychological treatment and its relation to mental health service avoidance. Prof Psychol-Res Pr. 1989;20:251–257. [Google Scholar]
- 10.Sanchez AR, Atkinson DR. Mexican-American cultural commitment, preference for counselor ethnicity, and willingness to use counseling. J Counsel Psychol. 1983;30:215–220. [Google Scholar]
- 11.Nickerson KJ, Helms JE, Terrell F. Cultural mistrust, opinions about mental illness, and Black students’ attitudes toward seeking psychological help from White counselors. J Counsel Psychol. 1994;41:385. [Google Scholar]
- 12.Sanchez AR, King M. Mexican Americans’ use of counseling services: Cultural and institutional factors. J Coll Student Person. 1986;27:344–349. [Google Scholar]
- 13.Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 14.Nadeem E, Lange JM, Miranda J. Mental health care preferences among low-income and minority women. Arch Womens Mental Health. 2008;11:93–102. doi: 10.1007/s00737-008-0002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sleath B, West S, Tudor G, Perreira K, King V, Morrissey J. Ethnicity and depression treatment preferences of pregnant women. J Psychosom Obstet Gynaecol. 2005;26:135–140. doi: 10.1080/01443610400023130a. [DOI] [PubMed] [Google Scholar]
- 16.Leaf PJ, Bruce ML, Tischler GL, Holzer CE., III The relationship between demographic factors and attitudes toward mental health services. J Community Psychol. 1987;15:275–284. doi: 10.1002/1520-6629(198704)15:2<275::aid-jcop2290150216>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 17.Furnham A, Andrew R. A cross-cultural study of attitudes towards seeking psychological help. Psychol Rep. 1996;79:289–290. doi: 10.2466/pr0.1996.79.1.289. [DOI] [PubMed] [Google Scholar]
- 18.Sheikh S, Furnham A. A cross-cultural study of mental health beliefs and attitudes towards seeking professional help. Soc Psychiatry Psychiatr Epidemiol. 2000;35:326–334. doi: 10.1007/s001270050246. [DOI] [PubMed] [Google Scholar]
- 19.Anglin DM, Alberti PM, Link BG, Phelan JC. Racial differences in beliefs about the effectiveness and necessity of mental health treatment. Am J Community Psychol. 2008;42:17–24. doi: 10.1007/s10464-008-9189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schnittker J, Pescosolido BA, Croghan TW. Are African Americans really less willing to use health care? Soc Probl. 2005;52:255–271. [Google Scholar]
- 21.Diala CC, Muntaner C, Walrath C, Nickerson K, LaVeist T, Leaf P. Racial/ethnic differences in attitudes toward seeking professional mental health services. Am J Public Health. 2001;91:805–807. doi: 10.2105/ajph.91.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takeuchi DT, Bui KV, Kim L. The referral of minority adolescents to community mental health centers. J Health Soc Behav. 1993;34:153–164. [PubMed] [Google Scholar]
- 23.Bindman J, Reid Y, Szmukler G, Tiller J, Thornicroft G, Leese M. Perceived coercion at admission to psychiatric hospital and engagement with follow-up—a cohort study. Soc Psychiatry Psychiatr Epidemiol. 2005;40:160–166. doi: 10.1007/s00127-005-0861-x. [DOI] [PubMed] [Google Scholar]
- 24.Whaley AL. Cultural mistrust of white mental health clinicians among African Americans with severe mental illness. Am J Orthopsychiatry. 2001;71:252–256. doi: 10.1037/0002-9432.71.2.252. [DOI] [PubMed] [Google Scholar]
- 25.Whaley AL. Cultural mistrust and mental health services for African Americans: a review and meta-analysis. Counsel Psychol. 2001;29:513–531. [Google Scholar]
- 26.Echeverry JJ. Treatment barriers accessing and accepting professional help. In: Garcia JG, Zea MC, editors. Psychological interventions and research with Latino populations. Allyn & Bacon; Needham Heights: 1997. [Google Scholar]
- 27.Mclean C, Campbell C, Cornish F. African-Caribbean interactions with mental health services in the UK: experiences and expectations of exclusion as (re)productive of health inequalities. Soc Sci Med. 2003;56:657–669. doi: 10.1016/s0277-9536(02)00063-1. [DOI] [PubMed] [Google Scholar]
- 28.Pescosolido BA, Wright ER, Alegria M, Vera M. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med Care. 1998;36:57–72. doi: 10.1097/00005650-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Abrams LS, Dornig K, Curran L. Barriers to service use for postpartum depression symptoms among low-income ethnic minority mothers in the United States. Qual Health Res. 2009;19:535–551. doi: 10.1177/1049732309332794. [DOI] [PubMed] [Google Scholar]
- 30.Peifer KL, Hu T, Vega W. Help seeking by persons of Mexican origin with functional impairments. Psychiatr Serv. 2000;51:1293–1298. doi: 10.1176/appi.ps.51.10.1293. [DOI] [PubMed] [Google Scholar]
- 31.Tijhuis MA, Peters L, Foets M. An orientation toward help-seeking for emotional problems. Soc Sci Med. 1990;31:989–995. doi: 10.1016/0277-9536(90)90108-5. [DOI] [PubMed] [Google Scholar]
- 32.Have M, Oldehinkel A, Vollebergh W, Ormel J. Does educational background explain inequalities in care service use for mental health problems in the Dutch general population? Acta Psychiatr Scand. 2003;107:178–187. doi: 10.1034/j.1600-0447.2003.00074.x. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez JM, Williams JW, Noel PH, Lee S. Adherence to mental health treatment in a primary care clinic. J Am Board Fam Pract. 2005;18:87–96. doi: 10.3122/jabfm.18.2.87. [DOI] [PubMed] [Google Scholar]
- 34.Fischer EH, Turner JI. Orientations to seeking professional help: development and research utility of an attitude scale. J Consult Clin Psych. 1970;35:79–90. doi: 10.1037/h0029636. [DOI] [PubMed] [Google Scholar]
- 35.Fischer EH, Farina A. Attitudes toward seeking professional psychological help: A shortened form and considerations for research. J Coll Student Dev. 1995;36:368–373. [Google Scholar]
- 36.Diala C, Muntaner C, Walrath C, Nickerson KJ, LaVeist TA, Leaf PJ. Racial differences in attitudes toward professional mental health care and in the use of services. Am J Orthopsychiatry. 2000;70:455–464. doi: 10.1037/h0087736. [DOI] [PubMed] [Google Scholar]
- 37.Leaf PJ, Bruce ML, Tischler GL. The differential effect of attitudes on the use of mental health services. Soc Psychiatry Psychiatr Epidemiol. 1986;21:187–192. doi: 10.1007/BF00583999. [DOI] [PubMed] [Google Scholar]
- 38.Norman RM, Sorrentino RM, Windell D, Manchanda R. The role of perceived norms in the stigmatization of mental illness. Soc Psychiatry Psychiatr Epidemiol. 2008;43:851–859. doi: 10.1007/s00127-008-0375-4. [DOI] [PubMed] [Google Scholar]
- 39.Kessler RC. National Comorbidity Survey: Replication (NCS-R), 2001–2003. [Accessed 12 August 2006];Inter-University Consortium for Political and Social Research (producer and distributor) 2006 http://www.hcp.med.harvard.edu/ncs/
- 40.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leaf PJ, Bruce ML, Tischler GL, Freeman DH, Jr, Weissman MM, Myers JK. Factors affecting the utilization of specialty and general medical mental health services. Med Care. 1988;26:9–26. doi: 10.1097/00005650-198801000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Albizu-Garcia CE, Alegria M, Freeman D, Vera M. Gender and health services use for a mental health problem. Soc Sci Med. 2001;53:865–878. doi: 10.1016/s0277-9536(00)00380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andrade LH, Viana MC, Tofoli LF, Wang YP. Influence of psychiatric morbidity and sociodemographic determinants on use of service in a catchment area in the city of Sao Paulo, Brazil. Soc Psychiatry Psychiatr Epidemiol. 2008;43:45–53. doi: 10.1007/s00127-007-0263-3. [DOI] [PubMed] [Google Scholar]
- 45.Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- 46.Briffault X, Sapinho D, Villamaux M, Kovess V. Factors associated with use of psychotherapy. Soc Psychiatry Psychiatr Epidemiol. 2008;43:165–171. doi: 10.1007/s00127-007-0281-1. [DOI] [PubMed] [Google Scholar]
- 47.Dew MA, Bromet EJ, Schulberg HC, Parkinson DK, Curtis EC. Factors affecting service utilization for depression in a white collar population. Soc Psychiatry Psychiatr Epidemiol. 1991;26:230–237. doi: 10.1007/BF00788971. [DOI] [PubMed] [Google Scholar]
- 48.Alegria M, Bijl RV, Lin E, Walters EE, Kessler RC. Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the United States with Ontario and The Netherlands. Arch Gen Psychiatry. 2000;57:383–391. doi: 10.1001/archpsyc.57.4.383. [DOI] [PubMed] [Google Scholar]
- 49.Muntaner C, Wolyniec P, McGrath J, Pulver AE. Differences in social class among psychotic patients at inpatient admission. Psychiatr Serv. 1995;46:176–178. doi: 10.1176/ps.46.2.176. [DOI] [PubMed] [Google Scholar]
- 50.Mechanic D, Bilder S. Treatment of people with mental illness: a decade-long perspective. Health Aff (Millwood) 2004;23:84–95. doi: 10.1377/hlthaff.23.4.84. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bancroft TA. Topics in Intermediate Statistics. Vol. 1. Iowa State University Press; Ames, Iowa: 1968. [Google Scholar]
- 53.Hosmer DW, Lemeshow S. Applied logistic regression. 1. Wiley; New Jersey: 1989. Model building strategies and methods for logistic regression. [Google Scholar]
- 54.Kleinbaum DG. Logistic regression: a self-learning text. Springer; New York: 1994. [Google Scholar]
- 55.Williams JW, Jr, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ. Primary care physicians’ approach to depressive disorders. Effects of physician specialty and practice structure. Arch Fam Med. 1999;8:58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]
- 56.Adeyemi JD, Olonade PO, Amira CO. Attitude to psychiatric referral: a study of primary care physicians. Niger Post-grad Med J. 2002;9:53–58. [PubMed] [Google Scholar]
- 57.Swindle R, Jr, Heller K, Pescosolido B, Kikuzawa S. Responses to nervous breakdowns in America over a 40-year period. Mental health policy implications. Am Psychol. 2000;55:740–749. doi: 10.1037//0003-066x.55.7.740. [DOI] [PubMed] [Google Scholar]
- 58.Dubow EF, Lovko KR, Kausch DF. Demographic differences in adolescents’ health concerns and perceptions of helping agents. J Clin Child Psychol. 1990;19:44–54. [Google Scholar]
- 59.West JS, Kayser L, Overton P, Saltmarsh R. Student perceptions that inhibit the initiation of counseling. School Counselor. 1991;39:77–83. [Google Scholar]
- 60.Schnittker J. Misgivings of medicine? African Americans’ skepticism of psychiatric medication. J Health Soc Behav. 2003;44:506–524. [PubMed] [Google Scholar]
- 61.Dana RH. Mental health services for African Americans: a cultural/racial perspective. Cultur Divers Ethnic Minor Psychol. 2002;8:3–18. [PubMed] [Google Scholar]
- 62.Wyatt GE, Powell GJ, Bass BA. The survey of Afro-American behavior: Its development and use in research. In: Bass B, Wyatt G, Powell GJ, editors. The assessment and treatment of Afro-American families: selected lectures. Grune & Stratton; New York: 1982. [Google Scholar]
- 63.Rogler LH, Cortes DE. Help-seeking pathways: a unifying concept in mental health care. Am J Psychiatry. 1993;150:554–561. doi: 10.1176/ajp.150.4.554. [DOI] [PubMed] [Google Scholar]
- 64.Croghan TW, Tomlin M, Pescosolido BA, Schnittker J, Martin J, Lubell K, Swindle R. American attitudes toward and willingness to use psychiatric medications. J Nerv Ment Disord. 2003;191:166–174. doi: 10.1097/01.NMD.0000054933.52571.CA. [DOI] [PubMed] [Google Scholar]
- 65.Andreasen A. Marketing social change: changing behavior to promote health, social development, and the environment. Jossey-Bass; San Francisco: 1995. [Google Scholar]